Abstract
Background
Moxibustion, a traditional Chinese medicine approach, stimulates blood circulation by burning wormwood at acupuncture points and is frequently used in conjunction with acupuncture for managing knee osteoarthritis. This review aims to compare the effectiveness of moxibustion and acupuncture in the management of knee osteoarthritis.
Methods
Our team conducted a comprehensive search across several databases: PubMed Central, EMBASE, MEDLINE, the Chinese Biomedical Literature Database (CBM), China National Knowledge Infrastructure (CNKI), and the Cochrane Library, covering the timeframe from January 1964 up until April 2022. We implemented a meta-analysis, utilizing a random-effects model, and we've presented the pooled standardized mean difference (SMD) and risk ratio (RR) inclusive of the 95% confidence intervals (CIs), in accordance with the nature of the outcome.
Results
21 studies were included, of which, half were identified as having high risk of bias. The pooled SMD for the pain score was found to be −0.53 (95% CI: −0.91 to −0.15). In-depth analysis focusing on the kind of moxibustion indicated that fire needle moxibustion was more effective in pain reduction (SMD = −0.56; 95% CI: −1.10 to −0.01) compared to alternative moxibustion methods (SMD = −0.47; 95% CI: −0.80 to −0.13). The pooled RR for the success rate in treatment was 1.39 (95% CI: 1.19 to 1.62). Subgroup analysis demonstrated that fire needle moxibustion reported a superior success rate (RR = 1.43; 95% CI: 1.19 to 1.72) in comparison to other types of moxibustion (RR = 1.33; 95% CI: 1.02 to 1.74).
Conclusion
Moxibustion, specifically fire needle moxibustion, demonstrated superior effectiveness in managing knee osteoarthritis compared to acupuncture.
Keywords: Acupuncture, Meta-analysis, Moxibustion, Osteoarthritis
Highlights
-
•
Moxibustion had better pain relief than acupuncture in osteoarthritis knee patients.
-
•
Moxibustion had better therapeutic effective rate than acupuncture.
-
•
Fire needle moxibustion performed better than other forms of moxibustion.
1. Introduction
Osteoarthritis manifests as a degenerative condition, marked by the deterioration of joint cartilage, calcification of the bone beneath the cartilage, also known as the subchondral bone, bone overgrowth, and changes in joint shape. This results from disruptions in the metabolism of joint cartilage and an increase in physical strain [1,2]. Most commonly affecting the knee joints, which bear significant weight, osteoarthritis triggers numerous complaints such as chronic pain, stiffness, limited range of motion, and joint instability, all of which can significantly impair function and diminish quality of life [[3], [4], [5]].
In China, knee osteoarthritis is primarily prevalent among the middle-aged and elderly populations, with an incidence of about 5–10% in these age groups [6]. Given the continuous aging of the population, the prevalence of knee osteoarthritis is projected to rise substantially in the coming years. Therefore, effective management of this condition is crucial to enhance the functional capacity and quality of life of the country's aging population. Current treatment strategies for knee osteoarthritis mainly encompass conservative measures such as physical activity, weight loss, heat wave therapy, prescription of non-steroidal anti-inflammatory drugs (NSAIDs), and intra-articular injections of hyaluronic acid. Surgical intervention may be considered for patients reporting chronic severe pain, joint instability, and significant movement limitation due to extensive degenerative changes [7].
Traditional Chinese medicine offers various treatment modalities for osteoarthritis, including acupuncture, moxibustion, and herbal medicines. Acupuncture and moxibustion, in particular, have demonstrated substantial effectiveness with minimal adverse reactions [8]. Moxibustion, a traditional Chinese medicine practice, promotes blood circulation by burning wormwood at acupuncture points and is commonly used alongside acupuncture to manage musculoskeletal disorders [9]. However, systematic evidence comparing the effectiveness of these two treatments in terms of recovery or pain reduction is lacking. By comparing the effectiveness of moxibustion and acupuncture in managing knee osteoarthritis, we aspire to guide healthcare providers in optimizing treatment strategies for their patients. Moreover, the results from this study would be instrumental in framing guidelines and policies pertaining to knee osteoarthritis management, particularly in settings where traditional Chinese medicine is practiced and integrated into routine healthcare. Hence, this study aims to compare the efficacy of moxibustion versus acupuncture in enhancing recovery and reducing pain among patients with knee osteoarthritis.
2. Materials and methods
We carried out this systematic review and meta-analysis in compliance with the guidelines laid down by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), as detailed in the Supplementary Appendix [10]. The structure of our review protocol and the formulation of our research query adhered to the PICOS framework, which defines the population, intervention, comparisons, outcomes, and study design.
2.1. Inclusion criteria
2.1.1. Study design
We included parallel-arm individual randomized or cluster randomized controlled trials in this study. Only full-text studies were considered, while case reports, series, conference abstracts, and unpublished grey literature were excluded.
2.1.2. Study participants
Participants in the studies consisted of adult (aged 18 years and above) osteoarthritis knee patients, irrespective of gender, or comorbid status.
2.1.3. Study interventions
Studies that directly compares the effectiveness of Moxibustion against Acupuncture were included.
2.1.4. Study outcomes
Clinical or therapeutic effective rate or recovery rate, reduction in the pain score were considered as outcomes for the review. Studies reporting any one of these outcomes were eligible for inclusion.
2.2. Exclusion criteria
We excluded review articles, editorials, commentaries, or case reports, as these do not present original research. We focused our review on adult individuals (18 years or older) with osteoarthritis knee, thus excluding studies on individuals below 18 years. Additionally, studies that did not use validated assessment tools for evaluating pain score were excluded.
2.3. Search strategy
An expansive, methodical, and all-encompassing literature review was conducted, involving searches across several databases, namely “PubMed Central, EMBASE, MEDLINE, Chinese biomedical literature database (CBM), China National Knowledge Infrastructure (CNKI), Cochrane library, Google Scholar, and ScienceDirect”. To ensure a comprehensive search strategy, we combined both medical subject headings (MeSH) and free-text terms. Appropriate Boolean operators (“AND”, “OR”, and “NOT”) were used in conjunction with our predetermined search terms. The search terms used were described in Supplementary Appendix. Further filtering was performed based on time period (January 1964 to April 2022), and language (English and Chinese). We also thoroughly inspected the reference sections of the retrieved articles to unearth any potentially missed studies.
2.4. Selection procedure
Two autonomous researchers (SX & JL) carried out the preliminary screening by scrutinizing the title, keywords, and abstract of each study. Full-text studies were procured for further screening in alignment with the eligibility criteria. Any disagreements during this stage were resolved through mutual consensus between the reviewers. In the next phase, full-text articles were inspected by two other researchers (ZY & CL), and those meeting the eligibility parameters were included in the review for subsequent analysis.
2.5. Procedure for data extraction
After identifying the appropriate full-text articles, both researchers manually extracted the required data using a preconceived semi-structured data collection form. This data included details like author names, study title, year of publication and study execution, study span, design, locale, the region of study, sample size, outcome assessment tool, mean age, details of intervention and comparator, as well as data on pain score and recovery rate. The primary author (SX) entered the data, after which it was cross-verified for accuracy by the second author (JL).
2.6. Assessment of bias risk
Lead and supporting researchers (SX and JL) used the Cochrane Risk of Bias Tool for Randomized Controlled Trials (RoB 2) to appraise the risk of bias across the studies incorporated into our analysis [11]. This instrument examines five distinct domains related to bias risk: the process of randomization, discrepancies from intended interventions, data omitted from the outcomes, outcome measurement, and the choice of reported results. Based on the scores acquired from these domains, each study was categorized as posing a “low,” “high,” or “some concerns” risk of bias in terms of the integrity of the evidence.
2.7. Statistical analysis
2.7.1. Estimation of pooled effect
The meta-analysis was conducted using the STATA software, version 14.2 (StataCorp, College Station, TX, USA). For binary outcomes (i.e., the rate of recovery), we used the count of events and the number of participants in each group to deduce the combined effect estimate in the form of risk ratio (RR). For the quantitative outcome (i.e., pain score), we collected the mean, standard deviation (SD), and the total sample size from both groups. The combined effect was articulated as the weighted mean difference (WMD) or the standardized mean difference (SMD) accompanied by a 95% confidence interval (CI). The weightage of individual studies was calculated using the inverse variance method in the context of the random effects model [12]. Both study-specific and combined estimates were visually presented via a forest plot. We scrutinized the variance between studies attributable to heterogeneity via a chi-square test and I2 statistics [12].
2.7.2. Additional analysis
We also carried out a sensitivity analysis to test the stability of the results by sequentially excluding studies and examining any significant shifts in the outcomes. We investigated the potential for publication bias using a funnel plot, substantiated statistically by the Egger's test (a p-value below 0.05 signifies statistically substantial publication bias) [13].
2.7.3. GRADE method
We utilized the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) methodology to assess the quality of evidence. This structure considers elements such as the risk of bias, inconsistency, indirectness, imprecision, and publication bias during the assessment of the quality of evidence [12]. The quality of evidence for each outcome was independently appraised by two reviewers, culminating in an overall GRADE rating.
3. Results
3.1. Study selection
The PRISMA flowchart in Fig. 1 illustrates the complete process of study selection. The primary screening yielded 124 full-text studies, reduced to 121 after removing duplicates. Along with three articles extracted from the bibliographies of the screened articles, these underwent a secondary screening. Eventually, 21 studies that fulfilled the inclusion criteria were incorporated into our review [[14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34]].
Fig. 1.
PRISMA flowchart.
3.2. Study characteristics
Our review exclusively included randomized controlled trials (RCTs), all of which were carried out in China. The number of participants in the acupuncture and moxibustion groups across these studies ranged from 28 to 120. Majority studies have used filiform needle in the acupuncture group while fire needle was used in the moxibustion group. Visual analog scale (VAS) was the most common measurement tool used for the assessment of pain (Table-1). In terms of quality assessment, half of the studies were identified as having a high risk of bias, while the remaining had some concerns, as per the RoB-2 checklist (Table 2).
Table 1.
Characteristics of the included studies (N = 21).
| Author and year | Country | Sample size Moxibustion arm | Sample size Acupuncture arm | Study design | Acupuncture arm | Moxibustion arm | Duration & Frequency of Interventions | Outcomes assessed | Pain assessment tool |
|---|---|---|---|---|---|---|---|---|---|
| Chen et al., 2020 | China | 28 | 28 | RCT | Neixiyan (EX-LE40), Dubi (ST35), Heding (EX-LE2), Liangqiu (ST34), Xuehai (SP10), Zusanli (ST36) and Ashi-point on the affected side of the body were punctured with filiform needles | Moxibustion applied to surrounding area of affected joint for 60 min | Once daily for 4 weeks | Therapeutic effect | NA |
| Chen et al., 2020 | China | 28 | 28 | RCT | Neixiyan (EX-LE40), Dubi (ST35), Heding (EX-LE2), Liangqiu (ST34), Xuehai (SP10), Zusanli (ST36) and Ashi-point on the affected side of the body for 30 mihns | Moxibustion at knee for 60 min | Once every 2 days for 4 weeks | Therapeutic effect | NA |
| Gao et al., 2012 | China | 35 | 34 | RCT | Acupoints for electric acupuncture | 2 moxacones (warm needling moxibustion) at each acupoint | Three times a week for 4 weeks | Therapeutic effect, pain | WOMAC |
| Huang et al., 2013 | China | 41 | 39 | RCT | Filiform needle acupuncture | Fire needle moxibustion for 30 min | Twice every week 24 times for 1 session | Therapeutic effect, pain | ISOA |
| Jianjun et al., 2018 | China | 30 | 28 | RCT | Twirling and tonifying method at acupoints | Acupuncture plus wheat grain moxibustion (performed 1 h after acupuncture | Once a day for 2 sessions | Therapeutic effect | NA |
| Jie et al., 2006 | China | 120 | 120 | RCT | Filiform needle acupuncture | Fire needle moxibustion | Once every 2 days 5 times for 2 sessions | Therapeutic effect | NA |
| Kuang et al., 2006 | China | 50 | 50 | RCT | Filiform needle acupuncture | Fire needle moxibustion | Twice every 2 days 10 times for 3 sessions | Therapeutic effect | NA |
| Li et al., 2011 | China | 32 | 30 | RCT | Filiform needle acupuncture | Fire needle moxibustion for 20 min | Twice every week, 16 times for 2 sessions | Therapeutic effect, pain | ISOA |
| Lu et al., 2013 | China | 27 | 27 | RCT | Filiform needle acupuncture | Fire needle moxibustion | Three times a week 12 times for 1 session | Pain | VAS |
| Lu et al., 2018 | China | 30 | 28 | RCT | Neixiyan (EX-LE40), Dubi (ST35), Heding (EX-LE2), Liangqiu (ST34), Xuehai (SP10), Zusanli (ST36) and Ashi-point on the affected side of the body were punctured with filiform needles | Acupuncture + Moxibustion with seed sized moxa cones | Once a day for 20 days | Therapeutic effect | NA |
| Su et al., 2012 | China | 35 | 35 | RCT | Filiform needle acupuncture | Fire needle moxibustion | Twice a week 4 times for 2 sessions | Therapeutic effect | NA |
| Tao et al., 2013 | China | 32 | 34 | RCT | Filiform needle acupuncture | Fire needle moxibustion for 30 min | Twice every 2 days 12 times for 1 session | Therapeutic effect, pain | WOMAC |
| Wang et al., 2015 | China | 39 | 39 | RCT | Filiform needle acupuncture | Fire needle moxibustion for 20 min s | Once daily 14 times for 1 session | Therapeutic effect | NA |
| Wu et al., 2014 | China | 31 | 30 | RCT | Filiform needle acupuncture | Fire needle moxibustion | Three times every week 10 times for 3 sessions | Therapeutic effect, pain | VAS |
| Zeng et al., 2008 | China | 73 | 56 | RCT | Filiform needle acupuncture | Fire needle moxibustion | Twice a week 4 times for 2 sessions | Therapeutic effect | NA |
| Zhang et al., 2010 | China | 32 | 30 | RCT | Xuehai (SP10) and Shenshu (BL23) | Acupuncture + non-scarring moxibustion | 2 sessions | Therapeutic effect, pain | VAS |
| Zhang et al., 2013 | China | 33 | 34 | RCT | Filiform needle acupuncture | Fire needle moxibustion for 30 min | Three times a week 12 times for 1 session | Therapeutic effect, pain | WOMAC |
| Zheng et al., 2017 | China | 30 | 30 | RCT | Liangqiu, Xuehai, Dubi, Neixeyan, Yanglingquan, Zusanli, Yinlingquan, Sanyinjiao, Xuanzhong and Taichong on the affected side | Ginger-partitioned moxibustion at the affected-side Heding point; | Once a day for 20 days | Therapeutic effect, pain | VAS |
| Zhou et al., 2014 | China | 39 | 44 | RCT | Electric acupuncture | Moxibustion | NR | Pain | VAS |
| Zhu et al., 2010 | China | 56 | 42 | RCT | Filiform needle acupuncture | Fire needle moxibustion for 30 min | Three times a week 6 times for 2 sessions | Therapeutic effect | NA |
| Zhu et al., 2013 | China | 33 | 30 | RCT | Filiform needle acupuncture | Fire needle moxibustion for 30 min | Twice every week 12 times for 1 session | Therapeutic effect | NA |
NR-Not reported; NA-Not appliable; RCT-Randomized controlled trial; VAS-Visual Analog Scale; WOMAC- Western Ontario and McMaster Universities Osteoarthritis Index; ISOA-Index of Severity of the Osteoarthritis.
Table 2.
Risk of bias assessment (N = 21).
| Author and year | Randomization process | Deviation from intended intervention | Missing data | Measurement of outcome | Selective reporting of results | Overall risk |
|---|---|---|---|---|---|---|
| Chen et al., 2020 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Chen et al., 2020 | Some concerns | Some concerns | Low risk | Low risk | Low risk | High risk |
| Gao et al., 2012 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Huang et al., 2013 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Jianjun et al., 2018 | Some concerns | Some concerns | Low risk | Low risk | Low risk | High risk |
| Jie et al., 2006 | Some concerns | Some concerns | Low risk | Low risk | Low risk | High risk |
| Kuang et al., 2006 | Low risk | Some concerns | Low risk | High risk | Low risk | High risk |
| Li et al., 2011 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Lu et al., 2013 | Low risk | Some concerns | Low risk | High risk | Low risk | High risk |
| Lu et al., 2018 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Su et al., 2012 | Low risk | Low risk | Low risk | High risk | Low risk | High risk |
| Tao et al., 2013 | Low risk | Low risk | Low risk | Low risk | Some concerns | Some concerns |
| Wang et al., 2015 | Low risk | Some concerns | Low risk | High risk | Low risk | High risk |
| Wu et al., 2014 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Zeng et al., 2008 | Low risk | Some concerns | Low risk | High risk | Low risk | High risk |
| Zhang et al., 2010 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Zhang et al., 2013 | Low risk | Low risk | Low risk | High risk | Low risk | High risk |
| Zheng et al., 2017 | Low risk | Low risk | Low risk | Low risk | Some concerns | Some concerns |
| Zhou et al., 2014 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Zhu et al., 2010 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Zhu et al., 2013 | Low risk | Some concerns | Low risk | High risk | Low risk | High risk |
3.3. Comparison of acupuncture and moxibustion for the management of osteoarthritis knee
3.3.1. Pain score
10 studies have reported on the difference in pain score between moxibustion and acupuncture groups. The pooled SMD was −0.53 (95% CI: −0.91 to −0.15; I2 = 82.6%), indicating that the patients undergoing moxibustion treatment had significant reduction in the pain score when compared to patients undergoing acupuncture treatment (Fig. 2). A subgroup assessment according to the moxibustion type revealed superior pain alleviation with fire needle moxibustion (pooled SMD = −0.56; 95% CI: −1.10 to −0.01) compared to other moxibustion techniques (pooled SMD = −0.47; 95% CI: −0.80 to −0.13).
Fig. 2.
Forest plot showing the difference in pain scores between moxibustion and acupuncture for osteoarthritis knee.
However, use of SMD disregards the metric and makes it difficult to determine the magnitude of improvement in pain score. Hence, additional analysis based on the results of the different scales were evaluated and interpreted based on the respective minimum clinically important differences. Analysis based on pain scale revealed that studies reporting pain score using WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) did not reveal a significant difference between moxibustion and acupuncture (pooled WMD = −0.10; 95% CI: −2.08 to 1.87). However, the studies reporting pain score using VAS (pooled WMD = −0.60; 95% CI: −0.73 to −0.48) and ISOA (Index of Severity of the Osteoarthritis) (pooled WMD = −0.93; 95% CI: −1.43 to −0.42) has revealed a significantly better pain relief in patients undergoing moxibustion compared to acupuncture (Fig. 3).
Fig. 3.
Subgroup analysis showing the difference in pain scores based on the type of pain measurement scale between moxibustion and acupuncture for osteoarthritis knee.
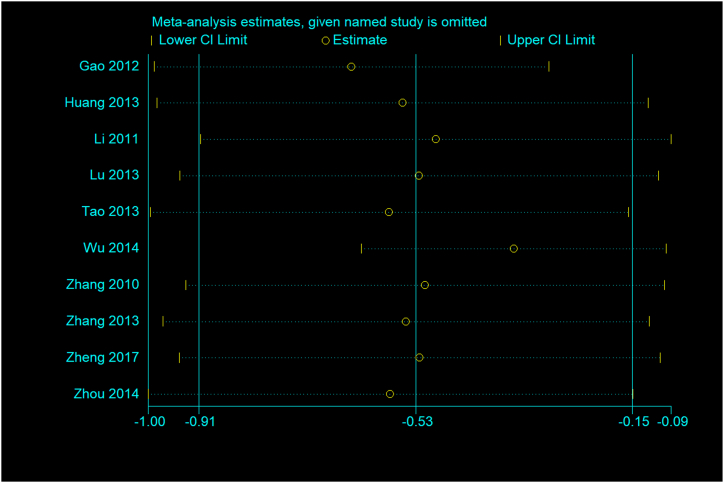
Significant publication bias was identified through an asymmetrical funnel plot (Fig. 4) and a statistically significant Egger's test (p = 0.009). The sensitivity analysis did not identify any individual study that substantially influenced the outcome direction or the estimate magnitude (Fig. 5). The analysis considering the evidence quality did not reveal a significant difference in the effect size between high- and low-quality studies.
Fig. 4.
Funnel plot for pain outcome.
Fig. 5.
Sensitivity analysis for pain outcome.
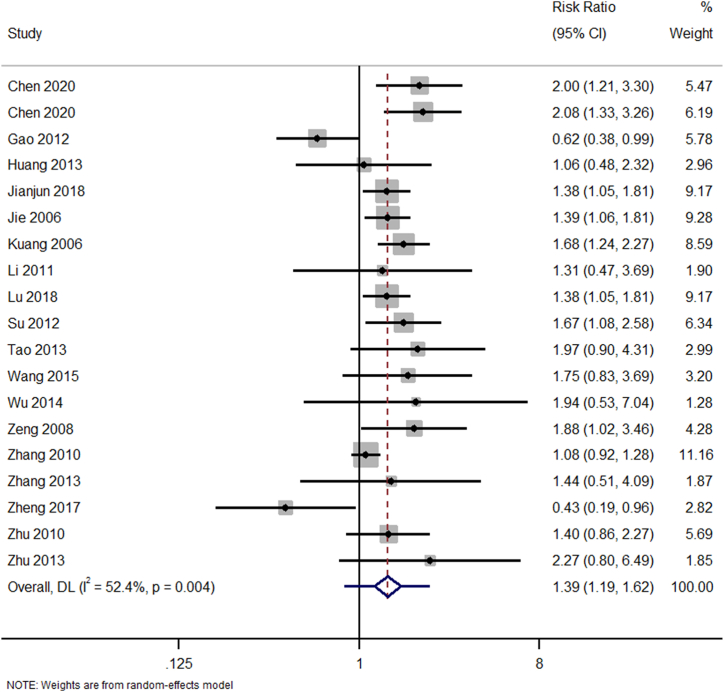
3.3.2. Therapeutic effective rate
19 studies have reported on the difference in therapeutic effective rate between moxibustion and acupuncture groups. The pooled RR was 1.39 (95% CI: 1.19 to 1.62; I2 = 52.4%), indicating that the patients undergoing moxibustion treatment has 1.39 times higher therapeutic effectiveness when compared to patients undergoing acupuncture treatment and this difference was statistically significant (p < 0.001) (Fig. 6). Subgroup analysis, based on moxibustion type, demonstrated a superior therapeutic effective rate for fire needle moxibustion (pooled RR = 1.43; 95% CI: 1.19 to 1.72) when juxtaposed with studies employing other moxibustion forms (pooled RR = 1.33; 95% CI: 1.02 to 1.74).
Fig. 6.
Forest plot showing the difference in therapeutic effective rate between moxibustion and acupuncture for osteoarthritis knee.
No publication bias was detected as determined by a symmetrical funnel plot (Fig. 7) and a non-significant Egger's test (p = 0.38). Sensitivity analysis did not indicate a single study effect on the effect size concerning the outcome's direction or the estimate's magnitude (Fig. 8). Also, the analysis based on the quality of evidence did not reveal any notable difference in effect size between high and low-quality studies.
Fig. 7.
Funnel plot for therapeutic effective rate.
Fig. 8.
Sensitivity analysis for therapeutic effective rate.
The application of the GRADE approach revealed very low-quality evidence for both the outcomes, despite including only RCTs. This reduction was due to a large number of studies exhibiting a high risk of bias and inconsistencies, as evidenced by measures of statistical heterogeneity.
4. Discussion
Acupuncture and moxibustion are two of the most common forms of traditional medicine used widely in China [[35], [36], [37]]. They have numerous applications, and their use in treating knee osteoarthritis has been extensively studied, with an ever-growing body of evidence, ranging from case reports to longitudinal studies or RCTs. However, there have been no systematic reviews specifically comparing the effectiveness of these two interventions to determine the best form of treatment for knee osteoarthritis. This review aims to address this gap and identify the comparative effectiveness of moxibustion and acupuncture for the management of knee osteoarthritis.
Our review found that moxibustion has significantly more effect than acupuncture in managing knee osteoarthritis, both in terms of pain relief and clinical or therapeutic effective rate. While no previous reviews directly compare these findings, there are several overviews, network meta-analyses, and pairwise meta-analyses that either compare these two interventions or assess the effectiveness of each compared to a control arm. Our findings align with these previous pieces of evidence, which also report a higher level of effectiveness for moxibustion in both the magnitude and direction of the association [[38], [39], [40], [41]].
Moxibustion therapy works by reducing cartilage damage and the infiltration of macrophages, thereby improving blood circulation at the knee joint. It also inhibits the expression of inflammatory mediators such as the tumor necrosis factor, interleukin-6, and mast cell cyclooxygenase, thereby facilitating the repair of articular chondrocytes [[42], [43], [44], [45]]. There's also evidence to suggest that moxibustion can increase limb pedal strength of the knee joint by regulating insulin-like growth factor and transformed growth factor [46]. These mechanisms, either alone or in combination, might be responsible for the effective management of knee osteoarthritis in patients. However, it should be noted that several forms of moxibustion have been tried and tested across the studies included.
The data from WOMAC, VAS, and ISOA pain scales indicate that the choice of assessment tool could influence the perceived effectiveness of moxibustion versus acupuncture. Despite both methods belonging to traditional Chinese medicine, their efficacy, as measured by different scales, varied. While WOMAC did not reveal a significant difference, both VAS and ISOA demonstrated better pain relief with moxibustion. It is essential to further explore the reasons behind these discrepancies. One potential explanation for these discrepancies might be the difference in sensitivity and specificity between the pain scales used. Another factor to consider is that the pain scales used could be capturing different aspects of osteoarthritis knee pain. For example, the WOMAC scale focuses more on physical function, whereas the VAS and ISOA scales provide a broader assessment of pain.
Although the studies included in our review featured various forms of moxibustion, we found the greatest effectiveness in studies that reported the use of fire needle moxibustion. A possible explanation for this finding is that the fire needle was used to concentrate energy on a specific part of the body in the studies reported. High-energy stimuli during fire needle moxibustion could sufficiently expand the blood vessels, thus improving blood supply, metabolism, and circulation, especially within the narrow range around the fire needle body [47]. Lesions present were burnt to carbonization, expediting the relief of local tissue edema, exudation, hyperemia, adhesions, contracture, and calcification, which in turn promoted the absorption of inflammatory exudate.
Another proposed mechanism for the effectiveness of the fire needle in knee osteoarthritis involved the regulation of IL-1 signal transduction pathways, specifically IL-1Rα, IL-1β level, and the IL-1Rα/IL-1β ratio [48]. This adjustment may balance the decomposition and regeneration of the articular cartilage. Prior research indicates that administering active acupuncture treatments through different experimental heat pain stimulation methods can efficiently convey the expectation of pain reduction when managing chronic knee osteoarthritis pain [49,50]. This could potentially elucidate the impact of fire needle moxibustion. This process, a novel hypothesis rooted in placebo analgesia, connects the enhancement of expectations with the pain regulation system [49,50]. Despite these findings, current research exploring this form of intervention for knee osteoarthritis is limited and requires further examination through large-scale RCTs.
Furthermore, the GRADE approach's outcome, which revealed very low-quality evidence, underscores the necessity for more rigorous and standardized studies in this area. Despite including only RCTs, which are considered the gold standard for evaluating the effectiveness of interventions, the high risk of bias and inconsistency among the studies could not be ignored. These findings should inform future research directions, including the design of RCTs with robust methods to minimize bias and ensure consistent methodologies across studies.
The strengths of this meta-analysis is that it amalgamates a significant number of studies, each with substantial sample sizes (21 studies with over 1000 participants). Our study contributes to the scant evidence on the comparative effectiveness of moxibustion and acupuncture. Sensitivity analysis showed the robustness of results, and there was no discernible difference in terms of study quality, which bolsters the credibility of our findings. However, our review does come with limitations. Most studies were of lower quality across various domains under RoB-2, and we detected significant publication bias for the outcome of pain relief, which may affect the interpretation of results. We also found significant inter-study heterogeneity for both outcomes, further limiting our ability to make conclusions based on pooled results.
Nonetheless, the results from this meta-analysis carry significant clinical implications for managing osteoarthritis of the knee. They provide evidence that moxibustion treatment can be used as an effective mode of treatment. However, while this systematic review and meta-analysis demonstrate potential benefits of moxibustion, particularly when evaluated using the VAS and ISOA scales, the GRADE approach's outcomes underscore the necessity for cautious interpretation of these results. They suggest that additional high-quality, large-scale RCTs are needed to corroborate these findings and offer more reliable evidence for the use of moxibustion and acupuncture in managing osteoarthritis knee pain. Furthermore, among the various forms of moxibustion available, the fire needle form may be the most beneficial for effectively managing knee osteoarthritis patients. Future reviews should compare the therapeutic effectiveness of various newer forms of traditional Chinese medicine and identify the best intervention to develop optimal treatment strategies.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
This research is supported by Science and Technology Program of Hebei (No. H2022406057) Scientific Research Project of Beijing Electric Power Hospital (No. Y2021002) University-level scientific research project in CDMU (No. 202119).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e17805.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Korean Acupuncture & Moxibustion Society . Jibmoondang; Seoul (Korea): 2012. The Acupuncutre and Moxibustion Medicine. pp. 559–564, 573-577. [Google Scholar]
- 2.Issa S.N., Sharma L. Epidemiology of osteoarthritis: an update. Curr. Rheumatol. Rep. 2006;8(1):7–15. doi: 10.1007/s11926-006-0019-1. [DOI] [PubMed] [Google Scholar]
- 3.Ettinger W.H., Afable R.F. Physical disability from knee osteoarthritis: the role of exercise as on intervention. Med. Sci. Sports Exerc. 1994;26:1435–1440. [PubMed] [Google Scholar]
- 4.Hsu H., Siwiec R.M. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL: 2022. Knee osteoarthritis. 2021 Jul 25. PMID: 29939661. [Google Scholar]
- 5.Kawahara T., Sasho T., Ohnishi T., et al. Stage-specific meniscal features predict progression of osteoarthritis of the knee: a retrospective cohort study using data from the osteoarthritis initiative. BMC Muscoskel. Disord. 2019;20:1. doi: 10.1186/s12891-019-2413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang X., Wang S., Zhan S., et al. The prevalence of symptomatic knee osteoarthritis in China: results from the China health and retirement longitudinal study. Arthritis Rheumatol. 2016;68(3):648–653. doi: 10.1002/art.39465. [DOI] [PubMed] [Google Scholar]
- 7.Yu S.P., Hunter D.J. Managing osteoarthritis. Aust. Prescr. 2015;38(4):115–119. doi: 10.18773/austprescr.2015.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang M., Jiang L., Wang Q., Chen H., Xu G. Traditional Chinese medicine for knee osteoarthritis: an overview of systematic review. PLoS One. 2017;12(12) doi: 10.1371/journal.pone.0189884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deng H., Shen X. The mechanism of moxibustion: ancient theory and modern research. Evid. Based Complement. Alternat. Med. 2013;2013 doi: 10.1155/2013/379291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Moher D. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021;134:103–112. doi: 10.1016/j.jclinepi.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Sterne J.A., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.Y., Corbett M.S., Eldridge S.M., Emberson J.R. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019:366. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 12.Higgins J.P., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2011. [Google Scholar]
- 13.Egger M., Davey Smith G., Schneider M., et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang K.D. Treatment of 41 cases of knee osteoarthritis with therapy of fire-needle and cupping. Chin. J. Geriatr. Care. 2013;11:11–12. [Google Scholar]
- 15.Su M. Clinical effect of blood-letting puncture combined with red-hot needle therapy on knee osteoarthritis. Chin. Med. Guide. 2012;34:611–612. [Google Scholar]
- 16.Zhou Y.L., Li J., Hou W.G., Bao C.L., Zhang Q., Wang S.S., et al. Clinical observation of moxibustion in treatment of knee osteoarthritis. Shanghai J. Acupunct. 2014;33:1086–1088. [Google Scholar]
- 17.Zeng H.-W., Nie B., Shi L.-L. Observation on therapeutic effect of blood-letting puncture combined with red-hot needle therapy on knee osteoarthritis. Zhongguo Zhen Jiu. 2008;28(7):493–495. [PubMed] [Google Scholar]
- 18.Chen Y., Wang R.Q., Liu J.X., Zhang Z.D., Jia Y.J., Lv J.H., Shi J., Xu J., Jia C.S. [Effect of moxibustion on inflammatory factors and oxidative stress factors in patients with knee osteoarthritis: a randomized controlled trial] Zhongguo Zhen Jiu. 2020;40(9):913–917. doi: 10.13703/j.0255-2930.20200310-k0011. [DOI] [PubMed] [Google Scholar]
- 19.Jie P.X., Peng Y.Y., Jing H.T. Treatment of 120 cases of knee osteoarthritis with fire needle therapy. J. Hebei TCM Pharmacol. 2006;21:25–26. [Google Scholar]
- 20.Zhang Q.R., Fu W.B. Osteoarthritis of knee joint treated with acupuncture and moxibustion. Zhongguo Zhen Jiu. 2010;30:375–378. (in Chinese) [PubMed] [Google Scholar]
- 21.Li B., Xie X.C., Wang P.L. Clinical observation of treatment on knee osteoarthritis with fire-needle moxibustion. Beijing J. Tradit. Chin. Med. 2011;30(12):25–26. [Google Scholar]
- 22.Lu D.J., Wang Q., Mei S.W. Analogical research on the clinical efficacy of treating knee osteoarthritis with fire needle and moxa needle. New Tradit. Chin. Med. 2011;43:94–96. [Google Scholar]
- 23.Zhang G.B., Wang W.L., Zhang Q. Comparative study between fire needling and warm needling therapies for knee osteoarthritis. Shanghai J. Acupunct. Moxibust. 2013;32:299–300. [Google Scholar]
- 24.Chen Y., Jia Y.J., Lü J.H., Liu J.X., Zhang Z.D., Wang R.Q., Jia C.S. Comparision of therapertic effect of different acupuncture methods for knee osteoarthritis. Zhen Ci Yan Jiu. 2020;45(7):569–573. doi: 10.13702/j.1000-0607.191015. PMID: 32705832. [DOI] [PubMed] [Google Scholar]
- 25.Kuang Q.H. Treatment of 50 cases of knee osteoarthritis with fire needle therapy. J. Clin. Acupunct. Moxibust. 2006;22:19–20. [Google Scholar]
- 26.Zhu H. Treatment of 56 cases of knee osteoarthritis with therapy of fire-needle and cupping. J. Nanjing TCM Univ. 2010;26:475–476. [Google Scholar]
- 27.Tao S.P., He T.F., Luo Y.B. Observations on the efficacy of fire acupuncture plus filiform needle acupuncture in treating knee osteoarthritis. Shanghai J. Acupunct. Moxibust. 2013;32:742–746. [Google Scholar]
- 28.Lü J.J., Yang X.C., Ji T.T., Xue M.X. Randomized controlled clinical trials of treatment of knee osteoarthritis of yang-deficiency pattern by acupuncture plus moxibustion. Zhen Ci Yan Jiu. 2018;43(10):661–665. doi: 10.13702/j.1000-0607.170789. PMID: 30365263. [DOI] [PubMed] [Google Scholar]
- 29.Zheng J., Zhang H., Liu J. Different acupuncture and moxibustion methods at Heding (EX-LE 2) for knee osteoarthritis with yang-deficiency and coldstagnation syndrome. Zhongguo Zhen Jiu. 2017;37:594–598. doi: 10.13703/j.0255-2930.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Zhu L. Analogical research on the clinical efficacy of treating knee osteoarthritis with fire needle and cupping needle. Beijing J. Tradit. Chin. Med. 2013;32:605–607. [Google Scholar]
- 31.Wang Z. Treatment of 39 cases of knee osteoarthritis with therapy of fire-needle and Chinese medicine. TCM Res. 2015;28:45–47. [Google Scholar]
- 32.Gao J., Ouyang B.S., Zhang Y., Li J., Yang H.Z., Ji L.L., Wu Y.J., Wang W. Comparison of the clinical therapeutic effects between electroacupuncture and warming needle moxibustion for knee osteoarthritis of kidney deficiency and marrow insufficiency pattern/syndrome. Zhongguo Zhen Jiu. 2012;32(5):395–398. PMID: 22650121. [PubMed] [Google Scholar]
- 33.Wu J., Tian C. Observation on therapeutic effect of fire needle on gonarthritis of type of accumulation of pathogenic cold due to yang deficiency. Chin. Med. Mod. Distance Educ. China. 2014;32:2969–2978. [Google Scholar]
- 34.Lv J., Yang X., Ji T., Xue M. Clinical randomized controlled study of acupuncture and moxibustion with grains of wheat in the treatment of knee osteoarthritis of yang deficiency and cold congealing type. Acupunct. Res. 2018;43:10. [Google Scholar]
- 35.Lim M.Y., Huang J., Zhao B., et al. Current status of acupuncture and moxibustion in China. Chin. Med. 2015;10:12. doi: 10.1186/s13020-015-0041-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nguyen D.H. Thorsons; Wellingborough, UK: 1987. The Dictionary of Acupuncture and Moxibustion: A Practical Guide to Traditional Chinese Medicine. [Google Scholar]
- 37.Xu J., Yang Y. Traditional Chinese medicine in the Chinese health care system. Health Pol. 2009;90(2):133–139. doi: 10.1016/j.healthpol.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang Y., Xie X., Zhu X., Chu M., Lu Y., Tian T., Zhuang X., Jiang L. Fire-needle moxibustion for the treatment of knee osteoarthritis: a meta-analysis. Evid. Based Complement. Alternat. Med. 2016;2016 doi: 10.1155/2016/1392627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Park J.M., Lee C.K., Kim K.H., Kim E.J., Jung C.Y., Seo B.K., Goo B.H., Baek Y.H., Lee E.Y. A systematic review and meta-analysis of moxibustion treatment for knee osteoarthritis. J. Acupunct. Res. 2020;37(3):137–150. [Google Scholar]
- 40.Li S., Xie P., Liang Z., Huang W., Huang Z., Ou J., Lin Z., Chai S. Efficacy comparison of five different acupuncture methods on pain, stiffness, and function in osteoarthritis of the knee: a network meta-analysis. Evid. Based Complement. Alternat. Med. 2018;2018 doi: 10.1155/2018/1638904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yuan T., Xiong J., Wang X., Yang J., Zhou X., Liao K., Xu L. The effectiveness and safety of moxibustion for treating knee osteoarthritis: a PRISMA compliant systematic review and meta-analysis of randomized controlled trials. Pain Res. Manag. 2019;2019 doi: 10.1155/2019/2653792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Han J.S. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003;26(1):17–22. doi: 10.1016/s0166-2236(02)00006-1. [DOI] [PubMed] [Google Scholar]
- 43.Hu L., Wang L., Wei J., et al. Heat induces adenosine triphosphate release from mast cells in vitro: a putative mechanism for moxibustion. J. Tradit. Chin. Med. 2015;35(3):323–328. doi: 10.1016/s0254-6272(15)30105-9. [DOI] [PubMed] [Google Scholar]
- 44.Li X., Li Z., Wang L., et al. Effect of mild indirect moxibustion on hemorheology of knee osteoarthritis. Chin. Arch. Tradit. Chin. Med. 2012;30(9):2098–2099. [Google Scholar]
- 45.Liu D., Wu Y.L., Li C., Wang M.L., Ma X.X., Liu J.W., et al. Warming moxibustion attenuates inflammation and cartilage degradation in experimental rabbit knee osteoarthritis. J. Tradit. Chin. Med. 2021;41(6):959–967. doi: 10.19852/j.cnki.jtcm.2021.06.013. [DOI] [PubMed] [Google Scholar]
- 46.He J., Cortina M.S., Bazan H.E.P. The PEDF neuroprotective domain plus DHA induces corneal nerve regeneration after experimental surgery. Invest. Ophthalmol. Vis. Sci. 2015;56(6):3505–3513. doi: 10.1167/iovs.15-16755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou Y.L., He T.F., Bing X.H. Comparative study of the efficacy of fire needling versus electroacupuncture in treating knee osteoarthritis of kidney and marrow deficiency type. Shanghai J. Acu-Mox. 2017;36(5):513–518. [Google Scholar]
- 48.Wang C., Wang X.M., Wu H.G. Overview on clinical and mechanism Studies of Acupuncture and moxibustion Treatment of knee osteoarthritis. Tradit. Chin. Med. 2017;6(3):169–174. [Google Scholar]
- 49.Kong J., Wang Z., Leiser J., et al. Enhancing treatment of osteoarthritis knee pain by boosting expectancy: a functional neuroimaging study. Neuroimage: Clin. 2018;18:325–334. doi: 10.1016/j.nicl.2018.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barroso J., Wakaizumi K., Reis A.M., Baliki M., Schnitzer T.J., Galhardo V., Apkarian A.V. Reorganization of functional brain network architecture in chronic osteoarthritis pain. Hum. Brain Mapp. 2021 Mar;42(4):1206–1222. doi: 10.1002/hbm.25287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.