Abstract
Aims and Objectives:
Route of choice to access cervical paravertebral lesions with foraminal involvement is the anterolateral corridor with its variants. Main limitation of these techniques is represented by the limited surgical access to periforaminal area due to the bulk generated by the anterior scalene muscle (ASM). Over the years, alternative techniques for ASM surgical management have been developed, which are still today a matter of debate. Most popular include ASM scalene complete section (SCS) and ASM medial detachment (SMD). Authors describe an innovative, minimally invasive muscle section technique, the anterior selective scalenectomy (ASS), which reduces the risk of iatrogenic morbidity and optimizes exposure of periforaminal area in anterolateral cervical routes.
Materials and Methods:
A laboratory investigation was conducted. Technique was applied in a surgical setting, and an illustrative case was reported.
Results:
ASS is a quick and easy technique to perform. It allows optimization of surgical visibility and control on the periforaminal area in the cervical anterolateral corridor. It respects muscle anatomy and vascularization, favoring functional recovery and management of peri-operative pain; it reduces the risk of morbidity on phrenic nerve and pleura. Considering the minimally invasive nature of the technique, it allows for a slightly more limited exposure compared to traditional techniques while ensuring optimal surgical maneuverability on the target area.
Conclusions:
ASS represents an effective and safe alternative to traditional ASM section techniques for the exposure of periforaminal area in anterolateral cervical routes. It is indicated in case of lesions with paravertebral development and minimal intraforaminal component in the C3-C6 segment.
Keywords: Brachial plexus, cervical anterolateral approach, cervical paravertebral tumors, scalenectomy, ventral supraclavicular approach
INTRODUCTION
Surgery for cervical spinal tumors with both intra and extracanalar extension still represents a great matter of debate in terms of which approach should be the best to adopt in terms of minimizing morbidity and enriching exposure.[1,2,3,4,5,6,7,8,9,10,11,12]
The need to simultaneously control different anatomical compartments and the regional density of critical structures makes surgery in this area particularly challenging, even for experienced surgeons.[1,2,3,4,5,6,7,8,9,10,11,12]
In the case of lesions with predominantly paravertebral growth, in which the intracanalar component is limited to the intraforaminal portion, the approach of choice is represented by the anterolateral corridor in its different variants.[13,14,15,16] The main limitation of these techniques is represented by the poor surgical accessibility to the periforaminal area, mainly due to the bulk generated by the anterior scalene muscle (ASM).[13,14,15,16]
ASM surgical management is, therefore, a critical element in tumor resection. Finding the appropriate balance between the risk of iatrogenic morbidity and anatomical control on critical structures is essential for the safety and effectiveness of surgical excision, as well as for the patient's functional outcome. Historically, alternative ASM section techniques have been developed, each of them with its own proponents and detractors.[6,14,17]
In the present study, authors describe an innovative, minimally invasive muscle section technique, the anterior selective scalenectomy (ASS), which reduces the risk of iatrogenic morbidity and optimizes surgical exposure of the periforaminal area in anterolateral cervical routes.
TECHNICAL NOTE
A standard ventral supraclavicular approach is performed.[13,14,15,16] The patient is positioned supine, with the head turned on the contralesional side, and the ipsilateral shoulder is elevated.[14]
A linear skin incision is performed along the lateral margin of the sternocleidomastoid muscle (SCM). Alternative incisions are V or L-shaped, with one side along the SCM lateral edge and the other parallel to the clavicle. Soft-tissue dissection is carried out.[14]
The platysma is divided parallel into the skin incision. SCM integrity is preserved, but some authors suggest its division, which might cause additional tissue trauma and prolonged recovery.[17] As an alternative to SCM transection, some authors suggest muscle dilation between its sternal and clavicular heads to create an intramuscular window or division of the only sternal head.[17]
The underlying omohyoid is retracted; in case of a need for more caudal extension, it can be transected.[14]
The fat pad is transected under neurophysiological monitoring, taking care not to damage accessory nerve branches, deep to scalene muscles, and brachial plexus exposure. The supraclavicular artery and vein are ligated and divided. The phrenic nerve is identified on the ASM belly.[14] The C5 spinal nerve is the first brachial plexus element to be exposed. Following the nerve, the upper trunk is identified. Progressively, the middle and lower trunks are exposed.[14]
At this point, to optimize surgical visibility and control of the periforaminal area, two different techniques have been described. The traditional techniques of the interscalene approach entail the transection of the ASM belly section (complete scalene section, SCS) and its detachment from the underlying apical pleura.[14,17] An alternative procedure, scalene medial detachment (SMD), consists of muscle detachment from cervical tubercles, opening a corridor medial to the muscle, with the advocated advantage of preserving ASM function.[6] The surgical technique and anatomic principles of selective scalenectomy are depicted in Figure 1.
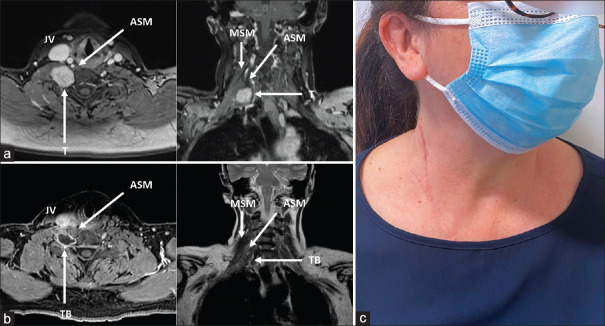
Figure 1.
Schematic drawing showing anatomic principles of selective scalenectomy for periforaminal exposure. (a) Coronal view. (b) Axial view. AN - Accessory nerve, ASM - Anterior scalene muscle, CA - Carotid artery, CL - Clavicle, IT - Inferior trunk, JV - Jugular vein, LC - Longus colli, MSM - Median scalene muscle, MT - Medial trunk, NR - Nerve root, PN - Phrenic nerve, PSM - Posterior scalene muscle, SCM - Sternocleidomastoid muscle, ST - Superior trunk, VN - Vagal nerve
Alternatively, the ASS, a minimally invasive muscle section technique, is proposed. The technique consists of a T-shaped incision, with the transverse cut directed in a lateral to the medial direction and a further orthogonal longitudinal splitting of muscle fibers. The incision level should be centered on the root, which has to be exposed and carried out parallel to it in a lateral to medial direction. The extension in the axial plane must be kept less than one-third of the thickness of the muscle belly to minimize the risk of functional damage. Longitudinal fiber splitting optimizes access extension while respecting muscle anatomy.
ASS reduces the risk of iatrogenic morbidity and optimizes surgical exposure of the periforaminal area in anterolateral cervical routes.
Figures 2 and 3 show the application of the technique in a surgical setting. The clinical case of the resection of a brachial plexus schwannoma is reported. Pre- and postoperative magnetic resonance imaging, intraoperative view, and patient picture are provided.
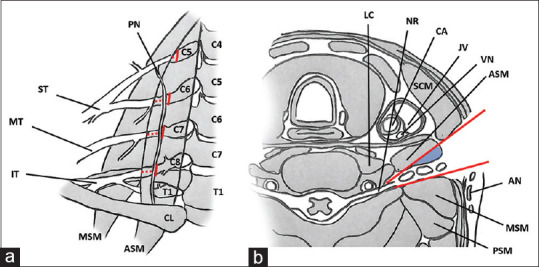
Figure 2.
Intraoperative view (a) with correspondent schematic drawing (b). ASM - Anterior scalene muscle, CA - Carotid artery, JV - Jugular vein, PN - Phrenic nerve, R - Retractor, SCM - Sternocleidomastoid muscle, ST - Superior trunk, TB - Tumor bed
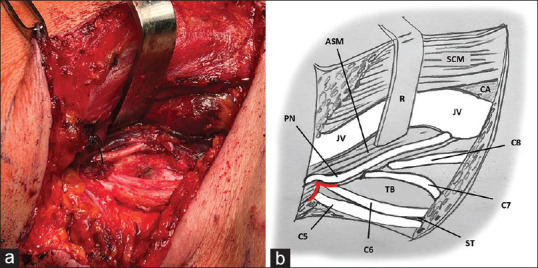
Figure 3.
Preoperative MRI (a), postoperative MRI (b), and picture of the patient (c). ASM - Anterior scalene muscle, JV - Jugular vein, MSM - Median scalene muscle, T - Tumor, TB - Tumor bed, MRI - Magnetic resonance imaging
DISCUSSION
Surgery for cervical spinal tumors with both intra and extracanalar extension still represents a topic of great debate within the neurosurgical community regarding which should be the best route to approach this kind of lesion.[1,2,3,4,5,6,7,8,9,10,11,12]
The need to simultaneously control different anatomical compartments and the regional density of critical neurovascular structures makes surgery in this area particularly demanding, even in expert hands.[1,2,3,4,5,6,7,8,9,10,11,12]
One of the most relevant pathologies in this area is brachial plexus schwannomas with foraminal involvement. The entity of intracanalar extension is a determining element in the selection of a single-versus multi-staged approach,[18] eliging patients with relevant intracanalar extension to staged surgery.[6,8,10,18]
In cases of lesions with predominantly paravertebral growth and only a small intraforaminal portion, the elective route is the anterolateral approach in its main variants: the George's approach (GA)[19,20,21] and the ventral supraclavicular approach (VSA).[13,14,15,16] Surgical maneuverability, in terms of the angle of incidence of the surgical corridor on target areas and conizing effect, makes both these approaches significantly more advantageous compared to the anterior route to cervical foramen as described by Verbiest.[22]
GA is mainly indicated in pure foraminal and periforaminal pathologies involving the most proximal radicular compartment, also allowing access to the intracanalar space through its transcorporeal variant.[19,20,21]
On the other side, VSA is indicated in pathologies with prevalent paravertebral extracanalar development with minimal foraminal involvement, as in the case of brachial plexus schwannomas. VSA allows for optimal control of brachial plexus elements from C5 to T1 but suffers from poor surgical exposure and maneuverability at the periforaminal area, with consequent poor control over the vertebral artery and the most proximal component of the nerve root.[17]
The major boundary for foraminal accessibility is represented by ASM.[13,14,15,16] Its surgical management is, therefore, a critical element in tumor resection. Finding the appropriate balance between the risk of iatrogenic morbidity and control of neurovascular structures is essential for the safety and extension of surgical excision and for the maintenance of the patient's functional outcome. Historically, alternative intraoperative ASM section techniques have been described.[6,14,17]
Traditional techniques of the interscalene approach (i.e., the corridor between middle and ASMs) include a complete muscle belly section SCS and its detachment from the underlying parietal pleura at the pulmonary apex.[6,14,17] A variant of the approach involves muscle detachment from cervical tubercles SMD, opening a corridor medial to the muscle, with the advocated advantage of preserving ASM function.[6] Actually, in both cases, scalene atrophy is not a negligible complication; in the first case, it is due to the complete interruption of muscle fibers, and in the second one to muscle proximal deafferentation. ASM vascular supply is indeed guaranteed by distal afferents deriving from the first rib and proximal afferents deriving from transverse processes of cervical vertebrae from C3 to C6. Considering muscle function, both as its own and synergistic activity, functional insufficiency can lead to thoracic girdle imbalance with potentially significant consequences in terms of chronic pain and patient's quality of life worsening.
In the present study, authors describe an innovative technique of selective muscle section, which ensures its functional preservation, optimizing visibility, and surgical accessibility on the periforaminal area. The technique consists of a T-shaped incision, with the transverse cut directed in a lateral to the medial direction and a further orthogonal longitudinal splitting of muscle fibers. The extension in the axial plane must be kept less than one-third of the thickness of the muscle belly to minimize the risk of functional damage. The longitudinal fibers splitting optimizes access extension while respecting muscle anatomy.
To demonstrate the feasibility of the technique, an illustrative case of complete resection of brachial plexus schwannoma in a 50-year-old woman is reported.
The maneuver is easy and quick to perform. It allows for improving the visibility and surgical control of the periforaminal area in VSA. At the end of the surgery, section margins can be quickly reapproximated with a single stitch. ASS respects muscle vascularization and maintains the overall integrity of the muscle belly. It does not require neurolysis and transposition of the phrenic, thus reducing the risk of inadvertent damage to the nerve. To the same extent, the risk of injury to the parietal apical pleura is minimized as compared to SCS since there is no surgical dissection.
Given the minimally invasive nature of the technique, ASS can be applied in selective exposure of a single foramen, allowing for a slightly more limited exposure than traditional interscalene techniques, SCS and SMD. Compared to the latter, however, the viewing angle obtained by ASS is more direct, as it is coaxial to those of the main surgical corridor, an aspect that ultimately optimizes maneuverability on target areas. Limitation of muscle trauma promotes quick functional recovery and better management of perioperative pain.
The technique is indicated for lesions with anterolateral paravertebral extraforaminal development with minimal intraforaminal component in the C3-C6 segment.
CONCLUSION
ASS represents an effective and safe alternative to traditional scalene section techniques for exposing the periforaminal area in anterolateral cervical approaches.
It allows for optimized visibility and surgical control, respecting muscle anatomy and vascularization, thus reducing the risk of iatrogenic morbidity on the phrenic nerve and pleura.
Given its minimally invasive nature, it allows for a slightly more limited exposure than traditional techniques while ensuring optimal surgical maneuverability on the target area.
It is indicated in lesions with extraforaminal paravertebral extension with minimal intraforaminal component in the C3-C6 segment.
Ethical standards
This article does not contain any studies with living human participants or animals performed by any of the authors.
Financial support and sponsorship
Nil.
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
REFERENCES
- 1.Binder DK, Smith JS, Barbaro NM. Primary brachial plexus tumors: Imaging, surgical, and pathological findings in 25 patients. Neurosurg Focus. 2004;16:E11. doi: 10.3171/foc.2004.16.5.12. [DOI] [PubMed] [Google Scholar]
- 2.Das S, Ganju A, Tiel RL, Kline DG. Tumors of the brachial plexus. Neurosurg Focus. 2007;22:E26. doi: 10.3171/foc.2007.22.6.27. [DOI] [PubMed] [Google Scholar]
- 3.Go MH, Kim SH, Cho KH. Brachial plexus tumors in a consecutive series of twenty one patients. J Korean Neurosurg Soc. 2012;52:138–43. doi: 10.3340/jkns.2012.52.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang JH, Zaghloul K, Zager EL. Surgical management of brachial plexus region tumors. Surg Neurol. 2004;61:372–8. doi: 10.1016/j.surneu.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Jia X, Yang J, Chen L, Yu C, Kondo T. Primary brachial plexus tumors: Clinical experiences of 143 cases. Clin Neurol Neurosurg. 2016;148:91–5. doi: 10.1016/j.clineuro.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State University health sciences center. J Neurosurg. 2005;102:246–55. doi: 10.3171/jns.2005.102.2.0246. [DOI] [PubMed] [Google Scholar]
- 7.Kline DG, Judice DJ. Operative management of selected brachial plexus lesions. J Neurosurg. 1983;58:631–49. doi: 10.3171/jns.1983.58.5.0631. [DOI] [PubMed] [Google Scholar]
- 8.Lee HJ, Kim JH, Rhee SH, Gong HS, Baek GH. Is surgery for brachial plexus schwannomas safe and effective? Clin Orthop Relat Res. 2014;472:1893–8. doi: 10.1007/s11999-014-3525-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lusk MD, Kline DG, Garcia CA. Tumors of the brachial plexus. Neurosurgery. 1987;21:439–53. doi: 10.1227/00006123-198710000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Vučemilo L, Lajtman Z, Mihalj J, Plašćak J, Mahović Lakušić D, Mužinić D. Brachial plexus schwannoma – Case report and literature review. Acta Clin Croat. 2018;57:366–71. doi: 10.20471/acc.2018.57.02.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiani B, El-Farra MH, Dahan A, Endres P, Taka T, Delgado L. Brachial plexus tumors extending into the cervicothoracic spine: A review with operative nuances and outcomes. Clin Transl Oncol. 2021;23:1263–71. doi: 10.1007/s12094-020-02549-7. [DOI] [PubMed] [Google Scholar]
- 12.Hill JR, Lanier ST, Rolf L, James AS, Brogan DM, Dy CJ. Trends in brachial plexus surgery: Characterizing contemporary practices for exploration of supraclavicular plexus. Hand (N Y) 2023;18:14S–21S. doi: 10.1177/15589447211014613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kindl RP, Patel K, Trivedi RA. Supraclavicular brachial plexus approach for excision of C8 nerve root schwannoma: 3-dimensional operative video. Oper Neurosurg (Hagerstown) 2019;16:634–5. doi: 10.1093/ons/opy209. [DOI] [PubMed] [Google Scholar]
- 14.Saifuddin A. Imaging tumours of the brachial plexus. Skeletal Radiol. 2003;32:375–87. doi: 10.1007/s00256-003-0618-0. [DOI] [PubMed] [Google Scholar]
- 15.Tender GC, Kline DG. Anterior supraclavicular approach to the brachial plexus. Neurosurgery. 2006;58:S–4. doi: 10.1227/01.NEU.0000209027.52848.A3. [DOI] [PubMed] [Google Scholar]
- 16.Tschoe C, Holsapple JW, Binello E. Resection of primary brachial plexus tumor via a modified supraclavicular approach. J Neurol Surg Rep. 2014;75:e133–5. doi: 10.1055/s-0034-1376423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siqueira MG, Martins RS, Teixeira MJ. Management of brachial plexus region tumours and tumour-like conditions: Relevant diagnostic and surgical features in a consecutive series of eighteen patients. Acta Neurochir (Wien) 2009;151:1089–98. doi: 10.1007/s00701-009-0380-8. [DOI] [PubMed] [Google Scholar]
- 18.Desai KI. Primary benign brachial plexus tumors: An experience of 115 operated cases. Neurosurgery. 2012;70:220–33. doi: 10.1227/NEU.0b013e31822d276a. [DOI] [PubMed] [Google Scholar]
- 19.Bruneau M, Cornelius JF, George B. Microsurgical cervical nerve root decompression by anterolateral approach. Neurosurgery. 2006;58:S108–13. doi: 10.1227/01.NEU.0000193521.98836.C5. [DOI] [PubMed] [Google Scholar]
- 20.Cornelius JF, Bruneau M, George B. Microsurgical cervical nerve root decompression via an anterolateral approach: Clinical outcome of patients treated for spondylotic radiculopathy. Neurosurgery. 2007;61:972–80. doi: 10.1227/01.neu.0000303193.64802.8f. [DOI] [PubMed] [Google Scholar]
- 21.George B, Zerah M, Lot G, Hurth M. Oblique transcorporeal approach to anteriorly located lesions in the cervical spinal canal. Acta Neurochir (Wien) 1993;121:187–90. doi: 10.1007/BF01809273. [DOI] [PubMed] [Google Scholar]
- 22.Verbiest H. Lateral operations on the cervical spine. Neurochirurgie. 1970;16(Suppl 2):123. doi: 10.1007/BF01647460. [DOI] [PubMed] [Google Scholar]