Abstract
Introduction
During stent grafting, managing the internal iliac artery (IIA) becomes a significant issue when an abdominal aortic aneurysm (AAA) is complicated by bilateral common iliac artery (CIA) aneurysms. The iliac branch system (IBS) has a defined length; therefore, the CIA should be sufficiently long. However, situations arise where the IBS must be used even in patients with a short CIA. A case of contralateral CIA occlusion due to deviation of the proximal iliac branched component of the IBS is reported.
Report
A 73 year old man underwent stent grafting with inferior mesenteric artery coil embolisation and IBS for a 70 mm AAA and >30 mm bilateral CIA aneurysm. As standard procedure, the right iliac branched component and the internal iliac component were used. After removing the guidewire used for deploying the internal iliac component, the left 12 Fr Dryseal and guidewire were pulled down. The proximal end of the right iliac branched component deviated over the left CIA origin, resulting in CIA occlusion. As a solution, a 12 Fr Dryseal was inserted with a dilator and guidewire in the 16 Fr Dryseal from the left side, following which the tip of the 12 Fr Dryseal dilator was used to push the iliac branched component to create a gap. The guidewire was successfully inserted, and the surgery was subsequently completed as planned. The post-operative course of the patient was uneventful.
Conclusion
When deploying an iliac branched component in cases where the CIA is shorter than the length of the component, it is crucial to place the contralateral guidewire into the aorta before pulling down the contralateral sheath. The iliac branched component may follow the pull through wire and occlude the contralateral CIA. Furthermore, if the element occludes the contralateral CIA, it can be managed using this method.
Keywords: Abdominal aortic aneurysm, Common internal artery aneurysm, Endovascular aortic repair, Iliac branch endoprosthesis
Highlights
-
•
Common iliac artery aneurysms complicate abdominal aortic aneurysms.
-
•
Managing the internal iliac artery in such cases is challenging.
-
•
Deviation of the proximal end of the iliac branched component covered and occluded the contralateral common iliac artery origin.
-
•
The iliac branched component may follow the pull through wire and occlude the contralateral common iliac artery.
-
•
Placing a guidewire in the aorta before pulling the contralateral sheath is crucial.
Introduction
Nearly 10% of abdominal aortic aneurysms (AAAs) are reportedly complicated by common iliac artery (CIA) aneurysms.1 For stent graft surgery, preserving the internal iliac artery (IIA) in the presence of bilateral CIA aneurysms is essential. In addition, many Asians, including the Japanese,2 have a short CIA. The iliac branch system (IBS) has a defined length; therefore, the CIA should be sufficiently long. However, situations arise where the IBS must be used in patients with a short CIA to avoid open surgery.
A case of contralateral CIA occlusion is reported that was caused by deviation of the proximal end of the iliac branched component of the IBS during the treatment of an AAA complicated by bilateral CIA aneurysms using the Gore Excluder Iliac Branch System (W. L. Gore & Associates, Flagstaff, AZ, USA).
Report
A 73 year old man visited an orthopaedic surgeon complaining of left thigh pain. He was referred on after magnetic resonance imaging (MRI) incidentally revealed an AAA and bilateral CIA aneurysms. He had no history of regular visits to the hospital and had undergone percutaneous coronary intervention for unstable angina three months prior to his visit to the department. Since then, he had been treated for hypertension and dyslipidaemia on an outpatient basis. Contrast enhanced computed tomography (CT) showed an infrarenal AAA with a maximum infrarenal diameter of 70 mm and CIA aneurysms 32 mm on the right and 30 mm on the left with a 5 mm inferior mesenteric artery (IMA) (Fig. 1). The distance from the lowest renal artery to the aortic bifurcation was 156 mm, the right CIA was 47 mm, and the left CIA was 50 mm in length. As the patient was in the early post-percutaneous coronary intervention period, discontinuation of antiplatelet medications was not an option. After discussing with the patient, the method of preserving the internal iliac artery, including the advantages of gluteal blood flow and sexual function and the disadvantages of procedural complexity, the patient was treated with stent grafting using a bilateral IBS followed by IMA coil embolisation.
Figure 1.
Pre-operative contrast enhanced computed tomography.
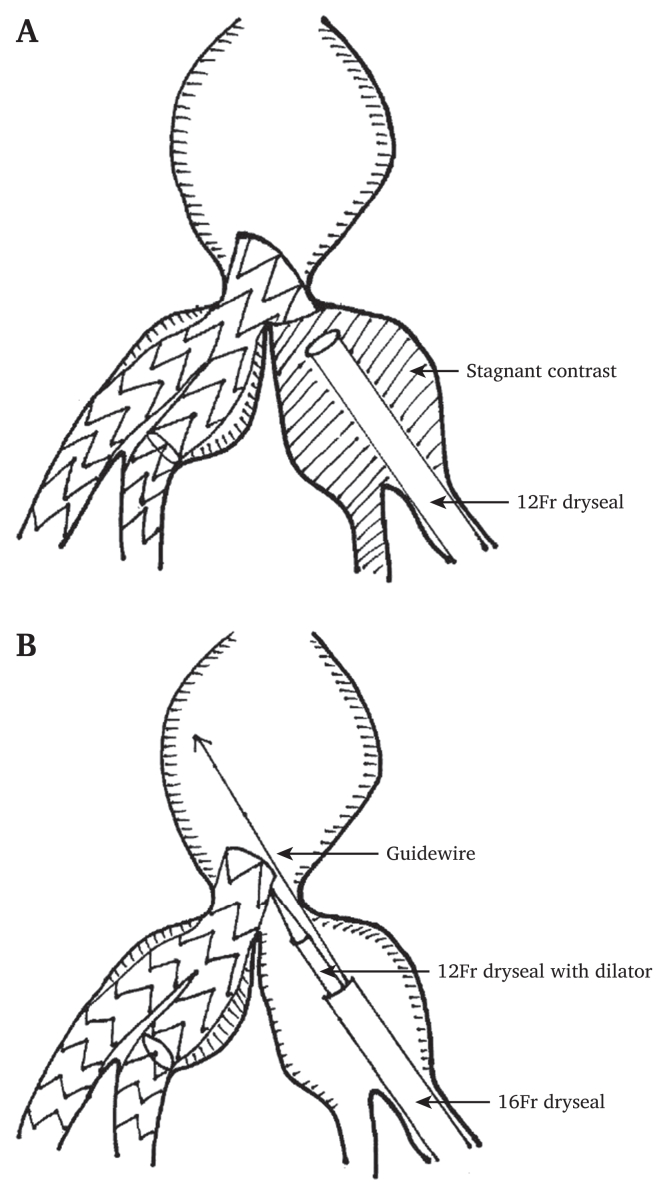
Surgery was performed under general anaesthesia. The approach was via both common femoral arteries, and a percutaneous technique was used. IMA coil embolisation was performed first. The right proximal iliac branched component and the internal iliac component were deployed following standard manoeuvres. After removing the pull through wire, the external iliac part of the iliac branched component was completely deployed, and the left 12 Fr Dryseal (W. L. Gore & Associates, Flagstaff, AZ, USA) was pulled down into the left CIA. Then, the Amplatz straight, short tip super stiff wire (Cook Medical, Bloomington, IN, USA) used for internal iliac component deployment could not proceed into the aorta due to insufficient back up force. Therefore, the super stiff wire was removed because the intention was to change the flexible wire for safety. The proximal end of the right proximal iliac branched component deviated to cover the left CIA origin following a pull through wire procedure, resulting in complete left CIA occlusion (Fig. 2A). Subsequently, the passage of the guidewire became impossible. As a solution, a 12 Fr Dryseal was inserted with a dilator in the 16 Fr Dryseal from the left side and a guidewire from the side of the 12 Fr Dryseal. Following this, the tip of the 12 Fr Dryseal dilator was used to push the iliac branched component to create a gap through which the guidewire passed successfully (Fig. 2B). The left iliac branched component was then inserted. Subsequently, the trunk ipsilateral leg, contralateral leg, and aorta extender were placed, and the surgery was completed.
Figure 2.
(A) The proximal side of the right iliac branched component deviates to cover the left CIA origin following a pull through wire procedure, resulting in complete CIA occlusion. (B) The tip of the 12 Fr Dryseal dilator is used to push the iliac branched component to create a gap.
The post-operative course was uneventful. CT on a post-operative day five showed no endoleaks and a maximum infrarenal diameter of 70 mm, 50 mm at six months, and 40 mm at 12 months post-operatively, indicating a decrease in aortic sac diameter over time (Fig. 3). In addition, the enhanced CT at 12 months post-operatively showed thrombus in the left IIA graft, but all branches remained patent (Supplementary Video S1).
Figure 3.
(A) Post-operative contrast enhanced computed tomography. (B–D) Computed tomography images show no endoleaks and a significant reduction in the diameter of the aneurysm over time. These were at five days (B), six months (C), and 12 months (D) after surgery.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.ejvsvf.2023.05.017
The following is/are the supplementary data related to this article:
Pre-operative and 12-months after operative contrast enhanced CT.1
Discussion
Managing the internal iliac artery during stent grafting is concerning, especially when bilateral CIA aneurysms complicate AAA. Occlusion of the bilateral internal iliac arteries is associated with intestinal ischaemia, persistent buttock claudication, and impotence.3,4 Therefore, it is strongly recommended to preserve at least one IIA when treating AAAs with stent grafts.5 However, it remains debatable whether both IIAs should be preserved. As unilateral preservation is associated with more claudication and sexual dysfunction than bilateral preservation,6 it is necessary to design an appropriate strategy for each patient.
This was a case in which the proximal end of the iliac branched component occluded the contralateral CIA origin in a patient with a short right CIA that was rescued intra-operatively using an endovascular approach. The iliac branched component was delivered through a stiff guidewire inserted into the aorta. Simultaneously, when inserting the internal iliac component, it is necessary to cross the large diameter sheath after passing the guidewire through the contralateral side using the pull through technique. The iliac branched component of the Gore Excluder Iliac Branch System was 55 mm from the proximal edge of the iliac branched component to the distal edge of the internal iliac gate. Other available devices exist; however, their lengths are similar. If the CIA is shorter, it may extend out onto the contralateral side. Banzic et al. reported that Asians had significantly shorter CIAs than Caucasians (right: 33.1 vs. 65.0 mm, left: 35.2 vs. 65.0 mm).2 Hence, the risk of obstruction is always increased in cases with a short CIA, especially among Asians.
Ideally, the CIA should be longer than the device, but since the instructions for use do not limit the length of the CIA, the IBS may be selected after considering various treatment options, as in this case. To avoid this situation, there are some solutions to deal with the short CIA. First, the Gore Excluder Iliac Branch System has a length of 30 mm from the proximal edge to the origin of the internal iliac gate. After the proximal deployment, the device can be pulled down to insert the internal iliac part into the IIA. However, the technique cannot always be done because of anatomical variation. Second, to prevent deviation of the iliac branched component to cover the contralateral CIA origin, upper limb access or an up and over manoeuvre7 could be considered. However, it is essential to use covered stents that are not for internal iliac components, which might be off label use. If the CIA is extremely short, the above method may be chosen, but this matter can occur even when the standard procedure seems to work. For the above reasons, the guidewire should be advanced while the contralateral sheath tip is in the terminal aorta to avoid insufficient back up force.
In conclusion, when deploying the iliac branched component in cases of short CIA, it is crucial to place the guidewire into the aorta before pulling down the contralateral sheath because the iliac branched component may follow the pull through wire and occlude the contralateral CIA origin. Furthermore, if the element blocks the contralateral CIA, it can be managed using this method.
Conflict of interest and funding statement
None.
Ethics approval and informed consent
The study participant provided informed consent. This study was approved by the Sapporo Teishinkai Hospital Ethics Committee (Record 2022–98).
References
- 1.Dix F.P., Titi M., Al-Khaffaf H. The isolated internal iliac artery aneurysm – a review. Eur J Vasc Endovasc Surg. 2005;30:119–129. doi: 10.1016/j.ejvs.2005.04.035. [DOI] [PubMed] [Google Scholar]
- 2.Banzic I., Lu Q., Zhang L., Stepak H., Davidovic L., Oszkinis G., et al. Morphological differences in the aorto-iliac segment in AAA patients of Caucasian and Asian Origin. Eur J Vasc Endovasc Surg. 2016;51:783–789. doi: 10.1016/j.ejvs.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 3.Karch L.A., Hodgson K.J., Mattos M.A., Bohannon W.T., Ramsey D.E., McLafferty R.B. Adverse consequences of internal iliac artery occlusion during endovascular repair of abdominal aortic aneurysms. J Vasc Surg. 2000;32:676–683. doi: 10.1067/mva.2000.109750. [DOI] [PubMed] [Google Scholar]
- 4.Mehta M., Veith F.J., Ohki T., Cynamon J., Goldstein K., Suggs W.D., et al. Unilateral and bilateral hypogastric artery interruption during aortoiliac aneurysm repair in 154 patients: a relatively innocuous procedure. J Vasc Surg. 2001;33(Suppl):S27–S32. doi: 10.1067/mva.2001.111678. [DOI] [PubMed] [Google Scholar]
- 5.Chaikof E.L., Dalman R.L., Eskandari M.K. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018;67:2–77. doi: 10.1016/j.jvs.2017.10.044. [DOI] [PubMed] [Google Scholar]
- 6.Rayt H.S., Bown M.J., Lambert K.V., Fishwick N.G., McCarthy M.J., London N.J., et al. Buttock claudication and erectile dysfunction after internal iliac artery embolization in patients before endovascular aortic aneurysm repair. Cardiovasc Intervent Radiol. 2008;31:728–734. doi: 10.1007/s00270-008-9319-3. [DOI] [PubMed] [Google Scholar]
- 7.Tenorio E.R., Oderich G.S., Sandri G.A., Kärkkäinen J.M., Kalra M., DeMartino R.R., et al. Outcomes of an iliac branch endoprosthesis using an “up-and-over” technique for endovascular repair of failed bifurcated grafts. J Vasc Surg. 2019;70:497–508. doi: 10.1016/j.jvs.2018.10.098. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pre-operative and 12-months after operative contrast enhanced CT.1