ABSTRACT
Evidence-based health care is gaining prominence since the past many decades. The ultimate goal of evidence-based medicine is providing the best available treatment to patients. The boom in pharmacy sector has seen a rapid rise in randomised controlled clinical trials. Novel medicines or diagnostic tests must be tested before introducing to the target population. Randomised controlled trials are at the top hierarchy of evidence-based health care, especially for testing newly invented drugs. The results obtained from randomised controlled trials cannot be generalised to the entire population. This has led to the evolvement of multi-centre trials in evidence-based research. Multi-centre trials can overcome the barriers associated with single-centre clinical trials. The conduct of multi-centre trials is still in a budding stage in India. Although there are many ongoing multi-centre trials in India, very few trials are conducted among the dental fraternity. The conduct of such trials has its own set of challenges involving funding, ethical committee approval, and logistic requirements. This paper will discuss the growth of multi-centre research, steps involved in conduct of multi-centre trials, and the challenges faced in conducting these trials by the dental specialists in India.
Keywords: Collaborative research, evidence-based medicine, funding agencies, multi-centric trials, randomised controlled clinical trials
Introduction
The cornerstone of evidence-based health care and prevention is large, multi-centre clinical research. The idea of evidence-based medicine (EBM) sparked a great deal of attention among medical professionals over the past few decades. EBM, as defined, is the process of making decisions about a patient’s medical care that incorporates clinical competence, the patient’s values, and the best available evidence. Randomised clinical trials (RCTs) are at the top of hierarchy of EBM. The gold standard for assessing the effectiveness of health care interventions is large, well-designed, and well-implemented RCTs (therapy or prevention). RCTs are the most effective strategy to pinpoint causal links and establish efficacy (define categorically which treatment modalities are superior). They have an advantage over all other study designs in that they are less susceptible to bias from both known and unidentified variables. RCTs face their own sets of challenges. In addition to internal validity, which measures how likely it is that a study’s planning and execution prevented bias or systematic error, external validity, which is defined as the degree to which results can be extrapolated to situations outside of study populations, is one of the most important aspects of research. The results obtained from RCTs are prone to biases and methodological mistakes, which could produce contradictory or inconclusive findings. This has paved the way for collaborative research.[1,2]
Alexander Graham Bell, in his quote “Great discoveries and improvements invariably involve the co-operation of many minds”, emphasises the importance of collaborative research. Over the past several years, collaborations in biological and health research have gathered significant impetus. It provides an excellent opportunity to communicate important findings for the nation and actively involves researchers, communities, and/or policymakers throughout the study process. Researchers can work more frequently with peers who have the resources and/or knowledge necessary to complete a particular research project. This could be multi-centric, involving public and/or private research centres and agencies, as well as inter- departmental, inter-institutional, or international collaboration.[2]
Collaborations between multiple research centres provide opportunities to draw on a variety of scientific specialties to address significant research issues affecting larger demographic groupings. It is essential to conduct multi-site clinical trials to advance detection, diagnosis, and treatment as well as to provide trustworthy knowledge that can be applied to large integrated populations and health care systems.[3]
“Clinical trials are defined as research in which a therapeutic, preventive, or diagnostic intervention is tested”. They are research studies that are intended to adhere to high scientific criteria to assure patient safety and yield valid study results because they are a technique of addressing unresolved concerns regarding novel treatments (drugs or devices) or treatment regimens”.[1]
Search Strategy
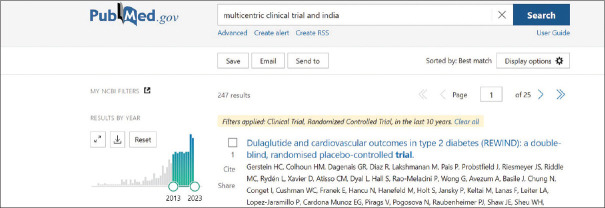
An electronic search was performed in the PubMed [Figure 1] database to search for the multi-centric clinical trials (MCCTs) in India conducted during the past 10 years. The keywords used were “Multicentre clinical trial” and “India”. The search resulted in 247 studies. Out of this, only 22 trials were conducted in India for medical trials and only three trials were conducted in the dental speciality. This is an alarming situation and requires introspection. The forthcoming sections will discuss the need for conducting MCCT, design structure for execution of MCCT, advantages, and the challenges faced by clinicians and academicians while conducting MCCT.
Figure 1.
Search strategy conducted for MCCT in India
Need for Clinical Trials
Any newly created medication, medical equipment, or treatment plan must not only be efficient in curing the identified disease condition but also be safe for usage in humans. All novel medicines are evaluated in “clinical trials” to determine their efficacy and safety.
The clinical trials are conducted in phases 1 to 4 to test the safety and efficacy of drugs. Among the different trial stages, phase 3 involves substantially larger trials with potentially thousands of individuals at multiple treatment facilities (hospitals). Such trials may compare a novel medication to the recommended course of therapy for a specific ailment, a different route of administration, a different dosage of the recommended medication, or both. These constitute the “Multicentric clinical trials”.[4,5]
Multi-Centre Clinical Trials Need of the Hour
Well planned single-centre studies are no doubt invaluable and have altered clinical practice, but there are some research problems that are best addressed with multi-centre studies. In particular, multi-centre research gives access to more people, and the findings are probably more applicable to a range of settings.[4,6]
Nursing, public health, community settings, and translational science research questions are particularly suited for multi-site trials. Predominantly, when the subject of study is a novel technology, process, treatment, or intervention, the medical research literature as a whole is sometimes described as having conflicting or inconclusive evidence. Systematic literature reviews and meta-analyses are conducted widely. However, this corpus of literature as a whole has a lot of results that are ambiguous, inconclusive, and conflicting. Findings from multi-site studies are more likely to give evidence to transform clinical practice and influence policy because of the advantages of scientific rigour, reproducibility, and design.[7]
Studies aiming to learn about various experiences, estimate treatment by site interaction effects, and investigate various care or service delivery structures benefit from multi-site trials. If the expected differences between the groups are minimal, large sample sizes are required. A higher sample size may provide sufficient power to investigate differences in pre-planned sub-groups of patients in situations when those patients’ responses or behaviours may vary.[3,4,7]
Shift from Global to Indian Scenario
Clinical trials were typically performed in the developed western nations, which served as the headquarters of the major multi-national pharmaceutical companies until the post-World Trade Organisation (WTO) era.
In the past decade, the clinical trials sector has experienced a tremendous growth, and India has become one of the top international locations for clinical trials. The major driving force was WTO’s modification of the intellectual property laws, and the key ideological basis for the expansion of the clinical trial sector in India is profit maximisation over any philanthropic goals.[7]
Over the years, there has been a profound change in conduct of clinical trials. Clinical trials were primarily conducted in academic medical institutions in the initial stages. However, as the pharma industry grew and new drug molecules were discovered, a need arose to enrol an ever-increasing number of patients with a wider range of diseases in order to test these molecules. Academic medical centres by themselves were unable to meet this demand. Subsequently, Clinical/Contract Research Organizations (CROs) emerged to fill the need. More than 3000 multi-centre research studies are performed globally.[8] In India, especially in the dental fraternity, very few dental multi-centre studies have been performed and published.
Types of Multi-centre Clinical Research
There are two main types of multi-centre research conducted in the research settings:
Collaborative group research, which is based on researchers who frequently interact with one another and is conducted at a small number of research sites.
Large-scale investigator-led research, which is conducted at a large number of research sites under the direction of a central group of investigators.[9]
Design Characteristics of an MCCT
MCCT is conducted in three phases, namely, pre-planning, planning, and execution. The following steps should be performed while executing a multi-centre trial.
a. Pre-Planning Phase
Research Question
The first step is the formulation of a research question which will dictate future decisions on research design. Literature search, by performing systematic literature reviews and meta-analyses, and attending conferences to understand current issues can help to comprehend the current state of evidence.[10]
Pilot Studies
Pilot studies are smaller-scale research studies carried out to improve the methodical conduct of subsequent related investigations. There are two different kinds of pilot studies: internal and external. Typically, these studies are conducted at a smaller scale than the larger scale study that is intended. In contrast to internal pilot studies, external pilot studies operate independent of the intended larger-scale study. Before investing and funding in the entire experiment, many granting organisations need this documentation demonstrating the study’s viability and error margins. The objective is to provide more precise sample size calculations and time predictions for the study’s completion.[11]
b. Planning Phase
Planning Grants
It is expensive and time-consuming to plan an MCCT because there are numerous centres involved. Indian Council of Medical Research (ICMR), Department of Science and Technology, and various other organisations in India announce grants especially intended to support the planning stage of an MCCT. These grants are intended to help researchers get ready for a phase III clinical trial (effectiveness study) which would eventually result in the submission of grant application to fund an MCCT.
Research teams are developed, new collaborative centres are hired, and each institution receives institutional review board permission protocols, study designs, and the manual of operating procedures (MOP). The purpose of the MOP is to promote consistency among investigators in data collecting across trial sites and protocol execution. The Institutional Examine Board and Data Safety Monitoring Board must review this document, which is created during the planning stage.[9]
Protocol Development
The collaborative research teams pool their collective experience to give the study protocol’s design due consideration. The protocol must be simple and clearly written.[9]
Co-ordinating centre
This is led by a co-ordinating Principal Investigator (PI). Depending on the study, the coordinating centre team may consist of one or two clinicians who are not involved in its execution, a statistician, an epidemiologist, a pharmacologist, and a representative of the organisation that requested the trial. There should be adequate amenities including secretarial services, calculation tools, and phone lines that are simple to use. Functions of co-ordinating centres include protocol development and consultation with interested parties. They have to schedule initial meetings and equally distribute credits among participants. They have to set up the randomisation process, package trial-specific items, and educate the participant about trial. The collected data have to be centralised. They have to supervise the protocol adherence and follow the time lines. They have to verify the individual observations, monitor serious adverse reactions, and exclude a participating centre because of a dearth of solid data.[10,11,12,13]
Each centre can have one PI and several CO-PIs. The PI is the person who takes an overall responsibility for the conduct of multi-centre research at his participating centre.
Ethical Committee (EC) – The Participating Centre ECs in multi-centre research are located at the participating centres. They should ensure respect of participants and communities, incorporate changes in informed consent documents, with translations in local language if necessary, and monitor research as per local requirements of their respective centres.[14,15]
Collaborator meetings and discussions – These are focused on solving problems. Face-to-face meetings between the collaborators are an important and successful team building activity that is required to make this kind of progress.[9,10,11,12,13,14,15,16]
c. Initiation of the investigation, the execution phase
The successful submission of research grant marks the beginning of the execution phase.
Sampling and sample size estimation – This involves appropriate block randomisation and use of balanced treatment allocation.[17]
These rigorous methodological steps are indispensable in the planning and conducting of an MCCT.
Advantages of MCCT
A large number of participants can be recruited in a shorter time frame, which would improve the outcomes of the study’s generalisability and external validity. Multi-site studies improve generalisability by allowing subject recruitment from a larger geographic area and improve research fidelity. Large sample sizes make it possible for studies to have enough power to identify differences between study groups that are clinically relevant. This is crucial when the intended outcomes such as death or disability are rare but substantial. The ability for future research will be increased by networking, communication, the necessity of joint research training, and the exchange of resources such as research templates to set up and conduct a multi-centre study. The inclusion of more centres and number of researchers can contribute to creating a solid foundation of skilled and knowledgeable researchers. Funding organisations seeking the best return on their investment are drawn to the advantages of capacity building. Multi-centre research can be used to standardise and enhance clinical care at various locations for a particular condition and continue the best practice long after the research programme has ended at participating sites and by clinical staff.[5,6,7,8,9]
Challenges in MSCCT
The pharmaceutical industry in India has experienced incredible growth, and numerous avenues for multi-centre research are emerging. Despite the fact that MSCCT has several benefits, conducting the trials presents numerous difficulties for the researchers. There are various obstacles to increasing the number of research locations because of India’s fragmented health-care system.[7,18] An ayurvedic multi-centric trial with USA on rheumatoid arthritis was recently announced by AYUSH. In India, very few MSCCTs, particularly those involving dentistry, are being undertaken. Various challenges experienced by researchers are discussed in the following paragraphs.
The main issue dental academicians face is a lack of funding from governmental organisations. Although numerous organisations offer funding, the dental community has relatively few opportunities because of a lack of clearly defined research questions (according to govt proposals) and a limited amount of funding provided to private institutions. A significant obstacle in conducting multi-centre research is a lack of adequate infrastructure. To account for variations and the inherent complexity of sampling, sophisticated statistical techniques are frequently required. Putting procedures into practice can be difficult because of the implications for data integrity, communication, dependability, and cost. The lack of consistency in clinical practices, institutional traditions and routines of care, and varying clinical privileges for research workers may make it challenging to standardise across sites. It may be difficult to hire and train project workers at each location. Competition from other studies and progressive departures from the intervention protocol can occur.[19]
Telecommunication expenditures between and across sites must be properly anticipated and included in the research budget. Maintaining the study’s internal validity and getting all sites to stay committed and work together during the study time are the key concerns. Sufficient staff is required to maintain protocol compliance and communication, solve issues, and guarantee that recruiting rates are maintained when managing several sites. Data cleansing, entry, and searches need greater effort and complexity.[20]
Communication with locations might be challenging to arrange because of probable time zone differences, language barriers, and varying cultural expectations. At each study site, project approval from the participating ethics committee is necessary. This has typically involved submitting an application to the committee at each site. Nevertheless, regional agreements for multi-site ethical approval are starting to help with this effort and lighten the burden. A letter of agreement must be signed between the PECs and DECs deciding the common protocol and review methodologies. Good clinical practice and ICMR 2019 guidelines should be adhered.[4,19]
A skilled clinical trial unit and trial manager are needed to coordinate the governance and administrative requirements for a large trial. The PI must also be able to oversee the protocol’s content and guarantee that all investigators follow the study’s methodology. The co-ordinating centre manager and the PI must view the trial through the perspective of the local investigators at each trial site because it is obviously impossible for all trial participants to be involved in directing the research.[20,21]
Financial considerations are always important to address, given the substantial resources, time and effort required to plan an MCCT. Some cost-cutting measures include choosing a geographic area centrally positioned as a mid-point for all collaborating centres, thereby reducing travel and time costs. The ownership of resources and data, intellectual property rights (IPRs), joint publications, management of research findings and conflicts of interest, and research outputs with commercial potential are matters of concern. Maintaining group commitment is important to carry out a productive MCCT investigation and sustaining the effort. Strategies that maintain group commitment include continuous communication and preparatory activities such as getting early IRB approvals and pilot testing data forms and outcome measures to assess centre readiness and maintain commitment while awaiting appropriate funding.[21,22]
Conclusion
Multi-centre research involves complexity and challenges that are not present in single-centre investigations. However, thorough preparation and execution will increase the likelihood of a successful outcome. The academic genius of the research hypothesis is significantly less critical to the success of a multi-centre trial than sustained leadership, inter-personal skills, communication, and determination. There will be a sense of accomplishment and teamwork as well as the creation of linkages and infrastructure for future research projects.
Clinical trials have come under close examination in India over the past 10 years. The media frequently portrays trials as a for-profit venture rather than a scientific effort to address issues of public health. The conversation must shift to assisting the public in making educated decisions about trial participation. It is admirable that the ICMR has established a nationwide network of clinical trial sites in this regard. The Government should bring out proposals targeted at the dental community, particularly to private institutions where researchers struggle to find funding and a suitable infrastructure to carry out multi-centre research.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Szajewska H. Evidence-based medicine and clinical research:Both are needed, neither is perfect. Ann Nutr Metab. 2018;72:13–23. doi: 10.1159/000487375. [DOI] [PubMed] [Google Scholar]
- 2.Masic I, Miokovic M, Muhamedagic B. Evidence based medicine - new approaches and challenges. Acta Inform Med. 2008;16:219–25. doi: 10.5455/aim.2008.16.219-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Draft ICMR Guidelines for Common Ethics Review of Multicentre Research 2019 [Google Scholar]
- 4.Thiers FA, Sinskey AJ, Berndt ER. Trends in the globalization of clinical trials. Nat Rev Drug Discov. 2008;7:13–4. [Google Scholar]
- 5.Gupta YK, Padhy BM. India's growing participation in global clinical trials. Trends Pharmacol Sci. 2011;32:327–9. doi: 10.1016/j.tips.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 6.Bajpai V. Rise of clinical trials industry in India:An analysis. ISRN Public Health. 2013;2013:17. doi:10.1155/2013/167059. [Google Scholar]
- 7.Nundy S, Gulhati CM. A new colonialism?Conducting clinical trials in India. N Engl J Med. 2005;352:1633–6. doi: 10.1056/NEJMp048361. [DOI] [PubMed] [Google Scholar]
- 8.Maiti R, M R. Clinical trials in India. Pharmacol Res. 2007;56:1–10. doi: 10.1016/j.phrs.2007.02.004. doi:10.1016/j.phrs. 2007.02.004. [DOI] [PubMed] [Google Scholar]
- 9.Chung KC, Song JW WRIST Study Group. A guide to organizing a multicentre clinical trial. Plast Reconstr Surg. 2010;126:515–23. doi: 10.1097/PRS.0b013e3181df64fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burns PB, Chung KC. Developing good clinical questions and finding the best evidence to answer those questions. Plast Reconstr Surg. 2010;126:613–8. doi: 10.1097/PRS.0b013e3181de24a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung KC, Song JW WRIST Study Group. A guide to organizing a multicentre clinical trial. Plast Reconstr Surg. 2010;126:515–23. doi: 10.1097/PRS.0b013e3181df64fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neugebauer EA. Development of a consensus-assisted protocol--a new approach to improve study design. Eur J Surg Suppl. 1999:7–11. doi: 10.1080/11024159950188475. doi:10.1080/11024159950188475. [DOI] [PubMed] [Google Scholar]
- 13.Commiskey P, Armstrong AW, Coker TR, Dorsey ER, Fortney JC, Gaines KJ, et al. A blueprint for the conduct of large, multisite trials in telemedicine. J Med Internet Res. 2021;23:e29511. doi: 10.2196/29511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ibia E, Binkowitz B, Saillot JL, Talerico S, Koerner C, Ferreira I, et al. Ethical considerations in industry-sponsored multiregional clinical trials. Pharm Stat. 2010;9:230–41. doi: 10.1002/pst.458. [DOI] [PubMed] [Google Scholar]
- 15.Rathi S, Kalantri SP. Ethics of clinical research and practice in India during the Covid-19 pandemic. Indian J Med Ethics. 2020;5:175–80. doi: 10.20529/IJME.2020.080. [DOI] [PubMed] [Google Scholar]
- 16.Stiell IG, Perry JJ, Brehaut J, Brown E, Curran JA, Emond M, et al. How to conduct implementation trials and multicentre studies in the emergency department. CJEM. 2018;20:448–452. doi: 10.1017/cem.2017.433. [DOI] [PubMed] [Google Scholar]
- 17.Harden M, Friede T. Sample size calculation in multi-centre clinical trials. BMC Med Res Methodol. 2018;29(18):156. doi: 10.1186/s12874-018-0602-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith L, Tan A, Stephens JD, Hibler D, Duffy SA. Overcoming challenges in multisite trials. Nurs Res. 2019;68:227–36. doi: 10.1097/NNR.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 19.Cook D, Brower R, Cooper J, Brochard L, Vincent JL. Multicentre clinical research in adult critical care. Crit Care Med. 2002;30:1636–43. doi: 10.1097/00003246-200207000-00039. [DOI] [PubMed] [Google Scholar]
- 20.Broder HL, Crerand CE, Ruff RR, Peshansky A, Sarwer DB, Sischo L. Challenges in conducting multicentre, multidisciplinary, longitudinal studies in children with chronic conditions. Community Dent Oral Epidemiol. 2017;45:317–22. doi: 10.1111/cdoe.12293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hagen NA, Stiles CR, Biondo PD, Cummings GG, Fainsinger RL, Moulin DE, et al. Establishing a multicentre clinical research network:Lessons learned. Curr Oncol. 2011;18:e243–9. doi: 10.3747/co.v18i5.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Irving SY, Curley MAQ. Challenges to conducting multicenter clinical research ten points to consider. AACN Adv Crit Care. 2008;19:164–9. doi: 10.1097/01.AACN.0000318119.67061.0f. [DOI] [PubMed] [Google Scholar]