Abstract
Chronic granulomatous disease (CGD) is a rare X-linked or autosomal recessive disorder of early childhood due to defective nicotinamide adenine dinucleotide phosphate (NADPH) oxidase enzyme in leukocytes. It increases susceptibility to infections by catalase-positive bacteria and fungi. We report a case of an 18-year-old man with CGD who presented to the hospital with septic shock due to bacteremia, pneumonia, and osteomyelitis due to multiple rare microorganisms. Despite aggressive management, he did not survive. Increasing awareness about the common infections in this rare disease, their prevention, and lifelong treatment is warranted.
Keywords: rare autoimmune disease, antimicrobial prophylaxis , catalase positive, nadph oxidase, chronic granulomatous disease
Introduction
Chronic granulomatous disease (CGD) is a rare X-linked or autosomal recessive disorder that usually presents in early childhood between one to three years of age [1]. It affects about one in 250,000 individuals annually due to a defect in the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase enzyme in phagocytes [2]. The defect decreases the production of reactive oxygen species (ROS) for the respiratory burst reaction required to eliminate microorganisms. Individuals with CGD are prone to recurrent infections due to catalase-positive organisms such as Staphylococcus, Burkholderia, Aspergillus, Serratia, and Norcardia [3]. Early detection and treatment of infections and life-long antibiotic and antifungal prophylaxis are essential for survival. Unfortunately, many patients with CGD die in childhood due to infectious complications and survival up to adulthood has not been common until recently. We report a case of an 18-year-old man with a history of CGD and pulmonary aspergillosis who presented with recurrent catalase-positive infections.
Case presentation
An 18-year-old man presented to the Emergency Room (ER) with shortness of breath and cough of three weeks duration. He also reported low-grade fever and episodic vomiting. His past medical history was significant for CGD since early childhood, and a three-year history of pulmonary aspergillosis. Unfortunately, he was non-compliant with prophylactic levofloxacin and voriconazole. The patient’s family history was significant for CGD in his brother.
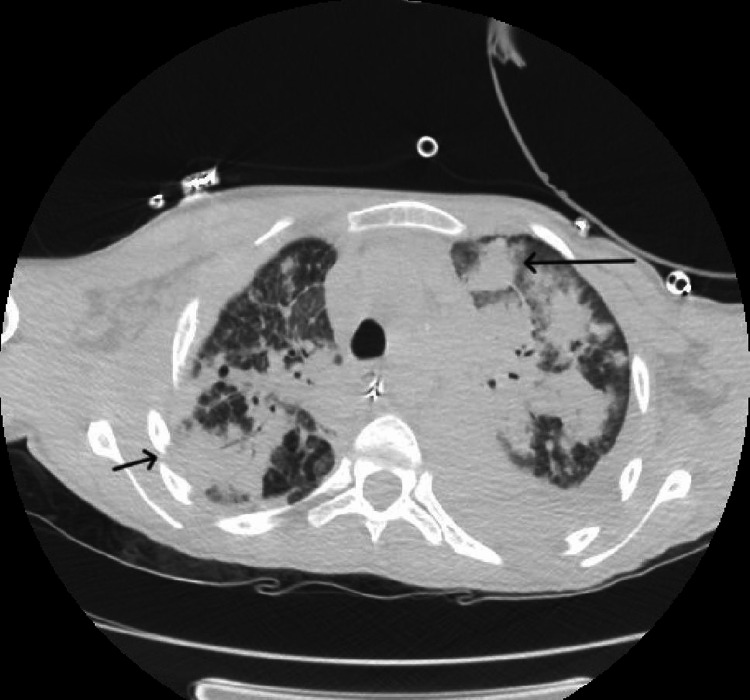
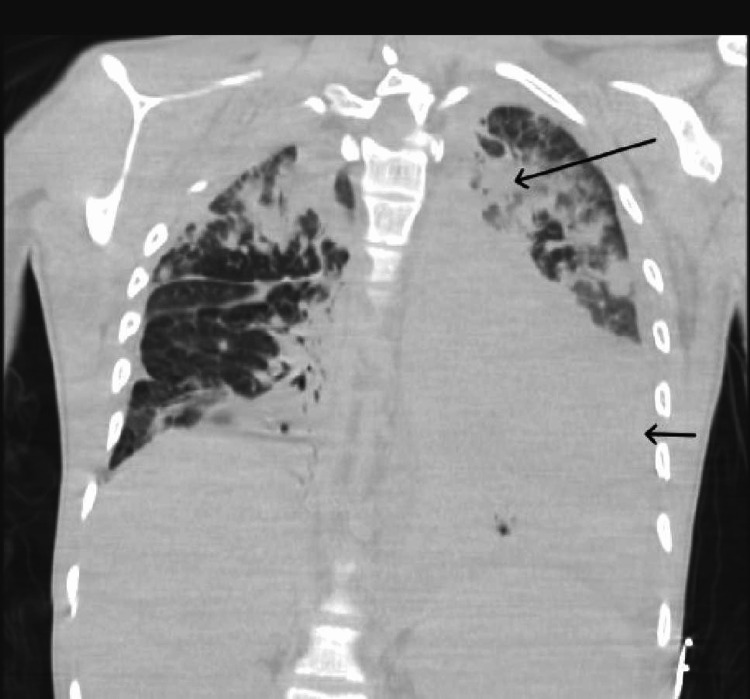
On physical examination, he had a temperature of 97.6 F, blood pressure of 97/61 mmHg, pulse of 137 per minute, respiratory rate of 30 per minute, and oxygen saturation of 82% on room air. He was in respiratory distress with diffuse bilateral crackles on lung examination. Despite initial resuscitation with fluids and oxygen, his hemodynamic instability escalated to require emergent intubation, initiation of mechanical ventilation, and vasopressors within a short time after the presentation. Laboratory results revealed leukocytosis, elevated transaminases, and acute renal failure (Table 1). Chest imaging showed bilateral nodular alveolar opacities, left pleural effusion, and bony destruction of the ribs (Figures 1, 2). Intravenous vancomycin, meropenem, and voriconazole were started, and he was admitted to the intensive care unit for further care.
Table 1. Blood investigations on admission.
| Test | Result | Reference range |
| White Blood Cell count | 130300 cells/mm3 | 4.8-10.8 x 1000 |
| Hemoglobin | 11.7 g/dL | 14.0-18.0 g/dL |
| Platelet | 218 x 1000 cells/mm3 | 130-400 x 1000 cells/mm3 |
| Sodium | 138 mmol/L | 136-145 mmol/L |
| Potassium | 5.6 mmol/L | 3.5-5.1 mmol/L |
| Chloride | 104 mmol/L | 98-107 mmol/L |
| Carbon Dioxide | 20 mmol/L | 25-35 mmol/L |
| Anion Gap | 14 | 8-14 |
| Blood Urea Nitrogen | 25 mg/dL | 8-22 mg/dL |
| Glucose | 158 mg/dL | 70-104 mg/dL |
| Creatinine | 1.0 mg/dL | 0.7-1.2 mg/dL |
| Calcium | 8.2 mg/dL | 8.8-10.2 mg/dL |
| Ferritin | 7717 ng/dL | 6-320 ng/dL |
| Aspartate Aminotransferase | 203 U/L | 10-34 U/L |
| Alanine Aminotransferase | 155 U/L | 10-44 U/L |
| Alkaline Phosphatase | 431 U/L | 30-224 U/L |
| Lactate Dehydrogenase | 429 U/L | 135-225 U/L |
| Creatine Kinase | 22 U/L | 24-204 U/L |
| C-Reactive Protein, Quantitative | 252.84 mg/L | 0-5 mg/L |
| Pro-B-Natriuretic Peptide | 2947 pg/mL | 5-93 pg/mL |
| Total Protein | 5.9 g/dL | 6.3-8.3 g/dL |
| Albumin | 2.4 g/dL | 3.5-5.0 g/dL |
| Lipase | 7 U/L | 13-60 U/L |
| Aspergillus galactomannan Antigen | >=3.750 | <0.5 index |
| Beta-(1,3)-D-Glucan | 339 pg/mL | <60 pg/mL |
| Blood culture | Burkholderia Cepacia, Staphylococcus Hominis |
Figure 1. CT chest with IV contrast demonstrating pulmonary nodules surrounded by ground glass opacities (big arrow) and bony destruction of ribs (small arrow).
CT: Computed Tomography, IV: Intravenous
Figure 2. CT chest with IV contrast demonstrating a large left pleural effusion (small arrow) and pulmonary nodules surrounded by ground glass opacities (large arrow).
CT: Computed Tomography, IV: Intravenous
Screening for Cryptococcus, Histoplasma, Legionella, Streptococcus, and SARS were negative. Screening for Aspergillus and Beta-(1, 3)-D-Glucan were positive (Table 1). Blood cultures returned positive for Burkholderia cepacia and Staphylococcus hominis. As a result, diagnoses of septic shock due to bilateral multifocal pneumonia, aspergillus osteomyelitis, and polymicrobial bacteremia were established. Unfortunately, the patient’s condition deteriorated over the next 48 hours with worsening hypoxia, hypotension, and multi-organ dysfunction. Although renal replacement therapy was attempted, it was interrupted due to hemodynamic instability. Ultimately, he went into cardiac arrest, and despite aggressive measures, recovery was unsuccessful, and the patient expired.
Discussion
CGD is an inherited immunodeficiency disorder due to a defective NADPH oxidase enzyme in phagocytes, which presents with recurrent infections and a persistent inflammatory state [4]. Genetic mutations in the structural proteins of NADPH oxidase complex lead to decreased hydrogen peroxide and ROS production, and inadequate respiratory burst [1,2,4]. Catalase-positive microorganisms break down even the limited hydrogen peroxide in phagocytes, making those with CGD more vulnerable to these species. Aspergillus, Staphylococcus aureus, Nocardia, Burkholderia, and Serratia are the most common organisms causing pneumonia, bacteremia, osteomyelitis, cellulitis, and abscess formation in CGD patients [5]. Additional complications arise from increased inflammatory response due to poor clearance of microbial material [3,4]. Phagocyte accumulation forms non-caseating granulomas, especially in the lungs and gastrointestinal tract [3,4]. Patients may also develop hepatosplenomegaly, chorioretinitis, interstitial pulmonary fibrosis, and inflammatory bowel disease [6].
Dihydrorhodamine 123 test (DHR) or Nitroblue Tetrazolium (NBT) test is performed to diagnose CGD. Following positive results, genetic testing is performed to determine the type of CGD: X-linked or autosomal recessive [7]. Lifelong prophylaxis with an antibiotic, e.g., trimethoprim-sulfamethoxazole, and an antifungal, e.g., itraconazole, remains a cornerstone in managing CGD [8]. However, infections occur in about 0.3% of patients with CGD per year, regardless [4]. Prompt treatment of acute infections with empiric antimicrobials targeting the above organisms is crucial [2,4]. Additional treatment with interferon-gamma (IFN-y) and corticosteroids is being considered but large-scale clinical trials have not studied their efficacy [4]. Although a cure for CGD is still being investigated, advanced knowledge in its management has recently improved median life expectancy to around 30-40 years. Hematopoietic stem cell transplantation and gene therapy are treatment alternatives but accompany their own risks [9,10].
The patient in the present case was non-compliant with the antimicrobial prophylaxis for about one year despite having a past history of pulmonary aspergillosis. This drastically placed him at extreme risk for recurrent infections. Also, there was a significant delay in seeking medical attention. Despite aggressive resuscitation and the institution of broad-spectrum antibiotics and antifungals, an untoward outcome could not be averted.
Conclusions
This case provides a classic clinical presentation of a rare clinical entity. The patient was found to have infections with two catalase-positive organisms: Burkholderia and Aspergillus. His imaging also revealed bilateral diffuse granulomas classically seen in pulmonary aspergillosis. Pneumonia and osteomyelitis due to such rare organisms leading to septic shock were unique to this case. Although rare, this case highlights the importance of knowledge of the infections CGD patients are susceptible to. Increasing life expectancy among these patients means more patients with CGD present with infectious manifestations in adulthood. Hence, knowledge about CGD, early diagnosis, and aggressive management of infections are essential. Life-long prophylaxis with antimicrobials reduces the rate of severe infections and remains the cornerstone of CGD management.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Chronic granulomatous disease: Epidemiology, pathophysiology, and genetic basis of disease. Rider NL, Jameson MB, Creech CB. J Pediatric Infect Dis Soc. 2018;7:0–5. doi: 10.1093/jpids/piy008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chronic granulomatous disease. Roos D. Br Med Bull. 2016;118:50–63. doi: 10.1093/bmb/ldw009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Progress in treating chronic granulomatous disease. Gennery AR. Br J Haematol. 2021;192:251–264. doi: 10.1111/bjh.16939. [DOI] [PubMed] [Google Scholar]
- 4.A review of chronic granulomatous disease. Arnold DE, Heimall JR. Adv Ther. 2017;34:2543–2557. doi: 10.1007/s12325-017-0636-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chronic granulomatous disease. Report on a national registry of 368 patients. Winkelstein JA, Marino MC, Johnston RB Jr, et al. Medicine (Baltimore) 2000;79:155–169. doi: 10.1097/00005792-200005000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Images in clinical medicine. Chronic granulomatous disease. Esfandbod M, Kabootari M. N Engl J Med. 2012;367:753. doi: 10.1056/NEJMicm1106350. [DOI] [PubMed] [Google Scholar]
- 7.Genotype-dependent variability in flow cytometric evaluation of reduced nicotinamide adenine dinucleotide phosphate oxidase function in patients with chronic granulomatous disease. Vowells SJ, Fleisher TA, Sekhsaria S, Alling DW, Maguire TE, Malech HL. J Pediatr. 1996;128:104–107. doi: 10.1016/s0022-3476(96)70437-7. [DOI] [PubMed] [Google Scholar]
- 8.Chronic granulomatous disease: recent advances in pathophysiology and treatment. Seger RA. https://www.njmonline.nl/getpdf.php?id=979. Neth J Med. 2010;68:334–340. [PubMed] [Google Scholar]
- 9.Outcome of chronic granulomatous disease - conventional treatment vs stem cell transplantation. Dedieu C, Albert MH, Mahlaoui N, et al. Pediatr Allergy Immunol. 2021;32:576–585. doi: 10.1111/pai.13402. [DOI] [PubMed] [Google Scholar]
- 10.Late diagnosis and advances in genetics of chronic granulomatous disease. Di Matteo G, Finocchi A. Clin Exp Immunol. 2021;203:244–246. doi: 10.1111/cei.13554. [DOI] [PMC free article] [PubMed] [Google Scholar]