Abstract
Background
Disorders of Gut‐Brain Interaction (DGBI) are highly prevalent worldwide, but their effect on work productivity has not gained much attention.
Aims and Methods
We aimed to compare work productivity and activity impairment (WPAI) in persons with and without DGBI in a large population‐based cohort and identify factors independently associated with WPAI in subjects with DGBI. Data were collected from Germany, Israel, Italy, Japan, the Netherlands, Poland, Spain and Sweden via Internet surveys as part of the Rome Foundation Global Epidemiology Study. Apart from the Rome IV diagnostic questionnaire, questionnaires evaluating WPAI related to general health (WPAI:GH), psychological distress (PHQ‐4), somatic symptom severity (PHQ‐15) and other factors were assessed.
Results
Of the 16,820 subjects, 7111 met the criteria for DGBI according to the Rome IV diagnostic questionnaire. Subjects with DGBI were younger (median (interquartile range) age 43 (31–58) vs. 47 (33–62)) and more often female (59.0% vs. 43.7%) compared to subjects without DGBI. Subjects with DGBI had higher absenteeism, presenteeism (poor work productivity due to illness), overall work impairment and activity impairment (p < 0.001) compared with subjects without. For subjects with DGBI affecting more than one anatomical region, WPAI was incrementally higher for each additional region. There were significant differences in WPAI for subjects with DGBI in different countries. Subjects from Sweden had the highest overall work impairment and from Poland the lowest. Using multiple linear regression, male sex, fatigue, psychological distress, somatic symptom severity and number of anatomical regions were independently associated with overall work impairment (p < 0.05 for all).
Conclusion
In the general population, people with DGBI have substantial WPAI compared with those without DGBI. The reasons for these findings should be explored further, but having multiple DGBI, psychological distress, fatigue and somatic symptom severity seem to contribute to this impairment associated with DGBI.
Keywords: activity impairment, fatigue, gut‐brain axis, psychological distress, Rome Foundation, Rome IV criteria, somatic symptom, work productivity
Key summary.
Summarize the established knowledge on this subject
Some Disorders of Gut‐Brain Interaction (DGBI) are associated with high work loss.
Previous studies have focused on only a few DGBI, assessed patient groups or were limited to one country.
Work productivity impairment in DGBI as a group has not been examined to date in a population‐based, multinational cohort.
What are the significant and/or new findings of this study?
In the general population, persons with DGBI have greater work productivity and activity impairment (WPAI) compared with those without DGBI.
Painful DGBI, presence of DGBI in multiple anatomical regions, psychological distress, and somatic symptom severity were associated with even higher WPAI.
WPAI in persons with DGBI differs among countries.
INTRODUCTION
Disorders of Gut‐Brain Interaction (DGBI), previously referred to as functional gastrointestinal (GI) disorders, are highly prevalent disorders with symptoms in different parts of the GI tract such as pain, discomfort, bloating, vomiting, or abnormal bowel habits. Although patients suffer from troublesome symptoms, results of clinical tests and examinations are normal and the diagnosis is based on fulfilling the symptom‐based Rome IV criteria for DGBI. 1 The pathophysiology is multifactorial with different combinations of altered central nervous system processing, visceral sensitivity, GI motility, gut microbiota, and immune and mucosal function. 1
Apart from symptoms, many DGBIs have a large impact on daily living and quality of life for the affected individuals and comorbidity with mental disorders (e.g., anxiety and depression) is common. Healthcare utilization is high, and both direct (e.g., healthcare visits, medications, examinations) and indirect (e.g., work absence) costs can be substantial for the individual and society. Even though studies from as early as 1993 have shown a negative impact of DGBI in terms of work absence and employment status compared to the general population, 2 studies specifically focusing on other DGBI than irritable bowel syndrome (IBS) and the impact on work are few and those that did examine job loss focused primarily on economic aspects and not underlying causes. One study examining costs in functional bowel disorders (functional diarrhea, functional abdominal bloating, unspecified functional bowel disorder, functional constipation and IBS) reported that indirect costs, largely driven by reduced productivity, were over 10 times higher than direct costs. 3 Chronic constipation has been reported to cause school and work absenteeism, and lowered productivity, seemingly affected by the severity of symptoms. 4 Having multiple DGBI (e.g., functional dyspepsia, functional constipation and IBS with constipation), and gastroesophageal reflux disease has been found to affect productivity and the number of missed days from work or school. 5 In a previous study from our group including 525 patients with IBS, we found that IBS symptom severity, fatigue and GI‐specific anxiety were independently associated with work impairment. 6
Hence, studies assessing WPAI in DGBI have so far mainly focused on individual DGBI, used patient cohorts, not included population‐based samples, used previous versions of the diagnostic criteria for DGBI, and focused on single countries. Therefore, we aimed to investigate WPAI in persons with DGBI in a large multinational population‐based study and to identify factors independently associated with WPAI in persons with Rome IV DGBI.
MATERIALS AND METHODS
Data collection
We used data from the Rome Foundation Global Epidemiology Study (RFGES), a study of DGBI conducted in 33 countries, 26 of which used Internet surveys. 7 Apart from the adult Rome IV diagnostic questionnaire 8 and an 80‐item supplemental questionnaire, which all participants completed, other validated questionnaires could be added to the survey in some of the countries, one of which was the Work Productivity and Activity Impairment Questionnaire: General Health (WPAI:GH). 9 Here, we used data from the eight countries that used Internet surveys and collected data on WPAI with the WPAI:GH: Germany, Israel, Italy, Japan, the Netherlands, Poland, Spain and Sweden. The collection of data was done through Qualtrics Inc., a professional company that specializes in Internet surveys. Persons already registered in online survey panels were invited to participate in a “health survey” based on demographic quotas to fulfill predefined demographic parameters of sex (50% female and 50% male), and age (40% for 18–39 years, 40% for 40–64 years, and 20% for 65+ years). Participants were rewarded with points that they could trade for gifts. Data collection has been described in greater detail elsewhere, and data were collected 2017–2018. 7 Some of the data in this paper have already been reported in previous RFGES papers. This is inevitable since the original paper included a broad range of descriptive statistics for all countries (33) and all disorders (22). Other papers, including the present one, which use the same database, are reporting in‐depth analyses for countries, disorders, and methods, and these include a brief overview of some specific data previously reported.
All participants provided electronic consent before completing the study. The study was reviewed and deemed exempt from ethics board oversight due to the anonymity of the survey method using the Biomedical Institutional Review Board of the University of North Carolina at Chapel Hill (UNC IRB application number: 16‐2486), the institution that served as Data Coordination Center and collected the survey data electronically from subjects in all the countries surveyed.
Questionnaires
All subjects completed the adult Rome IV diagnostic questionnaire, assessing 22 DGBI according to Rome IV criteria 8 and the 80‐item questionnaire assessing potential factors that can affect or be affected by DGBI (such as organic diseases, socioeconomics, medications, surgeries). The supplemental questionnaire was then used together with the Rome IV diagnostic questionnaire to diagnose DGBI, where subjects reporting organic diseases that could disqualify them from a DGBI diagnosis were excluded (e.g., subjects reporting having inflammatory bowel disease or GI cancer).
The WPAI:GH assesses four domains over the last 7 days; absenteeism, absence from work due to health issues; presenteeism, that is, reduced work productivity while at work due to health issues; overall work impairment, that is, presenteeism and absenteeism combined; as well as impairment in activities and productivity outside of work due to health issues. Scores ranging from 0% to 100% impairment were calculated for each domain. For some comparisons, we also calculated the proportion of participants reporting any health‐related WPAI as a percentage for each domain. Only subjects currently employed answer questions concerning the first three domains, whereas all subjects answer the question on activity impairment. 9
The Patient Health Questionnaire‐4 (PHQ‐4) is a validated questionnaire assessing psychological distress using four questions rated on a 4‐point Likert scale (“Not at all,” “Several days,” “More than half the days,” “Nearly every day”) with a total score ranging from 0 to 12. 10 In some analyses, we used validated cutoffs to divide the subjects into groups of normal (0–2), mild (3–5), moderate (6–8), and severe (9–12) psychological distress. 11
Overall somatic symptom severity, including GI symptoms, was assessed using the Patient Health Questionnaire‐15 (PHQ‐15) which consists of 15 questions on a range of somatic symptoms rated on a 3‐point Likert scale (“Not at all,” “Bothered a little,” “Bothered a lot”) with a total score ranging from 0 to 30. 12 PHQ‐15 has standardized cutoffs for no (0–4), mild (5–9), moderate (10–14), and high (≥15) somatic symptom severity. 13
Fatigue was assessed with the question “How would you rate your fatigue on average?” from the PROMIS Global‐10 questionnaire. 14 The respondents answered on a 5‐point Likert scale (“None,” “Mild,” “Moderate,” “Severe,” “Very severe”) giving a score from 1 to 5.
Data analysis and statistics
To compare demographics and WPAI in subjects with versus without DGBI, participants with DGBI were identified according to the Rome IV diagnostic questionnaire. The DGBI was then divided into different anatomical regions in line with the Rome IV criteria: esophageal, gastroduodenal, bowel and anorectal disorders, where one subject could have a DGBI in multiple regions. Differences in WPAI between subjects with DGBI in no, one, two, three, or four anatomical regions were assessed. For many of the DGBI characterized by the Rome IV criteria, pain is a qualifying symptom, and we compared differences in WPAI between subjects with painful and non‐painful DGBI, based on the hypothesis that pain is particularly relevant for reduced work productivity. For these comparisons, subjects fulfilling the criteria for at least one painful and at least one non‐painful DGBI were classified as having painful DGBI, that is, there was no overlap between the groups. Which DGBI were classified as painful and non‐painful is provided in supplementary table 1. Subgroups of “no or low” and “medium or high” somatic symptom severity, and “normal or mild” and “moderate and severe” psychological distress, were compared regarding WPAI. 13 WPAI for the subjects with DGBI in the different countries was assessed. Finally, we examined factors independently associated with reduced WPAI in DGBI, where factors previously found to be of potential relevance were entered as independent variables. 6 , 15 , 16
In general, non‐parametric tests were used to compare group differences in WPAI. For descriptive data, the median percentage of work impairment (interquartile range) and the proportion reporting any health‐related WPAI for the respective groups are presented as percentages. Comparisons between groups were made using the Mann‐Whitney U Test when comparing two groups and the Kruskal‐Wallis test when comparing more than two groups. To examine if there was a linear association between WPAI (dependent variable) and the number of anatomical regions affected by DGBI (independent variable), we used one‐way between‐group analysis of variance with linear trend analysis, and with effect sizes demonstrated as partial eta squared (η 2), where effect sizes were defined as small (η 2 0.01–0.05), medium (η 2 0.06–0.13) or large (η 2 > 0.14). 17 To identify factors independently associated with WPAI (dependent values) multiple linear regression was performed, with age, sex as well as factors that have been postulated or previously found to affect job loss (fatigue, somatic symptom severity, overlapping DGBI, anxiety and depression) being entered as independent variables, 6 , 15 , 16 where a p‐value <0.05 was considered significant. The statistical analyses were performed using SPSS version 28.0 and R version 4.1.3.
RESULTS
Study population
In total, there were 16,820 subjects in our cohort, with approximately 2000 subjects from each country (Germany, n = 2020; Israel, n = 2008; Italy, n = 2063; Japan, n = 2504; the Netherlands, n = 2008; Poland, n = 2057; Spain, n = 2072; and Sweden, n = 2084). Of the included subjects, 7111 had at least one DGBI according to the Rome IV diagnostic questionnaire. The subjects with a DGBI were younger, more often female, had slightly lower body mass index and had higher psychological distress and somatic symptom severity scores than subjects without a DGBI (Table 1).
TABLE 1.
Descriptive data in all subjects divided into two groups: Subjects with at least one DGBI according to Rome IV diagnostic criteria and subjects without DGBI.
| DGBI, n = 7111 | No DGBI, n = 9709 | p‐value | |
|---|---|---|---|
| Female | 4193 (59.0) | 4240 (43.7) | <0.001 |
| Age, years | 43 (31–58) | 47 (33–62) | <0.001 |
| Education, years | 14 (12–17) | 14 (12–16) | 0.071 |
| Currently employed | |||
| All participants | 3984 (56.0) | 5588 (57.6) | 0.048 |
| 18–64 years | 3779 (63.7) | 5235 (69.2) | <0.001 |
| BMI | 24.5 (21.5–28.1) | 24.8 (22.0–27.8) | 0.009 |
| Psychological distress (PHQ‐4) | <0.001 | ||
| None | 3052 (42.9) | 6873 (70.8) | |
| Mild | 2403 (33.8) | 2118 (21.8) | |
| Moderate | 884 (12.4) | 479 (4.9) | |
| Severe | 772 (10.9) | 239 (2.5) | |
| Somatic symptom severity (PHQ‐15) | <0.001 | ||
| No | 1368 (19.2) | 5205 (53.6) | |
| Low | 2838 (39.9) | 3403 (35.0) | |
| Medium | 2026 (28.5) | 897 (9.2) | |
| High | 879 (12.4) | 204 (2.1) | |
Note: Continuous variables are summarized with median (interquartile range) and categorical by count (%).
Abbreviations: BMI, body mass index; DGBI, disorders of brain‐gut interaction; PHQ‐4, Patient Health Questionnaire‐4; PHQ‐15, Patient Health Questionnaire‐15.
Work productivity and activity impairment and DGBI
Significantly higher degrees of absenteeism, presenteeism, overall work impairment and activity impairment were seen for subjects with at least one DGBI, both in scores and in the proportion of subjects reporting any health‐related WPAI compared to subjects without DGBI (Figure 1 and Table S2). Work productivity and activity impairment scores for each of the different DGBI diagnoses are presented in Table S3, with unspecified functional bowel disorder and functional abdominal bloating/distension having the lowest and functional heartburn the highest scores for overall work impairment. Work productivity and activity impairment scores and proportions of subjects reporting any health‐related WPAI for the different anatomical regions affected by DGBI can be seen in Table 2. Bowel disorders had the lowest WPAI of the regions, while the other three regions had similar levels. However, since one subject can have a DGBI in several anatomical regions, these differences were not evaluated statistically.
FIGURE 1.
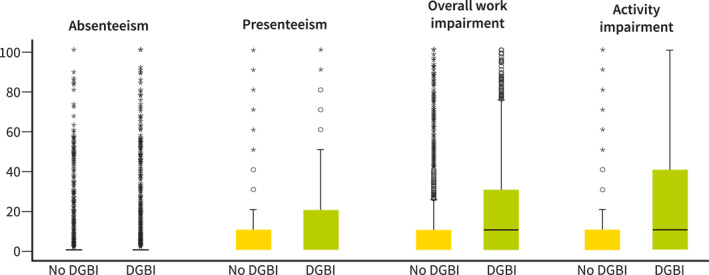
Work productivity and activity impairment scores for subjects with and without DGBI. There were significant differences (p < 0.001) for comparisons of all the WPAI variables between subjects with and without DGBI. DGBI, disorders of brain‐gut interaction; WPAI, work productivity and activity impairment.
TABLE 2.
Work productivity and activity impairment: Scores and proportions reporting any health‐related WPAI for each of the different anatomical GI regions affected by DGBI.
| Absenteeism | Presenteeism | Overall work impairment | Activity impairment | |||||
|---|---|---|---|---|---|---|---|---|
| Median (IQR) (%) | Proportion reporting (%) | Median (IQR) (%) | Proportion reporting (%) | Median (IQR) (%) | Proportion reporting (%) | Median (IQR) (%) | Proportion reporting (%) | |
| Esophageal disorders, n = 1058 | 0 (0–6.35) | 29.9 | 20 (0–40) | 63.7 | 20 (0–50) | 67.3 | 30 (0–60) | 73.9 |
| Gastroduodenal disorders, n = 1729 | 0 (0–7.55) | 31.3 | 20 (0–40) | 63.4 | 20 (0–50.1) | 67.3 | 30 (0–60) | 74.4 |
| Bowel disorders, n = 6107 | 0 (0–0) | 19.3 | 10 (0–30) | 50.7 | 10 (0–30) | 54.2 | 10 (0–40) | 61.9 |
| Anorectal disorders, n = 1319 | 0 (0–4.26) | 28.6 | 20 (0–30) | 67.1 | 20 (0–50) | 69.8 | 30 (10–50) | 75.1 |
Note: One subject can have DGBI in several regions.
Abbreviations: DGBI, disorders of brain‐gut interaction; GI, gastrointestinal; IQR, interquartile range; WPAI, work productivity and activity impairment.
There were 4884, 1533, 505 and 187 subjects with DBGI affecting 1, 2, 3, and 4 anatomical regions, respectively. With the increasing number of anatomical regions affected by DGBI, a gradual increase in absenteeism, presenteeism, overall work impairment and activity impairment was seen, with small effect sizes for absenteeism and medium effect sizes for presenteeism, overall work impairment and activity impairment (Figure 2a–d).
FIGURE 2.
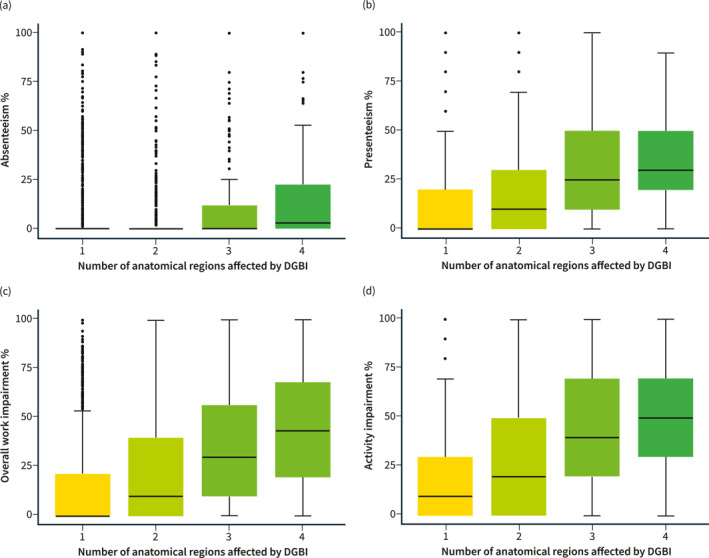
(a) Absenteeism scores and number of GI regions affected with a diagnosed DGBI. Partial ƞ 2 = 0.018, p‐value ≤ 0.001. (b) Presenteeism scores and number of GI regions with a diagnosed DGBI. Partial ƞ 2 = 0.075, p‐value ≤ 0.001. (c) Overall work impairment‐scores and number of GI regions with a diagnosed DGBI. Partial ƞ 2 = 0.067, p‐value ≤ 0.001. (d) Activity impairment‐scores and number of GI regions with a diagnosed DGBI. Partial ƞ 2 = 0.068, p‐value ≤ 0.001. DGBI, disorders of brain‐gut interaction; GI, gastrointestinal; WPAI, work productivity and activity impairment.
Association between work productivity and activity impairment and painful DGBI, somatic symptom severity and psychological distress
Subjects with at least one painful DGBI had significantly greater work and activity impairment, both in scores and in the proportion reporting any health‐related work and activity impairment than subjects with non‐painful DGBI (Figure 3a and Table S4). The same pattern was seen for DGBI subjects with medium or high (scores ≥10) versus no or low somatic symptom severity according to PHQ‐15, and for DGBI subjects with moderate or severe (scores ≥6) versus normal or mild psychological distress according to PHQ‐4 (Figure 3b,c and Table S4).
FIGURE 3.
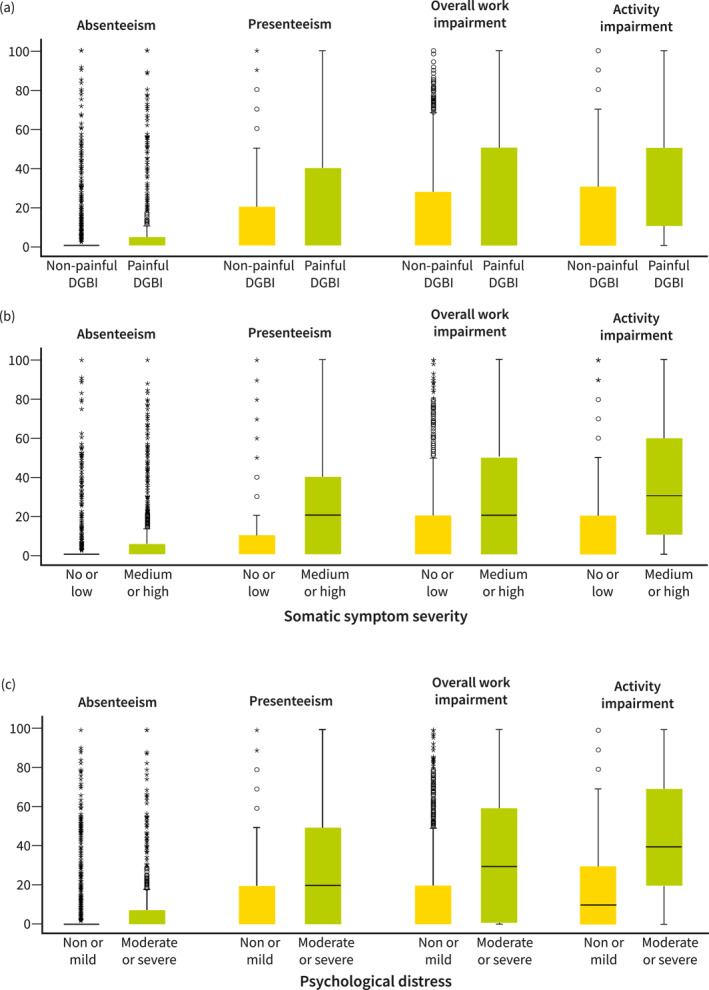
(a) WPAI scores for subjects with non‐painful versus painful DGBI. There were significant differences (p < 0.001) for all the WPAI variables between subjects with non‐painful versus painful DGBI. (b) WPAI scores for subjects with no or low versus medium or high somatic symptom severity according to the Patient Health Questionnaire‐15. There were significant differences (p < 0.001) for all the WPAI variables between subjects with no or low versus medium or high somatic symptom severity. (c) WPAI scores for subjects with none or mild versus moderate or severe psychological distress according to the Patient Health Questionnaire‐4. There were significant differences (p < 0.001) for all the WPAI variables between subjects with none or mild versus moderate or severe psychological distress. DGBI, disorders of brain‐gut interaction; WPAI, work productivity and activity impairment.
WPAI in the different countries
As seen in Table 3, there were significant differences between countries in absenteeism, presenteeism, overall work impairment and activity impairment, both in scores and proportions of subjects reporting any health‐related work and activity impairment. For absenteeism, subjects from Japan had the lowest scores and subjects from Spain the highest scores and proportions reporting any health‐related absenteeism. For presenteeism and overall work impairment, subjects from Poland had the lowest levels of impairment while subjects from Sweden had the highest, scores and proportions reporting impairment. Subjects from Sweden had the highest activity (i.e., non‐work) impairment scores, while subjects from the Netherlands had the highest proportion reporting any health‐related activity impairment and subjects from Israel had the lowest activity impairment.
TABLE 3.
Work productivity and activity impairment: Scores and proportions reporting any health‐related WPAI for subjects with DGBI for each of the participating countries.
| Absenteeism | Presenteeism | Overall work impairment | Activity impairment | |||||
|---|---|---|---|---|---|---|---|---|
| Median (IQR) | Proportion reporting | Median (IQR) | Proportion reporting | Median (IQR) | Proportion reporting | Median (IQR) | Proportion reporting | |
| Germany, n = 792 | 0 (0–1.47)% | 25.1% | 10 (0–30)% | 55.6% | 10 (0–42.7)% | 59.9% | 20 (0–50)% | 68.1% |
| Israel, n = 768 | 0 (0–0)% | 17.5% | 0 (0–20)% | 45.7% | 0 (0–22.3)% | 49.1% | 10 (0–30)% | 52.0% |
| Italy, n = 969 | 0 (0–0)% | 20.5% | 10 (0–30)% | 53.4% | 10 (0–30)% | 56.5% | 10 (0–30)% | 59.4% |
| Japan, n = 1025 | 0 (0–0)% | 9.8% | 10 (0–20)% | 52.1% | 10 (0–30)% | 53.9% | 10 (0–30)% | 58.4% |
| The Netherlands, n = 650 | 0 (0–0)% | 22.8% | 5 (0–30)% | 50.0% | 10 (0–40)% | 56.0% | 20 (0–60)% | 69.7% |
| Poland, n = 994 | 0 (0–0)% | 12.6% | 0 (0–20)% | 42.7% | 0 (0–20)% | 46.7% | 10 (0–30)% | 60.1% |
| Spain, n = 962 | 0 (0–2.04)% | 25.5% | 0 (0–20)% | 45.1% | 0 (0–30)% | 49.7% | 10 (0–40)% | 56.4% |
| Sweden, n = 951 | 0 (0–0)% | 24.6% | 10 (0–30)% | 57.3% | 20 (0–50)% | 60.8% | 30 (0–60)% | 69.3% |
| p‐value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Note: p‐values indicate if there were significant differences between the countries using the Kruskal–Wallis test.
Abbreviations: DGBI, disorders of brain‐gut interaction; IQR, interquartile range; WPAI, work productivity and activity impairment.
Factors independently associated with WPAI
Multiple linear regression models were performed with presenteeism, overall work impairment, and activity impairment as dependent variables, respectively, and age, sex, fatigue, psychological distress, somatic symptom severity and number of anatomical regions affected by DGBI as independent variables (Table 4). Fatigue, psychological distress, somatic symptom severity and number of anatomical regions affected by DGBI were independently associated with all the dependent variables, presenteeism, overall work impairment and activity impairment. Female sex was independently associated with presenteeism and overall work impairment, with a negative β‐coefficient meaning that male sex was a predictor of higher degrees of these variables. Age was independently associated with presenteeism and activity impairment, with a negative β‐coefficient for presenteeism and a positive for activity impairment.
TABLE 4.
Linear regression analyses: Presenteeism, overall work impairment, and activity impairment.
| Predictors | Presenteeism | ||
|---|---|---|---|
| β‐coefficient | 95% confidence interval | p‐value | |
| (Intercept) | −7.00 | −10.12 to −3.88 | <0.001 |
| Female sex | −2.54 | −3.78 to −1.30 | <0.001 |
| Age | −0.06 | −0.11 to −0.02 | 0.009 |
| Fatigue | 2.71 | 1.91 to 3.51 | <0.001 |
| Psychological distress (PHQ‐4) | 1.54 | 1.31 to 1.78 | <0.001 |
| Somatic symptom severity (PHQ‐15) | 0.96 | 0.80 to 1.12 | <0.001 |
| Number of anatomical regions affected by DGBI | 3.32 | 2.45 to 4.19 | <0.001 |
| Observations | 3709 | ||
| R 2/R 2 adjusted | 0.239/0.238 | ||
| Predictors | Overall work impairment | ||
|---|---|---|---|
| β‐coefficient | 95% confidence interval | p‐value | |
| (Intercept) | −8.76 | −12.74 to −4.78 | <0.001 |
| Female sex | −2.41 | −4.01 to −0.82 | 0.003 |
| Age | −0.04 | −0.10 to 0.02 | 0.199 |
| Fatigue | 3.33 | 2.31 to 4.35 | <0.001 |
| Psychological distress (PHQ‐4) | 1.62 | 1.32 to 1.92 | <0.001 |
| Somatic symptom severity (PHQ‐15) | 1.23 | 1.03 to 1.43 | <0.001 |
| Number of anatomical regions affected by DGBI | 3.96 | 2.85 to 5.07 | <0.001 |
| Observations | 3807 | ||
| R 2/R 2 adjusted | 0.205/0.204 | ||
| Predictors | Activity impairment | ||
|---|---|---|---|
| β‐coefficient | 95% confidence interval | p‐value | |
| (Intercept) | −25.17 | −27.72 to −22.51 | <0.001 |
| Female sex | 0.02 | −1.13 to 1.16 | 0.979 |
| Age | 0.19 | 0.16 to 0.23 | <0.001 |
| Fatigue | 6.51 | 5.81 to 7.21 | <0.001 |
| Psychological distress (PHQ‐4) | 2.03 | 1.83 to 2.24 | <0.001 |
| Somatic symptom severity (PHQ‐15) | 1.24 | 1.09 to 1.38 | <0.001 |
| Number of anatomical regions affected by DGBI | 2.72 | 1.92 to 3.53 | <0.001 |
| Observations | 7012 | ||
| R 2/R 2 adjusted | 0.305/0.304 | ||
Abbreviations: DGBI, disorders of brain‐gut interaction; PHQ‐4, Patient Health Questionnaire‐4; PHQ15, Patient Health Questionnaire‐15.
DISCUSSION
In this study, WPAI was examined in a large, population‐based, multinational cohort comprising more than 16,800 subjects. This is, to our knowledge, the first study investigating work productivity impairment in DGBI in a large cohort and with an international population‐based approach using uniform methodology. We found that persons with Rome IV DGBI had substantial work and activity impairment due to health issues compared with those without DGBI in the general population. This was especially true for those with painful DGBI, DGBI in several anatomical regions, high somatic symptom severity or high psychological distress. In addition, we demonstrated that male sex, fatigue, psychological distress, somatic symptom severity and the number of anatomical regions affected by DGBI were independent predictors of WPAI.
Subjects with painful DGBI had higher work productivity impairment in our study. This is in line with previous studies where abdominal pain in persons with IBS was found to affect work and school. 18 , 19 Pain has also been shown to impact work productivity in other diseases. A study on immune‐mediated inflammatory diseases (inflammatory bowel disease, multiple sclerosis and rheumatoid arthritis) and mental disorders (major depressive disorder and anxiety disorders) found significant associations between absenteeism, presenteeism and general activity impairment and impact of pain on well‐being and functioning, together with fatigue impact, depression and anxiety. 20 Treating pain successfully with a GnRH antagonist has been shown to reduce both absenteeism and presenteeism in patients with endometriosis, 21 while ergonomic interventions aimed at reducing work‐related musculoskeletal disorders were effective in treating pain but did not seem to affect work productivity. 22 , 23 We argue that the characteristics of pain related to endometriosis, primarily pelvic pain, could be closer to the pain experienced by persons with painful DGBI compared with pain related to work‐related musculoskeletal disorders. Thus, interventions aimed at reducing pain using different strategies in DGBI could help reduce both pain and work impairment.
We found differences in WPAI among the participating countries. The basis for this finding is probably multifactorial, and could not be assessed thoroughly in this study. Differences in work productivity among countries were seen in other conditions previously. van der Zee‐Neuen et al. 24 studied work productivity impairment in patients with rheumatoid arthritis in 17 countries and found that countries with higher human development index (HDI) scores and higher economic wealth (GDP) had lower absenteeism and higher presenteeism. This is in line with our findings for presenteeism, where Sweden had the highest levels of presenteeism and Poland the lowest, but we did not find the same pattern for absenteeism. In addition, differences in work culture and ability to take sick days as well as how the care in case of activity impairment (e.g., help in the household) and sick leave is organized in the different countries may also explain differences among countries.
Fatigue was one of the factors that we found to be independently associated with WPAI. In a recent study on work life in persons with IBS, fatigue was described as a prominent negative factor, affecting several aspects of work. 25 The effect of fatigue on work productivity in other non‐IBS DGBIs has not been reported previously and needs to be further examined. Psychological distress was also found to be independently associated with WPAI in subjects with DGBI. This has been shown previously for example, for IBS and GI‐specific anxiety. 6 , 15 With many DGBI being associated with mental disorders, and major depressive disorder being associated with both higher unemployment rates and higher absenteeism and presenteeism than the general population and among general workers, 26 it is difficult to determine from this study alone what drives the job loss. However, this was a population‐based study where both mental disorders and DGBI can occur in participants. This underscores the importance of a broad approach to the treatment of symptoms, not one restricted to the GI tract.
This study has some limitations. The questionnaire used for assessing work and activity impairment assesses impairment due to all health issues, not only health issues caused by DGBI, meaning that comorbidities as well as other health issues that were not assessed in this study all can contribute to the impairment found. Also, we were able to explain only part of the variance in WPAI. Detailed data on occupation, education and socioeconomic status were not collected, factors that can affect work and activity impairment and might be able to strengthen our regression models. In addition, the focus of the survey was on European countries, and only one Asian country was included, and large parts of the world were not covered, limiting the possibility of generalizing our findings globally. Furthermore, some selection bias, due to the fact that participants were rewarded with points that they could trade for gifts, cannot be totally excluded. An additional limitation of our study is that participants could not be evaluated with clinical investigations, and we do not have access to medical records, so in some cases their symptom could have been caused by an “organic” disease instead of DGBI. However, the inclusion of a checklist of history of organic diagnoses that might account for GI symptoms and our exclusion of such cases from the DGBI group partially compensated for this. The strengths of the study were several, including the large cohort, the uniform methodology, the high‐quality population‐based and multinational data collection, and the use of validated questionnaires.
In summary, this study demonstrates the impact that DGBI can have on work productivity and life activities and illustrates the need for more research in this field, both for all DGBI and for the effects of overlapping DGBI. Based on our findings, where fatigue, psychological distress and somatic symptom severity were found to be independently associated with work productivity impairment in persons with DGBI, we suggest that in the management of these individuals, attention should be paid to their broader mental and physical well‐being and not only to symptoms limited to the GI tract.
CONFLICT OF INTEREST STATEMENT
The authors have no relevant conflicts of interest for this study.
Supporting information
Supporting Information S1
ACKNOWLEDGMENTS
This study was conducted under the auspices of the Rome Foundation Research Institute. The study was funded, in part, by research grants from Ironwood, Shire, Allergan, and Takeda. The study in Israel was funded by Takeda‐Israel. None of the funders was involved in the planning, design, implementation, statistical analyses, or any other aspect of the study.
Frändemark Å, Törnblom H, Hreinsson JP, Andresen V, Benninga MA, Corazziari ES, et al. Work productivity and activity impairment in disorders of gut‐brain interaction: data from the Rome Foundation Global Epidemiology Study. United European Gastroenterol J. 2023;11(6):503–13. 10.1002/ueg2.12425
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from Rome Foundation Global Epidemiology Study, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Rome Foundation Global Epidemiology Study.
REFERENCES
- 1. Drossman DA, Chang L, Chey WD, Kellow J, Tack J, Whitehead WE. ROME IV: functional gastrointestinal disorders. Raleigh: The Rome Foundation; 2016. [Google Scholar]
- 2. Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38(9):1569–80. 10.1007/bf01303162 [DOI] [PubMed] [Google Scholar]
- 3. Roshandel D, Rezailashkajani M, Shafaee S, Zali MR. A cost analysis of functional bowel disorders in Iran. Int J Colorectal Dis. 2007;22(7):791–9. 10.1007/s00384-006-0226-2 [DOI] [PubMed] [Google Scholar]
- 4. Nag A, Martin SA, Mladsi D, Olayinka‐Amao O, Purser M, Vekaria RM. The humanistic and economic burden of chronic idiopathic constipation in the USA: a systematic literature review. Clin Exp Gastroenterol. 2020;13:255–65. 10.2147/ceg.s239205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vakil N, Stelwagon M, Shea EP, Miller S. Symptom burden and consulting behavior in patients with overlapping functional disorders in the US population. United Eur Gastroenterol J. 2016;4(3):413–22. 10.1177/2050640615600114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Frändemark Å, Tornblom H, Jakobsson S, Simren M. Work productivity and activity impairment in irritable bowel syndrome (IBS): a multifaceted problem. Am J Gastroenterol. 2018;113(10):1540–9. 10.1038/s41395-018-0262-x [DOI] [PubMed] [Google Scholar]
- 7. Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation Global Study. Gastroenterology. 2021;160(1):99–114.e3. 10.1053/j.gastro.2020.04.014 [DOI] [PubMed] [Google Scholar]
- 8. Palsson OS, Whitehead WE, Van Tilburg MA, Chang L, Chey W, Crowell MD, et al. Development and validation of the Rome IV diagnostic questionnaire for adults. Gastroenterology. 2016;150(6):1481–91. 10.1053/j.gastro.2016.02.014 [DOI] [Google Scholar]
- 9. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–65. 10.2165/00019053-199304050-00006 [DOI] [PubMed] [Google Scholar]
- 10. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra‐brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–21. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- 11. Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4‐item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire‐4 (PHQ‐4) in the general population. J Affect Disord. 2010;122(1‐2):86–95. 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- 12. Kroenke K, Spitzer RL, Williams JB. The PHQ‐15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66. 10.1097/00006842-200203000-00008 [DOI] [PubMed] [Google Scholar]
- 13. Spitzer R, Kroenke K, Williams J. Instructions for patient health questionnaire (PHQ) and GAD‐7 measures; 1999. p. 1–9.
- 14. PROMIS Global‐10. https://www.codetechnology.com/blog/promis-global-10/
- 15. Goodoory VC, Ng CE, Black CJ, Ford AC. Impact of Rome IV irritable bowel syndrome on work and activities of daily living. Aliment Pharmacol Ther. 2022;56(5):844–56. 10.1111/apt.17132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Aziz I, Palsson OS, Törnblom H, Sperber AD, Whitehead WE, Simrén M. The prevalence and impact of overlapping Rome IV‐diagnosed functional gastrointestinal disorders on somatization, quality of life, and healthcare utilization: a cross‐sectional general population study in three countries. Am Coll Gastroenterol. 2018;113(1):86–96. 10.1038/ajg.2017.421 [DOI] [PubMed] [Google Scholar]
- 17. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Routledge; 2011. [Google Scholar]
- 18. Hellström PM, Saito YA, Bytzer P, Tack J, Mueller‐Lissner S, Chang L. Characteristics of acute pain attacks in patients with irritable bowel syndrome meeting Rome III criteria. Am J Gastroenterol. 2011;106(7):1299–307. 10.1038/ajg.2011.78 [DOI] [PubMed] [Google Scholar]
- 19. Niemyjska S, Ukleja A, Lawinski M. Evaluation of irritable bowel syndrome symptoms amongst Warsaw University Students. Pol Przegl Chir. 2015;87(5):252–9. 10.1515/pjs-2015-0050 [DOI] [PubMed] [Google Scholar]
- 20. Enns MW, Bernstein CN, Kroeker K, Graff L, Walker JR, Lix LM, et al. The association of fatigue, pain, depression and anxiety with work and activity impairment in immune mediated inflammatory diseases. PLoS One. 2018;13(6):e0198975. 10.1371/journal.pone.0198975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pokrzywinski RM, Soliman AM, Chen J, Snabes MC, Coyne KS, Surrey ES, et al. Achieving clinically meaningful response in endometriosis pain symptoms is associated with improvements in health‐related quality of life and work productivity: analysis of 2 phase III clinical trials. Am J Obstet Gynecol. 2020;222(6):592.e1–e10. 10.1016/j.ajog.2019.11.1255 [DOI] [PubMed] [Google Scholar]
- 22. Sweeney K, Mackey M, Spurway J, Clarke J, Ginn K. The effectiveness of ergonomics interventions in reducing upper limb work‐related musculoskeletal pain and dysfunction in sonographers, surgeons and dentists: a systematic review. Ergonomics. 2021;64(1):1–38. 10.1080/00140139.2020.1811401 [DOI] [PubMed] [Google Scholar]
- 23. Waongenngarm P, Areerak K, Janwantanakul P. The effects of breaks on low back pain, discomfort, and work productivity in office workers: a systematic review of randomized and non‐randomized controlled trials. Appl Ergon. 2018;68:230–9. 10.1016/j.apergo.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 24. van der Zee‐Neuen A, Putrik P, Ramiro S, Keszei AP, Hmamouchi I, Dougados M, et al. Large country differences in work outcomes in patients with RA–an analysis in the multinational study COMORA. Arthritis Res Ther. 2017;19(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Frändemark Å, Törnblom H, Simrén M, Jakobsson S. Maintaining work life under threat of symptoms: a grounded theory study of work life experiences in persons with Irritable Bowel Syndrome. BMC Gastroenterol. 2022;22(1):73. 10.1186/s12876-022-02158-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lerner D, Henke RM. What does research tell us about depression, job performance, and work productivity? J Occup Environ Med. 2008;50(4):401–10. 10.1097/jom.0b013e31816bae50 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
The data that support the findings of this study are available from Rome Foundation Global Epidemiology Study, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Rome Foundation Global Epidemiology Study.


