Background:
Late development of forefoot ulcers is a common finding after transmetatarsal amputation (TMA). The primary aim of this study was to examine whether concomitant prophylactic Achilles tendon lengthening (ATL) was associated with a reduction in the incidence of forefoot ulcers postoperatively.
Methods:
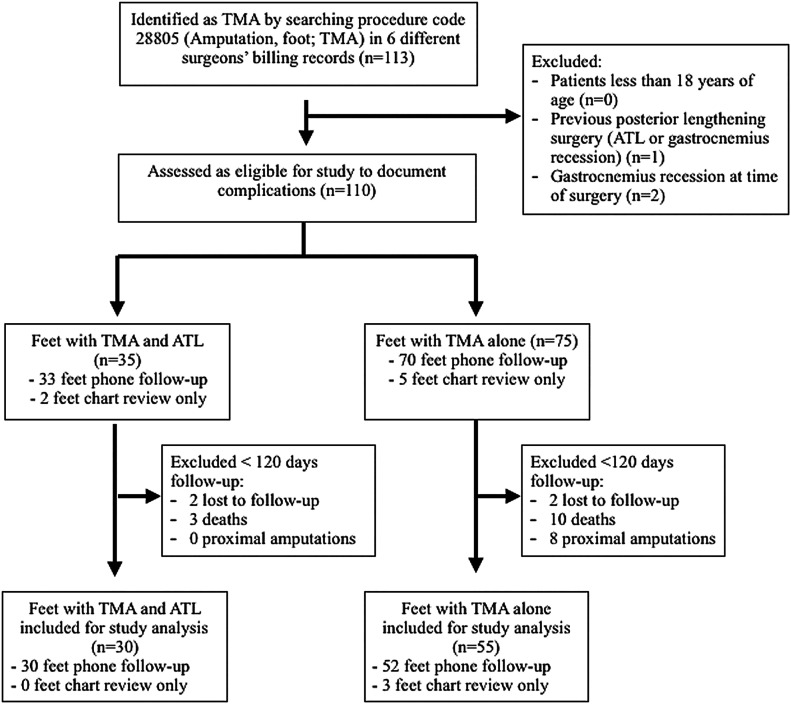
A retrospective chart review was performed by 2 authors to identify patients who underwent TMA over a period of 5.5 years from January 1, 2015, through July 31, 2020. They identified 110 feet in 107 patients; the 83 patients (85 feet) who had ≥120 days of follow-up were used for the study. Follow-up was performed with telephone calls (80 patients) or during the last office visit (3 patients). Those who were contacted by telephone were asked if they developed an ulcer after healing from the original surgery. Mean follow-up time was 672 ± 258 days for the 30 feet with concomitant Achilles lengthening and 663 ± 434 days for the 55 feet without Achilles lengthening. Demographic data were analyzed for association with late development of forefoot ulceration.
Results:
Eighty-five feet were included in the analysis. Late forefoot ulcers developed in 35% of feet that had a TMA alone (n = 55) compared with 3% of feet who received a concomitant ATL (n = 30; p < 0.001); the 2 groups had similar mean follow-up times. Mean time to ulcer development was 587 ± 420 days in the 19 patients without Achilles lengthening. Of the patients who developed late forefoot ulcers, 47% also developed osteomyelitis, and 16% went on to proximal amputation. Patients who developed forefoot ulcers were younger (55 ± 12 versus 63 ± 11 years of age; p = 0.006) than those who did not.
Conclusions:
ATL at the time of TMA is associated with a reduction in the risk of later development of forefoot ulcers, especially in younger patients.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Achilles tendon lengthening (ATL) has been shown to reduce pressure at the forefoot. Armstrong et al. examined 10 patients who underwent ATL for plantar ulcerations of the forefoot1. Force-plate dynamic pressure at the forefoot during gait was reduced from 86 N/cm2 preoperatively to 63 N/cm2 at 8 weeks postoperatively. Mueller et al. found that patients maintained the increased dorsiflexion from the ATL at 7 months postoperatively. However, peak torque of the plantar flexor muscles and peak pressure at the forefoot returned to baseline2. Maluf et al. confirmed that ATL provided only temporary reduction in strength and forefoot pressures although the increased dorsiflexion range of motion was maintained3.
Nonetheless, ATL is the only operative preventative strategy for diabetic foot ulcers that is supported by Level-I evidence2. Mueller et al. performed a prospective randomized trial and found that ATL with total contact casting (TCC) was more effective at preventing recurrent forefoot ulcers than TCC alone. Of their patients, 81% in the TCC-alone group and 38% in the TCC plus ATL group had recurrent ulcers2. Multiple Level-III and IV studies have supported the use of ATL to prevent recurrent forefoot ulcers4-7.
Prophylactic ATL is often performed with transmetatarsal amputation (TMA), but, to our knowledge, there are no comparative studies to support its use for this indication8 (Figs. 1-A and 1-B). Many previous studies on TMA have noted a high rate of nonhealing at the amputation stump but have not reported the late development of ulcers8-10. Clinicians often see patients who develop late ulcers after TMA, but only 1 study has reported on late ulcerations, with an incidence of 18% within the first year11. In a review article, Attinger et al. noted a reduction in the rate of ulceration (from 50% to 4%) after TMA when using a prophylactic ATL or tendon transfer12. When used to treat forefoot ulcers that develop after TMA, the results from ATL have been variable. Barry et al. performed 33 ATL procedures for ulcers after TMA and noted a 91% healing rate with no recurrence at 2 years13, although La Fontaine et al. reported an ulcer recurrence rate of 36%14.
Our aim was to examine our experience with ATL as an adjunct to TMA in reducing the development of late forefoot ulceration that was thought to be related to a biomechanical cause. Our secondary aim was to identify demographic risk factors for late ulceration and complications associated with prophylactic ATL.
Materials and Methods
A retrospective chart review was performed by 2 authors (M.J.B and C.M.G.). They identified 110 feet in 107 patients who had undergone TMA by 6 different surgeons. Following application of the exclusion criteria, 85 feet in 83 patients were included in the study; of these, 30 feet had a simultaneous prophylactic ATL procedure (Fig. 2). The decision to perform ATL was made by the surgeon. No clinical measure of Achilles contracture was used. Subjects were identified by searching hospital or office billing records for the procedure code 28805 (Amputation, foot; transmetatarsal) for a period of 5.5 years from January 1, 2015, through July 31, 2020. In addition to a review of medical records, a brief 4-question survey was conducted over the telephone to identify the late development of forefoot ulcers. Patients who were contacted by telephone were asked if they had developed an ulcer. If so, they were asked about its location and whether it was caused by trauma, a burn, or pressure. They were also asked if the ulcer was painful.
Fig. 2.
STROBE (Strengthening the Reporting of Observational studies in Epidemiology) diagram describing the selection of the 2 study groups.
Figs. 1-A and 1-B TMA.
Fig. 1-A.
Fig. 1-A Equinus deformity at the 15-month follow-up in a patient who underwent TMA without ATL.
Fig. 1-B.
Fig. 1-B Increased dorsiflexion of the ankle joint is noted at the 6-month follow-up in a patient who underwent TMA with ATL.
If an ipsilateral forefoot ulcer, an ipsilateral proximal amputation, or a death occurred, the date of the complication was noted as the final follow-up date. The authors attempted to contact all of the patient telephone numbers in the hospital and physician office database (Fig. 2). Two patients in each treatment group with <120 days of follow-up could not be contacted by telephone and were lost to follow-up. Three patients who underwent TMA alone and had ≥120 days follow-up could not be contacted by telephone, and their last office visit was used for final follow-up data. Late forefoot ulcers were defined as plantar ulcers distal to the tarsometatarsal joint directly plantar to the residual metatarsal bones. Ulcers were considered “late” if they occurred on the forefoot after an office note had documented a healed TMA incision or if they occurred in a new plantar forefoot location (as described in writing or noted in postoperative photographs).
ATL procedures were performed according to surgeon preference. Some surgeons who routinely did not perform ATL surgery began to perform it more frequently during the study period. The decision to perform ATL did not require the presence of preoperative equinus.
Surgical Technique and Postoperative Protocol
First, the ATL procedure was performed while the infected wounds were covered. The ATL procedure was done with a percutaneous technique, with a triple hemisection using 2 medial and 1 lateral hemisection (Fig. 3). The postoperative protocol included non-weight-bearing with the leg in a posterior splint or cast for the first 4 weeks. Patients then walked with a fracture boot until 8 weeks postoperatively. One surgeon had 8 patients use a heel lift inside the fracture boot partway through the study period.
Fig. 3.
Incision planning for a percutaneous ATL procedure. Two medial incisions and 1 lateral incision spaced 2.5 cm apart were marked along the border of the Achilles tendon in order to avoid the sural nerve laterally while making the proximal incision. The ankle was passively dorsiflexed until the Achilles tendon was adequately lengthened.
Inclusion and Exclusion Criteria
Inclusion criteria included patients who were ≥18 years of age who had undergone a TMA during the study period. Exclusion criteria included patients with previous posterior lengthening (1 foot), any patient who underwent a gastrocnemius recession (2 feet), and patients with <120 days of follow-up (25 feet) (Fig. 2). One patient was staged for an ATL procedure within 2 months of TMA because the severity of the infection precluded a posterior splint; this patient was included in the TMA with ATL group.
Outcome Measures
The primary outcome was the development of plantar forefoot ulcers after surgery. This outcome was self-reported during the telephone interview or identified from the medical record review. A secondary outcome was the time after surgery that the ulcer developed. Eighteen ulcerations were identified at an office visit, and the date of the ulcer was recorded as the date documented in the subjective portion of the note, or as the date of the office visit if the date of ulceration had not been documented. Two ulcerations were identified during telephone follow-up, and the patients were asked when the ulceration had developed. Lastly, we attempted to identify an association between ulcer occurrence and demographic and medical comorbidities, including sex, diabetes, smoking, peripheral vascular disease, age, hemoglobin (Hb) A1c levels, renal function (with use of the CKD-EPI [Chronic Kidney Disease Epidemiology Collaboration] formula), body mass index (BMI), and level of TMA. The level of TMA was considered distal to the proximal metatarsal metaphyseal-diaphyseal junction if it was >2.5 cm distal to the first metatarsal-cuneiform joint. Complications were evaluated, including new posterior heel wounds, Achilles tendon rupture, proximal amputation, and death. Proximal amputations included any amputation proximal to the Lisfranc joint. Osteomyelitis or a proximal amputation that was a direct sequela of late forefoot ulceration was documented separately. Osteomyelitis was diagnosed by an indium-labeled white blood-cell scintigraphy in 3 patients and by magnetic resonance imaging in 16 patients.
Statistical Methods
This was a retrospective observational study that used a consecutive sample of patients who met our inclusion and exclusion criteria. The characteristics of the study groups were compared using univariate analyses. A parametric independent-samples t test was performed to examine the mean difference in ulceration rate between the 2 study groups. Homogeneity of variance was checked and verified. A Fisher exact test was performed to examine differences in the proportions of categorical variables between the 2 groups. Kaplan-Meier survival curves were used to compare the risk of late ulceration between the groups, with a log-rank test used to assess significance. Finally, a binary logistic regression model was performed using the development of forefoot ulceration after surgery as a categorical dependent variable. A 2-tailed p value of ≤0.05 was considered significant. SPSS software (version 26; IBM) was used to perform all of the analyses.
Source of Funding
No funding was provided for this investigation.
Results
Primary Outcome Measures
Fifty-five cases consisted of TMA alone, and 30 cases were TMA with a concomitant ATL (Table I). Of the cases that had a TMA alone, 19 (35%) went on to develop forefoot ulcerations, compared with only 1 case (3%) that had a TMA and a concomitant ATL procedure (p < 0.001), with similar follow-up times (mean and standard deviation, 663 ± 434 versus 672 ± 258 days). The mean time from surgery to ulcer development in feet without ATL was 587 days, with a range of 149 to 1,727 days and a large standard deviation of 420 days. No patients had forefoot ulcerations within the first 120 days. Based on the log-rank test comparing the 2 curves, patients who underwent TMA with ATL differed significantly in remaining ulcer-free at approximately 860 days. Those who underwent TMA with ATL had a 92% probability of remaining ulcer-free, while those who underwent TMA only had a 55% probability of remaining ulcer-free (p < 0.01) (Fig. 4). The patients of all 4 surgeons who performed ≥5 TMA-only procedures had a high incidence of late forefoot ulceration development, ranging from 13% to 40%.
Fig. 4.
Kaplan-Meier survival curve, with shading of the 95% confidence interval, showing the probability of remaining ulcer-free after TMA with and without ATL. No late ulcers had developed by 120 days after TMA; however, after that period of time, patients who underwent concomitant ATL were more likely to remain ulcer-free.
TABLE I.
Primary Outcomes and Complications
| TMA Alone | TMA with ATL | P Value | |
|---|---|---|---|
| Primary outcomes | |||
| No. of feet | 55 | 30 | |
| Neuropathic forefoot ulcer development | 19 (35%) | 1 (3%) | <0.001 |
| Time to ulceration* (days) | 587 ± 420 | 695 | 0.85 |
| Follow-up time* (days) | 663 ± 434 | 672 ± 258 | 0.91 |
| Complications | |||
| No. of feet | 75 | 35 | |
| Death | 21 (28%) | 4 (11%) | 0.02 |
| Achilles tendon rupture | 0 (0%) | 2 (6%) | 0.03 |
| Proximal amputation | 7 (9%) | 2 (6%) | 0.04 |
| New plantar heel ulceration | 0 (0%) | 1 (3%) | 0.14 |
| New posterior heel wound | 3 (4%) | 0 (0%) | 0.23 |
| Achilles tendon infection | 0 (0%) | 0 (0%) | 0.99 |
| Sequelae of late forefoot ulcerations | |||
| No. of feet | 19 | 1 | |
| Osteomyelitis caused by forefoot ulcer | 9 (47%) | 0 (0%) | 0.99 |
| Proximal amputation caused by forefoot ulcer | 3 (16%) | 0 (0%) | 0.99 |
The values are given as the mean and standard deviation.
Secondary Outcomes Measures
Demographics and Medical Comorbidities
Demographic variables were compared between patients who developed plantar forefoot ulcerations (n = 20) and those who did not (n = 65; Table II). Those with ulceration were younger (55 ± 12 versus 63 ± 11 years; p = 0.006). Interestingly, peripheral vascular disease was more prevalent in those without ulcerations (46%) when compared with those with ulcerations (20%; p = 0.04), although patients with peripheral vascular disease were also older (p = 0.006). Other variables such as sex, diabetes, HbA1c level, smoking, BMI, renal function, and amputation level were not associated with ulceration. BMI and HbA1c level showed a significant difference between the treatment groups, but age did not (Table III).
TABLE II.
Demographic Data According to Development of Ulceration
| Feet with Development of Forefoot Ulcers (N = 20) | Feet without Development of Forefoot Ulcers (N = 65) | P Value | |
|---|---|---|---|
| Age* (yr) | 55 ± 12 | 63 ± 11 | 0.006 |
| Peripheral vascular disease | 4 (20%) | 30 (46%) | 0.04 |
| Smoker | 3 (15%) | 2 (3%) | 0.08 |
| Male sex | 18 (90%) | 51 (79%) | 0.34 |
| Glomerular filtration rate* (mL/min/1.73 m2) | 69.3 ± 34.7 | 64.1 ± 32.0 | 0.55 |
| Body mass index* (kg/m2) | 32.6 ± 6.5 | 31.6 ± 7.3 | 0.56 |
| Distal metatarsal amputation level | 7 of 19 (37%) | 15 of 49 (31%) | 0.77 |
| Hemoglobin A1c* (%) | 8.7 ± 2.7 | 8.6 ± 2.4 | 0.85 |
| Diabetes | 19 (95%) | 62 (95%) | 0.99 |
The values are given as the mean and standard deviation.
TABLE III.
Patient Demographics
| TMA Alone (N = 55 Feet) | TMA with ATL (N = 30 Feet) | P Value | |
|---|---|---|---|
| Hemoglobin A1c* (%) | 8.2 ± 2.4 | 9.4 ± 2.4 | 0.02 |
| Body mass index* (kg/m2) | 32.9 ± 6.8 | 29.8 ± 7.4 | 0.05 |
| Distal metatarsal amputation level | 18 of 49 (37%) | 4 of 19 (21%) | 0.26 |
| Peripheral vascular disease | 20 (36%) | 14 (47%) | 0.37 |
| Male sex | 43 (78%) | 26 (87%) | 0.40 |
| Age at surgery* (yr) | 60 ± 11 | 62 ± 13 | 0.59 |
| Smoker | 4 (7%) | 1 (3%) | 0.65 |
| Glomerular filtration rate* (mL/min/1.73 m2) | 65.9 ± 32.1 | 64.4 ± 33.7 | 0.85 |
The values are given as the mean and standard deviation.
Age at surgery and peripheral vascular disease were inserted into a binary regression model as potential predictors. Results revealed that peripheral vascular disease dropped out of the model as nonsignificant. Age at surgery was a significant predictor in the model. Older patients were less likely to develop a forefoot ulcer postoperatively. Specifically, the regression coefficient for a 1-year increase in age at the time of surgery was −0.066. The odds of a forefoot ulcer decreased by 6.4% (95% confidence interval, 1.1% to 12.4%) with each year of age (Table IV).
TABLE IV.
Binary Logistic Regression Model for Age and Peripheral Vascular Disease
| Regression Coefficient, ß | Standard Error | Degrees of Freedom | P Value | Odds Ratio, Exp(ß) | Lower 95% Confidence Interval | Upper 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|
| Age at surgery | −0.066 | 0.028 | 1 | 0.019 | 0.936 | 0.886 | 0.989 |
| Peripheral vascular disease | 1.022 | 0.633 | 1 | 0.107 | 2.78 | 0.803 | 9.62 |
Complications
Twenty-one of the 25 patients who were lost to early follow-up died or had a proximal amputation; these patients were included in Table I to document all of the complications. No patients in the TMA-only group developed a new plantar heel ulceration, compared with 1 (3%) of the patients who had an additional ATL procedure (Table I). Three patients in the TMA-only group developed posterior heel wounds, while none of the patients who underwent both TMA and ATL did. After the ATL procedure, 2 (6%) had an Achilles tendon rupture. TMA-only patients had a greater incidence of more proximal amputations (9% versus 6%; p = 0.04) and death (28% versus 11%; p = 0.02). Twenty-two (88%) of the 25 deaths were unrelated to COVID-19; the remaining 3 (12%) occurred during the pandemic and the cause of death could not be identified. Twenty feet in the study were in patients who had end-stage renal disease and 48 feet were in patients with peripheral vascular disease, both of which have been shown to increase the odds of mortality after TMA15. Nine (47%) of the 19 patients without ATL who developed postoperative ulcers developed subsequent osteomyelitis, and 3 patients (16%) went on to proximal amputation as a sequela.
Two of our patients who underwent TMA and ATL experienced Achilles tendon ruptures; however, both were treated with immobilization and functional rehabilitation and experienced no sequelae. Both patients with Achilles tendon rupture were ambulatory without the use of bracing and had no transfer lesions to the plantar heel at the time of the final follow-up. Additionally, 8 patients had a heel lift placed in their fracture boot to prevent overlengthening, and none had plantar heel ulcerations or Achilles tendon ruptures.
Discussion
Primary Outcome Measures
Our data confirm a reduction (from 35% to 3%) in the incidence of late forefoot ulceration after TMA in subjects who also underwent ATL. The 4 surgeons performing TMA without ATL the most often all had a high incidence of late ulceration, suggesting that late ulceration is a common complication regardless of surgeon experience or technique. In this small study, ATL was associated with reduced ulceration and prevention of subsequent major lower-extremity amputation.
Secondary Outcome Measures
Late forefoot ulcers took a fair amount of time to develop following TMA alone, with a mean time to ulceration of 587 days and a median time of 610 days. Our study contrasts with studies on recurrent ulcers after TCC, where the most common time to reulceration is within the first month that the patient stops wearing a cast16. A theory proposed by Attinger et al., that the loss of digital extensors creates a delayed contracture of the Achilles tendon, may explain the delayed nature of these forefoot ulcers12. Muscle imbalance may contribute to equinus postoperatively (Fig. 1-A), but further biomechanical data are needed to determine if delayed equinus contracture occurs after TMA.
The patients who developed late ulcers were significantly younger than the patients who did not (55 versus 63 years of age). This finding suggests that younger patients are at a greater risk for developing late ulcers and may obtain greater benefit from prophylactic ATL with TMA. Younger patients may be at greater risk for late ulceration because, on average, they have higher activity levels that place higher peak pressures on the distal stump.
Complications
Many studies that allowed early weight-bearing after ATL have reported a high incidence of transfer lesions at the heel, with reports ranging from 12% to 18%2,13,14. Colen et al. had a 1.3% incidence of transfer lesions at the heel after utilizing a conservative approach that included a double hemisection and non-weight-bearing for the first 3 to 4 weeks, with a total of 8 weeks wearing a fracture boot6. We also noted a low incidence (2.9%) of transfer lesions at the plantar heel after ATL when patients were kept non-weight-bearing with the leg in a cast for 4 weeks before transitioning to a fracture boot. The low incidence of transfer lesions at the plantar heel with the use of postoperative casting is an important finding because this is the most frequently cited concern after ATL.
In our study, the 1 patient with a transfer lesion at the heel developed osteomyelitis of the calcaneus at 8 months but had not had offloading treatment. Recalcitrant plantar heel ulcers are difficult to manage but have been successfully treated with flexor hallucis longus tendon transfer17.
We found lower rates of proximal amputations and mortality with the addition of the ATL procedure. Compared with our study, a review of 375 patients undergoing TMA reported a higher 3-year mortality rate (36.3%) and a higher proximal amputation rate (36.8%). Peripheral vascular disease and end-stage renal disease increased the odds of mortality15.
Limitations
The limitations of our study include its retrospective nature along with heterogeneous follow-up times. We attempted to mitigate the latter by presenting the data as a Kaplan-Meier curve (Fig. 4). Another limitation was that we did not measure ankle dorsiflexion and forefoot pressure preoperatively or postoperatively to determine whether equinus worsened over time postoperatively. Other limitations were the small sample size, data collection from medical records, and lack of a standardized treatment protocol among the surgeons performing the ATLs. BMI was higher in patients without ATL, and our study was not powered to identify whether BMI was a confounding variable. Only 4 patients in our study did not have diabetes; therefore, it is not known if the results apply to patients without diabetes.
Strengths
The strengths of the study included surgeons with different training using variable techniques and a long follow-up time. Our results may have important practical applications for a very common surgical procedure. Another strength is we did not identify any confounding variables that differed between the treatment groups. Age and follow-up time were confounding variables we identified, and both were similar between the 2 treatment groups (Tables I and III).
Conclusions
Although it was a retrospective study, our data identified an association between prophylactic ATL at the time of TMA and reduced ulceration, with low associated morbidity. Patients should be counseled preoperatively on the need for timely follow-up and offloading due to the risk of late ulceration after TMA.
Acknowledgments
Note: The authors thank Dr. Andrew Cohen, Dr. Eric Gaughan, Dr. Derek Tesoro, Dr. Randy Semma, and Dr. Danielle Duncan for providing cases for review in which they performed transmetatarsal amputation. We also thank Dr. Stephen Zyzanski for aiding with the study design and the statistical analysis and Dr. Neli Ragina for coordinating our research efforts.
Footnotes
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/H194).
References
- 1.Armstrong DG, Stacpoole-Shea S, Nguyen H, Harkless LB. Lengthening of the Achilles tendon in diabetic patients who are at high risk for ulceration of the foot. J Bone Joint Surg Am. 1999. Apr;81(4):535-8. [DOI] [PubMed] [Google Scholar]
- 2.Mueller MJ, Sinacore DR, Hastings MK, Strube MJ, Johnson JE. Effect of Achilles tendon lengthening on neuropathic plantar ulcers. A randomized clinical trial. J Bone Joint Surg Am. 2003. Aug;85(8):1436-45. [PubMed] [Google Scholar]
- 3.Maluf KS, Mueller MJ, Strube MJ, Engsberg JR, Johnson JE. Tendon Achilles lengthening for the treatment of neuropathic ulcers causes a temporary reduction in forefoot pressure associated with changes in plantar flexor power rather than ankle motion during gait. J Biomech. 2004. Jun;37(6):897-906. [DOI] [PubMed] [Google Scholar]
- 4.Lin SS, Lee TH, Wapner KL. Plantar forefoot ulceration with equinus deformity of the ankle in diabetic patients: the effect of tendo-Achilles lengthening and total contact casting. Orthopedics. 1996. May;19(5):465-75. [DOI] [PubMed] [Google Scholar]
- 5.Holstein P, Lohmann M, Bitsch M, Jørgensen B. Achilles tendon lengthening, the panacea for plantar forefoot ulceration? Diabetes Metab Res Rev. 2004. May-Jun;20(Suppl 1):S37-40. [DOI] [PubMed] [Google Scholar]
- 6.Colen LB, Kim CJ, Grant WP, Yeh JT, Hind B. Achilles tendon lengthening: friend or foe in the diabetic foot? Plast Reconstr Surg. 2013. Jan;131(1):37e-43e. [DOI] [PubMed] [Google Scholar]
- 7.Caputo WJ, Fahoury G, Johnson ES. Resurrection of the Achilles tenotomy. Surg Technol Int. 2012. Dec;22:66-9. [PubMed] [Google Scholar]
- 8.Pollard J, Hamilton GA, Rush SM, Ford LA. Mortality and morbidity after transmetatarsal amputation: retrospective review of 101 cases. J Foot Ankle Surg. 2006. Mar-Apr;45(2):91-7. [DOI] [PubMed] [Google Scholar]
- 9.Landry GJ, Silverman DA, Liem TK, Mitchell EL, Moneta GL. Predictors of healing and functional outcome following transmetatarsal amputations. Arch Surg. 2011. Sep;146(9):1005-9. [DOI] [PubMed] [Google Scholar]
- 10.Mueller MJ, Allen BT, Sinacore DR. Incidence of skin breakdown and higher amputation after transmetatarsal amputation: implications for rehabilitation. Arch Phys Med Rehabil. 1995. Jan;76(1):50-4. [DOI] [PubMed] [Google Scholar]
- 11.Sage R, Pinzur MS, Cronin R, Preuss HF, Osterman H. Complications following midfoot amputation in neuropathic and dysvascular feet. J Am Podiatr Med Assoc. 1989. Jun;79(6):277-80. [DOI] [PubMed] [Google Scholar]
- 12.Attinger C, Venturi M, Kim K, Ribiero C. Maximizing length and optimizing biomechanics in foot amputations by avoiding cookbook recipes for amputation. Semin Vasc Surg. 2003. Mar;16(1):44-66. [DOI] [PubMed] [Google Scholar]
- 13.Barry DC, Sabacinski KA, Habershaw GM, Giurini JM, Chrzan JS. Tendo Achillis procedures for chronic ulcerations in diabetic patients with transmetatarsal amputations. J Am Podiatr Med Assoc. 1993. Feb;83(2):96-100. [DOI] [PubMed] [Google Scholar]
- 14.La Fontaine J, Brown D, Adams M, VanPelt M. New and recurrent ulcerations after percutaneous Achilles tendon lengthening in transmetatarsal amputation. J Foot Ankle Surg. 2008. May-Jun;47(3):225-9. [DOI] [PubMed] [Google Scholar]
- 15.Adams BE, Edlinger JP, Ritterman Weintraub ML, Pollard JD. Three-Year Morbidity and Mortality Rates After Nontraumatic Transmetatarsal Amputation. J Foot Ankle Surg. 2018. Sep - Oct;57(5):967-71. [DOI] [PubMed] [Google Scholar]
- 16.Sinacore DR. Total contact casting for diabetic neuropathic ulcers. Phys Ther. 1996. Mar;76(3):296-301. [DOI] [PubMed] [Google Scholar]
- 17.Kim JY, Lee I, Seo K, Jung W, Kim B. FHL tendon transfer in diabetics for treatment of non-healing plantar heel ulcers. Foot Ankle Int. 2010. Jun;31(6):480-5. [DOI] [PubMed] [Google Scholar]