Abstract
Ischaemic heart disorders are among the leading causes of mortality worldwide. There has been a growing occurrence of heart disease among young adults. Thus, acute myocardial infarction (MI) should be considered in all patients with central chest pain. Herein, we report the case of a young, fit, active smoker with underlying dyslipidaemia presenting with acute MI, characterised by dynamic changes in lead aVL wherein T wave flattening progressed to inversion, suggestive of early reciprocal changes. Soon after, electrocardiogram (ECG) revealed ST elevation in leads III and aVF, indicative of acute inferior wall MI. Subsequently, coronary angiogram showed right coronary artery occlusion. This case report highlights the importance of serial ECGs in patients who present with chest pain and have a high clinical suspicion for acute MI with normal or inconclusive ECG findings. Measurement of highly sensitive serum troponin based on a 1- or 3-h protocol is important in diagnosing acute MI but not ST-elevation MI. An early sign of inferior wall MI may be a new T wave inversion in lead aVL.
Keywords: Myocardial infarction, Electrocardiogram, Coronary artery disease
Introduction
Electrocardiogram (ECG) is a convenient, noninvasive and important diagnostic tool for acute myocardial infarction (MI). There has been a growing occurrence of heart disease among young adults.1 Among patients presenting with acute coronary artery syndrome, inferior wall MI accounts for 40%–50% of all MIs.2 Although 91% of ‘subtle’ inferior wall ST-elevation myocardial infarction (STEMI) does not meet the STEMI criteria, ECG demonstrates ST depression in lead aVL.2
Case presentation
A 29-year-old male active smoker with underlying dyslipidaemia presented to our hospital 3 h after the initial onset of upper chest pain, which was pressing in nature, radiated to the neck and left upper limb and associated with dizziness, sweating and nausea. He had no family history of ischaemic heart disease.
At presentation, the patient was well and no longer had chest pain. On examination, his temperature was 36.5°C; blood pressure, 122/61 mmHg; pulse rate, 64 beats per minute; respiratory rate, 18 breaths per minute; and oxygen saturation, 100% on room air. He was able to speak in complete sentences and was not distressed. There were no heart murmurs heard on cardiac auscultation. The rest of the examination was unremarkable.
Twelve-lead ECG was conducted immediately upon arrival, which did not show any MI-related changes (Figure 1). Given the typical chest pain presentation, serial 12-lead ECGs and serum troponin measurements were performed for the patient.
Figure 1. Electrocardiogram of the patient upon arrival (pain score=0).

During the 3rd hour of observation in the emergency room, the patient complained of recurrent chest pain with a pain score of 7, radiating to the neck and bilateral arms. The patient appeared anxious. However, his haemodynamics remained stable. Twelve-lead ECG was immediately performed, showing a slight ST elevation over lead III and a flattening of the T wave in lead aVL (Figure 2). Rightsided ECG showed a 0.5-mm raised ST segment in lead V4R (Figure 3). Posterior ECG did not show any ST elevation over leads V7, V8 and V9 (Figure 4). With his symptoms and subtle ECG changes, he was diagnosed with inferior wall STEMI with right-side involvement. He was administered 300 mg of aspirin tablet and 300 mg of clopidogrel tablet and then underwent thrombolysis with alteplase within the thrombolytic period. Post thrombolysis, his chest pain resolved. ECG post thrombolysis showed resolved ST elevation (Figure 5) and T inversion in lead AVL.
Figure 2. Electrocardiogram of the patient upon recurrence of chest pain (pain score=7). He exhibits a negative T wave over lead aVL and ST straightening in the inferior leads (II, III and aVF). The first reciprocal finding for inferior wall myocardial infarction is frequently T wave inversion in lead aVL.

Figure 3. Right-sided electrocardiogram showing a 0.5-mm raised ST segment in lead V4R.

Figure 4. Posterior electrocardiogram showing no posterior involvement.
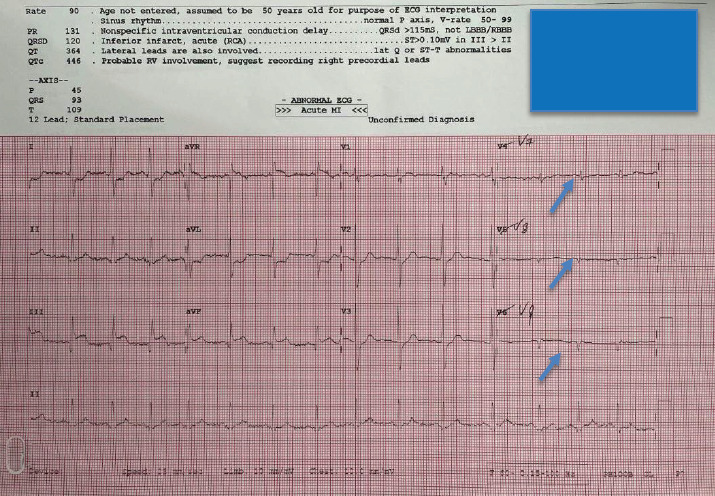
Figure 5. Electrocardiogram post thrombolysis showing the ST segment in an isoelectric line (pain score=0).

Upon arrival in the emergency room, his first troponin I level was 25 pg/mL. His repeated troponin I level increased to 50,000 pg/mL. His lipid profile showed elevated total cholesterol (5.8 mmol/L), triglyceride (2.4 mmol/L) and low density lipoprotein ( LDL) cholesterol levels (4.11 mmol/L) and low high density lipoprotein (HDL) cholesterol level (0.6 mmol/L).
Coronary angiogram was conducted, which showed right coronary artery occlusion; this occlusion was treated with a drug-eluting balloon (Figure 6). The patient was asymptomatic in the ward and subsequently discharged well.
Figure 6. (a) Coronary angiogram showing mild proximal right coronary artery (RCA) occlusion with distal discrete occlusion of 90%. The posterior descending artery and posterolateral vessel are normal. (b) Right coronary artery after percutaneous coronary intervention with a drug-eluting balloon to the distal RCA.

Discussion
Ischaemic heart disorders remained a principal cause of mortality in 2022 after COVID-19, accounting for 13.7% of all deaths in the same year.3 ECG manifestations can be substantially subtle. Hence, interpreting ECG findings can be challenging. Sometimes, the only early sign of inferior wall MI is T wave reciprocal changes in lead aVL. According to previous studies, 70%–97.2% of patients with inferior wall MI and 30% of those with anterior wall MI have reciprocal changes in lead aVL.4,5
It has been shown that T wave inversion in lead aVL can appear in individuals without an underlying cardiac disease, as seen in 10%–20% of the Caucasian population in Scotland.6 The degree of T wave inversion is critical in determining pathological T wave inversion such as the Pardee T wave. Any precordial lead with T wave inversion of at least 0.06 mV may be a predictor of ischaemic heart disease.6 Although a single T wave inversion may not predict coronary artery disease, serial ECGs should be performed to monitor for dynamic changes. Acute inferior wall MI, acute anterior wall MI, left ventricular hypertrophy, left bundle branch block and use of digitalis are possible diflerential diagnoses for reciprocal changes in lead aVL.7
In the present case, ECG demonstrated dynamic changes in lead aVL from T wave flattening to T wave inversion, indicating early reciprocal changes of acute MI. Subsequently, ECG revealed ST elevation in leads III and aVF, indicating acute inferior wall MI. T wave inversion in lead aVL can be a warning sign of severe cardiac pathologies, such as an evolving inferior wall MI with possible right-ventricle involvement or a significant mid-segment LAD lesion.8 No dynamic changes will be seen on serial ECGs for chronic LAD lesions.8 As seen on the serial ECGs of the present case, inferior wall MI causing T wave inversion may progress to either ST depression in lead aVL or ST elevation in leads II, III and aVF.
The importance of serial ECGs is highlighted in the present patient, who presented with a nondiagnostic initial ECG. Silber et al.9 showed that out of 94 acute MI cases, 20% had nondiagnostic ECGs on arrival and subsequently developed ECG changes meeting the thrombolytic criteria. In identifying acute MI and acute coronary syndrome, serial ECG is more sensitive and specific than initial ECG.10
Therefore, a dynamic ECG change can help identify ongoing myocardial ischaemia.
Serial measurements of highly sensitive biomarkers such as serum troponin I may facilitate the diagnosis of acute MI.11 However, in the case of STEMI, reperfusion therapy should not be delayed by waiting for the affirmation of the biomarkers of myocardial injury.
Conclusion
While many new more accurate diagnostic tools have been introduced since the advent of ECG, this procedure remains an essential tool for diagnosing acute cardiac events owing to its ease of usage and relative convenience. Thus, every clinician should have a mastery of ECG and be alert to new ECG findings. In unclear cases, serial monitoring of chest pain using ECG and a 1- or 3-hour measurement protocol for highly sensitive troponin is crucial. An early sign of inferior wall MI may be a new T wave inversion in lead aVL. Prompt identification of MI should be made, allowing for early intervention and complication prevention.
Acknowledgements
The authors would like to thank the patient for his permission in writing this case report.
Conflicts of interest
The authors declare there are no conflicts of interest relevant to this article.
Author Contributions
All authors contributed to the drafting, writing, editing and revision of the case report.
Patient’s consent for the use of images and content for publication
Written consent was obtained from the patient before the preparation of the case report.
What is new in this case report compared to the previous literature?
This case report highlights the importance of serial electrocardiograms (ECGs) and cardiac marker measurements in patients suspected of having acute coronary artery syndrome. Sometimes, T wave inversion in lead aVL can be seen in individuals without heart disease. In unclear cases, serial ECG is essential in detecting dynamic changes, along with a 1- or 3-h measurement protocol for highly sensitive troponin.
This case report also shows the importance of reciprocal changes in lead aVL in diagnosing inferior wall myocardial infarction. This will benefit primary healthcare doctors in early referrals to cardiac centres.
What is the implication to patients?
A proper interpretation of initial ECGs, serial ECGs and highly sensitive troponin measurements will help detect myocardial infarction, especially in patients with an atypical presentation, consequently ensuring early reperfusion intervention and better prognosis.
References
- 1.Centers for Disease Control and Prevention. Heart disease: it can happen in any age. [January 26; 2021 ]. [January 27; 2023 ]. [Google Scholar]
- 2.Buttner R, Burns E. Inferior STEMI. [September 8; 2021 ]; [January 24; 2023 ];Life in the fastlane. [Google Scholar]
- 3.Department of Statistics of Malaysia. Statistics on cause of death of Malaysia. 2022. [October 27; 2022 ]. [January 24; 2023 ]. http://dosm.gov.my [Google Scholar]
- 4.Birnbaum Y, Sclarovsky S, Mager A, Strasberg B, Rechavia E. ST segment depression in a VL: a sensitive marker for acute inferior myocardial infarction. Eur Heart J. 1993;14(1):4–7. doi: 10.1093/eurheartj/14.1.4. [DOI] [PubMed] [Google Scholar]
- 5.Morris F, Brady WJ. ABC of clinical electrocardiography: acute myocardial infarction-part I. BMJ. 2002;324(7341):831–834. doi: 10.1136/bmj.324.7341.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassen GW, Costea A, Carrazco C, et al. Isolated T wave inversion in lead aVL: an ECG survey and a case report. Emerg Med Int. 2015;2015:250614. doi: 10.1155/2015/250614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salim Rezaie MD. The importance of reciprocal changes in lead aVL. REBEL.EM. Medical category: cardiovascular. [November 1; 2013 ]. [January 24; 2023 ]. https://rebelem.com/importance-reciprocal-changes-avl/ [Google Scholar]
- 8.Hassen GW, Talebi S, Fernaine G, Kalantari H. Lead aVL on electrocardiogram: emerging as important lead in early diagnosis of myocardial infarction?. Am J Emerg Med. 2014;32(7):785–788. doi: 10.1016/j.ajem.2014.02.038. [DOI] [PubMed] [Google Scholar]
- 9.Silber SH, Leo PJ, Katapadi M. Serial electrocardiograms for chest pain patients with initial nondiagnostic electrocardiograms: implications for thrombolytic therapy. Acad Emerg Med. 1996;3(2):147–152. doi: 10.1111/j.1553-2712.1996.tb03403.x. [DOI] [PubMed] [Google Scholar]
- 10.Fesmire FM, Percy RF, Bardoner JB, Wharton DR, Calhoun FB. Usefulness of automated serial 12-lead ECG monitoring during the initial emergency department evaluation of patients with chest pain. Ann Emerg Med. 1998;31(1):3–11. doi: 10.1016/S0196-0644(98)70274-4. [DOI] [PubMed] [Google Scholar]
- 11.Sandoval Y, Apple FS, Mahler SA, et al. High-Sensitivity Cardiac Troponin and the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guidelines for the Evaluation and Diagnosis of Acute Chest Pain. Circulation. 2022;146(7):569–581. doi: 10.1161/CIRCULATIONAHA.122.059678. [DOI] [PubMed] [Google Scholar]


