ABSTRACT
Background:
The immediate impact of the pandemic on resident training has been well documented. As the pandemic and its effects persisted beyond what was initially predicted, this study aimed to assess the impact of the pandemic on the training of family medicine (FM) residents a year after it began and to assess the burnout residents experienced during this period.
Methods:
The survey was conducted between January 18 and February 18, 2021. Participation was solicited via an email sent to the program directors throughout the US, who were asked to circulate the survey among their residents. The questionnaire was divided into sections to assess the impact of the pandemic on clinical training, didactics, and preparedness for the next phase in the career. In addition, the burnout experienced was assessed using the Copenhagen Burnout Inventory.
Results:
227 responses were analyzed. 83% (n = 186) of respondents felt that the pandemic had a negative impact on their training and 63% (n = 141) felt that the pandemic had a negative impact on didactics. 50% (n = 44) of the third-year residents thought that they would be able to meet the graduation requirement for outpatient encounters. 41% (n = 36) of the third-year residents felt less prepared for the next step in their careers. 119 respondents met the cutoff threshold for personal burnout, 134 for work-related burnout, and 65 for client-related burnout.
Conclusion:
Residency training is difficult with high reported rates of burnout before the COVID-19 pandemic. This study reinforces the evidence that the pandemic made both mental well-being and adequate training more difficult for FM residents across the country.
Keywords: Burnout, clinical training, COVID-19, family medicine, resident training
Introduction
The coronavirus disease (COVID-19) pandemic placed tremendous strain on the healthcare system.[1] As the pandemic raged across the United States, the Centers for Medicare and Medicaid Services recommended the suspension of non-essential medical and surgical services to preserve critical resources.[2] Resident physicians were a critical workforce and had to be reorganized to provide coverage for essential services, all while preserving their own health and continuing their education. Innovative solutions were adopted for academic training. These included the incorporation of online platforms to host the didactics and the utilization of surgical videos to compensate for reduced procedural experience.[3,4] In this transition, residents had to deal with a unique set of challenges: uncertainty about meeting graduation requirements, licensing exams being canceled, and living in the constant fear of contracting a novel infection. These disruptive changes can be expected to exacerbate the effects of regular work-related stressors in a population with a baseline high burnout rate.[5] As programs struggled to provide patient care and a safe learning environment, strategies were implemented to limit resident exposure to COVID-19 which could have unintentionally compromised their training.[6]
Several researchers from different disciplines have studied the impact of COVID-19 on resident training during the early phase of the pandemic.[7,8,9,10,11,12,13] However, the pandemic and its effects on healthcare organizations persisted beyond what many experts initially predicted. Although the negative impact of the pandemic on resident training in the early phase has been well documented, there is a dearth of follow-up studies. This study aims to bridge this gap.
The objectives of this study were (1) to assess the impact of the pandemic on the training of family medicine (FM) residents a year after it began and (2) to assess the burnout residents experienced during the first year of the pandemic. The results of the study may help in formulating guidelines to better address the needs of FM residents during future public health emergencies.
Methods
Data source
This was a cross-sectional survey of FM residents in the United States administered between January 18 to February 18, 2021. The study was approved by the Institutional Review Board (IRB #21.0015). Participation in the study was solicited via an email sent to the program directors of accredited FM residency programs throughout the US, using the Association of Family medicine directors list serve. The program directors were asked to distribute the survey among their residents. Following the initial request, a reminder was sent 2 weeks later.
Questionnaire
The survey was divided into sections to focus on the demographics of respondents, the impact of the pandemic on didactics, clinical training, and resident perceptions of preparedness for graduation. Survey items assessing clinical activities were included from different domains such as inpatient and outpatient care, procedural experiences, and didactic sessions. These items were developed based on feedback and concerns from current residents and recent graduates from the authors’ residency program. Pretesting was completed on recent graduates before releasing it to the target population, and the survey was modified to shorten the completion time and improve readability.
Burnout assessment
Burnout among residents was assessed using the Copenhagen Burnout Inventory (CBI) which is a validated screening tool for measuring burnout and is freely available for use in the public domain.[14,15] The CBI assesses three domains of burnout, including personal, work-related, and client-related burnout. The section was modified to capture only the period spanning a year before completing the survey, targeting the year 2020. Following the instructions, the answers were converted into a scoring system from 0 to 100. The score for each scale corresponded to the calculated mean of the scale score.
Statistical analysis
Residents’ descriptors and survey question responses were summarized with frequency count and percentage. The association of responders’ characteristics on the responses was evaluated with logit models regressing the responses on all descriptors. The effect was presented with an odds ratio (OR) and associated 95% confidence intervals (CIs). For the burnout-related responses measured by the CBI subscales, the summary was presented using mean with SD, median with 1st and 3rd quartiles, and extremes (minimum and maximum). The effect of descriptors was analyzed with linear regression for each subscale and presented as a difference estimate with 95% CI. All tests were 2-sided, and the significance level was set to 5%. Statistical analyses were performed in SAS 9.4 (SAS Inc, Cary, NC).
Results
We analyzed 227 responses from 34 different states [Figure 1]. Residents from all 3 years of training were well represented. The complete demographics of all respondents are presented in Table 1.
Figure 1.
Regions represented in the study
Table 1.
Demographics of the FM residents surveyed
| Demographic variable | Number of respondents(%) |
|---|---|
| Residency level | |
| PGY-1, n (%) | 62 (27%) |
| PGY-2, n (%) | 74 (33%) |
| PGY-3, n (%) | 88 (39%) |
| Missing, n (%) | 3 (1%) |
| Age group | |
| <30 | 97 (43%) |
| 30+ | 127 (56%) |
| Missing, n (%) | 3 (1%) |
| Gender Identity | |
| Male, n (%) | 92 (41%) |
| Female, n (%) | 130 (57%) |
| Other/Prefer not to answer/missing n (%) | 5 (2%) |
| US Census Region | |
| West, n (%) | 49 (22%) |
| Midwest, n (%) | 48 (21%) |
| Northeast, n (%) | 45 (20%) |
| South, n (%) | 76 (33%) |
| Missing, n (%) | 9 (4%) |
| Residency program type | |
| University, n (%) | 103 (45%) |
| Community, n (%) | 113 (50%) |
| Other/Missing, n (%) | 11 (5%) |
| Living arrangements | |
| Living alone, n (%) | 69 (30%) |
| Living with friends or roommates, n (%) | 13 (6%) |
| Living with a partner/spouse, n (%) | 83 (37%) |
| Living with a partner/spouse and children, n (%) | 49 (22%) |
| Other/Missing, n (%) | 13 (6%) |
Clinical training: 83% (n = 186) of residents reported that the pandemic had a negative impact on their training. 64% (n = 144) reported more than a 25% decline in the number of patients seen in the continuity clinic in the early phase of the pandemic from March to April 2020. Later in the year, the situation changed; however, 34% still reported more than a 25% decline in the clinical volume between November and December 2020. A decline in hands-on procedural experience was reported by 59% (n = 133). 61%reported having missed a rotation. Among the reasons for missing rotations, the majority were reported secondary to facilities not accepting residents (41%). In addition, modified resident coverage, reassignment to other duties, (and being in quarantine were the other reported reasons. [Table 2]
Table 2.
Residents’ perception of the pandemic’s impact on their clinical training
| Survey questions | Number of respondents (%) |
|---|---|
| The COVID-19 pandemic has negatively impacted my residency training | |
| Strongly disagree | 6 (3%) |
| Somewhat disagree | 14 (6%) |
| Neutral | 18 (8%) |
| Somewhat agree | 136 (61%) |
| Strongly agree | 50 (22%) |
| My clinical experience on inpatient rotations (i.e., pediatrics, OBGYN) during the pandemic has been inferior to my colleagues’ experience before the pandemic | |
| Strongly disagree | 29 (13%) |
| Somewhat disagree | 50 (22%) |
| Neutral | 57 (25%) |
| Somewhat agree | 62 (28%) |
| Strongly agree | 26 (12%) |
| I have performed fewer procedures (i.e., joint injections, LARC placement, OB deliveries, etc.) as a result of the pandemic | |
| No | 34 (15%) |
| Yes | 133 (59%) |
| Unsure | 57 (25%) |
| During the pandemic, at some point, I was re-assigned to work on another service (inpatient/ER/ICU) | |
| No | 112 (50%) |
| Yes | 112 (50%) |
| During the pandemic, I had to miss any rotation (entirely or miss a significant time) | |
| No | 87 (39%) |
| Yes | 137 (61%) |
| I think I will have an opportunity to make up for missed rotations in the future | |
| No | 79 (35%) |
| Yes | 33 (15%) |
| Unsure | 44 (20%) |
| Does not apply to me | 67 (30%) |
Didactics: 63% (n = 141) of respondents reported that the pandemic had a negative impact on their didactic activities. 77% reported their programs transitioned to virtual didactics during the pandemic, and 26% (n = 58) felt that virtual didactics was superior to in-person learning. Although only about 30% (n = 68) were able to participate in didactics outside of their program, 68% (n = 151) indicated they would want to participate in interinstitutional lectures in the future [Table 3].
Table 3.
Residents’ perspective of the pandemic’s impact on Didactics
| Survey questions | Number of respondents (%) |
|---|---|
| The pandemic has had a NEGATIVE impact on didactics | |
| Strongly disagree | 18 (8%) |
| Somewhat disagree | 32 (14%) |
| Neutral | 33 (15%) |
| Somewhat agree | 76 (34%) |
| Strongly agree | 65 (29%) |
| I think learning through virtual interactive didactics is BETTER than in-person learning | |
| Strongly disagree | 60 (27%) |
| Somewhat disagree | 57 (25%) |
| Neutral | 49 (22%) |
| Somewhat agree | 40 (18%) |
| Strongly agree | 18 (8%) |
| After the pandemic is over, I would want to continue using online platforms for virtual didactics | |
| Strongly disagree | 47 (21%) |
| Somewhat disagree | 47 (21%) |
| Neutral | 27 (12%) |
| Somewhat agree | 64 (29%) |
| Strongly agree | 36 (16%) |
| Does not apply to me | 3 (1%) |
| I am interested in participating in interinstitutional lectures/webinars in the future | |
| Strongly disagree | 6 (3%) |
| Somewhat disagree | 14 (6%) |
| Neutral | 53 (24%) |
| Somewhat agree | 84 (38%) |
| Strongly agree | 67 (30%) |
Graduation requirements and Feeling of Preparedness: 50% of the PGY-3 (n = 44) and PGY-2 (n = 37) residents felt that they would be unable to meet the graduation requirement of 1650 completed in-person patient encounters at their FM practice site. Whereas 41% (n = 36) of the PGY-3 residents felt less prepared for the next phase of their career, 19% (n = 17) were unsure. Among the PGY-2 residents, 35% (n = 26) felt less prepared, whereas 34% (n = 25) were unsure [Figure 2]. The odds of feeling less prepared for the next step in the career were significantly higher for respondents from the North-East and the South compared to those in the West (respectively OR: 3.08, 95% CI (1.13, 8.46): and OR: 2.62, 95%CI: (1.03, 6.68).
Figure 2.
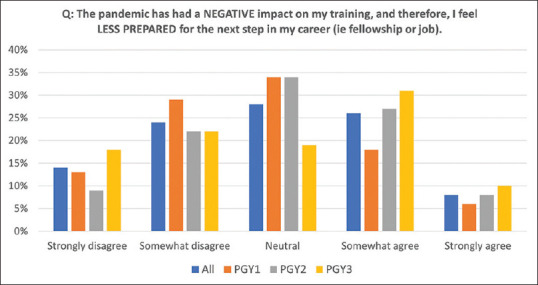
Residents’ perception of their preparedness for the next phase of their career
Burnout: The mean scores for the personal, work-related, and client-related burnout subscales were 50.6, 57.9, and 43.4, respectively. 52% (n = 119) of respondents met the threshold for personal burnout, 59% (n = 134) for work-related burnout, and 29% (n = 65) for client-related burnout [Table 4]. There was no statistically significant difference in burnout experienced by residents from the different regions of the country, nor did the training year demonstrate significance.
Table 4.
Residents’ burnout measured by Copenhagen Burnout Inventory (CBI). The threshold for burnout is a score of 50
| Burnout subscales | Score |
|---|---|
| Personal burnout | |
| Mean±SD | 50.68±22.75 |
| Median [Q1-Q3] | 50 [33-67] |
| Range, Min-Max | 0-100 |
| Above threshold | 52% |
| Work burnout | |
| Mean±SD | 57.95±19.57 |
| Median [Q1-Q3] | 57 [46-71] |
| Range, Min-Max | 18.00-100 |
| Above threshold | 59% |
| Client burnout | |
| Mean±SD | 43.41±25.79 |
| Median [Q1-Q3] | 46 [21-58] |
| Range, Min-Max | 0-92 |
| Above threshold | 29% |
Discussion
The pandemic significantly impacted the healthcare system including the training of physicians. Whereas the immediate impact on the training of physicians in FM has been documented, our study highlights the fact that a year after the pandemic started, FM residents continued to experience negative impacts on their training, skill acquisition, and overall feelings of competence and well-being.[10]
Clinical training: Traditionally, FM residents acquire their clinical skill set through managing patients in two settings: continuity clinic and inpatient services. In addition, they also broaden their knowledge and skills by working with physicians in various disciplines on clinical rotations. To ensure the standard across the training programs in the US, the accreditation council of graduate medical education (ACGME) sets guidelines and requirements for programs. One of these includes a requirement to complete 1650 in-person patient encounters at their continuity clinic. In addition, a required number of hours and/or patient visits have been set for certain rotations.[16]
Fashner in his study reported disruptions in rotations with several specialties during the pandemic.[6] A decline in clinical encounters in the continuity clinic has been previously reported and was also reported in our study.[10] This effect was more pronounced during the early phase of the pandemic (March–April 2020). This may be a reflection of practice-specific restrictions and patient avoidance of in-person services. Even as COVID-based restrictions were relaxed, the number of patients remained low. It is possible that the threat of exposure to the virus kept patients from coming to the clinic and caused a delay in having elective procedures performed. Consequently, there were fewer opportunities for residents to perform procedures such as joint injections and long acting reversible contraceptive (LARC) placements as noted in our study. A decline in LARC placement during the pandemic has been reported across the US.[17] The resurgence of COVID-19 cases in the Winter of 2020 correlated with a decline in patient volume in clinics, although the effect was not as pronounced as in the Spring of 2020.
To preserve the resident workforce administrators used several strategies which may have affected the learning opportunities. One strategy was to designate a single resident to take care of a COVID-19-positive patient and to perform any procedures required for them such as the delivery of an infant.[18] Perhaps strategies like this limited patient exposure, which led 40% of residents in our survey to report an inferior experience during the pandemic on rotations such as inpatient pediatrics and obstetrics. Similarly, to protect our vulnerable elderly population, most of the nursing homes were closed to non-essential personnel affecting residents’ access to geriatric clinical experience.[6,19]
Didactics: In response to social distancing guidelines, most residency programs discontinued in-person didactics and moved to an online platform. Gelineau et al., in their 3-month survey post-transition to virtual learning, found that 88% of their respondents (which included a mix of faculty, nurses, and residents) wished to continue having educational activities virtually.[20] Singhi reported that out of 30 respondents, 63% of their residents and fellows felt that they learned an equivalent amount from online didactics compared to that in-person.[21] The flexibility/practicality of distanced learning might have been particularly helpful for those with personal or family commitments during the pandemic. In our survey, although only 26% agreed that virtual learning was better than in-person, 42% wanted to continue using online platforms in the future. Many residents may appreciate the flexibility of online learning, but we must acknowledge that it has its limitations, especially in the procedural and practical skill domains.
Graduation requirements and preparedness for the next phase: One of the graduation requirements for FM residents is completing a minimum of 1650 in-person patient encounters.[16] Due to the decline in outpatient clinic visits during the pandemic, residents were reasonably concerned about meeting this requirement. 50% of the PGY-3 respondents felt that they would be unable to meet this requirement. The decline in clinical volume has been acknowledged among program directors (PDs).[6] However, the majority were confident that it would not cause accreditation issues. ACGME, in March 2020, stated that the PDs would have to consider the circumstances in collaboration with the Clinical Competency Committee to assess the readiness of each resident to progress to the next level of education or successfully complete the program.[22] However, the concern among the residents was not just about meeting the requirements. The decline in patient encounters also impacted their feelings of competence with 41% of the graduating residents reporting feeling less prepared than they expected under normal training circumstances. This feeling of lack of preparedness in professional life secondary to pandemic effects is also evident in surveys from the other disciplines.[8,23] Fewer patient encounters in continuity clinics, less patient exposure in other disciplines, and a reduction in elective procedures may all have contributed to these findings.
The objective impact on the overall competence of the graduating residents will require further evaluation. Perhaps, the results from this survey will help in developing and implementing strategies to mitigate the impact and increase the professional confidence of graduates. Some residents will have completed the majority of their post-graduate training during the pandemic. Though history is unchangeable, it is paramount that efforts are made to maximize residents’ education for the sake of their confidence and the patients they will care for. Evidence-based examples of this would include incorporating a case-based learning approach led by faculty members covering common clinical scenarios which is more engaging than traditional lecture approaches and can boost resident confidence in handling cases.[24] The use of simulators to make up for fewer procedures is one of the measures that can help minimize the impact of the pandemic on training. Technology can also be utilized to make recorded videos available for use and wider dissemination to trainees. Additionally, outside resources can be leveraged with the dissemination of information about programs (case discussions and lectures) on commonly visited websites such as the American Board of Family Medicine (ABFM) and the American Academy of Family Physicians (AAFP). Interinstitutional collaboration, as was utilized in some disciplines can be a quick and efficient way to capitalize on restructuring existing resources from multiple institutes and to create better learning experiences.[4,7,25,26] The majority of FM residents in our study were not aware/not able to participate in such programs, but if given the opportunity, they were willing to participate.
Burnout: Burnout among resident physicians is well documented.[5] It not only affects the quality of their life but also the quality of care they provide.[27] The fear of possible COVID-19 exposure was an additional stressor for already strained residents with 81% (n = 182) of surveyed residents endorsing a fear of contracting COVID-19 and transmitting it to family members (91%, n = 205).
Burnout was reported in 51% of residents in a metanalysis.[5] In the same study, the prevalence of burnout among the FM residents (n = 213) was reported to be 35.9%. There is a scarcity of studies assessing burnout specifically among FM residents before the pandemic.[28,29,30] Lebensohn et al., in their study on 168 residents, reported high emotional exhaustion in 13.7% and high depersonalization in 23.8%.[29] Rutherford in their study on 10 FM residents found that 75% met the criteria for burnout.[30] More recently, during the pandemic, Awadallah in their study reported burnout among 39.7% of FM residents.[10] In our study, personal burnout was reported in 52%, work-related burnout in 59%, and client-related burnout in 29% of respondents.
There are notable differences in measurement scales employed to assess burnout. However, the literature is consistent in finding that the pandemic has had a negative impact on residents with higher rates of burnout being reported. Zoorob et al. utilized the resident fellow well-being index, a 7-question tool that asks about feelings of burnout, symptoms of depression, and signs of fatigue.[12] They reported burnout in 51.5% of their respondents in the early stage of the pandemic. Awadallah utilized a single-item burnout question. Cravero in their study utilized two validated single-item measures of emotional exhaustion and depersonalization to assess burnout.[13]
The fear of contracting COVID-19 infection and transmitting it to friends and family was high in our survey. This was also one of the biggest concerns that were highlighted in the survey undertaken among general surgery residents in Boston.[31] In the same study, it was reported that to decrease this possibility, some residents chose to stay away from family when working with COVID-19 patients. In our study, we found that although the fear of contracting infection and passing it on was high, client (patient)-related burnout was reportedly lower compared to personal and work-related burnout, emphasizing the fact that despite the strains of working in the pandemic, the stress of working with patients was not the main contributor to burnout. In addition, as noted by Zaroob, the burnout scores were not significantly different when a subgroup analysis was performed.[12]
Limitations
The study has its limitations. We analyzed responses from 227 residents. However, we were unable to determine the true response rate as we were unsure of how many residents received the survey. In the 2020–21 academic year, there were 14,225 FM residents in ACGME-accredited programs. Based on this, the theoretical response rate was 1.5%. It is not possible at this stage to determine if the low response rate was due to residents not receiving the survey or other factors. At the time that this study was attempting to collect data, other researchers were also sending out surveys to the same population which could have led to “survey fatigue,” further blunting the response rate. Another limitation is that a portion of the questionnaire used for the study was not strictly validated. However, there is no widely available tool to assess the subjective impact of a health crisis of this magnitude on resident training and preparedness. This section of the survey was designed to characterize common resident concerns about their training. Finally, the utilization of the CBI for the assessment of burnout limits the comparability of our study to those that use other tools to measure burnout.
Conclusions
FM residents in training in the US during the COVID-19 pandemic reported negative impacts on their education as well as their mental well-being. These findings highlight the need for strategic interventions to maximize resident education and training opportunities, as well as additional support for their mental and emotional health. Such educational interventions may include the continuation of virtual didactics and technology-driven educational supplementation. Admittedly, more research is needed to evaluate the objective outcomes of pandemic-era resident education, but the resident-reported impact we describe here warrants immediate consideration and action from our FM programs nationally.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems:International perspectives. Best Pract Res Clin Anaesthesiol. 2021;35:293–306. doi: 10.1016/j.bpa.2020.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CMS Adult Elective Surgery and Procedure recommendations. [[Last accessed on 2022 May 24]]. Available from https://www.cms.gov/files/document/covid-elective-surgery-recommendations.pdf .
- 3.Tolu LB, Feyissa GT, Ezeh A, Gudu W. Managing resident workforce and residency training during COVID-19 Pandemic:Scoping review of adaptive approaches. Adv Med Educ Pract. 2020;11:527–35. doi: 10.2147/AMEP.S262369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson J, Chung MT, Carron MA, Chan EY, Lin HS, Hotaling J. Novel changes in resident education during a pandemic:Strategies and approaches to maximize residency education and safety. Int Arch Otorhinolaryngol. 2020;24:e267–71. doi: 10.1055/s-0040-1714147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Low ZX, Yeo KA, Sharma VK, Leung GK, McIntyre RS, Guerrero A, et al. Prevalence of burnout in medical and surgical residents:A meta-analysis. Int J Environ Res Public Health. 2019;16:1479. doi: 10.3390/ijerph16091479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fashner J, Espinoza A, Mainous Iii AG. COVID-19 disruption to family medicine residency curriculum:Results from a 2020 US programme directors survey. Fam Med Community Health. 2021;9:e001144. doi: 10.1136/fmch-2021-001144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aljuboori ZS, Young CC, Srinivasan VM, Kellogg RT, Quon JL, Alshareef MA, et al. Early effects of COVID-19 pandemic on neurosurgical training in the United States:A case volume analysis of 8 programs. World Neurosurg. 2021;145:e202–8. doi: 10.1016/j.wneu.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aziz H, James T, Remulla D, Sher L, Genyk Y, Sullivan ME, et al. Effect of COVID-19 on surgical training across the United States:A national survey of general surgery residents. J Surg Educ. 2021;78:431–9. doi: 10.1016/j.jsurg.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khusid JA, Weinstein CS, Becerra AZ, Kashani M, Robins DJ, Fink LE, et al. Well-being and education of urology residents during the COVID-19 pandemic:Results of an American National survey. Int J Clin Pract. 2020;74:e13559. doi: 10.1111/ijcp.13559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Awadallah NS, Czaja AS, Fainstad T, McNulty MC, Jaiswal KR, Jones TS, et al. The impact of the COVID-19 pandemic on family medicine residency training. Fam Pract. 2021;38((Suppl 1)):i9–15. doi: 10.1093/fampra/cmab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alkhamees AA, Assiri H, Alharbi HY, Nasser A, Alkhamees MA. Burnout and depression among psychiatry residents during COVID-19 pandemic. Hum Resour Health. 2021;19:46. doi: 10.1186/s12960-021-00584-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zoorob D, Shah S, La Saevig D, Murphy C, Aouthmany S, Brickman K. Insight into resident burnout, mental wellness, and coping mechanisms early in the COVID-19 pandemic. PLoS One. 2021;16:e0250104. doi: 10.1371/journal.pone.0250104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cravero AL, Kim NJ, Feld LD, Berry K, Rabiee A, Bazarbashi N, et al. Impact of exposure to patients with COVID-19 on residents and fellows:An international survey of 1420 trainees. Postgrad Med J. 2021;97:706–15. doi: 10.1136/postgradmedj-2020-138789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen burnout inventory:A new tool for the assessment of burnout. Work Stress. 2005;19:192–207. [Google Scholar]
- 15.Thrush CR, Gathright MM, Atkinson T, Messias EL, Guise JB. Psychometric properties of the Copenhagen burnout inventory in an academic healthcare institution sample in the U. S. Eval Health Prof. 2021;44:400–5. doi: 10.1177/0163278720934165. [DOI] [PubMed] [Google Scholar]
- 16.ACGME Program requirements for Graduate Medical Education in Family Medicine [Google Scholar]
- 17.Steenland MW, Geiger CK, Chen L, Rokicki S, Gourevitch RA, Sinaiko AD, et al. Declines in contraceptive visits in the United States during the COVID-19 pandemic. Contraception. 2021;104:593–9. doi: 10.1016/j.contraception.2021.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The American College of Obstetricians and Gynecologists. How Program directors can support Obstetrics and Gynecology residents during the COVID-19 Pandemic. 2020. Available from: https://www.acog.org/news/news-articles/2020/05/how-program-directors-can-support-ob-gyn-residents-during-covid-19 .
- 19.Centers for Disease Control and Prevention. Responding to Coronavirus in Nursing Homes. Considerations for the public health response to COVID -19 in nursing homes. [[Last accessed on 2022 Apr 21]]. Available from https://www.hsdl.org/?view&did=837597 .
- 20.Gelineau-Morel R, Dilts J. Virtual education during COVID-19 and beyond. Pediatr Neurol. 2021;119:1–2. doi: 10.1016/j.pediatrneurol.2021.02.008. [DOI] [PubMed] [Google Scholar]
- 21.Singhi EK, Dupuis MM, Ross JA, Rieber AG, Bhadkamkar NA. Medical hematology/oncology fellows'perceptions of online medical education during the COVID-19 pandemic. J Cancer Educ. 2020;35:1034–40. doi: 10.1007/s13187-020-01863-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Accreditation Council for Graduate Medical Education. COVID-19: Frequently asked questions. [[Last accessed on 2021 Sep 21]]. Available from https://www.acgme.org/about-us/acgme-frequently-askedquestions/
- 23.Bitonti G, Palumbo AR, Gallo C, Rania E, Saccone G, De Vivo V, et al. Being an obstetrics and gynaecology resident during the COVID-19:Impact of the pandemic on the residency training program. Eur J Obstet Gynecol Reprod Biol. 2020;253:48–51. doi: 10.1016/j.ejogrb.2020.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taurines R, Radtke F, Romanos M, König S. Using real patients in e-learning:Case-based online training in child and adolescent psychiatry. GMS J Med Educ. 2020;37:Doc96. doi: 10.3205/zma001389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zuo L, Dillman D, Miller JuvéA. Learning at home during COVID-19:A multi-institutional virtual learning collaboration. Med Educ. 2020;54:664–5. doi: 10.1111/medu.14194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guo T, Kiong KL, Yao CMKL, Windon M, Zebda D, Jozaghi Y, et al. Impact of the COVID-19 pandemic on Otolaryngology trainee education. Head Neck. 2020;42:2782–90. doi: 10.1002/hed.26368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.West CP, Dyrbye LN, Shanafelt TD. Physician burnout:Contributors, consequences and solutions. J Intern Med. 2018;283:516–29. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 28.Woodside JR, Miller MN, Floyd MR, McGowen KR, Pfortmiller DT. Observations on burnout in family medicine and psychiatry residents. Acad Psychiatry. 2008;32:13–9. doi: 10.1176/appi.ap.32.1.13. [DOI] [PubMed] [Google Scholar]
- 29.Lebensohn P, Dodds S, Benn R, Brooks AJ, Birch M, Cook P, et al. Resident wellness behaviors:Relationship to stress, depression, and burnout. Fam Med. 2013;45:541–9. [PubMed] [Google Scholar]
- 30.Rutherford K, Oda J. Family medicine residency training and burnout:A qualitative study. Can Med Educ J. 2014;5:e13–23. [PMC free article] [PubMed] [Google Scholar]
- 31.He K, Stolarski A, Whang E, Kristo G. Addressing general surgery residents'concerns in the early phase of the COVID-19 pandemic. J Surg Educ. 2020;77:735–8. doi: 10.1016/j.jsurg.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]



