Abstract
Typical radiologic images of Covid-19 pneumonia consists in a wide spectrum of chest manifestations, which range from peripheral predominant ground-glass opacities to an organizing pneumonia pattern, with additional features including crazy-paving, consolidations, fibrotic streaks and linear opacities.
With variants imaging profile of Covid-19 evolves, producing relatively atypical/indeterminate CT pattern of pulmonary involvement, which overlap with imaging features of a variety of other respiratory diseases, including infections, drug reaction and hypersensitivity pneumonia. Our knowledge of these radiological findings is incomplete and there is a need to strengthen the recognition of the many faces of Covid-19 pneumonia.
Introduction
In March 2020, the World Health Organization (WHO) declared the coronavirus disease 2019 caused by Sars-CoV2 virus (COVID-19) as a pandemic and global public health emergency. This is the first pandemic in modern era presenting with unknown clinical syndrome and therapy: both of them were defined progressively, after the spread of the disease.
At first COVID-19 was interpreted as an infectious disease limited to the lungs, whereas only afterwards the vasculitic pathogenesis was described as affecting other organs. COVID-19 outcome and long-COVID syndrome have been described only recently.
Imaging features of COVID-19 were likewise progressively portrayed, after the widespread of the disease, leading to a new nosographic radiological entity. 1
Additional aspects of this infectious disease are represented by the wave-shaped trend of the pandemic (“waves”, variably named, depending on the countries), and by the outbreak of new variants of the virus. Few of them were declared by the WHO “Variant of Concern”, given their enhanced transmissibility or virulence, and their potential to weaken the effectiveness of therapy and vaccination strategies. Five variants have been designated by the WHO:
α (B. 1.1.7), first described in UK in late December 2020;
β (B. 1.351), first reported in South Africa in December 2020;
γ (P.1), first described in Brazil in January 2021;
δ (B.1.617.2): first reported in India in December 2020 and the more recent one, the Omicron (B. 1.1.529), reported in South Africa in October 2021. 2
δ variant was associated with increased viral load and prolonged viral shedding in respiratory samples compared to previous variants, with implications on infection control and public health policy: this leaded to higher rates of hospitalization, ICU admission and death. Many studies have shown that Omicron VOC have a less severe clinical presentation than the δ VOC. 3
Although reference standard for diagnosis is RT-PCR, chest CT remains a complementary diagnostic tool limited to specific indications, playing a role in clinical assessment of patients with moderate to severe illness. 1
This is a short pictorial guide showing the key imaging features of variants of COVID-19, which could be useful in daily radiological practice.
CT protocol
CT is the gold-standard in diagnostic imaging of COVID-19 pneumonia.
Chest CT examination should be performed with high-resolution non-contrast technique with a reconstructed slice thickness of 1.0–1.5 mm. 1
Imaging findings
The subsequent waves of pandemic showed different and atypical chest CT features, that are less specific or relatively uncommon, and can occur in association with or even mimic a variety of infectious and non-infectious processes. 4
GGO with predominant upper lobes involvement and random distribution
The typical Covid-19 started as bilateral ground-glass opacities (GGOs) in posterior segments of lower lobes with peripheral distribution, which then developed into the crazy paving appearance and subsequent consolidation. 5 With variants, GGO may present random distribution (no predilection for subpleural or central regions), with prevalent/exclusive involvement of upper lobes (Figure 1).
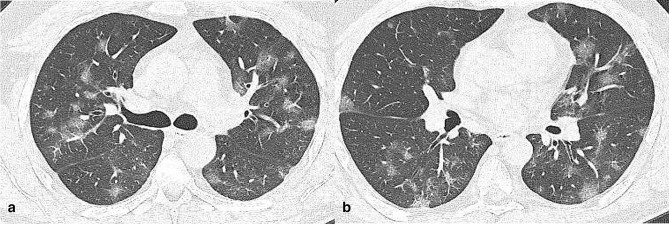
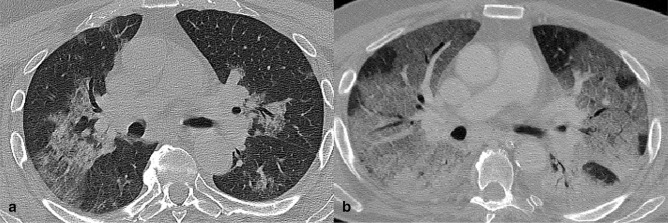
Figure 1.
Axial CT images (a, b) of a 34-year-old male infected by SARS-CoV-2 α variant (3 days since symptoms onset). CT showed centrally and peripherally located multifocal GGO opacities with mainly involvement of upper lobes.
Single isolated involvement
During third and fourth wave, we observed solitary involvement in any lobe, in the form of GGO or denser (Figures 2 and 3): in early stage of disease, if this sign is not accompanied by other features or patterns, like small areas of consolidation or interlobular septal thickening, alternative diagnoses should be considered. Crucial is the correlation with clinic and laboratory.
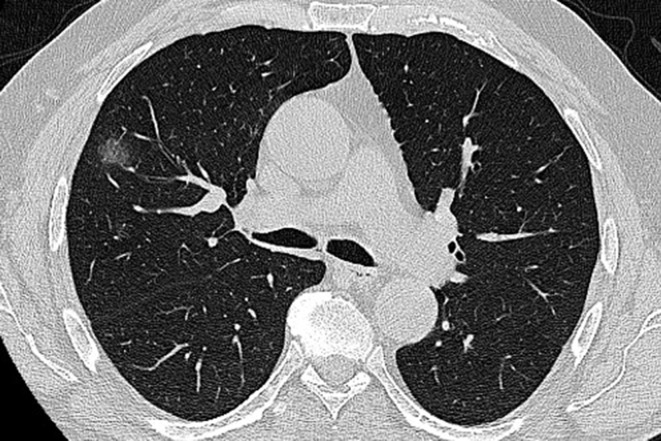
Figure 2.
A 54-year-old female COVID −19 patient (2 days since symptoms onset) infected by Omicron variant. CT scan shows single ground glass opacity with rounded appearance, in the right upper lobe.
Figure 3.
A 78-year-old male arriving at the emergency department with fever. Axial (a) and coronal reformatted (b) CT images documented a subpleural GGO in right lower lobe. Notably, there were signs of consolidation in the context of the lesion. The real-time reverse transcription polymerase chain reaction test was positive for Sars-Cov-2 infection. Subsequent genetic sequencing detected α variant. GGO, ground-glass opacity.
Isolated lobar consolidation
Consolidations were described as patchy, multifocal or segmental in the late phase of the disease, during first wave of pandemic; they also represented a possible indicator of disease progression. 6
With variants, we observed homogenous consolidations involving exclusively one lobe, with visible air-bronchogram sign.
This feature is not specific, since it could be caused by different infectious agents, like Pneumococcus or Legionella species (Figure 4). 7
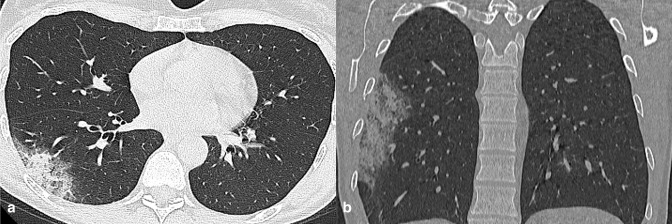
Figure 4.
A 57-year-old COVID-19 patient (δ variant) presenting fever and dry cough for 3 days. Axial (a) and coronal (b) reformatted CT images showed pneumonia with isolated lobar consolidation in the right lower lobe.
Pulmonary target sign (bullseye sign)
Considered as a variant of reverse halo sign, this pulmonary feature consists of central high attenuation focus surrounded by an inner ring of air and an outer complete or incomplete ring-like consolidation. 8 The central nodule is centrilobular, the outer ring of ground glass perilobular, while the inner ring of air corresponds to sparing of the remainder lobule (Figures 5 and 6).
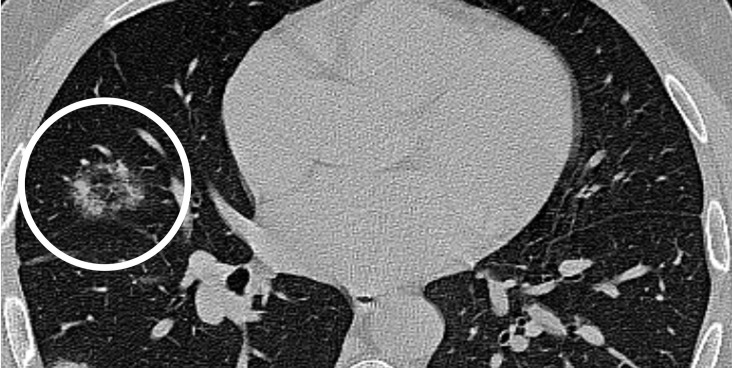
Figure 5.
A 32-year-old female infected with COVID-19 (δ Variant): axial unenhanced CT image showed focus of central ground glass nodule surrounded by an inner ring of air and an outer ring of ground glass (white circle). This appearance ressembles a bullseye.
Figure 6.
The “bullseye sign” in a 44-year-old male COVID-19 patient (Omicron variant) with fever and dry cough for 7 days.
Tree-in-bud appearance
Tree-in-bud appearance consists of centrilobular nodules connected to multiple branching linear structures, most observed in lung’s periphery (Figures 7 and 8). Originally described in cases of endobronchial Tubercolosis, this pattern is now considered as a CT feature of many differents infectious agents. 9
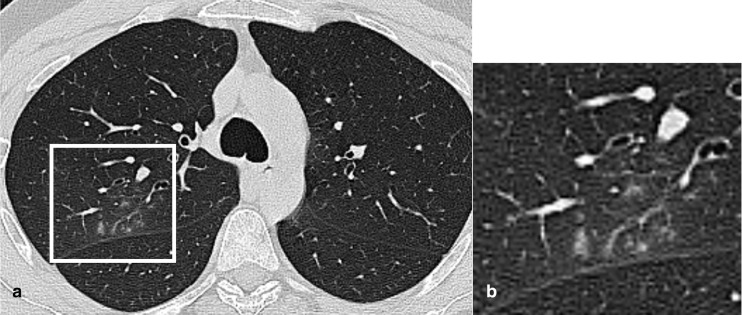
Figure 7.
Axial CT image of a 25-year-old male Covid-19 patient (γ variant) showed perifissural small centrilobular nodules connected to linear branching opacities (white box), in right upper lobe.
Figure 8.
Axial CT image of a 78-year-old male Covid-19 patient (α variant), showed tree-in-bud opacities in right upper lobe with bronchial wall thickening.
Diffuse GGO with centrilobular distribution
Variants show also diffuse symmetric, ill-defined GGO in both lung with centrilobular predominant distribution (Figures 9 and 10); this imaging pattern overlaps with other viral infections, such as CMV pneumonia. 10
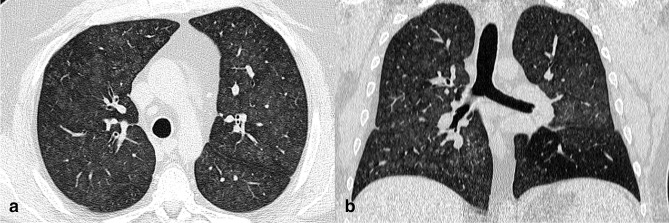
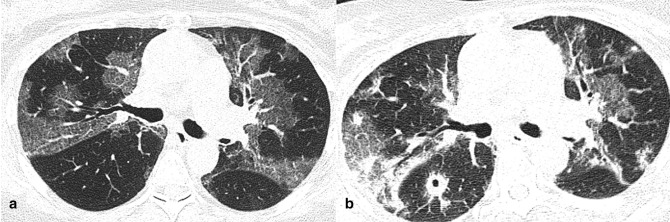
Figure 9.
CT images of a 58-year-old male patient with confirmed COVID-19 pneumonia (γ variant). Axial (a) and coronal reformatted (b) images showed diffuse lung involvement with ill-defined centrilobular GGO and subpleural sparing. GGO, ground-glass opacity.
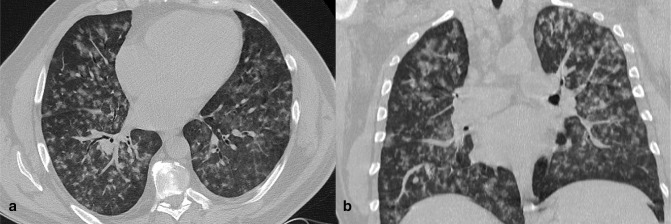
Figure 10.
A 42-year-old female COVID-19 patient (γ variant) presenting fever and chills for 4 days. Axial (a) and coronal reformatted (b) images showed bilateral ill-defined centrilobular GGO. GGO, ground-glass opacity.
White lung
As pulmonary impairment gets worse, GGOs increase, spreading to more lobes and merging each other, with inter- and intralobular septal reticular thickening and partial consolidation. In patients with complicated pneumonia, dense consolidation involving all lobes become prevalent. This pattern, called “white lung”, can also be observed in other lung diseases (viral infection, drug toxicity). It represents the CT correlate of the underlying pathophysiology of pneumonia as it progresses to acute respiratory distress syndrome (ARDS), predicting a worse outcome. 10 (Figures 11 and 12)
Figure 11.
Axial CT image of a 68-year-old patient with COVID-19 pneumonia (δ variant), with symptoms for 4 days, showed bilateral extensive consolidations. The patient died 5 days later.
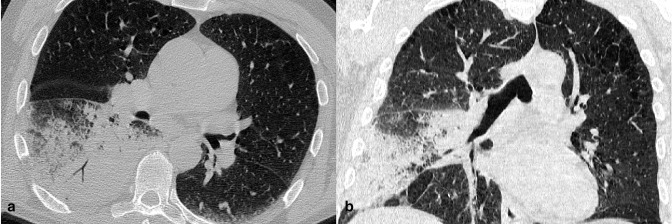
Figure 12.
Axial CT image slices of a female COVID-19 patient (α Variant) of 81-year-old. a) CT scan, performed after 1 day from symptoms onset, showed a mixed pattern of GGO and consolidation in upper lobes with peribronchovascular involvement. b) CT obtained after 5 days from symtoms onset. Lesions increased with higher density and superimposed thickening of the interlobular septum in both lungs, with predominant dorsal consolidations.
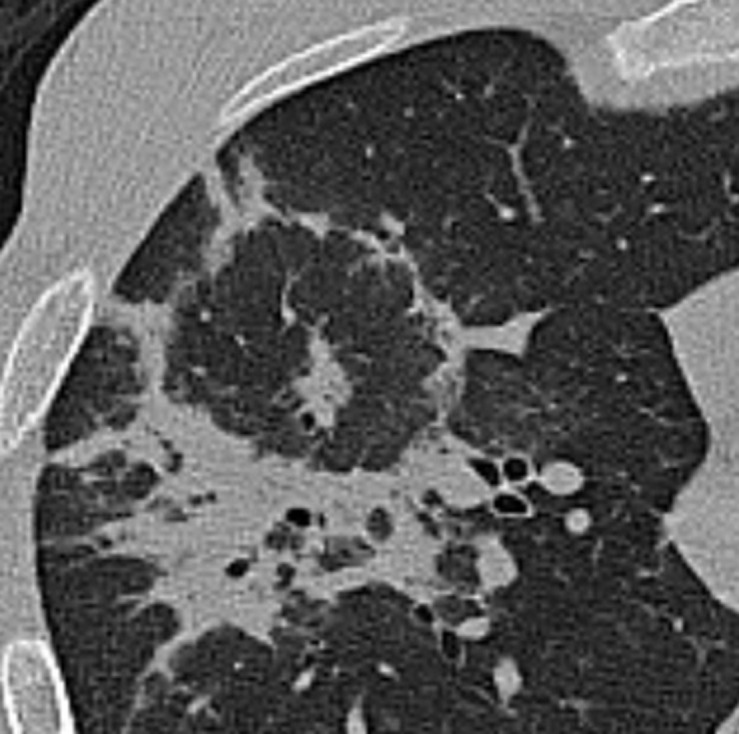
Cavitation
Cavitation is a circumscribed abnormal gas-filled space of the lung, seen as a low-density area within a pulmonary consolidation, a mass, a nodule. Salehi et al showed that cavitation represents the evolution of lung consolidation, visible on CT in later stage of Covid-19 pneumonia 11 (Figure 13).
Figure 13.
Evolution of CT findings in a 56-year-old female COVID-19 patient (δ variant). (a) CT scan, performed after 3 days from symptom onset, showed GGO with superimposed inter- and intralobular septal thickening (crazy-paving pattern) in upper lobes. (b) Scan obtained on day 7 from symptom onset, showed peripheral consolidations. In apical segment of right lower lobe, CT demonstrated rounded consolidation with cavitation in context.
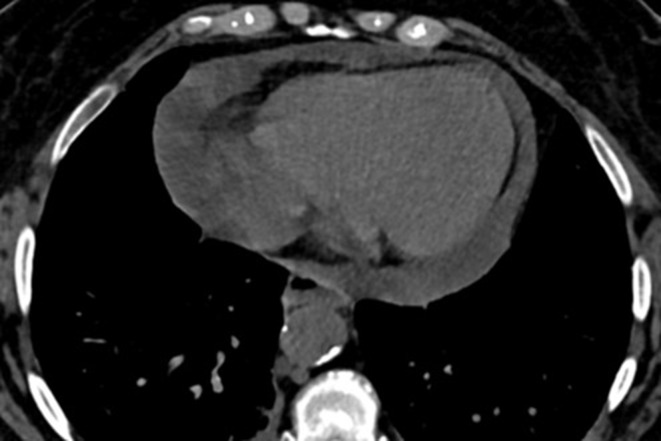
Pericardial effusion
Several studies stated that pericardial effusion is a rare finding in Covid-19 patients (5% of total population infected with wild type), especially in the later stage of pneumonia, representing a sign of disease progression. 11,12 Patients infected with variants frequently showed this feature from the earliest stage of disease (Figure 14).
Figure 14.
A 53-year-old female COVID-19 patient (Omicron variant), presenting with dry cough, dyspnea and fever up to 39° for 3 days. Axial CT image showed large amount of pericardial effusion.
Conclusions
This pictorial assay summarizes main chest radiological features identified in a wide range of spectrum of manifestation, in patients infected with Covid-19 variants, highlighting differences compared to wild type virus. In our routine screening CT for diagnosis in emergency department of Policlinico Umberto I, we reported atypical chest findings, non-specific or uncommon for Covid-19 pneumonia, potentially attributable to variants, that could be observed in a large number of conditions, leading to diagnostic difficulty.
The imaging hallmark of Covid-19 pneumonia, described in many publications, is a bilateral confluent and extensive GGO and patchy consolidation with prevalent subpleural distribution and lower lobes predominance, mostly posterior basal segments. Inter- and intralobular septal thickening may be present in more advanced cases (crazy paving).
Covid-19 variants produce different chest CT pattern, characterized by GGO with random distribution (both peripheral and central interest) and mainly upper lobe involvement; we reported single isolated GGO or lobar consolidation, thee-in-bud pattern, targeted pulmonary sign.
In the most critical cases, CT scan showed widespread consolidation involving all lobes (white lung).
Furthermore cavitation and pericardial effusion, quite rare findings during first wave of pandemic, were frequently observed with variants.
Diagnostic imaging of COVID has its own limitations. Imaging profile of Covid-19 infection is composite and constantly evolving, with a wide range of CT features, as well as clinical manifestations.
Our pictorial essay displays imaging findings of variants, to help radiologists in their detection to speed-up diagnostic workflow in symptomatic patients; these CT manifestations are not pathognomonic and are observed in other lung infectious and non-infectious processes; a lack of their detection may lead to misdiagnosis and delay in the isolation of Sars-CoV-2 patients.
Those limitations due to aspecific and variable CT features could be partially overcome by correlating them with clinical history.
The findings described and main differential diagnoses are summarized in Table 1.
Table 1.
CT features in patients infected with variants and main differentials diagnoses
| Features associated with variants | Differential diagnoses |
|---|---|
| GGO with prevalent upper lobes involvement and random distribution |
|
| Single isolated involvement |
|
| Isolated lobar consolidation |
|
| Pulmonary target sign (bullseye sign) |
|
| Tree in bud appearance |
|
| Diffuse GGO with centrilobular distribution |
|
| White lung |
|
| Cavitation |
|
| Pericardial effusion |
|
AAH, atypical adenomatous hyperplasia; ADV: adenovirus;AIP, acute interstitial pneumonia; CMV: cytomegalovirus; GGO, ground-glass opacity; HPIV: human para-influenza virus; MTB: Mycobacterium tubercolosis; NTM: non-tuberculous mycobacteria; RB-ILD: respiratory bronchiolitis interstitial lung disease; RSV: respiratory syncytial virus.
H1N1: subtype of Influenza A virus
Contributor Information
Giacomo Bonito, Email: giacomo.bonito@alice.it.
Valeria Martinelli, Email: valeria.martinelli@cloud.com.
Francesco Vullo, Email: francescovullo84@gmail.com.
Fabrizio Basilico, Email: fabriziobasilico.fb@gmail.com.
Eleonora Polito, Email: eleonpol@gmail.com.
Antonella Izzo, Email: antonella.izzo90@gmai.com.
Laura Corso, Email: laura-cor@hotmail.it.
Paolo Ricci, Email: paolo.ricci@uniroma1.it.
REFERENCES
- 1. Kanne JP, Bai H, Bernheim A, Chung M, Haramati LB, Kallmes DF, et al. COVID-19 imaging: what we know now and what remains unknown. Radiology 2021; 299: E262–79. doi: 10.1148/radiol.2021204522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boehm E, Kronig I, Neher RA, Eckerle I, Vetter P, Kaiser L, et al. Novel SARS-cov-2 variants: the pandemics within the pandemic. Clin Microbiol Infect 2021; 27: 1109–17. doi: 10.1016/j.cmi.2021.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kumar S, Thambiraja TS, Karuppanan K, Subramaniam G. Omicron and delta variant of sars-cov-2: A comparative computational study of spike protein. J Med Virol 2022; 94: 1641–49. doi: 10.1002/jmv.27526 [DOI] [PubMed] [Google Scholar]
- 4. Hochhegger B, Zanon M, Altmayer S, Mandelli NS, Stüker G, Mohammed T-L, et al. COVID-19 mimics on chest CT: a pictorial review and radiologic guide. Br J Radiol 2021; 94(1118): 20200703. doi: 10.1259/bjr.20200703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol 2020; 30: 4381–89. doi: 10.1007/s00330-020-06801-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology 2020; 295: 715–21. doi: 10.1148/radiol.2020200370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhou J, Liao X, Cao J, Ling G, Ding X, Long Q. Differential diagnosis between the coronavirus disease 2019 and Streptococcus pneumoniae pneumonia by thin-slice CT features. Clin Imaging 2021; 69: 318–23. doi: 10.1016/j.clinimag.2020.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shaghaghi S, Daskareh M, Irannejad M, Shaghaghi M, Kamel IR. Target-shaped combined halo and reversed-halo sign, an atypical chest CT finding in COVID-19. Clin Imaging 2021; 69: 72–74. doi: 10.1016/j.clinimag.2020.06.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. El Homsi M, Chung M, Bernheim A, Jacobi A, King MJ, Lewis S, et al. Review of chest CT manifestations of COVID-19 infection. Eur J Radiol Open 2020; 7: 100239. doi: 10.1016/j.ejro.2020.100239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Parekh M, Donuru A, Balasubramanya R, Kapur S. Review of the chest CT differential diagnosis of ground-glass opacities in the COVID era. Radiology 2020; 297: E289–302. doi: 10.1148/radiol.2020202504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): A systematic review of imaging findings in 919 patients. AJR Am J Roentgenol 2020; 215: 87–93. doi: 10.2214/AJR.20.23034 [DOI] [PubMed] [Google Scholar]
- 12. Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol 2020; 55: 327–31. doi: 10.1097/RLI.0000000000000672 [DOI] [PMC free article] [PubMed] [Google Scholar]