Abstract
Background:
Meniscal and chondral damage is common in the revision anterior cruciate ligament (ACL) reconstruction patient.
Hypothesis/Purpose:
The purpose of this study was to determine if either meniscal and/or articular cartilage (AC) pathology at the time of revision ACL surgery significantly influences a patient’s outcome at 6-year follow-up.
Study Design:
Cohort study
Methods:
Revision ACL reconstruction patients were prospectively enrolled between 2006–2011. Baseline demographics, surgical technique, pathology, and treatment, and four validated patient-reported outcome instruments (IKDC, KOOS, WOMAC, Marx activity rating score) were collected. Patients were followed up at 6 years and asked to complete the identical set of outcome instruments. Regression analysis assessed the meniscal and AC pathology risk factors for clinical outcomes 6 years after revision ACL reconstruction.
Results:
1234 patients were enrolled (716 [58%] males; median age of 26 years). Surgeons reported pathology at the time of revision surgery in the medial meniscus (45%), lateral meniscus (36%), medial femoral condyle (MFC; 43%), lateral femoral condyle (LFC; 29%), medial tibial plateau (MTP; 11%), lateral tibial plateau (LTP; 17%), patella (30%), and trochlea (21%). Six-year follow-up was obtained on 79% (980/1234). Meniscal pathology as well as AC pathology (in the MFC, LFC, LTP, trochlea, and patella) were found to be significant drivers of poorer outcomes at 6 years. The most consistent factors driving outcome were having a medial meniscus excision (either prior to revision surgery or at the time of revision surgery) and patellofemoral AC pathology. Six-year Marx activity levels were negatively impacted by having either a repair/excision of the medial meniscus (odds ratio [OR] range =1.45–1.72; p≤0.04) or having grade 3–4 patellar chondrosis (OR=1.72; p=0.04). Meniscal pathology occurring prior to the index revision surgery negatively affected all KOOS subscales except for sports/recreation (p<0.05). Articular cartilage pathology significantly impaired all KOOS subscales (p<0.05). Lower baseline outcome scores, higher BMI, being a smoker, and incurring a subsequent surgery all significantly increased the odds of reporting poorer clinical outcomes at 6 years.
Conclusion:
Meniscal and chondral pathology at the time of revision ACL reconstruction have continued significant detrimental effects on patient-reported outcomes 6 years after revision surgery.
INTRODUCTION
Revision anterior cruciate ligament (ACL) reconstruction remains a difficult clinical problem. Orthopaedic surgeons continue to be challenged not only by the technical aspects of returning ligamentous stability to the knee, but also the difficulty of optimizing clinical results to meet the expectations of the patients. Results of revision ACL reconstructions rarely match the clinical results of primary ACL reconstructions. Revision ACL patient cohorts commonly report outcomes inferior with regards to reoperations, graft failure and patient-reported outcomes as compared to primary ACL reconstructions.1,3,5,9,14,19,21
The Multicenter ACL Revision Study (MARS) was developed to try to identify both the modifiable and non-modifiable factors that contribute to results following revision ACL reconstruction. A better understanding of this complex clinical issue would allow us to potentially change our technical approach and better counsel patients as to appropriate expectations following these surgeries. This prospective multi-surgeon and multicenter group has assembled a large cohort of patients which allows us to critically assess results and predictors. One area of significant concern amongst our group was the level of meniscal and chondral damage noted at the time of revision ACL reconstruction in these patients. Previous analysis of these patients at the time of enrollment and revision reconstruction noted that ~90% had sustained either meniscal or chondral (modified Outerbridge Grade 2 or greater) damage.10 Both meniscal and chondral damage was noted in 59% of these patients. Only 9% had neither meniscal nor chondral damage. These patients underwent previous analysis at 2-year follow-up and findings demonstrated that the strongest predictors of outcome were the presence of trochlear groove chondral damage and the history of a previous lateral meniscectomy.10 The current study was undertaken to evaluate this same cohort of patients at minimum 6 years after revision ACL reconstruction to determine if later follow-up showed broader, more significant impact on outcome as the articular cartilage potentially deteriorated further with time. We hypothesized that additional meniscal and chondral factors would impact the outcomes of these patients 6 years following their revision ACL reconstruction.
METHODS
Study Design
The MARS Group was assembled in cooperation with the American Orthopaedic Society for Sports Medicine as a collection of 83 sports medicine fellowship-trained surgeons working at 52 sites. The surgeons are a mix of academic and private practitioners. Surgeon inclusion criteria included maintaining an active institutional review board (IRB) approval, completing a training session that integrated articular cartilage and meniscus agreement studies, reviewing the study design and patient inclusion criteria, and reviewing the surgeon questionnaire. Surgeons could perform the ACL revision surgery according to their own practice preferences. If an allograft was chosen for reconstruction the surgeon was required to utilize a Musculoskeletal Transplant Foundation graft to standardize and record allograft preparation methods.
The objective of this consortium has been to assess both the short- and long-term outcomes following revision ACL reconstruction, and to determine how the initial factors at the time of revision surgery may influence and predict disease progression. This study design involves a longitudinal prospective cohort for whom we currently have baseline, 2-year, and 6-year follow-up.
Setting and Participants
After Institutional Review Board approval from each institution, 1234 patients with documented ACL reconstruction failure that underwent revision ACL reconstruction surgery qualified for and were consented to be in this study (Figure 1). This multicenter consortium began patient enrollment in 2006 and ended in 2011. Study inclusion criteria were revision ACL reconstructions performed by a MARS surgeon on ACL deficient patients that had failed a previous ACL reconstruction as identified by either magnetic resonance imaging, physical exam (positive pivot shift and Lachman test), KT-1000 testing demonstrating > 5mm side-to-side difference, functional instability or arthroscopic confirmation.
Figure 1.
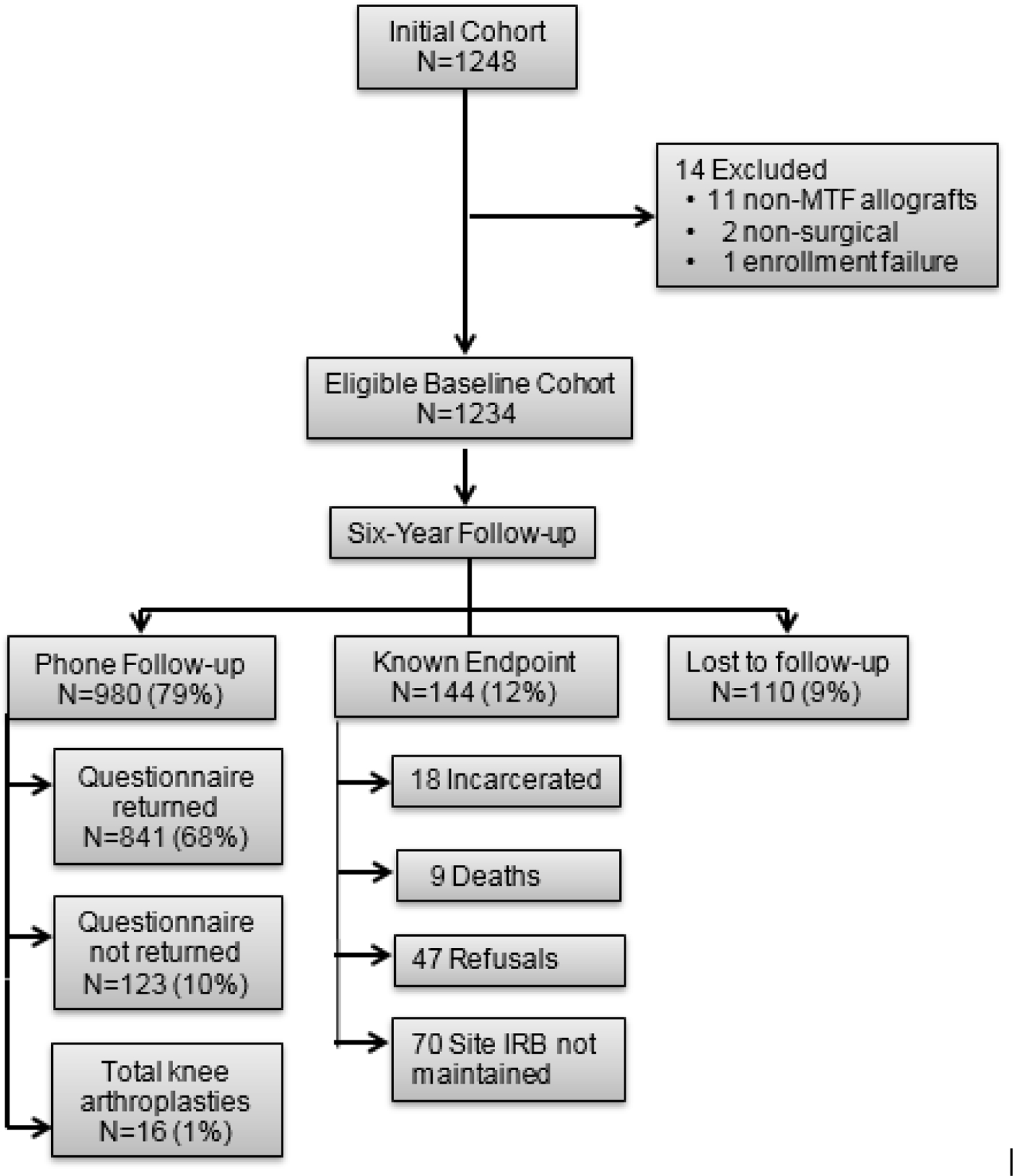
Patient Enrollment Flow Diagram
Data Sources
After informed consent was obtained, each patient completed a self-reported questionnaire examining demographics, injury characteristics, sports participation history, and health status prior to their revision ACL reconstruction surgery. Within this questionnaire, each participant completed a series of validated general and knee-specific outcome instruments, including the Knee Injury and Osteoarthritis Outcome Score (KOOS), the International Knee Documentation Committee (IKDC) Subjective form, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the Marx activity rating scale. Surgeons filled out a questionnaire that included physical exam findings, surgical technique utilized and the intra-articular findings and surgical management of meniscal and chondral damage. Chondral damage was described using the modified Outerbridge system,6 with worse grade defined in this study as being a grade 2 or higher. Meniscal injuries were classified by location (i.e. medial, lateral; anterior, posterior, anterior + posterior) and partial versus complete tears, while treatment was recorded as no treatment, repair, resection, or other (i.e., abrade and trephine, meniscal transplant, etc.). For the purposes of this study, “previous” or “prior” refers to meniscal or articular cartilage injuries sustained and documented before the time of the ACL revision surgery. This was determined either by previous operative reports or by noting surgical changes consistent with previous meniscal resection. “Current” refers to meniscal or articular cartilage damage noted for the first time at the time of ACL revision surgery.
Completed data forms were mailed from each participating site to our data coordinating center. Data from both the patient and surgeon questionnaires were scanned with Teleform™ software (OpenText; Waterloo, Ontario, Canada) utilizing optical character recognition, and the scanned data was verified and exported to a master database. A series of custom logical error and quality control checks were subsequently performed prior to data analyses.
Patient Follow-up
At 6 years, the same questionnaire was administered as at baseline and at 2-year follow-up. Patients were also contacted by phone or email to determine if subsequent graft failure and/or any additional knee surgery had occurred.
Variables and Statistical Analysis
Descriptive statistics of each of the baseline patient and surgical characteristics were examined and reported. The effect of the independent (risk factor) variables on the, 1) outcome measures of IKDC, KOOS, WOMAC, and the Marx activity scale were modeled with proportional odds logistic regression, and 2) binary outcome of subsequent surgery (yes/no) was modeled with logistic multivariable regression. Odds ratios (OR) and 95% confidence intervals (CI) were obtained by exponentiation the parameter estimates. Both patient and previous and current surgical-related covariates were included and controlled for in the models. Patient-related covariates included sex (male/female), age at the time of their revision ACL reconstruction, body mass index (BMI), smoking status (non-smoker, quit, current), education level (years), baseline Marx activity level, and baseline outcome measures (IKDC, KOOS, WOMAC, Marx). Covariates related to previous surgical information included time (in years) since the patient’s last ACL reconstruction, number of revisions, previous ACL reconstruction on the contralateral knee (yes/no), previous meniscal surgery (medial and lateral; yes/no), previous articular cartilage surgeries (yes/no), prior graft type (autograft vs. allograft), prior graft source (bone-patellar tendon-bone [BTB] vs. soft tissue), surgeon’s opinion of failure (traumatic, technical, biologic, other, combination), and surgeon’s revision of his/her own failure (yes/no). Covariates related to current surgical information included surgeon years of experience, mechanism of injury (non-traumatic, traumatic, contact, non-contact), surgical technique (1 incision transtibial, 1 incision anteromedial portal, 2 incision), graft type (BTB autograft, soft tissue autograft, BTB allograft, soft tissue allograft), meniscal pathology and treatment (medial, lateral; normal/no tear, no treatment for tear, repair, excision), articular cartilage pathology (normal/grade 1, grade 2, grade 3, grade 4 in each of the six compartments – medial femoral condyle [MFC], lateral femoral condyle [LFC], medial tibial plateau [MTP], lateral tibial plateau [LTP], patella, and trochlea), articular cartilage treatment (none, chondroplasty, other), and biological enhancement used (yes/no). Due to the low frequency counts of grade 4 chondral lesions in the MTP, LTP, patella, and trochlear compartments, these grades were combined with their respective grade 3 compartment lesion to form a combined “grade 3 to 4” variable for each of these 4 compartments for analysis purposes. Three-knot restricted cubic splines were used for all continuous covariates to allow for nonlinear relationships with the outcomes.
The changes in outcome scores between baseline and 6 years were assessed through a comparison and medians and interquartile ranges (IQR) at each time point and tested with Kruskal-Wallis tests. Additionally, minimal clinically important differences (MCID) were examined between time points. MCID for IKDC was 11 points, 8–10 points for each of the 5 KOOS subscales, 8–10 points for the WOMAC, and 2 points for Marx activity scale. Alpha was set at 0.05 for all statistical tests. Multiple imputation using predictive mean matching was used to address missing baseline data. Specifically, the “smoking status” and “time since the patient’s last ACL reconstruction” variables were missing in 14 cases and were imputed. The six-year data was not imputed. The Hmisc and rms packages of the open source R statistical software (https://www.r-project.org) was used for statistical analysis.
RESULTS
The study cohort included 1234 patients who met the inclusion criteria, with 716 (58%) males and a median cohort age of 26 years (Appendix 1). Surgeons noted previous pathology (prior to the revision ACL reconstruction) in the medial meniscus (38%), lateral meniscus (21%), and articular surfaces (12%) at the time of revision surgery. Surgeons reported current pathology (defined as the time of the revision ACL reconstruction) in the medial meniscus (45%), lateral meniscus (36%), medial femoral condyle (MFC; 43%), lateral femoral condyle (LFC; 29%), medial tibial plateau (MTP; 11%), lateral tibial plateau (LTP; 17%), patella (30%), and trochlea (21%).
Six-year follow-up was obtained on 79% (980/1234; Figure 1). Previous (prior to revision ACL reconstruction) and current (at the time of revision ACL reconstruction) meniscal pathology, as well as current AC pathology (in the MFC, LFC, LTP, trochlea, and patella) were found to be significant drivers of poorer outcomes at six years. The most consistent factors driving outcome in revision patients at 6 years were either a previous or current excision of the medial meniscus and patellofemoral AC pathology.
Marx Activity Levels
Six-year Marx activity levels were negatively impacted by having either a repair or an excision of the medial meniscus (odds ratio [OR] range=1.45–1.72; 95% CI=1.02, 2.70; p≤0.04; Table 1) or having grade 3–4 patellar chondrosis at the time of the revision ACL reconstruction (OR=1.72; 95% CI= 1.02, 2.94; p=0.04; Table 1). Conversely, 6-year activity levels were significantly higher if a patient had either a lateral meniscus repair or excision at the time of their revision ACL reconstruction (OR=1.44–2.13; 95% CI=1.02, 3.88; p≤0.04; Table 1).
Table 1.
Significant Odds Ratios (95% CI) for Individual Meniscus and Articular Cartilage Variables
| KOOS | WOMAC | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Structure | Comparison | Worse Outcome | Marx | Symptoms | Pain | ADL | Sports/Rec | QoL | IKDC | Stiffness | Pain | ADL | |
| MENISCAL STATUS (Previous pathology prior to enrollment) |
Medial | No tear vs. excised | excised | 1.45 (1.05, 2.04) p=0.025 | 1.67 (1.19, 2.33) p=0.003 | 1.41 (1.01, 2.00) p=0.046 | 1.41 (1.00, 1.96) p=0.047 | 1.56 (1.12, 2.17) p=0.009 | 1.59 (1.12, 2.22) p=0.008 | 1.41 (1.01, 2.00) p=0.046 | |||
| No tear vs. unstable, not healed repair | no tear | 2.07 (1.05, 4.06) p=0.035 | 2.04 (1.03, 4.05) p=0.042 | 2.07 (1.09, 3.90) p=0.025 | 2.06 (1.04, 4.10) p=0.039 | 2.04 (1.03, 4.05) p=0.042 | |||||||
| Lateral | No tear vs. excised | excised | |||||||||||
| No tear vs. stable/healed repair | stable/healed repair | 2.78 (1.12, 6.67) p=0.027 | 2.70 (1.11, 6.67) p=0.029 | 3.85 (1.52, 9.09) p=0.004 | 2.86 (1.12, 7.14) p=0.028 |
||||||||
| MENISCAL STATUS (at time of revision ACLR) |
Medial | normal vs. repair | repair | 1.72 (1.12, 2.70) p=0.013 | |||||||||
| normal vs. excision | excision | 1.45 (1.02, 2.04) p=0.038 | 1.59 (1.13, 2.22) p=0.007 | 1.63 (1.16, 2.30) p=0.005 | 1.62 (1.16, 2.27) p=0.005 | ||||||||
| Lateral | normal vs. repair | normal | 2.13 (1.17, 3.88) p=0.028 | ||||||||||
| normal vs. excision | normal | 1.44 (1.02, 2.03) p=0.039 | |||||||||||
| ARTICULAR CARTILAGE STATUS (Previous) | yes vs. no | ||||||||||||
| ARTICULAR CARTILAGE STATUS (at time of revision ACLR) | MFC | Normal/G1 vs. G2 | G2 | 1.61 (1.12, 2.27) p=0.009 | |||||||||
| Normal/G1 vs. G4 | G4 | 1.92 (1.06, 3.45) p=0.032 | |||||||||||
| LFC | Normal/G1 vs. G2 | G2 | 1.56 (1.05, 2.33) p=0.027 | ||||||||||
| Normal/G1 vs. G4 | G4 | 1.92 (1.00, 3.66) p=0.050 | 2.41 (1.27, 4.57) p=0.007 | 1.88 (1.05, 3.39) p=0.035 | 1.91 (1.00, 3.66) p=0.050 | ||||||||
| MTP | Normal/G1 vs. G3/4 | G3/4 | |||||||||||
| LTP | Normal/G1 vs. G3/4 | G3/4 | 2.22 (1.12, 4.55) p=0.022 | ||||||||||
| Patella | Normal/G1 vs. G2 | G2 | 1.54 (1.06, 2.22) p=0.021 | 1.52 (1.05, 2.22) p=0.026 | |||||||||
| Normal/G1 vs. G3/4 | G3/4 | 1.72 (1.02, 2.94) p=0.042 | 1.69 (1.02, 2.86) p=0.042 | 2.17 (1.30, 3.70) p=0.003 | |||||||||
| Trochlea | Normal/G1 vs. G3/4 | G3/4 | 1.89 (1.18, 3.03) p=0.009 | 2.00 (1.25, 3.23) p=0.004 | 2.22 (1.35, 3.70) p=0.002 | ||||||||
Key: Cells are populated as Odd Ratios (95% confidence intervals) and p-values where significant
An empty cell indicates that the particular knee rating at the top of the column was not signficantly affected by meniscal and articular surface conditions. Light shaded cells indicate result was counter-intuitive to initial hypothesis.
ADL=activities of daily living; G1=grade 1; G2=Grade 2; G3=grade 3; G4=grade 4; G3/4=grades 3–4
LFC=lateral femoral condyle; LTP=lateral tibial plateau; MFC=medial femoral condyle; MTP=medial tibial plateau; Sports/Rec=sports and recreation; QoL=quality of life
IKDC
Six-year IKDC scores were negatively impacted in patients who had previous medial meniscus surgery prior to the index revision ACL reconstruction, as well as having patellar chondrosis documented at the time of the index revision ACL reconstruction (Table 1). Specifically, a medial meniscal repair or excision performed prior to their revision ACL reconstruction was an independent predictor of having a poorer 6-year IKDC score (OR range=1.56–2.07; 95% CI=1.09, 3.90; p≤0.03). Grade 2 patellar chondrosis documented at the time of the index revision ACL reconstruction was also a significant predictor or lower 6-year IKDC scores (OR=1.52; 95% CI: 1.05, 2.22; p=0.026).
KOOS
Meniscal pathology negatively affected all KOOS subscales except for sports/recreation (p<0.05; Table 1). Specifically, having a medial meniscectomy (performed either prior to the index revision ACL reconstruction or at the time of the revision ACL surgery) resulted in significantly lower KOOS symptom (OR range=1.45–1.59; 95% CI: 1.05, 2.22; p≤0.03), pain (OR range=1.63–1.67; 95% CI: 1.16, 2.33; p<0.01), ADL (OR=1.41; 95% CI: 1.01, 2.00; p=0.046), and quality-of-life (OR range=1.41–1.62; 95% CI: 1.0, 2.27; p≤0.05) scores at 6 years. Patients who had a previous lateral meniscal repair prior to the index revision ACL reconstruction resulted in significantly lower KOOS symptom (OR=2.78; 95% CI: 1.12, 6.67; p=0.027), pain (OR=2.70; 95% CI: 1.11, 6.67; p=0.029), and quality-of-life (OR=3.85; 95% CI: 1.52, 9.09; p=0.004) scores at 6 years.
Articular cartilage pathology significantly impaired all KOOS subscales (p<0.05; Table 1). The 6-year KOOS symptoms subscale was negatively impacted by MFC (OR=1.61; 95% CI: 1.12, 2.27; p=0.009) and trochlear (OR=1.89; 95% CI: 1.18, 3.03; p=0.009) chondrosis. The KOOS pain subscale was negatively impacted by LFC (OR=1.56; 95% CI: 1.05, 2.33; p=0.027) and patellar (OR=1.69; 95% CI: 1.02, 2.86; p=0.042) chondrosis. The KOOS ADL subscale was significantly affected by LFC (OR=1.92; 95% CI: 1.00, 3.66; p=0.005) chondrosis. The KOOS sports/recreation subscale was significantly affected by LFC (OR=2.41; 95% CI: 1.27, 4.57; p=0.007), LTP (OR=2.22; 95% CI: 1.12, 4.55; p=0.022) and trochlear (OR=2.0; 95% CI: 1.25, 3.23; p=0.004) chondrosis. The 6-year KOOS quality-of-life subscale was negatively impacted by LFC (OR=1.88; 95% CI: 1.05, 3.39; p=0.035), and patellar chondrosis (OR=1.54; 95% CI: 1.06, 2.22; p=0.021).
WOMAC
Six-year WOMAC scores were negatively impacted by having a previous medial meniscal excision (prior to the index revision ACL reconstruction), and MFC, LFC, patellar and trochlear chondrosis documented at the time of the index revision ACL reconstruction (Table 1). Previous medial meniscectomies (OR=1.41; 95% CI: 1.01, 2.00; p=0.046) and grade 4 LFC chondrosis (OR=1.91; 95% CI: 1.00, 3.66; p=0.05) were predictive of significantly lower six-year WOMAC ADL scores. Previous medial meniscectomies (OR=1.59; 95% CI: 1.12, 2.22; p=0.008), previous lateral meniscal repairs (OR=2.86; 95% CI: 1.12, 7.14; p=0.028), and grades 3–4 patellar chondrosis (OR=2.17; 95% CI: 1.30, 3.70; p=0.003) were predictive of significantly lower six-year WOMAC pain scores. Grade 4 MFC chondrosis (OR=1.92; 95% CI: 1.06, 3.45; p=0.032) and grades 3–4 trochlear chondrosis (OR=2.22; 95% CI: 1.35, 3.70; p=0.002) and were predictive of significantly lower WOMAC stiffness scores.
Subsequent Surgeries
Predictors of having a subsequent surgery by 6 years included patients who had a medial meniscal repair done at the time of their index revision ACL reconstruction (OR=2.2; 95% CI: 1.27, 3.88; p=0.005), compared with patients who had no medial meniscal pathology at the time of their revision surgery. Similarly, patients who had either grade 2 MFC chondrosis (OR=1.7; 95% CI: 1.04, 2.82; p=0.035), or grade 3–4 MTP chondrosis (OR=3.0; 95% CI: 1.07, 8.54; p=0.037) at the time of the index revision ACL reconstruction were 1.7 to 3 times more likely to have a subsequent surgery by their 6-year follow-up.
Secondary Covariates
Lower baseline outcome scores, higher BMI, and being a smoker at the time of the revision surgery significantly increased the odds of reporting consistently poorer clinical outcomes at 6 years (Table 2).
Table 2.
Significant Odds Ratios (95% CI) for Secondary Variables in Model
| KOOS | WOMAC | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Comparison | Worse Outcome | Marx | Symptoms | Pain | ADL | Sports/Rec | QoL | IKDC | Stiffness | Pain | ADL | |
| Baseline Patient-Reported Outcome Score | lower baseline score | 2.54 (1.69, 3.80) p<0.0001 | 2.98 (2.34, 3.79) p<0.0001 | 3.17 (2.49, 4.04) p<0.0001 | 5.09 (3.67, 7.06) p<0.0001 | 2.43 (1.94, 3.03) p<0.0001 | 2.23 (1.80, 2.77) p<0.0001 | 2.62 (2.11, 3.25) p<0.0001 | 2.53 (1.93, 3.31) p<0.0001 | 3.27 (2.40, 4.47) p<0.0001 | 5.09 (3.67, 7.07) p<0.0001 | |
| Patient Demographics | ||||||||||||
| Age (years) | older age | 3.03 (1.89, 5.00) p<0.0001 | ||||||||||
| Sex | male vs. female | females | 2.22 (1.64, 2.94) p<0.0001 | 1.35 (1.01, 1.79) p=0.044 | ||||||||
| Smoking status | never vs. current | current smoker | 2.08 (1.16, 3.70) p=0.013 | 3.13 (1.82, 5.56) p<0.001 | 3.45 (2.00, 5.88) p<0.001 | 3.85 (2.27, 6.67) p<0.001 | 3.13 (1.79, 5.26) p<0.001 | 3.85 (2.27, 6.67) p<0.001 | 4.17 (2.44, 7.14) p<0.001 | 3.33 (1.96, 5.88) p<0.001 | 3.23 (1.89, 5.56) p<0.001 | 3.85 (2.27, 6.67) p<0.001 |
| Body mass index (BMI) | higher BMI | 1.04 (1.01–1.07) p=0.014 | 1.04 (1.01–1.07) p=0.008 | 1.06 (1.03–1.10) p<0.001 | 1.04 (1.01–1.07) p=0.003 | 1.04 (1.01–1.07) p=0.012 | 1.06 (1.03–1.09) p<0.001 | 1.05 (1.02–1.09) p=0.001 | 1.06 (1.03–1.10) p<0.001 | |||
| Baseline Marx Activity Level | lower baseline Marx score | 2.54 (1.69, 3.80) p<0.0001 | 1.65 (1.09, 2.50) p=0.003 |
|||||||||
| Previous Surgical Information | ||||||||||||
| Time since last ACLR (years) | less time since last ACLR | 1.87 (1.23, 2.86) p=0.037 | 1.60 (1.02, 2.51) p=0.021 | |||||||||
| Previous ACLR on contra. knee | no vs. yes | yes | 1.61 (1.03, 2.56) p=0.035 | 1.67 (1.08, 2.63) p=0.023 | ||||||||
Key: An empty cell indicates that the particular knee rating at the top of the column was not signficantly affected by meniscal and articular surface conditions. ACLR= anterior cruciate ligament reconstruction; ADL = activities of daily living; contra = contralateral; QoL = quality of life; sports/rec = sports and recreation
DISCUSSION
Meniscal and chondral damage, both prior to the time of the revision ACL surgery, as well as at the time of revision ACL surgery, have a significant detrimental impact upon patient-reported outcomes six years later. Previous (prior to revision ACL reconstruction) and current (at the time of revision ACL reconstruction) meniscal pathology, as well as current articular cartilage pathology (in the MFC, LFC, LTP, trochlea, and patella) were found to be significant drivers of poorer patient-reported outcomes (Marx, IKDC, KOOS and WOMAC), as well as subsequent surgery outcomes at 6 years follow-up. This was a broader, but different pattern than seen at two years follow-up in this cohort.10
This longitudinal cohort study design allows us to analyze how various baseline factors impact outcomes over time. There is little comparative data from the literature as only 5 previous studies with 159 patients have a minimum 5-year follow-up to revision ACL reconstruction,4,7,8,11,12 so the most relevant comparison is to our previously published 2-year results10. Meniscal and/or chondral damage did not predict Marx activity level at 2-year follow-up. At six years, Marx activity levels were significantly lower in patients who underwent repair or excision of the medial meniscus and in patients with grade 3 or 4 patella chondrosis. Conversely, 6-year activity levels were higher in patients who underwent a lateral meniscus repair or excision. The latter was counterintuitive as lateral meniscus excision might be expected to promote articular cartilage deterioration and decreased activity after 6 years. We are uncertain as to why the intuitively expected deterioration of Marx activity level results with lateral meniscus excision did not occur by 6 years and in fact predicted higher activity levels. Less surprising is the fact that repair of a lateral meniscus tear had reasonable results at 6 years. Planned follow-up at 10 years will investigate this relationship further.
Lateral meniscus injury prior to the index revision ACL reconstruction, but not previous medial meniscus injury had been shown to impact 2-year outcomes (IKDC, all KOOS and WOMAC subscales).10 New meniscal pathology found at the time of revision reconstruction was not found to be a significant risk factor for KOOS, IKDC, or WOMAC scores at 2 years. However, at 6-year follow-up, both medial and lateral meniscal pathology prior to the index revision ACL reconstruction negatively affected all KOOS subscales in this cohort. These findings are consistent with previous literature reporting that meniscal pathology negatively impacts outcome scores in the revision ACL reconstruction setting.2,4,15,17,18 Anand et al. reported on 136 patients with mean 5-year follow-up.2 Patients with an intact medial meniscus had significantly higher KOOS-QOL scores at follow-up compared with the patients with medial meniscal pathology. Return to sport was not impacted by meniscal status. Webster et al. collected IKDC, KOOS-QOL, Marx, and SANE scores in 180 revision ACL patients with a mean follow-up of 4.6 years (range, 2–8 years).17 They reported that patients with medial meniscal pathology at the time of revision surgery had significantly lower functional and quality of life scores than patients without pathology. No difference was found in any outcome score between patients with and without lateral meniscal pathology.
In a separate study, Webster et al. investigated the outcomes of re-revisions in 128 young patients aged less than 25 years.18 In this study, the mean follow-up was 4.5 years (range, 2–9 years). Twenty-seven percent (35/128) of the patients had a third ACL injury by 2 years. Of the group who had graft re-ruptures, 70% had medial meniscal pathology (i.e, tear or previous repair/resection). They found a significant association between having medial meniscal pathology and sustaining a graft re-rupture (p=0.02). There was no association with graft re-rupture and lateral meniscal pathology or chondral pathology. They concluded that medial meniscal pathology and returning to high-risk sports are factors associated with re-revisions.
Our study found that meniscal and chondral pathology documented at the time of revision surgery are risk factors for incurring a subsequent surgery within 6 years. Specifically, patients who had a medial meniscal repair were over 2 times more likely to have a subsequent surgery occur when compared to patients who had no medial meniscal pathology at the time of their revision surgery. Similarly, patients who had grade 2 chondrosis in the MFC or grades 3–4 chondrosis in the MTP at the time of revision surgery were 1.7 to 3 times more likely to incur a subsequent surgery by their 6-year follow-up. These results are consistent with our previous work at two-year follow-up20 and are in concordance to published results from both primary as well as revision ACL reconstruction cohorts.13,16 Sullivan et al. reported on the predictors of subsequent surgery after primary ACL reconstruction.13 This cohort consisted of 3276 patients (56.3% male) with a median age of 23 years and a six-year follow-up rate of 91.5%. They found that having a medial meniscal repair at the time of index primary ACL surgery was an independent significant risk factor for incurring a subsequent meniscus-related surgery within six years. Similarly, Vindfeld et al. investigated the patient-related risks of inferior outcomes leading to revision surgery after ACL reconstruction.16 A total of 100 revision cases and 100 matched controls, with a median follow-up time of 11 years were included in the study. They demonstrated that a failed meniscal repair was among the significant factors which were associated with primary ACL reconstruction failure and was found to affect the risk of undergoing revision ACL surgery.
Chondral pathology has also been found to negatively impact patient outcomes in the mid-term follow-up revision setting.2,4,17 Anand et al. reported significantly lower 5-year Marx activity, KOOS-QOL, and IKDC scores for patients with initial grade 3 or 4 chondral damage at the time of revision surgery, compared to those with grade 0, 1, or 2 changes.2 Similarly, Webster et al. reported significantly reduced functional scores (IKDC, KOOS-QOL, Marx activity and SANE scores) and lower rates of return to sport after 5 years in revision ACL patients who had grade 3 or 4 chondral damage noted at the time of their revision surgery.17 Boyle et al. followed 43 revision ACL patients over a mean follow-up of 9 years (range, 5–15 years), and found a statistically significant correlation between increasing age and worse functional outcome scores in the Lysholm in those who had grade 3 or 4 chondral damage.4 Patients who had grade 3 or 4 chondral damage showed a reduction of about 25 points in the Lysholm score for every 10 years increase in age.
In our previous 2-year analysis, having grade 3 or 4 articular cartilage chondrosis of the trochlea at the time of revision ACL reconstruction consistently resulted in significantly poorer outcomes across all outcome measures (IKDC, KOOS, and WOMAC subscales), except for activity level (which was not affected).10 In the current 6-year study, chondral pathology continued to negatively impact 6-year outcome measures, with the addition of activity level (Table 1). This negative impact spanned across all AC regions, except for the MTP region. Because overall activity levels continue to trend downwards for this cohort, patients may be decreasing their activity to control their pain level.
There are strengths and limitations to this study. Patients were not brought back to each clinic to have a physician’s assessment of the knee performed, nor were follow-up x-rays or MRI images taken as part of the study protocol. As such, we cannot verify the integrity of the ACL in those that did not undergo subsequent MRI, physician, or surgical verification. Similarly, we can only report on the meniscal and chondral findings at the time of the revision ACL reconstruction, and not at the time of 6-year follow-up. It is likely that the meniscal and/or chondral pathology worsened over the course of follow-up in a subset of these patients, and this study could not determine this progression. Strengths include the prospective enrollment and size of the cohort which is the largest ever followed at six years after revision reconstruction. The retained follow-up at six years strengthens our conclusions. The multiple sites and surgeons make the findings generalizable to the sports medicine surgeon and the revision ACL patient.
CONCLUSIONS
Meniscal and chondral pathology in the knee at the time of revision ACL reconstruction have significant detrimental effects on patient-reported outcomes 6 years after surgery. The impact is more wide-ranging at 6 years following revision ACL surgery compared to 2-year follow-up. Medial meniscal repair/excision and patellofemoral chondrosis predict a lower activity level at 6 years, although lateral meniscal repair/excision predicts a higher activity level at 6 years. Independent predictors of lower IKDC, KOOS and WOMAS scores at 6-year follow-up include chondrosis and a history of medial meniscus repair prior to the revision ACL reconstruction. Longer term follow-up of this cohort will further characterize the role of meniscal and articular cartilage pathology in predicting outcomes of this procedure.
What is known about the subject:
Both meniscal and articular cartilage pathology is common in the revision ACL setting and more common than that found in primary ACL reconstructions. Both pathologies independently contribute to worse significantly outcomes at 2 years following a revision ACL reconstruction.
What this study adds to existing knowledge:
This study provides evidence from a prospective cohort that meniscal pathology, particularly medial meniscectomies, as well as articular cartilage damage noted at the time of the revision surgery predict significantly worse outcomes 6 years following revision ACL reconstruction, as measured by patient reported outcome measures.
Acknowledgements:
This project was funded by grant No. 5R01-AR060846 from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases.
We express our appreciation to the late Barton Mann, PHD (AOSSM, Rosemont, IL USA), Timothy M. Hosea, MD (University Orthopaedic Associates LLC, Princeton, NJ USA), and Allen F. Anderson, MD (Tennessee Orthopaedic Alliance, Nashville, TN USA) whose contribution to this work was of great significance.
We would also like to thank Jack T. Andrish, MD (Cleveland Clinic, Cleveland, OH USA), John D. Campbell, MD (Bridger Orthopedic and Sports Medicine, Bozeman, MT USA) and Diane L. Dahm, MD (Mayo Clinic, Rochester, MN USA) for their effort and leadership on this project. All are enjoying a well-deserved and happy retirement after many years of dedication to the advancement of orthopedics.
Appendix 1. Baseline Cohort Characteristics at the Time of Revision ACL Reconstruction
| Patient Characteristics | Cohort (n=1234) |
|---|---|
| Sex • Males • Females |
58% (716) 42% (518) |
| Age, years | 26 (20, 34) |
| Body Mass Index (BMI) | 25.1 (22.6, 28.6) |
| Smoking Status • Non-smoker • Quit • Current • Blank/missing |
77% (949) 13% (157) 9% (109) 2% (19) |
| Education Level, years | 14 (12, 16) |
| Activity Level (Marx, 0–16 points) | 11 (4, 16) |
| Previous Surgery Information (prior to the revision ACL reconstruction) | |
| Time since last ACL reconstruction, years | 3.3 (1.4, 8.0) |
| Number of Revisions • 1 • 2 • 3 or more |
87% (1077) 11% (131) 2% (26) |
| Previous ACL reconstruction on the contralateral knee • No • Yes |
90% (1110) 10% (124) |
| Previous Medial Meniscal Surgery • No • Yes, repair healed/stable • Yes, repair not healed/unstable • Yes, excision |
62% (765) 3% (32) 6% (69) 30% (368) |
| Previous Lateral Meniscal Surgery • No • Yes, repair healed/stable • Yes, repair not healed/unstable • Yes, excision • Blank/missing |
79% (979) 2% (30) 2% (23) 16% (198) <1% (4) |
| Previous Articular Cartilage Surgeries • No • Yes |
88% (1086) 12% (148) |
| Prior Graft Type • Autograft • Allograft • Both autograft + allograft • Unknown/missing |
68% (834) 29% (354) 3% (34) <1% (12) |
| Prior Graft Source • BTB • Soft tissue • BTB + soft tissue • Unknown/missing |
52% (642) 38% (473) <1% (11) 9% (108) |
|
Current Surgical Information
(at the time of the revision ACL reconstruction) | |
| Surgeon Experience, years | 13 (8, 18) |
| Graft Type • Autograft • Allograft • Both autograft + allograft |
48% (598) 49% (599) 3% (37) |
| Graft Source • BTB • Soft tissue • Other (i.e. both, quadriceps-bone, etc) |
50% (616) 47% (580) 3% (37) |
| Graft Type x Source • BTB autograft • Soft tissue autograft • BTB allograft • Soft tissue allograft • Other (i.e. both autograft + allograft, both BTB + soft tissue, quad-bone grafts, etc) |
26% (325) 20% (251) 23% (289) 25% (302) 5% (67) |
| Medial Meniscus Pathology/Treatment • Normal (no tear) • No treatment for tear • Repair • Excision • Other |
55% (680) 2% (29) 13% (166) 27% (336) 2% (23) |
| Lateral Meniscus Pathology/Treatment • Normal (no tear) • No treatment for tear • Repair • Excision • Other |
64% (790) 5% (58) 5% (63) 26% (316) <1% (7) |
| LFC Articular Cartilage Pathology • Normal/grade 1 • Grade 2 • Grade 3 • Grade 4 |
71% (881) 15% (189) 8% (99) 5% (65) |
| MFC Articular Cartilage Pathology | |
| Normal/grade 1 • Grade 2 • Grade 3 • Grade 4 • Blank/missing |
57% (699) 24% (295) 13% (166) 6% (72) <1% (2) |
| LTP Articular Cartilage Pathology • Normal/grade 1 • Grade 2 • Grade 3 • Grade 4 |
83% (1019) 13% (162) 4% (46) <1% (7) |
| MTP Articular Cartilage Pathology • Normal/grade 1 • Grade 2 • Grade 3 • Grade 4 |
89% (1098) 8% (94) 2% (21) 1% (16) |
| Patella Articular Cartilage Pathology • Normal/grade 1 • Grade 2 • Grade 3 • Grade 4 |
70% (867) 19% (239) 10% (119) <1% (9) |
| Trochlea Articular Cartilage Pathology • Normal/grade 1 • Grade 2 • Grade 3 • Grade 4 |
79% (979) 9% (105) 8% (94) 4% (55) |
| Biologic Enhancement Used • No • Yes • Blank/missing |
91% (1117) 9% (112) <1% (5) |
Key: continuous variables are listed as median (25% quartile, 75% quartile); categorical variables are listed as percentage (frequency); ACL = anterior cruciate ligament; BMI = body mass index; BTB = bone-patellar tendon-bone; LFC = lateral femoral condyle; LTP = lateral tibial plateau; MFC = medial femoral condyle; MTP = medial tibial plateau.
Contributor Information
Rick W. Wright, Vanderbilt University, Nashville, TN USA.
Laura J. Huston, Vanderbilt University, Nashville, TN USA.
Amanda K. Haas, Washington University in St. Louis, St. Louis, MO USA.
Jacquelyn S. Pennings, Vanderbilt University, Nashville, TN USA.
Christina R. Allen, Yale University, New Haven, CT USA.
Daniel E. Cooper, W.B. Carrell Memorial Clinic, Dallas, TX USA.
Thomas M. DeBerardino, The San Antonio Orthopaedic Group, San Antonio, TX USA.
Warren R. Dunn, Texas Orthopedic Hospital, Houston, TX USA.
Brett (Brick) A. Lantz, Slocum Research and Education Foundation, Eugene, OR USA.
Kurt P. Spindler, Cleveland Clinic, Cleveland, OH USA.
Michael J. Stuart, Mayo Clinic, Rochester, MN USA.
John P. Albright, University of Iowa Hospitals and Clinics, Iowa City, IA USA.
Annunziato (Ned) Amendola, Duke University, Durham, NC USA.
Jack T. Andrish, Cleveland Clinic, Cleveland, OH USA.
Christopher C. Annunziata, Commonwealth Orthopaedics & Rehabilitation, Arlington, VA USA.
Robert A. Arciero, University of Connecticut Health Center, Farmington, CT USA.
Bernard R. Bach, Jr, Rush University Medical Center, Chicago, IL USA.
Champ L. Baker, III, The Hughston Clinic, Columbus, GA USA.
Arthur R. Bartolozzi, 3B Orthopaedics, University of Pennsylvania Health System, Philadelphia, PA USA.
Keith M. Baumgarten, Orthopedic Institute, Sioux Falls, SD USA.
Jeffery R. Bechler, University Orthopaedic Associates LLC, Princeton, NJ USA.
Jeffrey H. Berg, Town Center Orthopaedic Associates, Reston, VA USA.
Geoffrey A. Bernas, State University of New York at Buffalo, Buffalo, NY.
Stephen F. Brockmeier, University of Virginia, Charlottesville, VA USA.
Robert H. Brophy, Washington University in St. Louis, St. Louis, MO USA.
Charles A. Bush-Joseph, Rush University Medical Center, Chicago, IL USA.
J. Brad Butler, Orthopedic and Fracture Clinic, Portland, OR USA.
John D. Campbell, Bridger Orthopedic and Sports Medicine, Bozeman, MT USA.
James L. Carey, University of Pennsylvania, Philadelphia, PA USA.
James E. Carpenter, University of Michigan, Ann Arbor, MI USA.
Brian J. Cole, Rush University Medical Center, Chicago, IL USA.
Jonathan M. Cooper, HealthPartners Specialty Center, St. Paul, MN USA.
Charles L. Cox, Vanderbilt University, Nashville, TN USA.
R. Alexander Creighton, University of North Carolina Medical Center, Chapel Hill, NC USA.
Diane L. Dahm, Mayo Clinic, Rochester, MN USA.
Tal S. David, Synergy Specialists Medical Group, San Diego, CA USA.
David C. Flanigan, The Ohio State University, Columbus, OH USA.
Robert W. Frederick, The Rothman Institute/Thomas Jefferson University, Philadelphia, PA USA.
Theodore J. Ganley, Children’s Hospital of Philadelphia, Philadelphia, PA USA.
Elizabeth A. Garofoli, Washington University in St. Louis, St. Louis, MO USA
Charles J. Gatt, Jr, University Orthopaedic Associates LLC, Princeton, NJ USA.
Steven R. Gecha, Princeton Orthopaedic Associates, Princeton, NJ USA.
James Robert Giffin, Fowler Kennedy Sport Medicine Clinic, University of Western Ontario, London Ontario, Canada.
Sharon L. Hame, David Geffen School of Medicine at UCLA, Los Angeles, CA USA.
Jo A. Hannafin, Hospital for Special Surgery, New York, NY USA.
Christopher D. Harner, University of Texas Health Center, Houston, TX USA.
Norman Lindsay Harris, Jr, Grand River Health in Rifle, CO USA.
Keith S. Hechtman, UHZ Sports Medicine Institute, Coral Gables, FL USA.
Elliott B. Hershman, Lenox Hill Hospital, New York, NY USA.
Rudolf G. Hoellrich, Slocum Research and Education Foundation, Eugene, OR USA.
David C. Johnson, National Sports Medicine Institute, Leesburg, VA USA.
Timothy S. Johnson, National Sports Medicine Institute, Leesburg, VA USA.
Morgan H. Jones, Cleveland Clinic, Cleveland, OH USA.
Christopher C. Kaeding, The Ohio State University, Columbus, OH USA.
Ganesh V. Kamath, University of North Carolina Medical Center, Chapel Hill, NC USA.
Thomas E. Klootwyk, Methodist Sports Medicine, Indianapolis, IN USA.
Bruce A. Levy, Mayo Clinic Rochester, MN USA.
C. Benjamin Ma, University of California, San Francisco, CA USA.
G. Peter Maiers, II, Methodist Sports Medicine Center, Indianapolis, IN USA.
Robert G. Marx, Hospital for Special Surgery, New York, NY USA.
Matthew J. Matava, Washington University in St. Louis, St. Louis, MO USA.
Gregory M. Mathien, Knoxville Orthopaedic Clinic, Knoxville, TN USA.
David R. McAllister, David Geffen School of Medicine at UCLA, Los Angeles, CA USA.
Eric C. McCarty, University of Colorado Denver School of Medicine, Denver, CO USA.
Robert G. McCormack, University of British Columbia/Fraser Health Authority, British Columbia, Canada.
Bruce S. Miller, University of Michigan, Ann Arbor, MI USA.
Carl W. Nissen, Connecticut Children’s Medical Center, Hartford, CT USA.
Daniel F. O’Neill, Littleton Regional Healthcare, Littleton, NH USA.
Brett D. Owens, Warren Alpert Medical School, Brown University, Providence, RI USA.
Richard D. Parker, Cleveland Clinic, Cleveland, OH USA.
Mark L. Purnell, Aspen Orthopedic Associates, Aspen, CO USA.
Arun J. Ramappa, Beth Israel Deaconess Medical Center, Boston, MA USA.
Michael A. Rauh, State University of New York at Buffalo, Buffalo, NY USA.
Arthur C. Rettig, Methodist Sports Medicine, Indianapolis, IN USA.
Jon K. Sekiya, University of Michigan, Ann Arbor, MI USA.
Kevin G. Shea, Intermountain Orthopaedics, Boise, ID USA.
Orrin H. Sherman, NYU Hospital for Joint Diseases, New York, NY USA.
James R. Slauterbeck, University of South Alabama, Mobile, AL USA.
Matthew V. Smith, Washington University in St. Louis, St. Louis, MO USA.
Jeffrey T. Spang, University of North Carolina Medical Center, Chapel Hill, NC USA.
LTC Steven J. Svoboda, Keller Army Community Hospital, United States Military Academy, West Point, NY USA.
Timothy N. Taft, University of North Carolina Medical Center, Chapel Hill, NC USA.
Joachim J. Tenuta, Albany Medical Center, Albany, NY USA.
Edwin M. Tingstad, Inland Orthopaedic Surgery and Sports Medicine Clinic, Pullman, WA USA.
Armando F. Vidal, University of Colorado Denver School of Medicine, Denver, CO USA.
Darius G. Viskontas, Royal Columbian Hospital, New Westminster, BC Canada.
Richard A. White, Fitzgibbon’s Hospital, Marshall, MO USA.
James S. Williams, Jr, Cleveland Clinic, Euclid, OH USA.
Michelle L. Wolcott, University of Colorado Denver School of Medicine, Denver, CO USA.
Brian R. Wolf, University of Iowa Hospitals and Clinics, Iowa City, IA USA.
James J. York, Orthopaedic and Sports Medicine Center, LLC, Pasedena, MD.
REFERENCES
- 1.Ahn JH, Lee YS, Ha HC. Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am J Sports Med 2008;36(10):1889–1895. [DOI] [PubMed] [Google Scholar]
- 2.Anand BS, Feller JA, Richmond AK, Webster KE. Return-to-sport outcomes after revision anterior cruciate ligament reconstruction surgery. Am J Sports Med 2016;44(3):580–584. [DOI] [PubMed] [Google Scholar]
- 3.Andriolo L, Filardo G, Kon E, et al. Revision anterior cruciate ligament reconstruction: clinical outcome and evidence for return to sport. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 2015;23(10):2825–2845. [DOI] [PubMed] [Google Scholar]
- 4.Boyle C, Pagoti R, Eng KH, McMahon SE, Nicholas R. Revision ACL reconstruction with autograft: long-term functional outcomes and influencing factors. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie 2019;29(1):157–161. [DOI] [PubMed] [Google Scholar]
- 5.Cristiani R, Engstrom B, Edman G, Forssblad M, Stalman A. Revision anterior cruciate ligament reconstruction restores knee laxity but shows inferior functional knee outcome compared with primary reconstruction. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 2019;27(1):137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curl WW, Krome J, Gordon ES, et al. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy : the journal of arthroscopic & related surgery: official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 1997;13(4):456–460. [DOI] [PubMed] [Google Scholar]
- 7.Franceschi F, Papalia R, Del Buono A, et al. Two-stage procedure in anterior cruciate ligament revision surgery: a five-year follow-up prospective study. International Orthopaedics 2013;37(7):1369–1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liden M, Ejerhed L, Sernert N, et al. The course of the patellar tendon after reharvesting its central third for ACL revision surgery: a long-term clinical and radiographic study. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 2006;14(11):1130–1138. [DOI] [PubMed] [Google Scholar]
- 9.Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med 2012;40(7):1551–1557. [DOI] [PubMed] [Google Scholar]
- 10.MARS Group. Meniscal and articular cartilage predictors of clinical outcome following revision anterior cruciate ligament reconstruction. Am J Sports Med 2016;44(7):1671–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayr HO, Willkomm D, Stoehr A, et al. Revision of anterior cruciate ligament reconstruction with patellar tendon allograft and autograft: 2- and 5-year results. Archives of Orthopaedic and Trauma Surgery 2012;132(6):867–874. [DOI] [PubMed] [Google Scholar]
- 12.Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K. Revision anterior cruciate ligament reconstruction with hamstring tendon autograft: 5- to 9-year follow-up. Am J Sports Med 2006;34(10):1604–1614. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan JP, Huston LJ, Zajichek A, et al. Incidence and predictors of subsequent surgery after anterior cruciate ligament reconstruction: a 6-year follow-up study. Am J Sports Med 2020;48(10):2418–2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Svantesson E, Hamrin Senorski E, Kristiansson F, et al. Comparison of concomitant injuries and patient-reported outcome in patients that have undergone both primary and revision ACL reconstruction-a national registry study. Journal of Orthopaedic Surgery and Research 2020;15(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trojani C, Sbihi A, Djian P, et al. Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 2011;19(2):196–201. [DOI] [PubMed] [Google Scholar]
- 16.Vindfeld S, Strand T, Solheim E, Inderhaug E. Failed meniscal repairs after anterior cruciate ligament reconstruction increases risk of revision surgery. Orthopaedic Journal of Sports Medicine 2020;8(10):2325967120960538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Webster KE, Feller JA, Kimp A, Devitt BM. Medial meniscal and chondral pathology at the time of revision anterior cruciate ligament reconstruction results in inferior mid-term patient-reported outcomes. Knee surgery , sports traumatology, arthroscopy: official journal of the ESSKA. 2018;26(4):1059–1064. [DOI] [PubMed] [Google Scholar]
- 18.Webster KE, Feller JA, Kimp AJ, Whitehead TS. Revision anterior cruciate ligament reconstruction outcomes in younger patients: medial meniscal pathology and high rates of return to sport are associated with third ACL injuries. Am J Sports Med 2018;46(5):1137–1142. [DOI] [PubMed] [Google Scholar]
- 19.Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. Journal of Bone and Joint Surgery American volume 2012;94(6):531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wright RW, Huston LJ, Haas AK, et al. Meniscal repair in the setting of revision anterior cruciate ligament reconstruction: results from the MARS cohort. Am J Sports Med 2020;48(12):2978–2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright RW, Johnson L, Brophy RH, et al. Revision anterior cruciate ligament reconstruction outcomes at a minimum of 5-year follow-up: a systematic review. J Knee Surg 2019;32(3):218–221. [DOI] [PubMed] [Google Scholar]


