Highlights
-
•
Acute seizure care in schools should use the least invasive seizure rescue therapy.
-
•
School nurse knowledge of intranasal rescue therapy is high but use to date is low.
-
•
School nurses view positively the ease and comfort using an approved nasal spray.
-
•
Clear delegation policies could optimize use of intranasal seizure rescue therapy.
-
•
Seizure education for school nurses and personnel can support better student care.
Keywords: Benzodiazepine, Rescue therapy, Intranasal, Epilepsy, Diazepam, School
Abstract
School nurses play a crucial role in the prompt, appropriate response to epilepsy-related seizure emergencies among students in the school setting. Two intranasal benzodiazepine rescue therapies are now approved and offer potential benefits of being easy to use and socially acceptable. In July 2021, a survey was sent to 49,314 US school nurses to assess knowledge, perceptions, and practice with seizure rescue therapy. Responses were received from 866 (1.8% response rate). Of respondents, 45.7% had used rectal diazepam gel; 9.3%, midazolam nasal spray; and 6.0%, diazepam nasal spray. The majority (58.7%) had not delegated authority to administer rescue therapy, with state/local regulations and lack of willingness of school personnel being the most common barriers to delegation (37.7% and 20.1%, respectively). Additional training of nurses and school staff and progress on delegation policies may help optimize appropriate use of intranasal rescue therapy for seizures and enhance care of students with epilepsy in schools.
1. Introduction
Of the estimated 3.5 million Americans with epilepsy, 470,000 are younger than 18 years of age [1]. >30% of these people continue to experience seizures despite appropriate antiseizure drug therapy [2]. Children and adolescents with epilepsy may experience seizure clusters at school, and treatment in the school setting may be required [3]. School nurses should facilitate quick implementation of personalized seizure action plans (SAPs) that include administration of rescue medications [3], [4]. Prompt, effective treatment of seizure clusters is critical to prevent progression to prolonged seizures or status epilepticus [5]. The 2018 National Association of School Nurses (NASN) School Nursing Evidence-Based Practice Clinical Guidelines: Students With Seizures and Epilepsy recommends that nurses advocate for the least restrictive medication choice for rescue therapy (ie, buccal or nasal rather than rectal formulations) [3], [4].
Benzodiazepines are the foundation of acute treatment for seizure clusters [5]. Before 2019, rectal diazepam gel was the only rescue therapy for seizure clusters approved by the US Food and Drug Administration (FDA). However, rectal administration presents challenges in the school setting, including providing adequate privacy to the student, availability of the nurse at the time of seizure, issues of staff anxiety or fear; and issues around who can administer the medication [6], [7]. The FDA approval of 2 intranasal formulations—midazolam nasal spray in 2019 [8] and diazepam nasal spray in 2020 [9]—has provided new rescue therapy options that offer the potential benefits of having a noninvasive and easy-to-access route of administration, not requiring patient cooperation, and having social acceptability [10].
The approved intranasal benzodiazepine rescue therapies are indicated for the acute treatment of intermittent, stereotypic episodes of frequent seizure activity (ie, seizure clusters, acute repetitive seizures) that are distinct from a patient’s usual seizure pattern in people with epilepsy [11], [12]. Midazolam nasal spray (Nayzilam®) is indicated for patients 12 years and older, whereas diazepam nasal spray (Valtoco®) is indicated for patients 6 years and older. In 2021, shortly after approval of the therapies and during the COVID-19 global pandemic, a survey of US school nurses was conducted to better understand and contextualize the use of diazepam nasal spray within the current practices and challenges surrounding the use of rescue therapy for seizure clusters related to epilepsy in the school setting.
2. Methods
2.1. Survey
The survey was developed by the authors based on insights gleaned from discussions among stakeholders that identified unmet needs in current school-nursing practice. The 33-question survey started generally, with high-level questions on practices related to seizure care for students at school, then narrowed to experience with rescue medications, before finally focusing on barriers to delegation of authority and the possibility of changes in school practice during off-campus activities, such as sports. This arc was intended to build an initial broad understanding before seeking out specific information on barriers to care that could guide future potential solutions. The survey specifically measured perceptions related to the most recently introduced treatment, diazepam nasal spray, which can help gauge how rapidly school nurses gained awareness and experience with the new treatment. Although the 2 approved intranasal treatments use different active agents and excipients and have somewhat different clinical profiles and patient age ranges, both intranasal treatments use a similar spray device; thus, some of the survey findings, particularly related to use or training would be expected to also apply to both treatments. Categorical responses were preferred in order to standardize and quantify responses. Five-point Likert scales were used to assess perceptions of therapeutic options.
2.2. Data collection
Registered school nurses were identified from an opt-in contact list of school nurses from across the US maintained by NASN. During July 2021, the survey was emailed to 49,314 school nurses across the US, with follow-up emails sent to increase response rate. The email linked to a survey hosted online by SurveyMonkey (Momentive, San Mateo, CA). Respondent consent was implied by submission of the survey and respondents were not required to respond to all questions. Compensation was not offered to respondents.
2.3. Data analysis
Data were imported from SurveyMonkey and managed in Excel (Microsoft, Redmond, WA). For freeform data fields presented here, all entries were converted to numeric data points if appropriate. Frequency and percentages were generated from data and analyzed. Proportions are provided for those responding to that specific question.
3. Results
3.1. Respondent demographics and epilepsy experience
Surveys were submitted by 866 (1.8% response rate) respondents. Almost all nurses (96.4%; 831/862) worked full-time providing care for students in grade levels ranging from preschool to high school, with a reported median school health experience of 13 years (Table 1). Nurses were responsible for a median of 680 students each. The majority (80.1%; 689/860) estimated that they were responsible for < 10 students with epilepsy. A majority (77.1%; 663/860) treated < 1 seizure per month; 10.1% (87/860) treated 1 seizure per month; 9.3% (80/860), 2 to 5 seizures per month; and 3.5% (30/860), ≥6 seizures per month.
Table 1.
Characteristics of School Nurses From Across the United States* Who Responded to the Survey (n = 866).
| Characteristic | Respondents (%) |
|---|---|
| Employment status (n = 862) | |
| Full time | 831 (96.4) |
| Part time | 31 (3.6) |
| Experience as a school nurse, y (n = 853) | |
| Median | 13 |
| Schools supervised, n (n = 862) | |
| Median | 1 |
| Grade levels overseen (n = 863) | |
| Preschool | 347 (40.2) |
| Elementary school | 578 (67.0) |
| Middle/junior high school | 391 (45.3) |
| High school | 340 (39.4) |
| Student population size, n (n = 862) | |
| Median | 680 |
| Students with epilepsy in school, n (n = 860) | |
| 1–9 | 689 (80.1) |
| ≥10 | 158 (18.4) |
| I don’t know | 13 (1.5) |
| Seizure events per month requiring care, n (n = 860) | |
| <1 | 663 (77.1) |
| 1 | 87 (10.1) |
| 2–5 | 80 (9.3) |
| ≥6 | 30 (3.5) |
*While all major regions of the US (West, Southwest, Midwest, Southeast, and Northeast) were represented, respondent location was not specifically requested and not available for all respondents.
3.2. School policies and nurse experience with rescue therapy
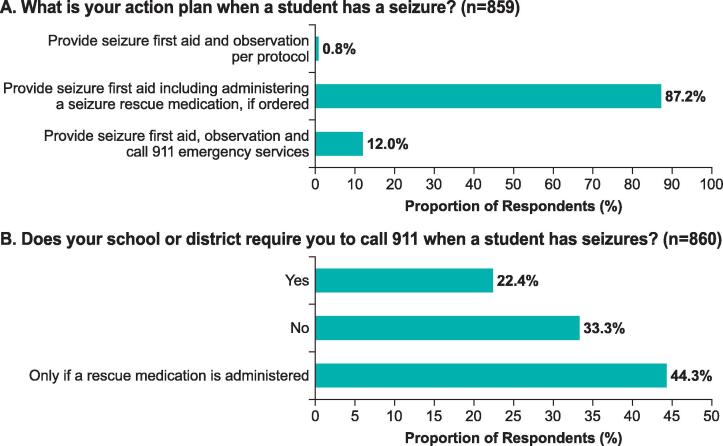
Most nurses (93.6%; 808/863) replied that their schools required an SAP for students with epilepsy. The majority reported that the plan called for administration of rescue medication if ordered, and many responses also indicated that 911 was to be called, although conditions for placing the call varied (Fig. 1).
Fig. 1.
Details of seizure action plans requirements.
Just under half (45.7%; 336/735) of nurses reported experience administering rectal diazepam, whereas experience with intranasal benzodiazepine therapy was reported by 9.3% (68/735) of nurses for midazolam nasal spray and 6.0% (44/735) for diazepam nasal spray. In addition, 46.7% (343/735) reported no experience with any of the available rescue therapies. At the same time, 82.5% (710/861) of respondents stated that they were familiar with diazepam nasal spray as a rescue treatment for seizure clusters.
3.3. Experience and practice with diazepam nasal spray, the most recently approved of the intranasal rescue therapies
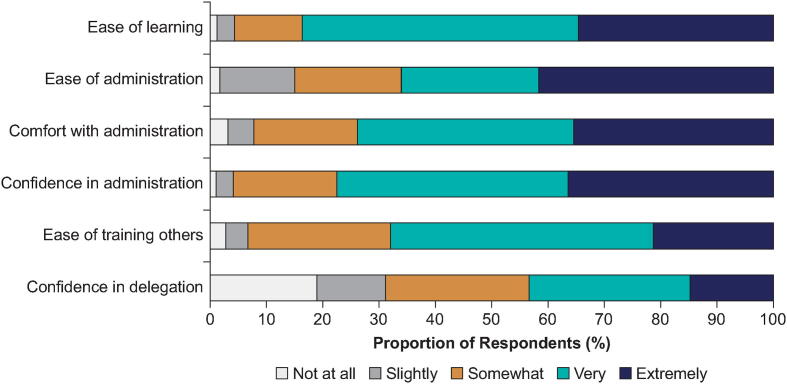
Respondents were asked their perceptions of diazepam nasal spray (Fig. 2): 83.6% (138/165) who provided an applicable response found it very/extremely easy to understand the correct way to administer it, and 85.0% (51/60) who rated ease of administration found it very/extremely easy to administer. Reported levels of comfort with and confidence in administration were likewise high. With respect to training, 29.0% (62/214) have trained other nurses or school personnel on the use of diazepam nasal spray (details on people trained are found in Supplementary Table 1), with 68.0% (51/75) finding it very/extremely easy to train another person. The majority (58.4%; 125/214) have not yet trained someone, and the remainder of school nurses (12.6%; 27/214) plan to train others.
Fig. 2.
Perceptions of diazepam nasal spray use. Questionsa: How easy was it to understand the correct way to administer intranasal diazepam? (n=165); How easy was it for you to administer intranasal diazepam? (n=60); How comfortable was it for you to administer intranasal diazepam in a school setting? (n=65); How confident do you feel in administering intranasal diazepam as a seizure rescue medication to students who may need it? (n=195); How easy was it to train [another] person or persons [on diazepam nasal spray]? (n=75); After understanding how to use intranasal diazepam and that it is approved for use by nonmedical personnel, what is your comfort level delegating the authority to administer it? (n=196). a“N/A” responses were excluded from these tabulations.
When asked about the administration of an intranasal rescue therapy, such as diazepam nasal spray, when required, 65.1% (28/43) of those reporting administration of diazepam nasal spray stated that they administered it all of the time (Supplementary Table 2). Among nurses who administered it all the time, 75.0% (21/28) were responsible for 1 school. Also among these nurses, 71.4% (20/28) responded to < 1 seizure per month. Moreover, 89.3% (25/28) stated that administration was very/extremely easy, and 96.4% (27/28) reported being very/extremely confident in administering it. In contrast, 8 nurses stated that they administered the treatment ≤ 24% of the time, 75.0% (6/8) of whom were responsible for > 1 school building. Also, 87.5% (7/8) of this group responded to ≤ 1 seizure per month. Although 75.0% (6/8) thought it was very/extremely easy to use, levels of confidence in administration varied in this group. Finally, in a related question about administration, nurses also were asked about the possibility of a student being allowed to self-administer intranasal rescue therapy according to doctor’s orders: 7.4% (15/202) responded “Yes”; 56.9% (115/202) responded “No”; and 35.6% (72/202) responded “Unknown.”
3.4. Delegation of authority
The majority of school nurse respondents (58.7%; 507/863) had not delegated authority to another individual at the school to administer a seizure rescue medication to a student, although 68.9% (135/196) of nurses with an opinion about comfort were somewhat/very/extremely comfortable with delegation with an understanding of how to use intranasal rescue therapy such as diazepam nasal spray, and the knowledge that it is approved for use by nonmedical personnel.
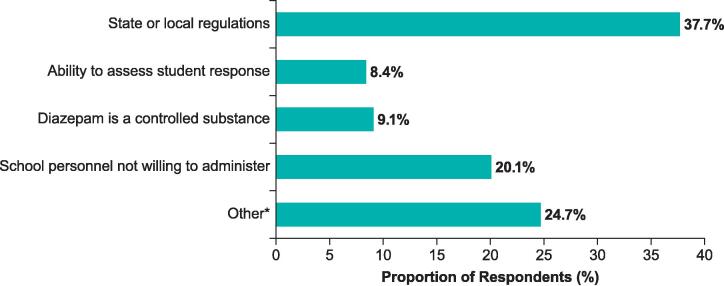
The most common factor identified as preventing delegation of authority to administer rescue therapy such as diazepam nasal spray was state or local regulations, chosen by 37.7% (58/154) of respondents (Fig. 3). Of these nurses, 62.1% (36/58) reside in states that did not have legislation permitting the delegation of authority to administer rescue medication in schools at the time the survey was distributed. (The state data were not available for 6 respondents.) Of the 13 nurses who stated that the “ability to assess student response to treatment” was a barrier, 46.2% (6/13) are responsible for > 1 school (2–26 schools). Among nurses responding that “school personnel is not willing,” 16.1% (5/31) had access to demo sprayers and 12.9% (4/31) had access to demo kits for training purposes.
Fig. 3.
Factors preventing delegation of authority to administer diazepam nasal spray (n=154). *Other remained undefined with no option for specification.
3.5. Implications for student participation in school activities
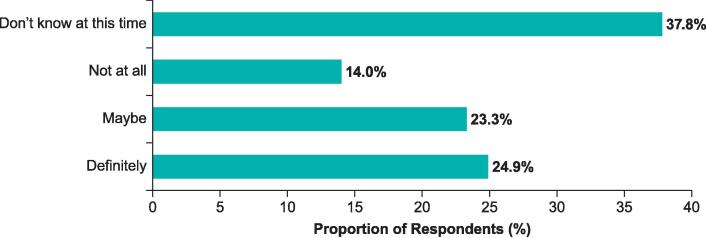
Approximately one-quarter (48/193) of respondents responded that, with the availability of intranasal rescue therapy such as diazepam nasal spray, they anticipate that a change will definitely occur that will now allow students with seizure clusters to participate in extracurricular activities or activities off school premises, and 23.3% (45/193) responded that a change might occur (Fig. 4). However, 37.8% (73/193) did not know at this time whether a change will occur in students’ participation levels. Nearly half of respondents (47.4%; 90/190) identified a teacher or coach as the person most likely to be required to carry intranasal rescue therapy for students participating in extracurricular activities or activities off school premises (Supplementary Table 3).
Fig. 4.
Anticipation of a change in student’s ability to participate in extracurricular activities or activities off school premises with the availability of diazepam nasal spray (n=193).
4. Discussion
Our survey represented a broad cross-section of epilepsy practice by US school nurses. School requirements for an SAP was high, with the majority of plans including the use of rescue medications, if ordered. Just under half of respondents reported no experience with administering rescue therapy of any kind. For those who had been given a rescue treatment, diazepam rectal gel was the most commonly used. Experience with the newer intranasal benzodiazepine rescue therapies was low. The availability of these medications—midazolam nasal spray was approved for use in 2019 and diazepam nasal spray in 2020 [8], [9]—unfortunately coincided with the COVID-19 global pandemic. Because many schools were closed to in-class learning, opportunities for nurses to be trained on and administer the newer therapies were limited. However, knowledge of intranasal rescue therapy was high (>80% of respondents). Nurses were generally open to the idea of delegation of authority to administer, but most had not done so.
The available formulations of intranasal benzodiazepine rescue therapy have distinct characteristics to be considered by school nurses in their practice. Midazolam nasal spray is indicated for the treatment of patients aged ≥ 12 years, whereas diazepam nasal spray can be used to treat children aged ≥ 6 years [11], [12]. Midazolam nasal spray is offered in a single dose (5 mg) for all patients. Dosing of diazepam nasal spray (5, 10, 15, 20 mg) is based on age and weight. Analysis of use of second doses to treat a single episode show that with midazolam, 61.5% of episodes were treated with 1 dose within the first 6 h, and 38.5% were treated with a second dose [13]. In a separate study of diazepam nasal spray, 94.2% of episodes were treated with 1 dose in the first 6 h, with 5.8% treated with a second dose. At 24 h after the initial dose, 87.4% of episodes treated with diazepam nasal spray were treated with a single dose [13].
Perceptions of diazepam nasal spray were positive with respect to training, use, comfort, and confidence. Moreover, one-quarter of respondents anticipated a definite change in students’ ability to participate in extracurricular activities or activities off school premises with the availability of intranasal rescue therapy. Positive perceptions of diazepam nasal spray have also been reported in a survey of caregivers and patients participating in a long-term phase 3 safety study [14]. The vast majority of caregivers (93.8%; 76/81) considered administration of diazepam nasal spray to be extremely/very easy. In contrast, 64.3% (36/56) of caregivers who also had experience with rectal diazepam gel rated the rectal gel as not at all easy to use compared to the nasal spray. Most caregivers (89.6%; 69/77) were extremely/very comfortable using the intranasal rescue therapy in a public setting, whereas 87.0% (47/54) of caregivers were not at all comfortable using rectal diazepam gel in a public setting [14]. Perceptions of the approved midazolam nasal spray formulation have also been shown to be favorable and improved over time during an open-label extension trial [15]. Numeric improvements were noted in patient responses on the effectiveness, side effects, convenience, and global satisfaction scales of the Treatment Satisfaction Questionnaire for Medication. Both patients and caregivers reported general decreases in anxiety and increases in confidence in traveling with an intranasal spray over time [15].
One barrier to appropriate care, including the use of rescue therapy, of schoolchildren with epilepsy identified in studies is a lack of knowledge among some school personnel about epilepsy and its treatment [4]. Although the current study identified widespread knowledge of intranasal rescue therapy, experience with the treatment was limited. School nurses often work alone without healthcare colleagues in a school, which may impede dissemination and uptake of advances in care practices [16]. Even among school nurses who are comfortable with managing seizures in a school setting, additional education on rescue therapies and individualized SAPs have been identified as needs for optimal student care [17].
The current study also identified a need for education of other school personnel, who may play a role in seizure management as unlicensed assistive personnel (UAP) with delegated medication administration authority. Unwillingness of school personnel to administer was identified by 1 in 5 school nurse respondents as a barrier to delegating authority to administer rescue therapy. Within this group, only a minority of respondents stated having access to diazepam nasal sprayer demo kit or demo sprayers. Training of school personnel has been shown to increase knowledge and self-confidence in rescue therapy administration, as well as to improve attitudes toward seizures [18]. A school staff education program started in 2016 on management of epilepsy, including administration of rescue therapy (individual therapies not specified), was delivered to 900 school staff through a children’s hospital in Rome, Italy [19]. In 2018, at the time of data analysis cutoff, pre- and post-training questionnaires showed increased knowledge in acute seizure management (8% to 68%, pre- to post-training, respectively) and readiness to administer rescue medication (54% to 89%), along with significant reductions in anxiety related to seizure management among the majority of staff [19].
Identifying a second potential barrier to appropriate use of rescue therapy, our survey found that the majority of nurses had not delegated authority to administer rescue therapy to other school personnel, although most were comfortable doing so. State or local regulations was the most cited factor (chosen by > 1 in 3 respondents) preventing delegation of the authority. A systematic review and meta-analysis of 42 studies investigating medication management among K–12 schools identified 2 specific topics related to delegation: misalignment of local- and state-level policies, and delegating medication administration for school events, such as field trips [20]. Authors noted that laws and guidelines on delegation sometimes conflict, and licensed school nurses may have difficulty determining which law or guideline takes precedence. Policies may be inconsistent with nursing practice in the jurisdiction. For example, these medications are approved by the FDA to be administered by nonmedical personnel, but schools and local authorities may place restrictions on storage and use of benzodiazepines and may mandate that only nurses administer these medications. On school field trips, the delegation of authority to UAPs may lead to concern that policies may not fully protect the delegating school nurse [20]. The complexity of the issue may explain, in part, why only 17.8% (154/866) of participants responded to this survey question.
The findings presented here provide insight into existing gaps and potential paths forward in awareness, attitudes, education, and policies between current use of newer intranasal benzodiazepine rescue therapy and the practice guidelines. First, training on recognizing and managing epilepsy in the school setting, and particularly the use of intranasal rescue therapies, continues to be needed among school nurses, teachers, other school staff, and students in order to optimize safety for students with epilepsy. Collaboration with other organizations may increase efficiencies through adaptation of existing programs to align with local and state policies. As an example, the Seizure Smart Schools program offered by the Epilepsy Foundation of Minnesota has shown success in increasing use of SAPs and in nurse confidence in managing seizures [21]. In addition, the presence of a school district policy requiring health services for students with certain chronic health conditions, including diabetes and asthma, has been associated with increased support for professional development on a variety of related topics [16]. Training content, including rescue therapies, and training frequency should be developed with active participation of school nurses and other stakeholders.
Second, the availability of noninvasive, easy-to-use intranasal formulations could also affect the practice of delegation of authority to administer rescue therapy, and survey respondents identified state and local regulations as the most frequent barrier to delegation. The authority to delegate medication administration to UAPs is typically derived from individual states’ Nurse Practice Act and education law [20]. Well-written, succinct, and consistent guidelines on delegation across state regulatory agencies could help provide clear interpretation of conflicting or overlapping legislation and policies. Intranasal formulations may also create the possibility of self-administration of benzodiazepine rescue therapy for appropriate patients. Although survey results suggest that the context for self-administration is not widespread in the school setting, clinical study results report self-administration of diazepam nasal spray by children as young as 11 years old [14], [22].
The Epilepsy Foundation recommends Seizure Safe Schools legislation across the nation. The model bill includes a requirement for training on seizure recognition and first aid for school personnel, a mandate for an SAP to be available, the administration of any prescribed FDA-approved treatments in school settings, education and training for students, and a Good Samaritan clause [23]. The number of states with legislation has increased from 3 states in 2019 to 12 in 2021 [24], [25]. Currently, 19 states have enacted a version of the legislation. Such nationwide projects have been successful in enacting legislation in all 50 states and the District of Columbia that ensure that students with asthma or anaphylactic reactions can possess and self-administer emergency medication [26].
The limitations of our study include a response rate of 1.8% and respondents who were self-selected, and a lack of location information for all respondents, which may limit the generalizability of response across the broader population of school nurses. Survey responses may have limited reliability due to nonresponse bias, recall bias, or self-report bias. Respondents were not required to answer all questions, and responses from a single respondent were sometimes inconsistent. Many of the findings in this survey align with findings from other studies, suggesting that the themes remain a high priority for school nurses, administrators, and other stakeholders. Although the survey referenced diazepam nasal spray in some questions, the ease-of-use results may be generalizable to both of the approved intranasal benzodiazepine rescue therapies, which are delivered using similar devices. The sprays have similar indications, with the notable exception of patient age (≥6 years for diazepam and ≥12 years for midazolam). Additional research is needed to identify specific individual, school, and regional barriers and solutions to increase knowledge and appropriate use of intranasal benzodiazepine rescue therapies. New and existing training programs could be evaluated for impact on epilepsy care and program implementation success. It would also be of interest to understand the impact of the availability of intranasal benzodiazepine rescue therapy on clinical and patient outcomes, including seizure management, empowerment, or quality of life.
5. Conclusions
The responses to this survey of school nurses from across the US revealed a high level of awareness and positivity for diazepam nasal spray as a rescue treatment for students with epilepsy, but low levels of experience with intranasal rescue therapy to date. A gap exists between current practice and guidelines as supported by national groups, and ongoing efforts are needed to educate school nurses and other relevant stakeholders in the educational system about seizure recognition and management, including the use of SAPs and the appropriate use of rescue therapies. Furthermore, delegation of authority to administer rescue therapy remains impeded by both individual-level and systems-level factors. Nurses should be active participants in efforts to address these barriers and further optimize care for students with epilepsy.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Ms Santilli is a consultant to Neurelis, Inc. Dr Dewar is a consultant for and member of the Neuroscience Council Advisory Board of Neurelis, Inc. Ms Guerra, Dr Misra, and Dr Rabinowicz are employees of and have received stock options from Neurelis, Inc. Dr Carrazana is an employee of and has received stock and stock options from Neurelis, Inc.
Acknowledgments
Acknowledgments
We thank Emma Gardner for support in data analysis. This study was funded by Neurelis (San Diego, CA). Medical writing support was provided by David McLay, PhD, of The Curry Rockefeller Group, LLC (Tarrytown, NY), and was funded by Neurelis (San Diego, CA).
Ethical statements
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Footnotes
Supplementary nurse survey results on use of intranasal rescue therapy for seizure clusters in students with epilepsy.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.euros.2023.04.012.
Supplementary materials
The following are the Supplementary data to this article:
Supplementary nurse survey results on use of intranasal rescue therapy for seizure clusters in students with epilepsy.
References
- 1.Zack M.M., Kobau R. National and state estimates of the numbers of adults and children with active epilepsy - United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66(31):821–825. doi: 10.15585/mmwr.mm6631a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Z., Brodie M.J., Liew D., Kwan P. Treatment outcomes in patients with newly diagnosed epilepsy treated with established and new antiepileptic drugs: a 30-year longitudinal cohort study. JAMA Neurol. 2018;75(3):279–286. doi: 10.1001/jamaneurol.2017.3949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dean P., O'Hara K., Brooks L., Shinnar R., Bougher G., Santilli N. Managing acute seizures: new rescue delivery option and resources to assist school nurses. NASN Sch Nurse. 2021;36(6):346–354. doi: 10.1177/1942602X211026333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lepkowski A.M., Maughan E.D. Introducing NASN's new evidence-based clinical guideline: students with seizures and epilepsy. NASN Sch Nurse. 2018;33(6):345–350. doi: 10.1177/1942602X18806824. [DOI] [PubMed] [Google Scholar]
- 5.Haut S.R. Seizure clusters: characteristics and treatment. Curr Opin Neurol. 2015;28(2):143–150. doi: 10.1097/WCO.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 6.O'Dell C., O'Hara K. School nurses' experience with administration of rectal diazepam gel for seizures. J Sch Nurs. 2007;23(3):166–169. doi: 10.1177/10598405070230030701. [DOI] [PubMed] [Google Scholar]
- 7.Terry D., Paolicchi J., Karn M. Acceptance of the use of diazepam rectal gel in school and day care settings. J Child Neurol. 2007;22(9):1135–1138. doi: 10.1177/0883073807306254. [DOI] [PubMed] [Google Scholar]
- 8.UCB. UCB Announces Nayzilam® (midazolam) Nasal Spray Now Approved by FDA to Treat Intermittent, Stereotypic Episodes of Frequent Seizure Activity in People Living With Epilepsy in the U.S., https://www.ucb.com/stories-media/Press-Releases/article/UCB-announces-NAYZILAM-midazolam-nasal-spray-now-approved-by-FDA-to-treat-intermittent-stereotypic-episodes-of-frequent-seizure-activity-in-people-living-with-epilepsy-in-the-U-S; 2019 [accessed Nov 30, 2021].
- 9.Neurelis, Inc. Neurelis Announces FDA Approval for Seizure Rescue Treatment VALTOCO® (Diazepam Nasal Spray) That Incorporates the Science of Intrvail® for Consistent and Reliable Absorption, https://www.neurelis.com/neurelis-news/neurelis-announces-fda-approval-seizure-rescue-treatment-valtocor-diazepam-nasal-spray-incorporates#comments; 2020 [accessed Nov 30, 2021].
- 10.Cloyd J, Haut S, Carrazana E, Rabinowicz AL. Overcoming the challenges of developing an intranasal diazepam rescue therapy for the treatment of seizure clusters. Epilepsia. 2021;62(4):846–856. doi: 10.1111/epi.16847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.UCB, Inc. Nayzilam® (midazolam nasal spray). Full Prescribing Information. Smyrna, GA: UCB, Inc.; 2023.
- 12.Neurelis, Inc. Neurelis, Inc.; San Diego, CA: 2023. VALTOCO® (diazepam nasal spray). Full Prescribing Information. [Google Scholar]
- 13.Rabinowicz A.L., Faught E., Cook D.F., Carrazana E. Implications of seizure-cluster treatment on healthcare utilization: use of approved rescue medications. Neuropsychiatr Dis Treat. 2022;18:2431–2441. doi: 10.2147/ndt.S376104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Penovich P., Wheless J.W., Hogan R.E., Guerra C., Cook D.F., Carrazana E., et al. Examining the patient and caregiver experience with diazepam nasal spray for seizure clusters: results from an exit survey of a phase 3, open-label, repeat-dose safety study. Epilepsy Behav. 2021;121:108013. doi: 10.1016/j.yebeh.2021.108013. [DOI] [PubMed] [Google Scholar]
- 15.Meng T.-C., Szaflarski J.P., Chen L., Brunnert M., Campos R., Van Ess P., et al. Psychosocial outcomes of repeated treatment of seizure clusters with midazolam nasal spray: results of a phase 3, open-label extension trial. Epilepsy Behav. 2023;138:108989. doi: 10.1016/j.yebeh.2022.108989. [DOI] [PubMed] [Google Scholar]
- 16.Everett Jones S., Brener N.D., Bergren M.D. Association between school district policies that address chronic health conditions of students and professional development for school nurses on such policies. J Sch Nurs. 2015;31(3):163–166. doi: 10.1177/1059840514547275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Terry D., Patel A.D., Cohen D.M., Scherzer D., Kline J. Barriers to seizure management in schools: perceptions of school nurses. J Child Neurol. 2016;31(14):1602–1606. doi: 10.1177/0883073816666738. [DOI] [PubMed] [Google Scholar]
- 18.Bert F., Pompili E., Gualano M.R., Venuti S., Minniti D., Siliquini R. Empowering seizure management skills: knowledge, attitudes, and experiences of school staff trained in administering rescue drugs in Northern Italy. Epilepsy Behav. 2021;114(Pt A) doi: 10.1016/j.yebeh.2020.107362. [DOI] [PubMed] [Google Scholar]
- 19.Renzetti T., Calabrese C., Pietrafusa N., Pannacci I., Rainò R., Giuffrida A., et al. Management of epileptic seizures in school-age children: educational project dedicated to school staff. Epilepsy Behav. 2020;105:106951. doi: 10.1016/j.yebeh.2020.106951. [DOI] [PubMed] [Google Scholar]
- 20.Lowe A.A., Gerald J.K., Clemens C., Gaither C., Gerald L.B. Medication administration practices in United States' schools: a systematic review and meta-synthesis. J Sch Nurs. 2022;38(1):21–34. doi: 10.1177/10598405211026300. [DOI] [PubMed] [Google Scholar]
- 21.Brook H.A., Hiltz C.M., Kopplin V.L., Lindeke L.L. Increasing epilepsy awareness in schools: a Seizure Smart Schools project. J Sch Nurs. 2015;31(4):246–252. doi: 10.1177/1059840514563761. [DOI] [PubMed] [Google Scholar]
- 22.Tarquinio D., Dlugos D., Wheless J.W., Desai J., Carrazana E., Rabinowicz A.L. Safety of diazepam nasal spray in children and adolescents with epilepsy: results from a long-term phase 3 safety study. Pediatr Neurol. 2022;132:50–55. doi: 10.1016/j.pediatrneurol.2022.04.011. [DOI] [PubMed] [Google Scholar]
- 23.Epilepsy Foundation. Seizure Safe Schools, https://www.epilepsy.com/advocacy/priorities/seizure-safe-schools; 2022 [accessed June 17, 2022].
- 24.Epilepsy Foundation . Landover; MD: 2019. Annual Report FY 2019. [Google Scholar]
- 25.Epilepsy Foundation . Landover; MD: 2021. Annual Report FY 2021. [Google Scholar]
- 26.Butler S.M., Boucher E.A., Tobison J., Phan H. Medication use in schools: current trends, challenges, and best practices. J Pediatr Pharmacol Ther. 2020;25(1):7–24. doi: 10.5863/1551-6776-25.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary nurse survey results on use of intranasal rescue therapy for seizure clusters in students with epilepsy.