Abstract
Background:
This study represents the clinical results, especially range of motion (ROM) improvement, of arthroscopic partial trapeziectomy with suture-button suspensionplasty for symptomatic grade II and III thumb carpometacarpal arthritis with a minimum 1-year follow-up.
Methods:
Thirty-two patients (mean: 67.5 years) with grade II and III thumb carpometacarpal arthritis treated with arthroscopic partial trapeziectomy with suture-button suspensionplasty were retrospectively followed up for at least 1 year. The physical assessments included ROM, pain visual analogue scale (VAS), strength, and the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire. The physical variables were retrospectively compared before surgery and at the final follow-up.
Results:
Preoperative radial abduction and palmar abduction (45.4 ± 16.4° and 54.3 ± 13.9°, respectively) were significantly increased at the final follow-up (59.7 ± 16.9° and 65.5 ± 14.2°, respectively). Preoperative VAS score, pinch strength, and DASH score (70.5 ± 14.0, 57.2 ± 24.8% and 36.8 ± 14.8, respectively) were also significantly improved at the final follow-up (7.9 ± 9.1, 91.0 ± 39.6%, and 11.7 ± 10.5, respectively). Complications involved 1 case of irritation of the superficial branch of the radial nerve and 1 case of dystonia. Two suture-buttons were removed due to patient discomfort.
Conclusions:
A significant increase in ROM and pain relief was obtained after suture-button suspensionplasty with arthroscopic partial trapeziectomy.
Keywords: carpometacarpal joint, arthroscopy, osteoarthritis, suture-button
Introduction
For symptomatic grades II and III thumb carpometacarpal (CMC) arthritis, which are characterized by joint-space narrowing, subluxation, sclerosis, and cystic changes with osteophytes or loose bodies, hand surgeons perform many kinds of surgery (eg, total or partial trapeziectomy with or without ligament reconstruction, hematoma distraction arthroplasty, arthrodesis, and arthroplasty).1-8 It has been reported that no single operation produces better outcomes than another, and surgeons tend to favor particular operations according to their own or their trainers’ personal biases. 9 The goal of the treatment for CMC arthritis should be to improve the pain and the joint movements. Carpometacarpal arthroplasty with suture-button suspensionplasty has been developed and predictable results have been reported.10-14 To date, however, few studies have reported that this procedure improves the range of motion (ROM) of the thumb CMC joint.
The purpose of this study is to report the treatment results of arthroscopic partial trapeziectomy with suture-button suspensionplasty for symptomatic grades II and III thumb CMC arthritis. We hypothesized that this procedure would improve the pain and the radial and palmar abduction ROM of the thumb CMC joint.
Materials and Methods
Between January 2016 and August 2020, we treated 33 patients who underwent suture-button suspensionplasty with arthroscopic partial trapeziectomy for symptomatic thumb CMC arthritis, which is resistant to conservative treatment. We designed a retrospective study with data obtained at a follow-up of 1 year or more. This study was approved by the institutional review board, the Ethics Committee of Kyoto University Graduate School and Faculty of Medicine. All patients signed written informed consent. We reviewed all medical records retrospectively to obtain surgical results and complications.
Indications for surgery were persistent symptoms despite a minimum of 6 months of nonsurgical treatment and radiographic signs of Eaton stage II or III osteoarthritis. Patients who underwent surgery to address thumb CMC arthritis with combined arthroscopic partial trapeziectomy and suture-button suspensionplasty were followed up at least 1 year after surgery. Contraindications included patients with Eaton stage IV osteoarthritis, systematic inflammatory arthritis, or hyperlaxity syndromes.
Surgical Technique
All partial trapeziectomies are performed under arthroscopy. General or regional anesthesia is used with tourniquet control. A standard wrist traction tower and equipment with a 1.9-mm arthroscope is used for the procedure. The thumb is placed alone in a finger trap and suspended with approximately 4 kg of longitudinal traction. At the level of the thumb CMC joint, a 1-R portal is made with a 5-mm skin incision radial to the abductor pollicis longus tendon. A 1-U portal is made in the same manner, immediately ulnar to the extensor pollicis brevis tendon. The 1.9-mm arthroscope is inserted through the 1-U portal, and the 1-R portal is used as the working portal. The scope and the working instrument are sometimes interchanged, depending on the location of the osteophytes. We also sometimes employ the thenar portal described by Walsh et al. 15 We use the thenar portal for the scope and the 1-U and 1-R portals for the abrader bar. All procedures are performed under dry conditions.
Synovium and degenerative articular cartilage are removed using a 2.0-mm cutting shaver through the 1-R portal. Any free bodies are removed using a small punch. Next, we begin the hemitrapeziectomy using a 2.9-mm barrel burr and a 3.5-mm abrader burr through the 1-R portal. The resection volume of the trapezium is approximately 3 mm from the CMC joint surface. Alternating the instruments and the arthroscope between the portals is carried out. Visualization through the thenar portal and working through the 1-R and 1-U portals is also employed for resection of the residual bone. The dorsomedial osteophyte of the trapezium surface was also removed and confirmed by fluoroscopy.
After making CMC space, a Mini-TightRope fixation system (Arthrex, Naples, Florida) is used to suspend and medialize the thumb metacarpal. The 1-R skin incision is extended 1 cm distally and the thenar muscle is dissected to expose the radial aspect of the proximal thumb metacarpal. The second 2-cm incision is made along the proximal second metacarpal to protect the radial sensory branch and expose the proximal part of the second metacarpal. A passer guidewire is passed from the volar-radial thumb metacarpal base to the second metacarpal proximal diaphysis. The Mini-TightRope is advanced with the passer guidewire and a button is placed at the volar-radial thumb metacarpal base. A second button is placed at the ulnar cortex of the second metacarpal diaphysis. Tightening the fiber wire with correct tension is performed under fluoroscopy control to check the radial abduction and volar abduction of the thumb metacarpal. After closing the wound, a thumb spica cast is applied.
Postoperative Rehabilitation
Ten days after the operation, sutures and the cast are removed, and ROM exercise is started by a hand therapist. Ten days are based on the wound healing period. Active ROM exercise of the finger joints, isometric exercises of the thenar eminence, and light activity of daily living (ADL) movement exercises are performed as pain permits. The therapist holds the metacarpal bones of the thumb so that the compensatory movement in the thumb metacarpophalangeal joint hyperextension is minimized and guides the movement from the CMC joint in a protective exercise. The ADL movement practice was used only for light work such as eating and writing that does not cause any overload. Four weeks after the operation, hand muscle strength exercises such as sponge and peg pinching and ball gripping are started. Ten weeks after the operation, ADL movement using the thumb is permitted without any restrictions.
Measurements
Patients completed the pain visual analogue scale (VAS), ROM and strength measurements, and the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire before surgery and at the final follow-up more than 1 year after surgery. The examinations were retrospectively assessed before surgery and at the final follow-up by 1 of the authors (who did not perform the operations in these patients). The VAS for the affected wrist was marked on a 10-cm line with 21 markers at 5-mm intervals. The 0-mm point indicated that the patient felt no pain, and the 100-mm point indicated maximum unendurable pain. Radial abduction and palmar abduction were used for ROM measurements. Pinch strength was measured using a baseline pinch gauge (Hydraulic Pinch Gauge NC70141; North Coast Medical, California), and grip strength using a hydraulic hand dynamometer in position 2 (Hydraulic Hand Dynamometer NC70142; North Coast Medical). Both the results were indicated as percentages of contralateral healthy side. Complications and removal of the Mini-TightRope were also retrospectively collected from patient medical records.
Statistical Analysis
Except for the VAS score, paired t tests were used to compare the assessment results before surgery with those at the final examination. The Wilcoxon signed-ranked test was used to analyze the VAS results. Statistical significance was set at P < .05.
Results
One patient withdrew from the follow-up study before the 1-year follow-up. Thirty-two patients met the inclusion criteria: 10 (4 men and 6 women) with stage II CMC arthritis and 22 (10 men and 12 women) with stage III CMC arthritis. The demographic data are shown in Table 1.
Table 1.
Demographic Data of Patients.
| Demographic variables | Total cases, n (%) |
|---|---|
| Patients, n | 32 (100) |
| Sex of patients | |
| Male | 14 (44) |
| Female | 18 (56) |
| Eaton stage | |
| Stage II | 10 (31) |
| Stage III | 22 (69) |
| Operated side | |
| Left | 15 (47) |
| Right | 17 (53) |
| Dominant hand operated | |
| Yes | 17 (47) |
| No | 15 (53) |
| Age at operation, y | |
| Mean | 67.5 |
| Range | 47-84 |
| Reason for operation, n | |
| Decrease pain | 25 (78) |
| Improve function | 3 (9) |
| Improve power | 3 (9) |
| Improve activity of daily living | 1 (4) |
| Follow-up, m | |
| Mean | 30.5 |
| Range | 12-61 |
The mean VAS score was 70.5 ± 14.0 before surgery and 7.9 ± 9.1 at the final follow-up (Figure 1). The mean VAS score at the final follow-up was significantly lower than that before surgery (P < .0001). The mean radial abduction value was 45.4 ± 16.4° before surgery and 59.7 ± 16.9° at the final follow-up (Figure 2). The mean palmar abduction value was 54.3 ± 13.9° before surgery and 65.5 ± 14.2° at the final follow-up. Both radial abduction and palmar abduction showed significant improvements (P = .0021 and .0038, respectively). The mean percentages of grip strength before surgery and at the final follow-up were 72.2 ± 27.4% and 81.4 ± 22.0% (Figure 3). About grip strength, there was no significant difference between before surgery and at the final follow-up. The mean percentages of pinch strength were 57.2 ± 24.8% before surgery and 91.0 ± 39.6% at the final follow-up. There was a significant difference between the percentages before surgery and at the final follow-up (P = .0035). The mean DASH scores were 36.8 ± 14.8 before surgery and 11.7 ± 10.5 at the final follow-up (Figure 1). The mean DASH score at the final follow-up was significantly lower than that before surgery (P < .0001).
Figure 1.

Visual analogue scale (VAS) and Disabilities of the Arm, Shoulder, and Hand (DASH) score before surgery and at the final follow-up.
Note. The mean VAS and DASH scores at the final follow-up are significantly lower than those before surgery. The bucket indicates significant difference.
Figure 2.
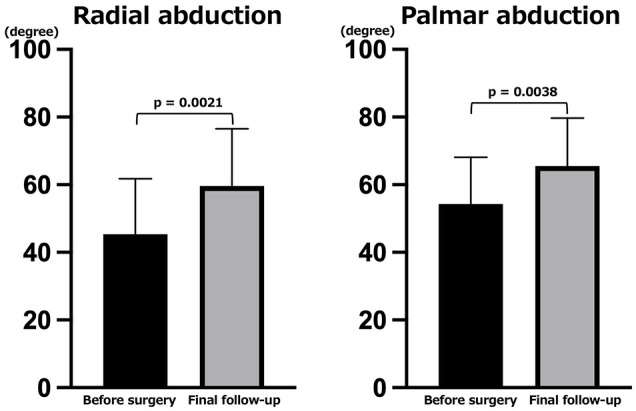
Range of motion before surgery and at the final follow-up. Both radial abduction and palmar abduction significantly increased. The bucket indicates significant difference.
Figure 3.

Grip strength and pinch strength before surgery and at the final follow-up.
Note. There was no significant difference in grip strength before surgery and at the final follow-up. The mean percentages of pinch strength at the final follow-up were significantly greater than those before surgery. The bucket indicates significant difference.
Two patients developed complications. One patient developed irritation of the superficial branch of the radial nerve, which was controlled with oral nonsteroidal anti-inflammatory drugs. Another patient developed dystonia and sought treatment from a neurologist. Two patients felt discomfort at the first web space and desired removal of the suture-button (Figure 4). Both these patients underwent surgery to remove the suture-button 11 months after the initial surgery. Except for these patients, no other patients required additional surgery.
Figure 4.
A case of suture-bottom removal.
Note. (a) Plain Radiograph films of a 48-year-old patient with stage II right thumb carpometacarpal (CMC) joint arthritis before surgery. (b) Computed tomography before surgery indicates joint narrowing and osteophytes. (c) Plain radiograph films immediately after arthroscopic partial trapeziectomy with suture-bottom suspension arthroplasty. (d) Plain radiograph films 11 months after surgery. The patient feels discomfort in the first web and elects to undergo suture-bottom removal. (e) Plain radiograph films 3 months after suture-bottom removal. The CMC joint height and first metacarpal alignment are preserved.
Discussion
Arthroscopic partial trapeziectomy is a minimally invasive technique, and it has been reported that patients can return to function earlier than with open surgical methods because the joint capsules and ligaments are preserved. 16 In this study, we used an arthroscopic technique to reduce pain, increase strength, and improve function. We found that, compared with preoperative status, the VAS score was significantly reduced, the pinch strength was significantly increased, and the DASH score was significantly improved at the final postoperative follow-up. In a systematic review and meta-analysis, the VAS score and DASH score were reported to improve an average of 40 mm and 22 points, respectively. 17 This study included no control group. As compared with this systematic review and meta-analysis, our results were consistent with these findings. It is of note, however, that grip strength did not improve. Grip force involves not only the thumb but also all 4 fingers and it is difficult to achieve improved thumb function.
The mean radial abduction and palmar abduction values were found to be significantly improved, which indicates that the ROM was significantly improved. In arthroscopic surgery, we usually remove the medial osteophyte and 3-mm joint surface of the trapezium. Using suture-button, the first metacarpal is suspended and medialized to correct the preoperative lateral subluxation. New space is created between the first metacarpal base and the trapezium because of bone removal and first metacarpal suspension. Because of the proximal new space, the motion of the first metacarpus improved, leading to ROM increase.
If suture-button is not employed, percutaneous Kirschner wire fixation is necessary for 3 to 6 weeks after arthroscopic partial trapeziectomy.18,19 Baker et al 9 reported that patients often find the Kirschner wire uncomfortable. Instead of uncomfortable percutaneous pinning, we use suture-button to maintain the newly created CMC space. Early active ROM rehabilitation can be started within 10 days after surgery in cases of suture-button. This may be 1 of the reasons for the improved ROM. It is possible that suture-button is effective in the first few postoperative months but after that it is not expected to be necessary. In this study, 2 patients desired the suture-buttons to be removed due to discomfort at the first web. We removed them 11 months after the first surgery in both cases. No subsidence of the CMC joint space after removal of the suture-buttons was observed. This phenomenon suggests that suture-button works effectively for a few months postoperatively.
This study has several limitations. First, we measured functional improvement using only the DASH score and did not use the Hand 20 or Michigan Hand Questionnaire scores. We used the DASH score because the Japanese Society for Surgery of the Hand version of the DASH score is available and many authors use the DASH score for hand function. Second, we measured the ROM with thumb radial and palmar abduction, which should be sufficiently accurate to measure the angle between the first and second metacarpus under fluoroscopy. Fluoroscopy involves radiation exposure, however, and it is important that patients realize ROM improvement. Given this, we use data collected using a goniometer in the outpatient clinic. Third, we started active ROM rehabilitation within 10 days after surgery because of arthroscopic methods and suture-button stabilization. However, other established surgical techniques can also start active ROM rehabilitation at the same time as our method. We should investigate the period to return to physical activity and compare it with other studies in future studies. Finally, the preoperative pain of CMC joints did not completely disappear after the operation and patients still have some pain. Postoperative pain is consistent with other reported outcomes. Carpometacarpal joint pain is not reflected in Radiograph images. The character of CMC joint pain should thus be elucidated in future studies.
Conclusion
Patients realized a significant increase in ROM and pain relief following suture-button suspensionplasty with arthroscopic partial trapeziectomy.
Footnotes
Ethical Approval: This study was approved by the institutional review board, the Ethics Committee of Kyoto University Graduate School and Faculty of Medicine. All patients signed written informed consent.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ryosuke Ikeguchi  https://orcid.org/0000-0003-4525-7849
https://orcid.org/0000-0003-4525-7849
References
- 1.Gangopadhyay S, McKenna H, Burke FD, et al. Five- to 18- year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am. 2012;37:411-417. [DOI] [PubMed] [Google Scholar]
- 2.Tomaino MM.Ligament reconstruction tendon interposition arthroplasty for basal joint arthritis. Rationale, current technique, and clinical outcome. Hand Clin. 2001;17:207-221. [PubMed] [Google Scholar]
- 3.Davis TR, Brady O, Dias JJ.Excision of the trapezium for osteo- arthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg Am. 2004;29:1069-1077. [DOI] [PubMed] [Google Scholar]
- 4.Gray KV, Meals RA.Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: minimum 6.5-year follow-up evaluation. J Hand Surg Am. 2007;32:23-29. [DOI] [PubMed] [Google Scholar]
- 5.Sandvall BK, Cameron TE, Netscher DT, et al. Basal joint osteoarthritis of the thumb: ligament reconstruction and tendon interposition versus hematoma distraction arthroplasty. J Hand Surg Am. 2010;35:1968-1975. [DOI] [PubMed] [Google Scholar]
- 6.Bufalini C, Perugia D.Distraction arthroplasty of the trapeziometacarpal joint. J Hand Surg Am. 2007;32:1443-1446. [DOI] [PubMed] [Google Scholar]
- 7.Leach RE, Bolton PE.Arthritis of the carpometacarpal joint of the thumb. Results of arthrodesis. J Bone Joint Surg Am. 1968;50:1171-1177. [PubMed] [Google Scholar]
- 8.Badia A, Sambandam SN.Total joint arthroplasty in the treatment of advanced stages of thumb carpometacarpal joint osteoarthritis. J Hand Surg Am. 2006;31:1605-1614. [DOI] [PubMed] [Google Scholar]
- 9.Baker RHJ, Al-Shukri J, Davis TRC. Evidence-based medicine: thumb basal joint arthritis. Plast Reconstr Surg. 2017;139:256e-266e. [DOI] [PubMed] [Google Scholar]
- 10.Özçelik İB, Uğurlar M, Sarı A. Arthroscopic hemitrapeziectomy and suture button suspensionplasty in the treatment of first carpometacarpal joint Eaton-littler stage 2-3 arthrosis. J Wrist Surg. 2019;8:132-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yao J, Cheah AE.Mean 5-Year follow-up for suture button suspensionplasty in the treatment of thumb carpometacarpal joint osteoarthritis. J Hand Surg Am. 2017;42:569.e1-569.e11. [DOI] [PubMed] [Google Scholar]
- 12.Parry JA, Kakar S.Dual mini TightRope suspensionplasty for thumb basilar joint arthritis: a case series. J Hand Surg Am. 2015;40:297-302. [DOI] [PubMed] [Google Scholar]
- 13.Yao J, Song Y.Suture-button suspensionplasty for thumb carpometacarpal arthritis: a minimum 2-year follow-up. J Hand Surg Am. 2013;38:1161-1165. [DOI] [PubMed] [Google Scholar]
- 14.Cox CA, Zlotolow DA, Yao J.Suture button suspensionplasty after arthroscopic hemitrapeziectomy for treatment of thumb carpometacarpal arthritis. Arthroscopy. 2010;26:1395-1403. [DOI] [PubMed] [Google Scholar]
- 15.Walsh EF, Akelman E, Fleming BC, et al. Thumb carpometacarpal arthroscopy: a topographic, anatomic study of the thenar portal. J Hand Surg Am. 2005;30:373-379. [DOI] [PubMed] [Google Scholar]
- 16.Abzug JM, Osterman AL.Arthroscopic hemiresection for stage II-III trapeziometacarpal osteoarthritis. Hand Clin. 2011;27:347-354. [DOI] [PubMed] [Google Scholar]
- 17.Wilkens SC, Bargon CA, Mohamadi A, et al. A systematic review and meta-analysis of arthroscopic assisted techniques for thumb carpometacarpal joint osteoarthritis. J Hand Surg Eur Vol. 2018;43:1098-1105. [DOI] [PubMed] [Google Scholar]
- 18.Hofmeister EP, Leak RS, Culp RW, et al. Arthroscopic hemitrapeziectomy for first carpometacarpal arthritis: results at 7-year follow-up. Hand. 2009;4:24-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chuang MY, Huang CH, Lu YC, et al. Arthroscopic partial trapeziectomy and tendon interposition for thumb carpometacarpal arthritis. J Orthop Surg Res. 2015;10:184. [DOI] [PMC free article] [PubMed] [Google Scholar]



