Abstract
Background:
This study aims to investigate whether compensation is equitable among the most commonly performed orthopedic hand surgeries and when compared with general orthopedic procedures.
Methods:
The National Surgical Quality Improvement Program database was queried for all orthopedic procedures, from 2016 to 2018, performed more than 150 times using Current Procedural Terminology (CPT) codes. Physician work relative value unit (wRVU) data were obtained from the 2020 US Centers for Medicare and Medicaid Services fee schedule. Linear regressions were used to determine whether there was an association among wRVU, operative time, and wRVU per hour (wRVU/h). Reimbursement for hand surgery CPT codes was compared with that of nonhand orthopedic CPT codes. The CPT codes were stratified into quartile cohorts based on mean operative time, major complication rate, mortality rate, American Society of Anesthesiologists class, reoperation rate, and readmission rate. Student t tests were used to compare wRVU/h between cohorts.
Results:
Forty-two hand CPT codes were identified from 214 orthopedic CPT codes, accounting for 32 333 hand procedures. The median wRVU/h was significantly lower for procedures in the longest operative time quartile compared with the shortest operative time quartile (P < .001). Compared with hand procedures, nonhand procedures were found to have significantly higher mean operative time (P < .001), mean complication rate (P < .001), mean wRVU (P = .001), and mean wRVU/h (P = .007).
Conclusions:
The 2020 Physician wRVU scale does not allocate proportional wRVUs to orthopedic hand procedures with longer mean operative times. There is a decrease in mean reimbursement rate for hand procedures with longer mean operative time. When compared with general orthopedic procedures, hand procedures have a lower mean wRVU/h and complication rate.
Keywords: RVU, reimbursement, hand surgery, NSQIP, physician compensation, physician productivity, orthopedic surgery
Introduction
The US health care system’s use of a fee-for-service model in assigning physician compensation is unique when compared with other industrial countries. The relative value unit (RVU) system was established by the US Centers for Medicare and Medicaid Services (CMS) to standardize the physician reimbursement process. 1 Each codified procedure is placed under the Common Procedural Terminology (CPT) system and assigned a certain number of work RVUs (wRVUs). The value of each CPT code is evaluated by a group of physicians who comprise the Relative Value Update Committee (RUC). The number of wRVUs assigned to each procedure is meant to reflect the time, intensity, and complexity in performing the procedure. 2
There has been an increased focus on understanding the trends in the wRVU scale. Many studies have found a discrepancy between the time it takes to perform a procedure and the rate of RVU per hour of operative time (wRVU/h). The Orthopedic literature has identified this discrepancy in revision arthroplasty, ankle fractures, and spine fusions.3-6 This pattern has also been identified in the literature of other fields; 1 study identified that urological procedures performed in less than 90 minutes earn 12.2 wRVU/h compared with 8.7 wRVU/h for longer procedures. 7 While in theory the wRVU for a procedure should be proportional to time, skill, stress, and effort, these measures are difficult to quantify in practice, which is reflected by a discrepancy in compensation for procedural services.8,9
As CMS determines the operative time to be a direct determinant of wRVU allocation, it can be used as an independent predictor of the number of wRVUs for a specified procedure. In addition, wRVU/h of operative time can be calculated for a given procedure and be used to compare rates of reimbursement for procedures with different operative lengths. If the wRVUs assigned to CPTs are theoretically proportional to operative time within the current CMS RVU scale, there should be a similar amount of wRVUs per unit time for shorter and longer procedures. To our knowledge, no study exists examining the global trends in reimbursement of orthopedic hand procedures. The goal of this study is to identify whether orthopedic hand procedures are reimbursed proportionally in terms of wRVU/h within the subspecialty of hand surgery and compared with all orthopedic procedures.
Methods
Database
The American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database was used to identify patients who underwent orthopedic hand procedures between 2016 and 2018. The NSQIP database is nationally validated and collects data from more than 700 participating hospitals in the United States and retrospectively collects 135 clinical variables. The variables collected were demographic characteristics, operative time, wRVU data, preoperative risk factors, American Society of Anesthesiologists (ASA) classification, surgical time, morbidity, and mortality data. The data are collected and verified by trained surgical reviewers, who ensure accuracy and quality. 10
Generation of Study Data Using CPT Codes
The NSQIP database was queried for all cases coded under the orthopedics subspecialty and reviewed by orthopedic residents. Cases missing wRVU, CPT, and operative time were excluded from the analysis. Procedures that were reimbursed less than 1 wRVU or those that had an operative time greater than 600 minutes or less than 10 minutes were excluded, as those cases do not represent a typical orthopedic procedure.
Procedures performed less than 150 times over the 3-year study period, as denoted by CPT codes, were excluded as these are uncommonly performed within the United States and would introduce a high variance in the operative time, leading to inaccurate calculation of mean operative time. Procedures that had more than 1 CPT code recorded were also excluded because secondary wRVUs are often not reimbursed at the full rate. Including these data would cause a skew in our statistical model toward higher RVU values, which would confound the analysis. Hand surgery CPTs were identified within the remaining CPT codes to verify that a procedure was within the scope of a fellowship-trained hand surgeon. Individual CPTs were assigned to hand surgery and nonhand surgery study groups by orthopedic surgery residents who individually reviewed each CPT.
Variables Studied and Statistical Analysis
The primary outcome variable assessed was wRVU/h, and wRVU/h was calculated by dividing wRVU from the 2020 CMS fee schedule by the mean operative time for CPT as obtained from the NSQIP database (measured in hours). Work RVUs were converted into estimated reimbursement rates using the CMS RVU dollar conversion factor of $36.0896 per RVU. The operative time is recorded in minutes and is defined as time from when the surgical incision is first made to wound closure. Secondary outcome variables for each CPT code studied were a 30-day major complication, reoperation, readmission, mortality rate, and ASA score. A major complication was defined as deep wound infection, deep organ infection, surgical site dehiscence, renal failure, pulmonary embolism or deep vein thrombosis, cerebrovascular accident, myocardial infarction, cardiac arrest, bleeding requiring transfusion, sepsis, postoperative ventilator dependence, unexpected reintubation, and death.
The CPT codes were stratified into quartile cohorts based on mean operative time in which the shortest 25% and the longest 25% mean operative time were compared. The CPT codes were then stratified into cohorts comprising the lowest and highest 25% in terms of major complication rate, mortality rate, ASA class, reoperation rate, and readmission rate. Student t tests or Wilcoxon tests were used to compare wRVU/h between cohorts based on mean operative time, complication rate, ASA class, reoperation, and readmission rates. P values <.05 were considered to be statistically significant. Univariate linear regression was used to model the association among wRVU, wRVU/h, operative time, and complication rate for both hand and nonhand study groups. Multivariate regression was performed to model the relationship between operative time and complication rate regarding their effect on wRVU and wRVU/h. Analysis of covariance was used to compare reimbursement rates between hand and nonhand cases, adjusting for complication rate.
Results
A total of 42 hand CPT codes identified from 172 orthopedic CPT codes met the inclusion criteria for this study, accounting for a total of 32 333 hand procedures. The mean wRVU was 7.99, operative time was 63.8 minutes, wRVU/h was 7.86, and the major complication rate was 2.2%.
When comparing CPTs stratified into longest and shortest quartile with regard to mean operative time (Table 1), the median wRVU/h was significantly lower for longer procedures (6.35 ± 0.94 vs 9.67 ± 2.72, P = .001). There was no significant difference in the complication rate of procedures in the bottom quartile versus the top quartiles in regard to the complication rate (8.10 ± 2.63 vs 7.82 ± 2.10, P = .797), mortality rate (7.61 ± 2.18 vs 8.23 ± 1.89, P = .274), ASA score (6.94 ± 1.59 vs 8.34 ± 2.30, P = .193), reoperation rate (7.91 ± 2.61 vs 7.73 ± 2.34, P = .797), or readmission rate (7.69 ± 2.76 vs 7.76 ± 2.06, P = .797).
Table 1.
Univariate Analysis of wRVU/h by Quartile for Hand Surgery Procedures.
| Study variable | No. of CPTs | Mean wRVU/h | P value |
|---|---|---|---|
| Operative time | |||
| Less than 40 | 11 | 9.67 ± 2.72 | .001 |
| 79 or more | 11 | 6.35 ± 0.94 | |
| Major complication rate, % | |||
| Less than 0.7 | 11 | 8.10 ± 2.63 | .797 |
| 1.8 or more | 11 | 7.82 ± 2.10 | |
| Mortality rate, % | |||
| 0 | 30 | 7.61 ± 2.18 | .274 |
| 0.06 or more | 11 | 8.23 ± 1.89 | |
| ASA class (score) | |||
| Less than 1.79 | 11 | 6.94 ± 1.59 | .193 |
| 2.15 or more | 11 | 8.34 ± 2.30 | |
| Reoperation rate, % | |||
| Less than 0.55 | 11 | 7.91 ± 2.61 | .797 |
| 1.35 or more | 11 | 7.73 ± 2.34 | |
| Readmission rate, % | |||
| Less than 0.56 | 11 | 7.69 ± 2.76 | .797 |
| 1.56 or greater | 11 | 7.76 ± 2.06 | |
Note. wRVU/h = work relative value unit per hour; CPT = Current Procedural Terminology; ASA = American Society of Anesthesiologists.
A total of 42 hand CPT codes were compared with 130 nonhand CPT codes (Table 2). Nonhand procedures were found to have significantly higher mean operative time (90.6 ± 39.8 vs 63.8 ± 24.7 minutes, P < .001), mean complication rate (10.51 ± 12.30 vs 2.15 ± 2.72%, P < .001), mean wRVU (13.94 ± 5.86 vs 7.98 ± 2.87, P < .001), and mean wRVU/h (9.75 ± 3.07 vs 7.86 ± 2.15, P < .001). After adjusting for the effect of complication rate, mean wRVU (P < .001) and mean wRVU/h (P = .007) remained significantly different between hand and nonhand cohorts.
Table 2.
Comparison of Hand and Nonhand Procedures.
| Hand procedures | Nonhand procedures | P value | Adjusted P value a | |
|---|---|---|---|---|
| No. of CPTs | 42 | 130 | ||
| Mean Operative Time (min) | 63.8 ± 24.7 | 90.6 ± 39.8 | <.001 | |
| Mean Complication Rate (%) | 2.15 ± 2.72 | 10.51 ± 12.30 | <.001 | |
| Mean wRVU | 7.98 ± 2.87 | 13.94 ± 5.86 | <.001 | <.001 |
| Mean wRVU/hour | 7.86 ± 2.15 | 9.75 ± 3.07 | <.001 | .007 |
Note. CPT = Current Procedural Terminology; wRVU = work relative value unit.
Adjusted P values determined using analysis of covariance to account for the effect of complication rate.
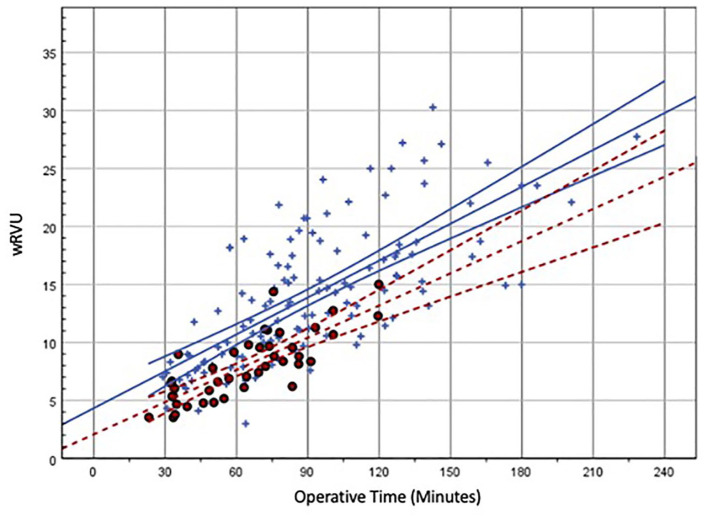
There was a negative correlation between wRVU/h and mean operative time. We identified that there was a decrease in -0.0384 wRVU/h for every additional minute of mean operative time (95 confidence interval: −0.063 to −0.014, R2 = 0.196, P = .003). This correlates with an hourly decrease in reimbursement of 2.31 wRVU/h or $83.19/h based on the 2020 Medicare conversion factor of $36.0896. This negative relationship is maintained even after adjusting for the mean complication rate for each CPT in the cohort (Figure 1).
Figure 1.
Scatter plot with linear regression of wRVU/h and operative time.
Note. Each red data point represents an individual Current Procedural Terminology code. Unadjusted linear regression depicting wRVU/h and operative time (solid black line) is y = 10.315 − 0.0384x, x-variable 95% confidence interval (CI): −0.063 to 0.014, P = .003, R2 = 0.196. The 95% CI is visually represented by dotted black lines. This correlates with an hourly decrease in reimbursement of 2.31 wRVU/h or $83.19/h. Multivariate regression of wRVU/h, operative time, and complication rate maintains this relationship: x-variable = −0.037 (95% CI: −0.063 to −0.010), P = .008, and R2 = 0.159. wRVU = work relative value unit.
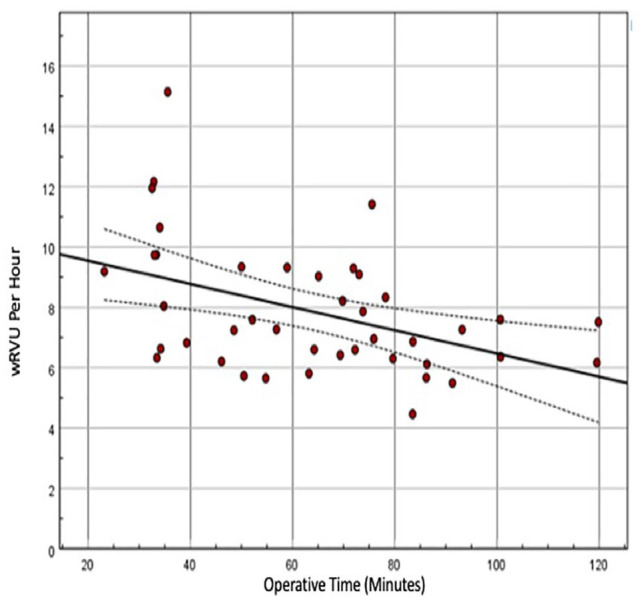
Univariate regression of wRVU and mean operative time for both hand and nonhand cohorts found a positive correlation between wRVU and mean operative time for CPT codes of both cohorts (Figure 2). Unadjusted linear regression for the hand surgery cohort found that each additional minute of mean operative time correlated with an allocation of an additional 0.093 wRVUs (P < .001, R2 = 0.627). For the nonhand surgery cohort, each additional minute of mean operative time correlated with an allocation of an additional 0.106 wRVUs (P < .001, R2 = 0.516). Multivariate regression was used to characterize the relationship among wRVU, operative time, and complication rate between hand and nonhand cohorts to reveal that even after adjusting for differing complication rates, not only was the allocation of wRVU per operative time unequal between groups (0.093 vs 0.106 wRVU/h, P < .001), but nonhand CPTs are reimbursed a higher baseline wRVU amount than hand CPTs (4.331 vs 2.073 wRVUs, Figure 2).
Figure 2.
Scatter plot with linear regressions of wRVU and operative time.
Note. Red circles represent hand Current Procedural Terminology (CPT) codes, and blue crosses represent nonhand CPT codes. Unadjusted linear regression of hand cases depicting wRVU and operative time (red dotted line) is y = 2.073 + 0.093x, P < .001, R2 = 0.627. The 95% confidence interval is visually represented by dotted red lines. Unadjusted linear regression of nonhand cases depicting wRVU and operative time (blue solid line) is y = 4.331 + 0.106x, P < .001, R2 = 0.516. The 95% confidence interval is visually represented by solid blue lines. Multivariate regression of wRVU, operative time, complication rate, and hand versus nonhand CPTs was performed to show that the complication rate does not fully account for different reimbursement rates (P < .001). wRVU = work relative value unit.
Discussion
The purpose of the CMS wRVU fee schedule is to provide physicians with an accurate compensation model that is proportional to the time, skill, and effort that is evoked to provide a service. The CMS further divides RVUs into work RVUs, malpractice RVUs, and practice expense RVUs. The RVU allocation for each CPT code is updated based on the recommendations of the RUC, a voluntary group of 31 physicians who represent the different subspecialties and primary care. Generally, when there is an increase in allocation toward a particular CPT, it often means that another CPT would proportionally decrease. The CMS fee schedule initially sought to fairly distribute Medicare dollars, but many health care organizations and private practices have also adopted the wRVU as a means to measure physician productivity and to determine reimbursement. 11 For this reason, the wRVU has become universally applicable to most orthopedists. This is the first study that examines a large cohort analysis of orthopedic hand cases in terms of operative time, complication rate, and wRVU.
In our analysis of hand surgery CPT codes and mean operative time by quartile, we identified that procedures with the highest mean operative times were reimbursed significantly less than those with the lowest mean operative times. Univariate linear regression showed that longer procedures are reimbursed at a lower hourly rate, with reimbursement decreasing at a rate of 2.31 wRVUs or $83.19 for each additional hour of mean operative time for a given procedure. This trend was maintained after adjusting for the complication rate associated with each CPT code. Theoretically, if the RUC is appropriately accounting for operative time in the allocation of wRVUs, the hourly reimbursement rate should be similar for procedures regardless of the mean operative time. Based on our analysis, it would appear that the 2020 CMS fee schedule favors shorter hand surgery procedures at the expense of longer hand surgery procedures.
There was no significant difference in reimbursement rate regarding major complication rate, mortality rate, ASA class, reoperation rate, and readmission rate between the top and bottom quartiles of CPT codes. This is an unexpected finding because the allotment of wRVUs should also consider procedures with higher complication rates. However, this supports the findings of Sathiyakumar et al 12 who found that the reimbursement rates in orthopedic trauma have not accurately accounted for the complication rate associated with a given CPT. Ramirez et al 13 identified a similar finding across all surgical subspecialties, where patient complexity did not correlate with the number of wRVUs assigned. The combination of these factors could theoretically incentivize surgeons to select for shorter cases and less-complex patients as a means to maximize productivity within physician practices that use RVU-based compensation models.
When comparing reimbursement rates between hand and nonhand CPT codes, there were some notable differences. Univariate linear regression for hand and nonhand CPT codes revealed that there are differences in the rate of reimbursement between case types; the nonhand cases are reimbursed at a significantly higher starting wRVU (Figure 2). For the CPTs included in the study, it is evident that the general orthopedic procedures are reimbursed on average 2 wRVUs more than hand procedures at any operative time point, and the rate at which general orthopedic procedures accrue RVUs is higher than that of hand procedures. The mean reimbursements for hand procedures are best modeled by the formula y = 2.073 + 0.093x, where “x” and “y” represent mean operative time (minutes) and wRVUs, respectively. In this model, 2.073 represents a base wRVU value, and 0.093 is the rate of wRVU allocation per minute of mean operative time. This is in contrast to the nonhand reimbursement formula of y = 4.331 + 0.106x. Using these regression models, one may calculate a mean difference in physician reimbursement between hand and nonhand procedures of 3.038 wRVUs or $109.64 (when using the Medicare wRVU-Dollar adjustment for 2020) for 1 hour of operative time. The difference in reimbursement rates can be explained in part by significantly higher complication rates for nonhand procedures compared with those of hand procedures, but in our multivariate model the complication rate did not fully account for this discrepancy. Procedures categorized as “hand” were found to be an independent predictor of lower hourly reimbursement.
Many of the findings in this study are reflected in the literature of other surgical subspecialties. Chakiryan et al 7 have shown that there is diminishing marginal reimbursement with increasing mean operative times for the 50 most frequently performed urology CPTs. Chakiryan et al also found that there were large discrepancies in reimbursement between urological subspecialties and that these discrepancies did not necessarily correlate with the mean complication rate. 7 Despite the fact that numerous other factors are included in the formulation of the CMS RVU fee schedule, operative time is listed as a direct determinant of wRVU allocation and should be an independent predictor of reimbursement. One simple explanation for these phenomena is that the estimates for operative times put forth by the RUC are inaccurate. Procedural data are derived from surveys gathered from cohorts of experienced surgeons who are theoretically familiar with the procedure. It has been suggested that RUC operative time data are frankly inaccurate, and operative times are overestimated specifically for practically shorter cases. 7 In fact, Chan et al 14 quantified a discrepancy of almost 200% for any given CPT code. Interestingly, the RUC estimates were neither systematically longer nor shorter than NSQIP times. These inconsistencies translate to a poor distribution in reimbursement and have the potential to impact the quality of care and supply of physician services. 15
There has been a steady decrease in reimbursement for orthopedic hand surgery cases. 16 This reimbursement includes the global surgical period which accounts for 3 to 4 postoperative visits over a 90-day period. 17 Hand cases, in particular pinning and tendon transfers/lengthening, often require more extensive postoperative rehabilitation that is not accurately captured in the wRVU scale due to the extensive aftercare that is required. 18 The $110 per hour difference in reimbursement between hand and nonhand procedures (sports, foot and ankle, etc.) may potentially affect patient care and incentivize higher compensating procedures. This phenomenon has previously been expressed by Nayar et al 19 when comparing operative times and wRVU for shoulder and elbow cases. With this valuation and hourly difference in reimbursement, certain procedures, including tendon surgeries (eg, extensor tendon repair) or ganglion excision, may constitute an overall loss of wRVU when accounting for operative time and postoperative care compared with more highly valued cases or simply seeing patients in the clinic. For minor hand procedures or procedures requiring extensive follow-up, elimination of the 90-day global period may help to offset the disparity in reimbursement between hand and nonhand procedures, similar to CPT 28825 (amputation of toe) that now carries a global period of zero while equivalent hand procedures do not.
This study has several limitations. There are many inputs other than operative time and complication rate in the determination of the number of wRVUs assigned to a given CPT, including many subjective factors that are difficult to quantify. Our analysis was limited by the variables provided in the NSQIP database. One variable that NSQIP fails to capture is the prior training of a surgeon and whether a procedure is performed by a general, plastics, or orthopedic trained hand surgeon. Furthermore, to prevent a skewed calculation of wRVU/h of operative time, multiple coded CPTs were removed. This may limit the generalizability of our study because hand surgical procedures can often involve multiple coded procedures. Another limitation is that the NSQIP database does not consider transverse carpal ligament or A1 pulley release to be a major surgery, and these procedures are not included in the data set. These procedures represent a significant portion of most hand surgeons’ volume, but for the purposes of our analysis they only represent 2 operations in the hand surgery cohort, and it is unlikely that their exclusion has impacted the significance of the results. 20 Finally, mean operative times were calculated from 2016 to 2018 NSQIP data, and the wRVU values were gathered from the 2020 CMS fee schedule. The use of different years’ data was done in an attempt to reflect the current reimbursement structure most accurately. Although updated surgical procedures may result in lower operative time for certain procedures, it is assumed that the operative time for most orthopedic procedures has not significantly changed in the past 5 years.
In conclusion, this is the first study in the orthopedic hand literature to examine trends within the subspecialty regarding wRVUs, operative time, and complication rate. We have shown, using real-world operative times and complication rates, that the 2020 physician wRVU scale does not allocate a sufficient number of wRVU for longer hand surgery procedures. This has the potential to incentivize hand surgeons to perform shorter procedures on a less medically complex patient population. Our results support the findings of prior literature, suggesting that the RUC is not using the most accurate data for the calculation of wRVU and is inadequately reimbursing longer procedures. Finally, the discrepancy in reimbursement between hand procedures and nonhand orthopedic procedures cannot be fully explained by the higher surgical complication rate for nonhand procedures. However, given the limited number of factors incorporated into our model, it is difficult to pinpoint the cause of this phenomenon or to account for other externalities that likely influence differences in wRVU allocation. Further research is warranted to elucidate these reimbursement discrepancies within the subspecialty of hand surgery and generally within orthopedics.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects and is exempt from institutional review board approval at our institution.
Statement of Informed Consent: Because this article does not contain any studies with human or animal subjects, it was not applicable to obtain informed consent for this study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Trevor Simcox  https://orcid.org/0000-0001-6435-5407
https://orcid.org/0000-0001-6435-5407
References
- 1.Childers CP, Dworsky JQ, Russell MM, et al. Association of work measures and specialty with assigned work relative value units among surgeons. JAMA Surg. 2019;154(10):915-921. doi: 10.1001/jamasurg.2019.2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsiao WC, Braun P, Yntema D, et al. Estimating physicians’ work for a resource-based relative-value scale. N Engl J Med. 1988;319(13):835-841. doi: 10.1056/NEJM198809293191305. [DOI] [PubMed] [Google Scholar]
- 3.Orr RD, Sodhi N, Dalton SE, et al. What provides a better value for your time? The use of relative value units to compare posterior segmental instrumentation of vertebral segments. Spine J. 2018;18(10):1727-1732. [DOI] [PubMed] [Google Scholar]
- 4.Sodhi N, Patel Y, Berger RJ, et al. Comparison of a posterior versus anterior approach for lumbar interbody fusion surgery based on relative value units. Surg Technol Int. 2019;35:363-368. [PubMed] [Google Scholar]
- 5.Peterson J, Sodhi N, Khlopas A, et al. A comparison of relative value units in primary versus revision total knee arthroplasty. J Arthroplasty. 2018;33:S39-S42. [DOI] [PubMed] [Google Scholar]
- 6.Samuel LT, Grits D, Acuna A, et al. Work relative value units do not adequately support the burden of infection management in revision knee arthroplasty. J Bone Joint Surg Am. 2020;102:230-236. [DOI] [PubMed] [Google Scholar]
- 7.Chakiryan NH, Jiang DD, Gillis KA, et al. Relative value units do not adequately account for operative time in urologic surgery. J Urol. 2020;203(5):1003-1007. [DOI] [PubMed] [Google Scholar]
- 8.Little DC, St Peter SD, Calkins CM, et al. Relative value units correlate with pediatric surgeons’ operating time: when perceived myth becomes reality. J Pediatr Surg. 2006;41(1):234-238; discussion 234. [DOI] [PubMed] [Google Scholar]
- 9.Jenkins KJ, Gauvreau K, Newburger JW, et al. Validation of relative value scale for congenital heart operations. Ann Thorac Surg. 1998;66(3):860-869. [DOI] [PubMed] [Google Scholar]
- 10.Ko CY, Hall BL, Hart AJ, et al. The American College of Surgeons National Surgical Quality Improvement Program: achieving better and safer surgery. Jt Comm J Qual Patient Saf. 2015;41(5):199-204. [DOI] [PubMed] [Google Scholar]
- 11.Hsiao WC, Braun P, Dunn D, et al. Resource-based relative values: an overview. JAMA. 1988;260(16):2347-2353. doi: 10.1001/jama.1988.03410160021004. [DOI] [PubMed] [Google Scholar]
- 12.Sathiyakumar V, Thakore RV, Molina CS, et al. Does physician reimbursement correlate to risk in orthopaedic trauma? J Surg Orthop Adv. 2017;26(1):48-53. [PubMed] [Google Scholar]
- 13.Ramirez JL, Gasper WJ, Seib CD, et al. Patient complexity by surgical specialty does not correlate with work relative value unit. Surgery. 2020;168(3):371-378. [DOI] [PubMed] [Google Scholar]
- 14.Chan DC, Huynh J, Studdert DM.Accuracy of valuations of surgical procedures in the medicare fee schedule. N Engl J Med. 2019;380(16):1546-1554. doi: 10.1056/NEJMsa1807379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McInerny TK, Cull WL, Yudkowsky BK.Physician reimbursement levels and adherence to American Academy of Pediatrics well-visit and immunization recommendations. Pediatrics. 2005;115(4):833-838. doi: 10.1542/peds.2004-1510. [DOI] [PubMed] [Google Scholar]
- 16.Eltorai AEM, Durand WM, Haglin JM, et al. Trends in Medicare reimbursement for orthopedic procedures: 2000 to 2016. Orthopedics. 2018;41(2):95-102. [DOI] [PubMed] [Google Scholar]
- 17.OWCP surgical services—global surgery. https://www.dol.gov/sites/dolgov/files/owcp/regs/compliance/GlobalSurgicalPolicy.pdf. Accessed June 16, 2021.
- 18.Nayar SK, Aziz KT, Zimmerman RM, et al. Misvaluation of hospital-based upper extremity surgery across payment, relative value units, and operative time. Iowa Orthop J. 2020;40(1):173-183. [PMC free article] [PubMed] [Google Scholar]
- 19.Nayar SK, Skolasky RL, LaPorte DM, et al. Reassessment of relative value in shoulder and elbow surgery: do payment and relative value units reflect reality? Clin Orthop Surg. 2021;13(1):76-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noland SS, Fischer LH, Lee GK, et al. Essential hand surgery procedures for mastery by graduating orthopedic surgery residents: a survey of program directors. J Hand Surg Am. 2013;38(4):760-765. doi: 10.1016/j.jhsa.2012.12.035. [DOI] [PubMed] [Google Scholar]