Abstract
Multiple independent frameworks to support continuous improvement have been proposed to guide healthcare organizations. Two of the most visible are High‐reliability Health care, (Chassin et al., 2013) which is emphasized by The Joint Commission, and Learning Health Systems, (Institute of Medicine, 2011) highlighted by the National Academy of Medicine. We propose that organizations consider tightly linking these two models, creating a “Highly‐reliable Learning Health System.” We describe several efforts at our organization that has resulted from this combined model and have helped our organization weather the COVID‐19 pandemic. The organizational changes created using this framework will enable our health system to support a culture of quality across our teams and better fulfill our tripartite mission of high‐quality care, effective education of trainees, and dissemination of important innovations.
Keywords: clinical informatics, high reliability, learning health system
Multiple independent frameworks have evolved to guide healthcare organizations on a journey of continuous improvement. Two of the most visible and promising are as follows: High‐reliability Healthcare 1 which is emphasized by The Joint Commission, and Learning Health Systems, highlighted by the National Academy of Medicine. 2 A key component of Learning Health Systems is the connection between the discovery of improvement opportunities and the implementation of changes to realize these opportunities. 3 Highly reliable healthcare organizations, on the other hand, develop and reward teams who embrace the responsibility to identify and address unsafe or problematic conditions before they lead to substantial harm to patients or the organization. 1 At UC San Diego Health, the COVID‐19 pandemic has highlighted the unique benefits of applying high‐reliability approaches to this “implementation arm” of the Learning Health System, resulting in an explicit focus on leveraging elements from both frameworks to develop a “Highly‐reliable Learning Health System.”
This intentional transformation involves deliberate coordination among clinical operations, electronic health record and informatics support, and clinical research infrastructure to analyze rapidly different types of data to generate new knowledge and efficiently incorporate it into care processes. This work is predicated on core tenets of sharing data within our organization, translating these data to actionable knowledge and efficiently feeding this knowledge back to our patients and care teams, and has been adopted at other organizations as well. 4 , 5 We credit this systematic approach and the resulting culture for the success our organization has had preserving our high‐quality care despite a national backslide in quality outcomes during the COVID‐19 pandemic. 6 Continual mining of data from our electronic health record is generating real‐world evidence that informs local healthcare practices and influences national policies.
In March 2020, shortly after the pandemic was recognized by the World Health Organization, our teams shared ways in which our electronic health records were being optimized for COVID treatment. 7 This infrastructure made it possible to rapidly provide highly‐reliable COVID screening and testing for our university students, 8 deploy artificial intelligence (AI) algorithms across all of our radiology imaging to aid in COVID diagnosis, 9 deploy one of the country's first vaccine superstations, 10 understand the implications of different exposure notification approaches, 11 track real‐world data on vaccine effectiveness in our employees 12 which was cited by the FDA 13 and CDC 14 in their evaluation of boosters, and track cancer stage at diagnosis pre‐ and post‐pandemic. 15
These examples of our efforts to engineer a highly‐reliable, learning health system were enabled by a set of intentional decisions about the organizational structure. 4 To better connect our data science and researchers to the decision‐making and operational needs of the health system, an academic biomedical informatics group established over a decade ago has become the academic home for health system leaders such as the Chief Medical Officer, Clinical Research Information Officer, Chief Medical Information Officer, and others. As a result, research faculty with expertise in the use of clinical data for modeling and implementing predictive algorithms are key partners with our operational teams.
Within the health system, we have also established a committee to Align and Coordinate Quality Improvement, Research, and Evaluation (ACQUIRE)—a multidisciplinary group with representation from clinicians (physicians, nurses, advanced practice providers, pharmacists), quality improvement leaders, researchers, institutional review board (IRB), medical education, and project management. Figure 1 shows the high‐level relationships between the different entities in our system. The ACQUIRE effort has four broad goals: supporting the alignment of improvement projects with the health system priorities, facilitating multidisciplinary involvement, improving the visibility of improvement activities across the organization, and supporting outcomes evaluation and scholarship.
FIGURE 1.
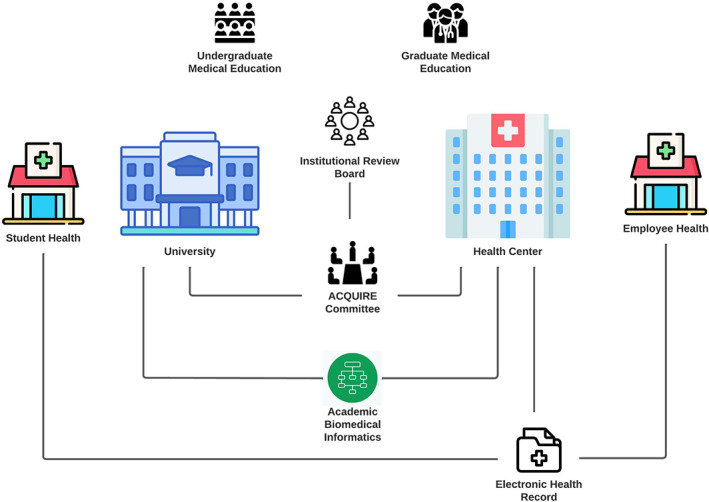
Highly reliable Learning health system
One of the intentional incentives we established for medical staff leaders to submit QI projects to ACQUIRE is the possibility of American Board of Medical Specialties maintenance of certification (MOC) credit through our organization's MOC Portfolio Program. Since inception during the pandemic, ACQUIRE has evaluated 90 projects with submissions occurring consistently over time, and MOC credit was granted to 30 physicians in our first year using this mechanism. Figure 2 displays the monthly counts of project submissions, broken down by the types of evaluations requested by the project teams. After establishing our ACQUIRE Committee, there was a concerted effort to communicate the efficiency, project visibility and MOC benefits of these new processes to our broad QI community. We believe that the increased number of submissions over time reflects the results of these efforts.
FIGURE 2.
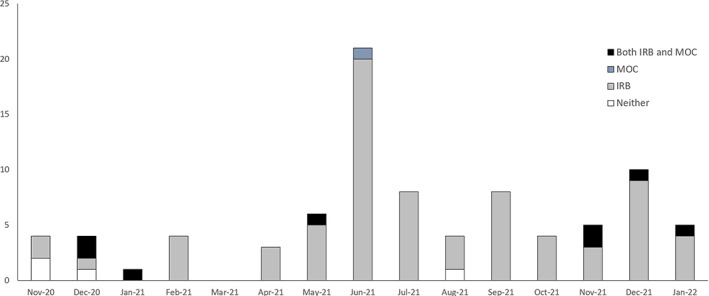
Project submissions to the ACQUIRE Committee at UC San Diego Health
An emphasis of the highly reliable, learning health system is to engage the capability for innovations from our clinical research community and link these efforts to the reliability focus of our operational implementation teams. To support this goal, we have worked to increase the visibility of active improvement efforts to catalyze opportunities for collaboration, and we also celebrate scholarship related to improvement efforts through multiple channels such as follows: weekly physician and advanced practice provider newsletter, monthly Transformation Team presentations that describe active projects, quarterly medical director town halls that highlight recent improvement publications authored by team members, and an annual GME Patient Safety/Quality Improvement Symposium which highlights the projects involving our graduate trainees. The ACQUIRE Committee contributes to this increased visibility by maintaining an organization‐wide repository of improvement projects. This searchable repository is accessible by all team members and has centralized visibility across the organization into a previously distributed collection of active projects. We are also connecting this project repository to our academic training programs to enable both undergraduate and graduate medical trainees to find opportunities to gain real‐world project experience within the healthcare setting. ACQUIRE serves as a key focal point for improvement efforts and enables all of our team members to identify quickly potential collaborators working on similar efforts and to efficiently initiate projects if there is not an existing team addressing the need.
Another strategy for integrating innovation and improvement into the fabric of our day‐to‐day work is broadly available training in quality improvement methodologies to all team members, including graduate medical trainees. A fundamental aspect of this philosophy is the value of the front‐line team members to identify improvement opportunities and help craft solutions. We reinforce the importance of this work by highlighting project outcomes and scholarship through multiple venues, including our daily engagement system huddles, employee and trainee town halls, quality improvement and clinical research symposia, and organization‐wide newsletters.
The pandemic has brought the benefits of rapid learning from our data into sharp focus. Like elsewhere, our patients, providers, trainees and healthcare leaders confronted evolving vaccine availability, vaccination recommendations and personal protective equipment policies. In addition to enabling data‐driven responses to these dynamic forces, our infrastructure enabled transparent sharing of near real‐time data to instill confidence in our approaches, reassurance about the safety of our work environments, and helped mitigate the considerable sense of uncertainty in our community.
Through the changes we describe, we aim to create a paradigm shift with an intentional organizational structure and processes that align quality improvement and clinical research innovations with our operational priorities, and to integrate their initiation and monitoring into standard clinical work. Key strategies are to: (1) Integrate individuals with informatics expertise into operational teams, (2) Align QI projects with health system priorities; (3) Utilize incentives to promote clinician engagement; (4) Make QI priorities, efforts and successes visible enterprise‐wide; (5) Provide QI training for all team members. These strategies align well with recently published recommendations by AHRQ and PCORI‐funded Learning Health Systems Centers of Excellence. 16 These efforts to develop a highly‐reliable learning health system have created a system that incentivizes and reinforces a culture of quality among a wide range of team members, and amplifies our tripartite mission of high‐quality care, education of trainees, and dissemination of important innovations.
CONFLICT OF INTEREST
None of the authors have conflicts to disclose.
ACKNOWLEDGMENTS
We thank and acknowledge members of UC San Diego Health who have been instrumental in supporting our organization's ongoing improvement, including Patty Maysent, Chief Executive Officer of UC San Diego Health, Chad VanDenBerg, Chief Quality and Patient Safety Officer; Dr. Lucila Ohno‐Machado, Associate Dean for Informatics and Technology, Kip Kantelo, Director of UC San Diego IRB; Peter Chu and Eric Lundin, Project Managers for ACQUIRE, and the dedicated members of our ACQUIRE Committee.
El‐Kareh R, Brenner DA, Longhurst CA. Developing a highly‐reliable learning health system. Learn Health Sys. 2023;7(3):e10351. doi: 10.1002/lrh2.10351
REFERENCES
- 1. Chassin MR, Loeb JM. High‐reliability health care: getting there from here. Milbank Q. 2013;91(3):459‐490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Institute of Medicine . The learning health system and its innovation collaboratives: update report. IOM. 2011;7‐31. [Google Scholar]
- 3. Friedman CP. What is unique about learning health systems? Learn Health Syst. 2022;6(1):e10328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Payne PRO, Wilcox AB, Embi PJ, Longhurst CA. Better together: integrating biomedical informatics and healthcare IT operations to create a learning health system during the COVID‐19 pandemic. Learn Health Syst. 2022;6(2):e10309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Johnson KB, Patel NR. Biomedical informatics and health information technology: a critical, pragmatic collaboration for clinical transformation. J Gen Intern Med. 2021;36(2):530‐532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fleisher LA, Schreiber M, Cardo D, Srinivasan A. Health care safety during the pandemic and beyond ‐ building a system that ensures resilience. N Engl J Med. 2022;386(7):609‐611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID‐19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020;27(6):853‐859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reeves JJ, Longhurst CA, San Miguel SJ, et al. Bringing student health and well‐being onto a health system EHR: the benefits of integration in the COVID‐19 era. J Am Coll Health. 2022;70(7):1968‐1974. [DOI] [PubMed] [Google Scholar]
- 9. Carlile M, Hurt B, Hsiao A, Hogarth M, Longhurst CA, Dameff C. Deployment of artificial intelligence for radiographic diagnosis of COVID‐19 pneumonia in the emergency department. J Am Coll Emerg Phys Open. 2020;1(6):1459‐1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Longhurst CA, Kremer B, Maysent PS. Rapid implementation of a vaccination superstation. JAMA. 2021;325(10):931‐932. [DOI] [PubMed] [Google Scholar]
- 11. Tai‐Seale M, May N, Sitapati A, Longhurst CA. A learning health system approach to COVID‐19 exposure notification system rollout. Learn Health Syst. 2022;6(2):e10290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Keehner J, Horton LE, Binkin NJ, et al. Resurgence of SARS‐CoV‐2 infection in a highly vaccinated health system workforce. N Engl J Med. 2021;385(14):1330‐1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Oliver S. Vaccines and related biological products advisory committee 2021 Meeting Presentation—Updates to COVID19 Epidemiology and Vaccines 2021; https://www.fda.gov/media/152243/download.
- 14. Oliver S. ACIP meeting: evidence to recommendation framework: Pfizer‐BioNTech COVID‐19 booster dose. 2021; https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-9-23/03-COVID-Oliver.pdf.
- 15. Zhou JZ, Kane S, Ramsey C, et al. Comparison of early‐ and late‐stage breast and colorectal cancer diagnoses during vs before the COVID‐19 pandemic. JAMA Netw Open. 2022;5(2):e2148581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lozano PM, Lane‐Fall M, Franklin PD, et al. Training the next generation of learning health system scientists. Learn Health Syst. 2022;6(4):e10342. [DOI] [PMC free article] [PubMed] [Google Scholar]


