Abstract
Summary
A 55-year-old patient was admitted to our department for the management of a repetitive alteration of consciousness. Biological investigation results were consistent with endogenous hyperinsulinemic hypoglycemia. Insulinoma was therefore suspected. Abdominal computed tomography and endoscopic ultrasound showed no obvious pancreatic mass.Somatostatin receptor scintigraphy showed abnormal radioactive uptake in both the pancreatic tail and the uncinate process. Contrariwise, abdominal magnetic resonance imaging showed a unique lesion in the pancreas tail. The patient was then proposed for pancreatic surgery. Both intraoperative manual palpation and intraoperative ultrasonography of the pancreas showed a single corporal lesion of 1.5 cm. No lesion was found in the uncinate process. After a left pancreatectomy, the lesion was histopathologically confirmed to be a well-differentiated neuroendocrine tumor. The symptoms of the patient resolved almost immediately following the surgery. The follow-up is one and a half years to date.
Learning points
The exact preoperative localization of the pancreatic mass remains the most challenging part of insulinoma diagnostic workup.
The radiologist’s experience is the best warrantor to a precise localization of the tumor.
111In-DTPA-octreotide uptake in the pancreatic uncinate process may be physiological and its interpretation must, therefore, be vigilant.
Manual palpation along with intraoperative ultrasonography is considered as the most effective method for the localization of insulinomas during open surgery.
Patient Demographics: Adult, Female, Other, Tunisia
Clinical Overview: Pancreas, Tumours and neoplasia
Publication Details: Unique/unexpected symptoms or presentations of a disease, May, 2023
Background
Insulinoma is the most common pancreatic neuroendocrine tumor. It is usually a benign, solitary lesion with a low incidence (1). Unprovoked episodic hypoglycemia is the main feature of the disease, reflecting the intermittent secretion of insulin.
Complete surgical removal of the tumor is the only curative treatment. This treatment is usually delayed considering the localization difficulties of the functioning lesion.
Here, we present a case of an insulinoma with confusing imaging in a Tunisian female patient. This case demonstrates the diagnostic challenges of small pancreatic lesions leading to delay of the curative treatment.
Case presentation
A 55-year-old woman presented in February 2020 with acute confusion and asthenia. She was found to be hypoglycemic (blood glucose: 2.2 mmol/L) and was given intravenous glucose with complete resolution of her symptoms.
The patient started to have episodic confusion two years prior. During these episodes, she was nonresponsive, asthenic and had speech difficulties and palpitations. These attacks occurred twice a month. Her clinical manifestations subsided after the consumption of carbohydrates. Thus, Whipple’s triad criteria are fulfilled.
She had neither previous psychological history nor diabetes. She had no notable family history either.
The patient was then admitted to our Endocrinology department and was further investigated for hypoglycemia. The general physical examination was within normal limits.
Investigation
Her baseline blood results were all within normal ranges. After excluding an adrenal insufficiency, a fasting test was performed. The biological results at the end of the test were consistent with endogenous hyperinsulinemic hypoglycemia and, according to existing guidelines, fulfilled the diagnostic criteria for an insulinoma (2) (Table 1). Screening for insulin antibodies and circulating sulfonylurea were not practiced in our case, due to their unavailability in our hospital.
Table 1.
Confirmation of endogenous hyperinsulinism in our patient.
| Values | End of fasting test (February 2020) | Spontaneous hypoglycemia (March 2021) | Criteria for insulinoma (3) |
|---|---|---|---|
| Glucose (mmol/L) | 2.2 | 1.37 | <2.47 |
| C-peptide (nmol/L) | 0.82 | 1.04 | ≥0.19 |
| Insulin (mU/L) | 71.52 | 218.75 | ≥20.83 |
| β-hydroxybutyrate (mmol/L) | - | - | ≤2.7 |
Her history and laboratory results were incompatible with multiple endocrine neoplasia type 1.
Abdominal computed tomography (CT) scan and endoscopic ultrasound did not detect any obvious pancreatic mass. The patient was planned for further radiological investigations but lost to follow-up due to the COVID-19 pandemic.
The patient was readmitted a year later (March 2021) to our department due to recurrent severe episodes of hypoglycemia for 2 months requiring continuous administration of rapidly absorbed carbohydrates.
Upon admission, the patient had a body mass index of 31.2 kg/m2. Over the past year, she gained 12 kg. Otherwise, her physical examination was normal.
Endogenous hyperinsulinism was noted simultaneously with spontaneous hypoglycemia as shown in Table 1. A complementary somatostatin receptor scintigraphy (SRS) was performed (Fig. 1) and the presence of two pancreatic lesions was detected: one in the pancreatic tail and the other in the uncinate.
Figure 1.
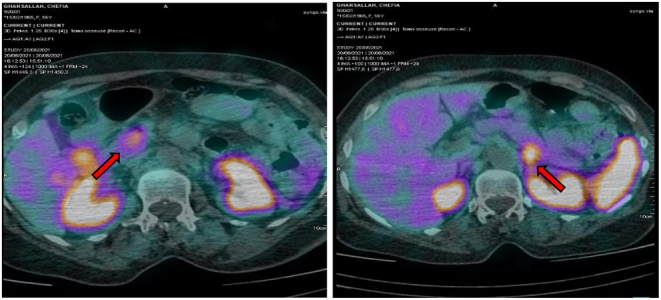
SRS featuring two pancreatic lesions (arrow).
Contrarily, an abdominal magnetic resonance imaging (MRI) showed a unique mass in the pancreas tail (Fig. 2).
Figure 2.
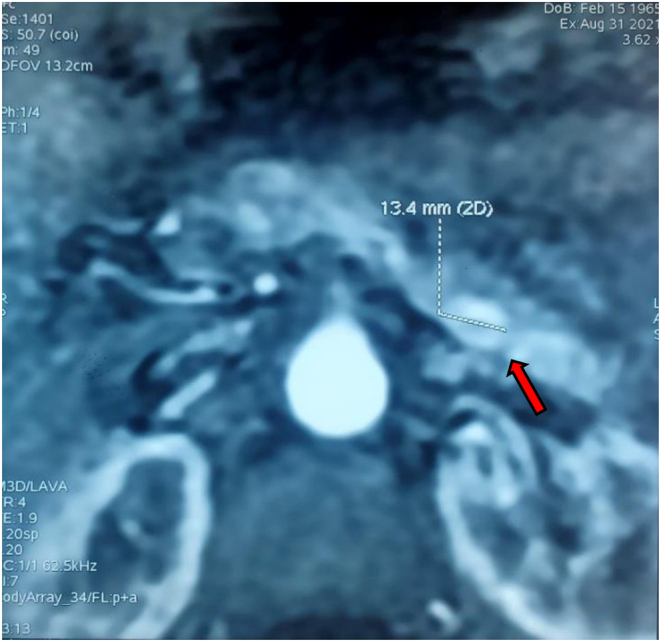
MRI findings revealing a unique pancreatic lesion.
Treatment
The patient was then proposed for pancreatic surgery. Both intraoperative manual palpation and intraoperative ultrasonography (IOUS) of the pancreas (Fig. 3) showed a single corporal lesion of 1.5 cm. No lesion was found in the uncinate process.
Figure 3.
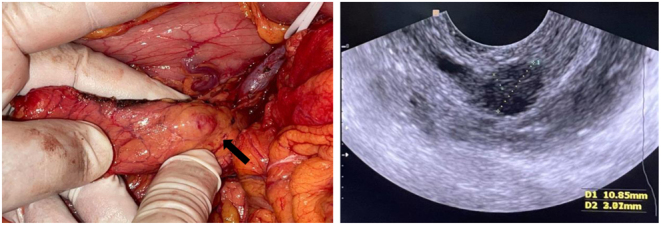
Left: Intraoperative photo of the insulinoma. Right: intraoperative ultrasonography of the pancreas showing a corporal mass.
After a left pancreatectomy, the lesion was histopathologically confirmed to be a well-differentiated neuroendocrine tumor.
Outcome and follow-up
The symptoms of the patient resolved almost immediately following the surgery. The follow-up is one and a half years to date with considerable improvement in her life quality and no recurrent episodes of hypoglycemia.
Discussion
Insulinoma is usually a solitary and slow-growing tumor causing non-specific symptoms. Typical Whipple’s triad with endogenous hyperinsulinemic hypoglycemia is suggestive of its diagnosis. The exact preoperative localization of the pancreatic mass remains the most challenging part of insulinoma diagnostic workup and may require multiple imaging techniques. The radiological investigation was indeed the most challenging part of our case. The first line of this investigation includes CT and MRI, which localize up to 80% of lesions (3). The sensitivity of contrast CT and MRI has been reported to range between 33 to 64% and 40 to 90%, respectively (4). The variability is dependent on tumor size, type of machine, protocols used, and the expertise of radiologists. Mostly (over 90%) the diameter of tumors is less than 2 cm, making it very difficult to accurately localize using MRI and CT prior to surgical excision. This may explain the absence in our case of a pancreatic lesion on CT in 2020 when the tumor was most probably of smaller size. Regarding its higher sensitivity in insulinoma detection (94%) (5), thin-section multidetector CT should be used in order to efficiently detect pancreatic lesions (6). Second-line investigations include endoscopic ultrasonography. This invasive technique has a sensitivity of 95% in the hands of skilled operators. It is considered as the study of choice if the non-invasive imaging modalities yield negative results (7). Nevertheless, it is limited by its poor evaluation of distal pancreatic lesions with a detection rate of 37–60% (8). Regarding its high sensitivity in the detection of pancreatic corporal lesions, the negativity of endoscopic ultrasonography in our case could be explained by the lack of experience of the endoscopist. When morphologic imaging is negative, SRS may be performed (9). It is positive in only 50% of cases due to the low density of somatostatin receptor subtypes 2 and 5 (7). Moreover, SRS may give misleading results. Intense physiological 111In-DTPA-octreotide uptake of the pancreatic uncinate process can occur in 17% of cases on SPECT-CT acquisitions. Given this high rate of false positives, the use of SRS is to be discouraged when investigating hyperinsulimic hypoglycemia. This tracer accumulation in the pancreatic uncinate process should be therefore correlated with morphologic examinations, such as CT, MRI, or somatostatin PET-CT if available (10). Our experience highlights that 111In-DTPA-octreotide uptake in the pancreatic uncinate process may be physiological and its interpretation must, therefore, be vigilant. The scintigraphic suspicion should consequently be confirmed before surgery. Manual palpation along with IOUS is considered the most effective method for the localization of tumors during open surgery. Laparoscopic ultrasonography combines the best features of laparoscopic exploration and intraoperative ultrasonography resulting in a sensitivity of 96.9% (11). Hence, it is considered the most accurate method for detecting insulinomas. However, with the implementation of modern localization strategies, the rate of blind pancreatic exploration has dropped significantly over the last decade (12). IOUS was indeed the most accurate localizing technique in our case and led subsequently to a successful distal pancreatectomy.
Declaration of interest
There is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported
Funding
This study did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Patient consent
Written informed consent for publication of their clinical details and clinical images was obtained from the patient.
Author contribution statement
F Mnif provided the idea of the case report and patient enrolment. W Belabed drafted the manuscript. A M Missaoui, M Elleuch , F Hadjkacem, N Rekik, M Mnif, N Charfi, and D Ben Salah were involved in patient enrolment and revising of the manuscript. A Mohammed approved the manuscript.
References
- 1.Öberg K. Management of functional neuroendocrine tumors of the pancreas. Gland Surgery 2018720–27. ( 10.21037/gs.2017.10.08) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cryer PE, Axelrod L, Grossman AB, Heller SR, Montori VM, Seaquist ER, Service FJ. & Endocrine Society. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline. Journal of Clinical Endocrinology and Metabolism 200994709–728. ( 10.1210/jc.2008-1410) [DOI] [PubMed] [Google Scholar]
- 3.Wei J Liu X Wu J Xu W Gao W Jiang K Zhang Z & Miao Y. Diagnosis and surgical management of insulinomas in 33 consecutive patients at a single institution. Langenbeck’s Archives of Surgery 20164011019–1025. ( 10.1007/s00423-016-1496-y) [DOI] [PubMed] [Google Scholar]
- 4.Sotoudehmanesh R Hedayat A Shirazian N Shahraeeni S Ainechi S Zeinali F & Kolahdoozan S. Endoscopic ultrasonography (EUS) in the localization of insulinoma. Endocrine 200731238–241. ( 10.1007/s12020-007-0045-4) [DOI] [PubMed] [Google Scholar]
- 5.Gouya H Vignaux O Augui J Dousset B Palazzo L Louvel A Chaussade S & Legmann P. CT, endoscopic sonography, and a combined protocol for preoperative evaluation of pancreatic insulinomas. American Journal of Roentgenology 2003181987–992. ( 10.2214/ajr.181.4.1810987) [DOI] [PubMed] [Google Scholar]
- 6.Giannis D Moris D Karachaliou GS Tsilimigras DI Karaolanis G Papalampros A & Felekouras E. Insulinomas: from diagnosis to treatment. A review of the literature. Journal of BUON 2020251302–1314. [PubMed] [Google Scholar]
- 7.Jensen RT, Cadiot G, Brandi ML, de Herder WW, Kaltsas G, Komminoth P, Scoazec JY, Salazar R, Sauvanet A, Kianmanesh R, et al. Enets Consensus Guidelines for the management of patients with digestive neuroendocrine neoplasms: functional pancreatic endocrine tumor syndromes. Neuroendocrinology 20129598–119. ( 10.1159/000335591) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tucker ON Crotty PL & Conlon KC. The management of insulinoma. British Journal of Surgery 200693264–275. ( 10.1002/bjs.5280) [DOI] [PubMed] [Google Scholar]
- 9.Taieb D, Legmann P, Prat F, Chevallier P, Tenenbaum F. & French Endocrine Society. Topographic diagnosis: respective roles of morphological and functional imaging. Annales d'Endocrinologie 201374185–190. ( 10.1016/j.ando.2013.05.008) [DOI] [PubMed] [Google Scholar]
- 10.Schwartz P Ceyrat Q Hindié E Fernandez P Bordenave L & Pinaquy J-B. Fréquence de la fixation physiologique de l’uncus pancréatique en scintigraphie à l’111In-pentétréotide: étude rétrospective chez 198 patients. Médecine Nucléaire 201741405–414. ( 10.1016/j.mednuc.2017.06.013) [DOI] [Google Scholar]
- 11.Wu M Wang H Zhang X Gao F Liu P Yu B Qiu H Huang G & Tan X. Efficacy of laparoscopic ultrasonography in laparoscopic resection of insulinoma. Endoscopic Ultrasound 20176149–155. ( 10.4103/2303-9027.194703) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Placzkowski KA Vella A Thompson GB Grant CS Reading CC Charboneau JW Andrews JC Lloyd RV & Service FJ. Secular trends in the presentation and management of functioning insulinoma at the Mayo Clinic, 1987–2007. Journal of Clinical Endocrinology and Metabolism 2009941069–1073. ( 10.1210/jc.2008-2031) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a