Abstract
Although pulmonary embolism (PE)-related mortality rate has decreased because of prompt diagnosis and effective therapy use, acute PE remains a potentially lethal disease. Due to its increasing prevalence, clinicians should pay attention to diagnosing and managing patients with acute PE. Echocardiography is the most commonly used method for diagnosing and managing acute PE; it also provides clues about hemodynamic instability in an emergency situation. It has been validated in the early risk stratification and impacts management strategies for treating acute PE. In hemodynamically unstable patients with acute PE, echocardiographic detection of right ventricular dysfunction is an indication for administering thrombolytics. In this review article, we discuss the role of echocardiography in the diagnosis and management of patients with acute PE.
Keywords: Pulmonary embolism, Echocardiography, Diagnosis, Management
INTRODUCTION
Pulmonary embolism (PE), a form of venous thromboembolism (VTE), is the third leading cause of cardiovascular death in Western countries, and its prevalence has increased over time [1–4]. Approximately 75 to 269 cases of VTE occur per 100,000 individuals yearly in Western Europe, North America, Australia, and southern Latin America [5]. In Korea, the annual incidence of VTE was 53.7 cases per 100,000 person-years in 2018, increasing from 32.8 in 2014, exhibiting a tendency to gradually increase over years [6]. Additionally, the annual incidence rate of PE also increased with age, with an approximately 26-fold higher rate in individuals aged ≥ 75 years than in those aged < 35 years. These data demonstrate the importance of PE in the aging population of Korea as well as Europe, further suggesting that PE will increasingly burden healthcare systems globally in the coming years [7]. PE contributes to approximately one-third of this VTE burden. Although prompt diagnosis and appropriate treatment have reduced all-cause and PE-related mortality, acute PE remains a potentially lethal disease, with a current mortality of approximately 5% to 7% [8,9].
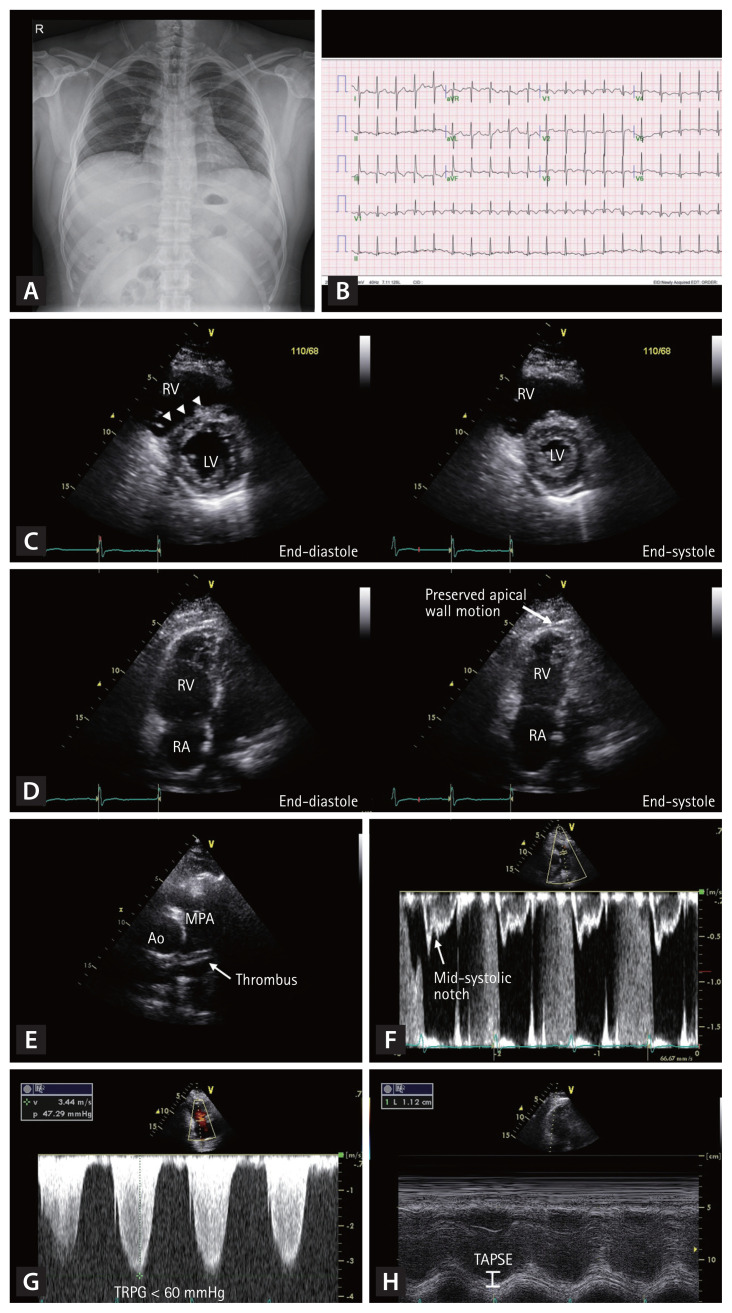
Herein, we illustrate a typical case of acute PE that a clinician may encounter in routine clinical practice. In this case, a 33-year-old man with a history of myotonic dystrophy presented with worsening dyspnea for 5 days. His initial blood pressure was 108/64 mmHg, heart rate was 120/min, respiratory rate was 25/min, and body temperature was 36.5°C. On physical examination, lung sounds were clear, and no cardiac murmur was found. The initial chest radiograph was normal (Fig. 1A). However, the electrocardiogram demonstrated sinus tachycardia and an S wave in lead I (S1), Q wave in lead III (Q3), T wave inversion in lead III (T3), and precordial leads V1–3 (Fig. 1B). We performed echocardiography to evaluate the cause of dyspnea. Echocardiography showed a D-shaped left ventricle (LV) (Fig. 1C), McConnell’s sign (Fig. 1D), linear thrombus in the main pulmonary artery (Fig. 1E), echocardiographic signs of the increased pulmonary arterial systolic pressure (Fig. 1F and 1G), and decreased right ventricular (RV) contractility assessed by tricuspid annular plane systolic excursion (TAPSE) (Fig. 1H). After the echocardiographic examination, we suspected the presence of acute PE and confirmed the diagnosis using contrast-enhanced computed tomography (CT) of the chest. After subcutaneous injection of low-molecular-weight heparin for 5 days, the patient was treated with oral warfarin therapy. Although echocardiographic examination was not used to confirm the diagnosis in this case, it provided diagnostic clues regarding the patient’s clinical presentation.
Figure 1.
Typical case of an acute pulmonary embolism (PE) in a 33-year-old man. The initial chest radiography is normal (A). The electrocardiogram demonstrates sinus tachycardia, S wave in lead I (S1), Q wave in the lead III (Q3), T wave inversion in lead III (T3), and precordial leads V1–3 (B). Echocardiography shows D-shaped left ventricle (C, arrowheads), McConnell’s sign (D, arrow), thrombus in the main pulmonary artery (E), mid-systolic notching in the pulsed-wave Doppler tracing of right ventricular outflow tract (F), increased maximal velocity of tricuspid regurgitation (G), and decreased right ventricular contractility assessed by tricuspid annular plane systolic excursion (H). RV, right ventricle; LV, left ventricle; RA, right atrium; Ao, aorta; MPA, main pulmonary artery; TRPG, tricuspid valve peak systolic gradient; TAPSE, tricuspid annular plane systolic excursion.
Echocardiography is the most used imaging modality for evaluating and managing acute PE. Besides to give clues about other etiologies for chest pain or dyspnea, echocardiography can be used in the early risk stratification and impact management strategies in patients with acute PE. In addition, it can be used to predict prognosis in these patients. Throughout this review, we discuss the role of echocardiography in diagnosing and predicting outcomes in patients with signs or symptoms of PE. Further, we describe the impact of echocardiography on risk stratification and management strategies of PE.
RECOMMENDATION OF ECHOCARDIOGRAPHY IN RECENT TREATMENT GUIDELINES
Bedside echocardiography is indicated for diagnosing suspected acute PE in high-risk patients in the recent guidelines for the diagnosis and management of acute PE by the European Society of Cardiology (ESC, class I, level of evidence C) [10]. In addition, echocardiographic parameters are valuable markers for early risk stratification of patients with acute PE [10]. The presence of RV dysfunction assessed by echocardiography can be an indication for thrombolysis, particularly in patients with hemodynamic instability [10,11]. The American Heart Association guidelines indicate the presence of RV dysfunction in patients with RV dilatation (RV to LV end-diastolic diameter ratio [RV/LV ratio] > 0.9) or RV systolic dysfunction on echocardiographic studies [11]. However, in the ESC and American Society of Hematology guidelines, thrombolytic therapy is not indicated in patients with acute PE who are hemodynamically stable and do not have RV dysfunction [10,12].
ECHOCARDIOGRAPHIC FINDINGS IN PATIENTS WITH PE
Although computed tomography pulmonary angiography (CTPA) with contrast enhancement and lung ventilation/ perfusion scan are the gold standard for diagnosing acute PE [10], echocardiography plays a key role in its diagnosis. As the most available, and noninvasive diagnostic modality that does not require contrast agents or radiation, echocardiography is a feasible imaging modality for diagnosing acute PE.
Acute PE causes RV pressure overload, potentially leading to RV systolic dysfunction. Echocardiography can provide several clues to rule in or rule out acute PE, including regional wall motion abnormality in patients with acute myocardial infarction and dissecting aortic flaps in patients with acute aortic dissection in an emergency setting. We searched all published articles in English focused on the calculation of diagnostic accuracy of transthoracic echocardiography in the PubMed (National Library of Medicine, www.pubmed.gov) database. We selected 13 studies reporting quantitative data and reanalyzed diagnostic power. Table 1 shows the diagnostic power of several echocardiographic signs for acute PE. An illustration showing parameters found in patients with PE is presented in Fig. 2.
Table 1.
Diagnostic accuracy of echocardiographic signs for pulmonary embolism
| Sign | Study | No. of PE (+) | No. of true positive | Sensitivity, % | Specificity, % | PPV, % | NPV, % |
|---|---|---|---|---|---|---|---|
| 60/60 sign | Grifoni et al. (1998) [15] | 63 | 26 | 41 | 91 | 84 | 57 |
| Kurzyna et al. (2002) [16] | 67 | 17 | 25 | 94 | 89 | 38 | |
| Lodato et al. (2008) [17] | 41 | 9 | 22 | 69 | 53 | 36 | |
| Afonso et al. (2019) [13] | 187 | 95 | 51 | 96 | 93 | 70 | |
| Total | 358 | 147 | 41 | 91 | 89 | 47 | |
|
| |||||||
| RV hypokinesis | Jackson et al. (2000) [18] | 27 | 6 | 22 | 99 | 86 | 82 |
| Ceccarelli et al. (2003) [19] | 37 | 7 | 18 | 97 | 88 | 49 | |
| Chen et al. (2006) [20] | 56 | 33 | 59 | 100 | 100 | 80 | |
| Dresden et al. (2014) [21] | 30 | 10 | 33 | 99 | 91 | 85 | |
| Tuzovic et al. (2016) [22] | 51 | 21 | 41 | 100 | 100 | 51 | |
| Total | 201 | 77 | 34 | 99 | 96 | 71 | |
|
| |||||||
| McConnell’s sign | Kurzyna et al. (2002) [16] | 67 | 13 | 19 | 100 | 100 | 38 |
| Lodato et al. (2008) [17] | 41 | 6 | 16 | 96 | 86 | 44 | |
| Dresden et al. (2014) [21] | 30 | 6 | 20 | 100 | 100 | 83 | |
| Daley et al. (2017) [26] | 32 | 4 | 13 | 97 | 57 | 80 | |
| Afonso et al. (2019) [13] | 187 | 97 | 52 | 97 | 90 | 82 | |
| Total | 357 | 126 | 35 | 98 | 94 | 62 | |
|
| |||||||
| RVEDD > 27 mm | Nazeyrollas et al. (1996) [31] | 27 | 19 | 90 | 86 | 79 | 80 |
| Jackson et al. (2000) [18] | 27 | 11 | 41 | 88 | 48 | 84 | |
| Chen et al. (2006) [20] | 56 | 50 | 89 | 89 | 83 | 93 | |
| Lodato et al. (2008) [17] | 41 | 23 | 56 | 73 | 77 | 51 | |
| Total | 103 | 48 | 68 | 86 | 74 | 82 | |
|
| |||||||
| RV/LV ratio > 1.0 | Grifoni et al. (1998) [15] | 63 | 24 | 38 | 93 | 86 | 56 |
| Bova et al. (2003) [33] | 65 | 20 | 31 | 94 | 80 | 65 | |
| Lodato et al. (2008) [17] | 41 | 27 | 66 | 77 | 82 | 59 | |
| Dresden et al. (2014) [21] | 30 | 15 | 50 | 98 | 88 | 88 | |
| Tuzovic et al. (2016) [22] | 51 | 43 | 84 | 16 | 62 | 38 | |
| Daley et al. (2017) [26] | 32 | 12 | 38 | 85 | 40 | 83 | |
| Total | 282 | 141 | 50 | 86 | 70 | 72 | |
|
| |||||||
| Paradoxical septal motion | Nazeyrollas et al. (1996) [31] | 31 | 12 | 39 | 90 | 75 | 65 |
| Grifoni et al. (1998) [15] | 63 | 15 | 24 | 96 | 88 | 52 | |
| Jackson et al. (2000) [18] | 27 | 5 | 19 | 98 | 71 | 81 | |
| Ceccarelli et al. (2003) [19] | 37 | 13 | 35 | 97 | 93 | 55 | |
| Chen et al. (2006) [20] | 56 | 16 | 29 | 96 | 80 | 69 | |
| Lodato et al. (2008) [17] | 41 | 11 | 27 | 81 | 67 | 44 | |
| Dresden et al. (2014) [21] | 30 | 8 | 27 | 100 | 100 | 84 | |
| Daley et al. (2017) [26] | 32 | 10 | 31 | 94 | 59 | 83 | |
| Total | 317 | 90 | 28 | 96 | 78 | 71 | |
|
| |||||||
| Pulmonary hypertension (TR Vmax > 2.7 m/sec) | Jackson et al. (2000) [18] | 27 | 5 | 19 | 94 | 45 | 81 |
| Bova et al. (2003) [33] | 55 | 28 | 51 | 88 | 74 | 72 | |
| Ceccarelli et al. (2003) [19] | 37 | 26 | 70 | 70 | 74 | 66 | |
| Chen et al. 2(2006) [20] | 56 | 27 | 48 | 83 | 63 | 72 | |
| Lodato et al. (2008) [17] | 41 | 23 | 56 | 38 | 59 | 36 | |
| Total | 216 | 109 | 50 | 82 | 66 | 71 | |
|
| |||||||
| Thrombi in RV/PA | Grifoni et al. (1998) [15] | 63 | 3 | 3 | 100 | 100 | 47 |
| Jackson et al. (2000) [18] | 27 | 0 | 100 | 78 | |||
| Chen et al. (2006) [20] | 56 | 2 | 4 | 100 | 100 | 63 | |
| Total | 146 | 5 | 4 | 100 | 100 | 69 | |
|
| |||||||
| RV strain | Grifoni et al. (1998) [15] | 63 | 31 | 49 | 87 | 82 | 59 |
| Kurzyna et al. (2002) [16] | 67 | 54 | 81 | 45 | 75 | 54 | |
| Ceccarelli et al. (2003) [19] | 37 | 24 | 65 | 67 | 71 | 61 | |
| Chen et al. (2006) [20] | 56 | 44 | 79 | 68 | 60 | 84 | |
| Lodato et al. (2008) [17] | 41 | 24 | 59 | 85 | 86 | 56 | |
| Total | 264 | 177 | 67 | 71 | 72 | 65 | |
PE, pulmonary embolism; PPV, positive predictive value; NPV, negative predictive value; RV, right ventricle; RVEDD, right ventricular end-diastolic dimension; LV, left ventricle; TR Vmax, maximal velocity of tricuspid valve regurgitation; PA, pulmonary artery.
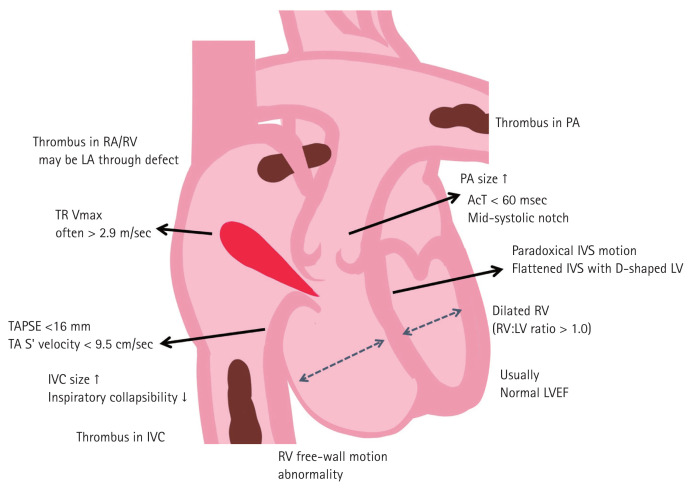
Figure 2.
Schematic illustration of echocardiographic findings can be found in acute pulmonary embolism. RA, right atrium; RV, right ventricle; LA, left atrium; TR Vmax, maximal velocity of tricuspid regurgitation; TAPSE, tricuspid annular plane systolic excursion; TA, tricuspid annulus; IVC, inferior vena cava; PA, pulmonary artery; AcT, acceleration time of right ventricular outflow tract; IVS, interventricular septum; LV, left ventricle; LVEF, left ventricular ejection fraction.
The “60/60” sign
The “60/60 sign” is defined as a pulmonary flow acceleration time < 60 ms in the presence of a tricuspid regurgitation (TR) pressure gradient of < 60 mmHg or a TR velocity < 3.9 m/sec, a Doppler echocardiographic PE sign based on a distorted RV ejection pattern. The pulsed wave Doppler-derived systolic flow velocity curve pattern in the RV outflow tract reflects the pulmonary arterial pressure level. The presence of short acceleration time and mid-systolic deceleration with a notched pattern is considered diagnostic of severe pulmonary hypertension; however, these patterns have also been observed in acute PE. Early systolic notching on the pulmonary Doppler flow tracing was found in 92% of patients with massive or submassive PE, and it was superior to McConnell’s sign in PE diagnosis [13].
However, with a relatively mild increase in systolic pulmonary arterial pressure, the most disturbed systolic flow velocity curve was found in patients with acute PE who manifested the shortest acceleration time and early mid-systolic deceleration. Whenever short acceleration time (< 60 ms) is found in patients with no more than a moderate increase in the TR pressure gradient (< 60 mmHg) as assessed by Doppler echocardiography, acute PE should be strongly suspected (specificity 98%, sensitivity 48%) [14]. In our re-analysis, the presence of the “60/60” sign had a sensitivity of 41% and a specificity of 91% in detecting acute PE in 358 patients (Table 1) [13,15–17].
Decreased RV free wall motion and systolic dysfunction
In patients with acute PE, RV hypokinesis can be observed. However, it can also be observed in patients with RV infarction. Its sensitivity and specificity were 34% and 99%, respectively, in our analysis of 201 patients with acute PE (Table 1) [18–22]. The presence of pulmonary hypertension in patients with acute PE helps to distinguish this finding from that in RV infarction [23].
Patients with acute PE show decreased RV free wall motion with preserved RV apical motion (McConnell’s sign), which is suggestive of acute PE [24]. Initially, McConnell et al. [24] reported that McConnell’s sign could diagnose acute PE with a sensitivity of 77% and a specificity of 94%. However, several studies reported that this finding was present in approximately 35% of 357 patients with acute PE (Table 1) [13,16,17,21,25,26]. The combination of the “60/60” and McConnell signs increased the sensitivity without compromising the specificity of echocardiographic acute PE diagnosis in a cohort of patients with a high prevalence of previous cardiorespiratory disorders [16].
There are several echocardiographic markers of RV systolic dysfunction. Decreased TAPSE may be present in patients with acute PE [27]. A TAPSE < 1.6 cm was associated with higher pulmonary arterial pressure, higher incidence of RV dilatation and free wall hypokinesis. In addition, a tricuspid annular systolic velocity < 10 cm/sec, derived from Doppler tissue imaging of the lateral tricuspid annulus, is another RV systolic dysfunction marker [28]. Midventricular peak systolic strains of RV using speckle-tracking echocardiography provide objective findings of decreased RV free wall motion [29]. These strain values improved with the resolution of regional wall motion abnormality. However, these echocardiographic parameters have low sensitivity for detecting acute PE as stand-alone findings. Moreover, these indices may be normal in hemodynamically stable patients with PE [30].
RV dilatation
RV dilatation could occur due to increased RV afterload; it can be diagnosed when the RV basal diameter is > 42 mm and the RV diameter at the midlevel is > 35 mm [28]. Right ventricular end-diastolic dimension (RVEDD) > 27 mm was found in 68% of 103 patients with acute PE (Table 1) [17,18,20,31]. However, its positive predictive value was only 74%.
Furthermore, an RV/LV ratio > 1.0 indicates RV dilatation [32]. It can be found in about 27.4% of patients with acute PE [25]. In one prospective study with 146 patients, RV dilatation on bedside echocardiography had high specificity (98%) and poor sensitivity (50%) in detecting PE [21]. PE diagnosis was more sensitive in younger patients or patients without evidence of lung diseases, including chronic pulmonary obstructive disease. The presence of an RV/LV ratio > 1.0 showed a sensitivity of 50% and a specificity of 86% in 282 patients with acute PE (Table 1) [15,17,21,22,26,33].
Morphology and motion of the interventricular septum
Patients with RV pressure overload can have a flattened or bowed interventricular septum (IVS) toward the LV at end-diastole and end-systole. In the parasternal short axis view, the LV becomes a D-shaped cavity as the IVS flattens and loses its convexity due to increased RV pressure during diastole [34]. Paradoxical septal motion on echocardiography, along with RV dilatation, RV hypokinesis, McConnell’s sign (RV free wall hypokinesis with apical sparing), and increased TR velocities, are evidences of RV dysfunction [15]. In a prospective observational study of 146 patients with moderate- to high-risk of PE or confirmed PE, advanced RV dysfunction signs, such as paradoxical septal motion, RV hypokinesis, and McConnell’s sign on bedside echocardiography had a high specificity for PE diagnosis. However, these had low sensitivity similar to RV dilatation and increased the pretest probability of a diagnosis before a definitive imaging test [21]. In addition, this study suggests that signs of advanced RV dysfunction were associated with a higher thrombus burden. These findings were more significant in patients with more proximal emboli, such as the saddle, lobar, and mainstem emboli in the pulmonary arterial bed. In our analysis, a paradoxical septal motion was observed in 90 of 317 patients with acute PE, with a sensitivity of 28% and a specificity of 96% (Table 1) [15,17–21,26,31].
Pulmonary hypertension
Pulmonary hypertension is high blood pressure affecting the pulmonary arteries. In patients with acute PE, increased total pulmonary resistance originates from mechanical obstruction of the pulmonary arteries and humoral factors secreted due to hypoxia [35]. The method of choice for noninvasive estimation of pulmonary arterial pressure is continuous wave Doppler measurement of the peak velocity of the regurgitant jet across the tricuspid valve (maximal velocity of tricuspid regurgitation [TR Vmax]). Based on the simplified Bernoulli equation and straightforward pathophysiological concepts, this method proved highly reliable in numerous cardiovascular diseases [36]. Grifoni et al. [15] reported that documenting a RV-to-atrial pressure gradient > 30 mmHg (equivalent to a TR Vmax > 2.7 m/sec) on echocardiography was poorly sensitive but highly specific in patients undergoing evaluation for possible PE. In a previous study evaluating the diagnostic utility of various noninvasive investigations for PE compared with CTPA, pulmonary hypertension on echocardiography showed a high sensitivity (83%) and positive predictive value (86%) in patients with clinically suspected PE [37]. Other studies reported similar findings in various clinical situations. In a prospective cohort study of emergency department patients with suspected PE, elevated pulmonary artery or RV systolic pressure (> 44 mmHg) had a sensitivity of 8% and a specificity of 96%, with a moderate possibility of a positive ratio (4.0) [18]. Nazeyrollas et al. [31] reported a possibility of a positive ratio ranging from 3.9 to 5.1 in an intensive care setting. In contrast, a normal TR Vmax < 2.5 m/sec is usually found in normal controls than in patients with acute PE, helping in ruling out and the decision-making on further invasive testing [31,38]. In our analysis involving 216 patients with acute PE, its sensitivity and specificity were 50% and 82%, respectively (Table 1) [17–20,33].
Visualization of emboli in the right heart and pulmonary arteries
Emboli, usually originating from deep vein thrombi, can be found anywhere in the inferior and superior venae cavae, right atrium (RA), RV, and pulmonary arteries. Since thrombi form in deep veins, emboli are usually elongated in shape. Sometimes, emboli from tumors or myxomas can be round in shape [18,20,39]. In one study with 130 patients with acute PE, RA thrombi were found in 23 (18%) [40]. In another study with 1,113 patients with acute PE, the incidence of right heart thrombi was 3.8% (42 patients) on baseline echocardiography [41]. The presence of mobile right heart thrombi was associated with acute PE in about 97% of cases, showing a high mortality rate of approximately 44% [41,42]. Right heart thrombi were found in five (4%) of 146 patients with acute PE (Table 1) [15,18,20]. However, its specificity and positive predictive value were 100%, suggesting that the presence of mobile thrombi can confirm PE. Furthermore, the presence of mobile RA thrombi or mobile RA thrombi prolapsed into the RV, particularly in patients with echocardiographic signs of RV pressure overload, can be a confirmative sign of acute PE.
Echocardiographic signs of RV strain
Echocardiographic RV strain parameters include RV dilatation (RVEDD > 30 mm at the apical four-chamber view), Mc-Connell’s sign, paradoxical interventricular septal motion, and visible thrombi in the right heart or pulmonary arteries [20]. In our analysis, RV strain was found in 173 of 264 patients with acute PE (67%) [15–17,19,20].
Diagnostic power of echocardiographic findings
In a previous systematic review and meta-analysis, 22 studies showed consistently high specificity and low sensitivity for echocardiography in diagnosing PE [43]. Moreover, we reanalyzed the sensitivity and specificity of several studies; these results are presented in Table 1.
Among 12 unique signs suggestive of acute PE, right heart strain was the most common sign (sensitivity 73%, specificity 75%) [16–18,20,33,44]. Table 1 shows the high specificity for all the signs, with none of them having a specificity < 80%; however, sensitivity was much lower, with only an increased RVEDD having a sensitivity > 70% for acute PE. These meta-analysis findings revealed that various echocardiographic parameters suggesting acute PE can be used to diagnose PE. However, echocardiographic signs showed a low negative predictive value; therefore, none of them can rule out PE except the presence of clots in the right heart chambers and pulmonary arteries. In clinically insignificant PE with no significant RV hemodynamic effects, echocardiography is usually normal. Therefore, it is important to note that signs can be interpreted differently depending on the situation. In addition, the positive predictive value of echocardiographic signs was insufficient as a stand-alone finding. Signs of RV overload or dysfunction may be observed even in the absence of acute PE with concomitant cardiac or respiratory disease condition. Thus, echocardiography is limited as a potential gold standard for ruling in or out a PE diagnosis, and clinicians should consider further advanced imaging tests in case of a discordance between clinical judgement and the echocardiographic parameters. However, multiple echocardiographic findings can be useful in diagnosing PE and deciding on the use of thrombolysis for patients who cannot receive other confirmatory studies, especially including the most critically ill patients.
ROLE OF ECHOCARDIOGRAPHY IN PE DIAGNOSIS IN SPECIAL SITUATIONS
Echocardiography can be useful in PE diagnosis, particularly in patients for whom performing CT is impossible or difficult [45]. Although echocardiography is not recommended in the diagnostic work-up for hemodynamically stable patients with PE, it can be included in the evaluation of suspected high-risk PE [45].
Considering this, echocardiography in pregnant women may be useful for PE diagnosis because it has no known adverse effect on the fetus. PE is a leading cause of pregnancy-related mortality in developed countries, accounting for 20% of maternal deaths in high-income countries [46]. VTE risk is higher in pregnant women than in non-pregnant women of similar age; it increases during pregnancy and reaches a peak during the post-partum period [47]. The most common PE symptoms include dyspnea (73%), pleuritic chest pain (66%), cough (37%), and hemoptysis (13%). The abrupt onset of pleuritic chest pain may be the first unique symptom. However, accurate clinical suspicion or VTE diagnosis during pregnancy is challenging because of the overlap of signs and symptoms between physiologic changes during pregnancy and the development of PE. The pregnant patient must undergo specific diagnostic tests to establish or exclude PE diagnosis because routine laboratory findings are not specific for confirming the diagnosis. Because radiation exposure during pregnancy can be associated with fetal teratogenic and oncogenic effects, conventional pulmonary angiography or standard-dose CT should be avoided, particularly in the first trimester [45]. Patients with chronic kidney disease (CKD) also have a high-risk of VTE due to activation of procoagulants, decreased anticoagulants, or decreased fibrinolytic activity [48]. A clinical diagnosis of acute PE in patients with CKD is frequently considered; however, the diagnostic approach is challenging. Current guidelines recommend CTPA as the gold standard for an imaging test. However, CTPA is prohibited for use in patients with severe renal impairment due to the increased risk of contrast-induced complications [10]. Thus, for these special populations, a D-dimer test and duplex ultrasound of the lower extremities play essential roles in PE diagnosis. Lung ventilation/perfusion scan, a lower-radiation and contrast medium-sparing procedure, may preferentially be applied if an imaging test is necessary, but it may not be used in an emergency setting [49]. Echocardiography can provide signs that may help in the differential diagnosis of shock; thus, the absence of echocardiographic findings of RV pressure overload can exclude PE as the cause of hemodynamic instability. Moreover, echocardiographic findings suggesting causes other than acute PE can help exclude the need for CT. However, a low-dose CT or ventilation/perfusion scan should be used to distinguish PE in patients with unequivocal echocardiographic signs of RV pressure overload.
ROLE OF ECHOCARDIOGRAPHY IN RISK STRATIFICATION
Acute PE mortality risk levels are conventionally divided into high, intermediate (high/low), and low levels. This stratification can be achieved using four diagnostic tools: the patient’s hemodynamic state, Pulmonary Embolism Severity Index (PESI) score, echocardiographic RV systolic dysfunction parameters, and cardiac markers (troponin). The ESC guidelines classify patients with acute PE into the following categories: (1) high-risk, defined as the presence of shock or persistent hypotension; (2) intermediate-risk, defined as not at high-risk, and a simplified PESI (sPESI) score ≥ 1; and (3) low-risk, defined as the absence of hypotension and an sPESI score of 0 [50]. Risk stratification is essential for allocating each patient to the appropriate treatment and considering more aggressive initial treatments, such as thrombolytic therapy or surgical embolectomy [51]. The presence of RV systolic dysfunction is a poor prognostic factor and represents a more advanced pathophysiologic PE stage. The assessment of RV systolic function is one of the crucial factors for the risk stratification and further management [52]. Although many methods exist for evaluating RV systolic function, no single measurement is accepted as the gold standard. The ESC risk stratification approaches use alternate imaging modalities, such as echocardiography and CT angiography, to assess RV systolic function. However, in hemodynamically stable patients with acute PE, further risk assessment is required based on clinical imaging, cardiac biomarkers (mostly related to RV function and myocardial injury), and the presence of comorbidities. Thus, current risk stratification has focused on identifying low-risk PE in hemodynamically stable patients. Of the 17 prognostic models of acute PE, PESI, and sPESI are the most widely validated and are now included in the risk classification of the ESC guidelines [53,54]. A recently updated prognostic model showed improvement in the prognosis of acute PE by adding one or more clinical-, biological-, and imaging-based markers of RV systolic dysfunction and myocardial injury to the existing models [55].
ROLE OF ECHOCARDIOGRAPHY IN THERAPEUTIC STRATEGIES
The standard treatment for most patients with PE in the acute phase is anticoagulation and thrombolytic therapy [10]. Recently, more effective therapies and interventions, such as greater use of anticoagulants, thrombolysis, and surgical embolectomy in practice, have contributed to the reduction in mortality and PE recurrence.
Because thrombolytic therapy dissolves thrombi in the pulmonary arterial system, it lowers pulmonary arterial pressure and improves RV systolic function more rapidly than anticoagulation only in selected patients with acute PE [56,57]. In patients with high-risk PE, thrombolysis was associated with a reduction in mortality (odds ratio [OR], 0.66; 95% confidence interval [CI], 0.45 to 0.97) [58]. All treatment guidelines recommend thrombolysis as the initial treatment of choice for patients with acute PE who are hemodynamically unstable. Thus, early identification of RV systolic dysfunction in high-risk patients with acute PE is essential in promptly deciding whether to administer thrombolytic therapy [59]. Many critically ill patients cannot undergo more advanced imaging; therefore, bedside echocardiography should be performed at an emergency department or intensive care unit to identify RV systolic dysfunction [60,61].
The role of thrombolysis is unclear in patients with intermediate-risk acute PE. Several large randomized controlled trials have investigated the impact of thrombolytic treatment. The Pulmonary Embolism Thrombolysis (PEITHO) trial compared systemic thrombolysis plus anticoagulation with anticoagulation alone in the largest trial involving 1,005 adult patients with intermediate-risk PE. The incidence of death or hemodynamic decompensation was 2.6% in the group receiving tenecteplase group; this value was much lower than the 5.6% in the group receiving heparin (OR, 0.44; 95% CI, 0.23 to 0.87; p = 0.02) [62]. Although thrombolytic therapy was associated with a significant reduction in the risk of hemodynamic decompensation or collapse, there was an increased risk of bleeding, including major extracranial bleeding (6.3% vs. 1.2% in heparin alone) and hemorrhagic stroke (2.4% vs. 0.2% in heparin alone). Furthermore, thrombolytic therapy showed no reduction in overall mortality, persistent exertional dyspnea or functional limitation, and chronic thromboembolic pulmonary hypertension on long-term follow-up (median duration, 38 months) in the PEITHO trial (709 of 1,006 initially randomized patients) [63]. Therefore, current guidelines do not recommend routine primary reperfusion treatment in patients with intermediate-risk PE [64,65]. “Rescue” thrombolysis should be reserved for these patients if they develop signs of hemodynamic instability despite anticoagulant treatment. Although echocardiographic evidence of RV dysfunction is not a compelling indication for systemic thrombolysis even in intermediate-high-risk patients, there has been an overall uptrend in the use of cardiac imaging in hemodynamically stable patients with PE over the past decade [66]. Because of its easy availability, low procedural cost and risk, and potential for guiding appropriate early management, echocardiography has been used increasingly in non-massive PE at the time of admission [67].
PROGNOSTIC VALUE OF ECHOCARDIOGRAPHIC PARAMETERS IN ACUTE PE
Presence of RV systolic dysfunction
The echocardiographic criteria for RV systolic dysfunction include RV dilatation and an increased end-diastolic RV/ LV ratio, RV free wall hypokinesis, increased TR Vmax, or combinations of these conditions [45]. Although the overall positive predictive power was low (< 10%), systematic reviews and meta-analyses have shown that RV dysfunction detected using echocardiography was associated with an increased risk of short-term mortality, even in hemodynamically stable patients with acute PE [68]. This might be related to the difficulty in standardizing the definition of RV systolic dysfunction in echocardiographic parameters between studies. Nevertheless, the echocardiographic assessment of the RV systolic function is widely recognized as a valuable tool for the prognostic assessment of hemodynamically stable patients with acute PE in current clinical practice (Table 2).
Table 2.
Prognostic value of echocardiographic parameters in acute pulmonary embolism
| Parameter | Study design | Outcomes | OR or HR (95% CI) | Main findings |
|---|---|---|---|---|
| RV dysfunction | Meta-analysis [68] (n = 1,249) | All-cause mortality | 2.4 (1.3–4.3) | The presence of echocardiographic RV dysfunction is associated with short-term mortality in PE patients without hemodynamic compromise. |
|
| ||||
| TAPSE | Prospective cohort [27] (n = 782) | All-cause mortality PE-related mortality |
2.3 (1.2–4.7) 4.4 (1.3–15.3) |
TAPSE ≤ 16 mm was a significant predictor of all-cause mortality and PE-related mortality in normotensive patients. |
| Prospective cohort [45] (n = 411) | PE-related mortality rescue thrombolysis | 27.9 (6.2–124.6) | TAPSE ≤ 15 mm was independent predictor of increased risk of 30-day PE-related mortality or rescue thrombolysis. | |
| Prospective cohort [69] (n = 76) | PE-related mortality | 26.2 (3.2–214.1) | TAPSE ≤ 15 mm was a significant predictor of PE-related mortality. The TAPSE is preferable to echo and MDCT RV to LV ratio for risk stratification in initially normotensive patients. | |
|
| ||||
| Right heart thrombi | Meta-analysis [73] (n = 15,220) | All-cause mortality PE-related mortality | 3.0 (2.2–4.1) 4.8 (2.0–11.3) |
In acute PE patients, concomitant right heart thrombi had a significant association with short-term all-cause mortality and PE-related mortality. |
| Prospective cohort [71] (n = 138) | PE-related mortality All-cause mortality |
2.7 (1.7–5.6) | In patients with concomitant right heart thrombi, 30-day all-cause mortality was greater than propensity score-matched controls. | |
|
| ||||
| RV strain (STE) | Prospective cohort [75] (n = 66) | PE-related adverse outcomes | 2.3 (1.5–3.9) | RV mid free wall longitudinal strain and 3-dimentional RV EF were independently associated with 6-month adverse outcomes. |
| Prospective cohort [76] (n = 144) | In-hospital events (PE-related death, need to inotropics, thrombolysis) | 1.1 (1.0–1.2) | RV free wall and global wall strain is an independent prognostic marker for in-hospital events in patients with acute non-massive PE. | |
OR, odds ratio; HR, hazard ratio; CI, confidential interval; RV, right ventricle; PE, pulmonary embolism; TAPSE, tricuspid annulus plane systolic excursion; MDCT, multidetector computed tomographic; LV, left ventricle; EF, ejection fraction; STE, speckle-tracking echocardiography.
Decreased TAPSE
TAPSE is a well-known, easy-to-measure, and reproducible echocardiographic parameter. It represents the RV longitudinal function measuring the longitudinal displacement of the systolic excursion of the tricuspid annular segment. A TAPSE < 16 mm is regarded as decreased RV systolic function and is the most frequently reported finding associated with unfavorable prognoses in acute PE. Patients with decreased TAPSE (< 16 mm) during diagnosis have a two-fold higher mortality rate (hazard ratio, 2.3; 95% CI, 1.2 to 4.7; p = 0.02) [27]. In some prospective observational studies, TAPSE ≤ 15–16 mm was an independent predictor of increased risk of PE-related mortality or rescue thrombolysis, even after adjusting for other echocardiographic findings of RV dysfunction [45]. Furthermore, TAPSE is a better predictor of acute PE-related outcomes than the RV/LV diameter ratio in normotensive patients [69]. Patients with TAPSE > 20 mm can be considered very low-risk patients who may be candidates for a short hospital stay or even outpatient treatment.
Presence of thrombi in the right heart
According to several studies, right heart thrombi can be detected using echocardiography or CT angiography in approximately 4% of unselected patients with acute symptomatic PE [70]. Prevalence of right heart thrombi may reach 18% among patients with PE in the intensive care setting. However, it is rarely found in normotensive patients without echocardiographic evidence of RV dysfunction (1.0%) [71]. The presence of right heart thrombi was associated with high early mortality in acute PE [72]. Systematic reviews and meta-analyses reported that right heart thrombi increased the risk of short-term all-cause mortality (OR, 3.0; 95% CI, 2.2 to 4.1) and PE-related mortality (OR, 4.8; 95% CI, 2.0 to 11.3) [73]. Associations between right heart thrombi and mortality were consistent after adjusting for demographics, cardiovascular comorbidities, and sPESI score [71]. In low-risk patients without hemodynamic instability or RV systolic dysfunction, the presence of right heart thrombi had no impact on mortality. In particular, the prognosis was more related to the hemodynamic status than to thrombi characteristics [71].
Decreased RV longitudinal strain
Recently, several researchers have shown considerable interest in evaluating RV function based on RV strain in patients with acute PE. Visual estimation of RV systolic function, TAPSE, RV fractional area change, Tei index, and tissue Doppler tricuspid valve annulus systolic wave has been used to estimate RV strain. However, these parameters have significant limitations [74]. Conversely, RV longitudinal strain measured by two-dimensional speckle-tracking echocardiography can assess RV myocardial systolic function without the confounding effect of angle dependency and tethering. RV strain value is closely related to prognosis in patients with hemodynamic stable acute PE. A small-scale prospective study reported that three-dimensional echocardiography-based RV ejection fraction and mid-portion of RV free wall longitudinal strain were independently associated with 6-month adverse outcomes in acute submassive PE [75]. These results remained even in the multivariate analysis after adjusting for cardiac biomarkers and other measured echocardiographic parameters. Lee et al. [76] demonstrated that RV free and global wall strains are independent prognostic markers for in-hospital events, such as in-hospital PE-related death or escalation of therapies.
CONCLUSIONS
Acute PE is the third leading cause of cardiovascular death, and its prevalence is increasing. Echocardiography has been validated for early risk stratification of patients presenting with acute PE and impacts management strategies. Despite decades of research, the role of echocardiography in diagnosing and predicting outcomes of acute PE remains under-estimated. The use of CTPA has facilitated early diagnosis in patients with suspected PE. However, echocardiography is the most available, noninvasive, and feasible imaging option (before performing CTPA) for patients with suspected PE.
Echocardiography has high specificity in diagnosing suspected PE in patients with adequate risk. Thus, it is helpful as a rule in test in the initial diagnosis of acute PE. Echocardiography may be particularly useful at the bedside in the emergency department or intensive care unit for patients who cannot undergo other confirmatory studies, especially those who are in the most critical condition. In addition, it can be a useful option in pregnant patients suspected of having acute PE. More effective therapies and interventions have contributed to reducing mortality and recurrence of acute PE in the last decade. Thrombolytic therapy is the initial treatment of choice in hemodynamically unstable patients with acute PE. Thus, echocardiography is widely used to identify RV dysfunction in high-risk patients with massive PE. For low-risk hemodynamically stable patients, echocardiography rarely yields additional prognostic information. Current guidelines do not recommend echocardiography as part of the diagnostic work-up in non-high-risk patients. However, the presence of RV systolic dysfunction is a poor prognostic factor and represents a more advanced pathophysiologic PE stage. RV dysfunction detected using echocardiography was associated with an increased risk of short-term mortality, even in hemodynamically stable patients with acute PE. Although echocardiography is not recommended for diagnostic work-up in hemodynamically stable patients with PE, echocardiographic assessment of RV systolic function is now widely recognized as a valuable tool for prognostic assessment of hemodynamically stable patients in current clinical practice. Furthermore, a recently updated prognostic model showed that specific echocardiographic RV dysfunction markers have the potential to improve prognosis beyond existing risk models. Furthermore, there has been an overall uptrend in cardiac imaging in the last decade, particularly echocardiography, even in patients with hemodynamically stable PE. Extensive validation and impact studies are needed to guide appropriate patient selection for echocardiography use in hemodynamically stable PE.
Acknowledgments
We would like to specially thank Sung-Won Park for drawing an excellent illustration.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Agnelli G, Becattini C. Acute pulmonary embolism. N Engl J Med. 2010;363:266–274. doi: 10.1056/NEJMra0907731. [DOI] [PubMed] [Google Scholar]
- 2.Keller K, Hobohm L, Ebner M, et al. Trends in thrombolytic treatment and outcomes of acute pulmonary embolism in Germany. Eur Heart J. 2020;41:522–529. doi: 10.1093/eurheartj/ehz236. [DOI] [PubMed] [Google Scholar]
- 3.Wendelboe AM, Raskob GE. Global burden of thrombosis: epidemiologic aspects. Circ Res. 2016;118:1340–1347. doi: 10.1161/CIRCRESAHA.115.306841. [DOI] [PubMed] [Google Scholar]
- 4.Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 5.Konstantinides SV. Trends in pulmonary embolism outcomes: are we really making progress? J Am Coll Cardiol. 2016;67:171–173. doi: 10.1016/j.jacc.2015.10.062. [DOI] [PubMed] [Google Scholar]
- 6.Hwang HG, Lee JH, Kim SA, et al. Incidence of venous thromboembolism: the 3rd Korean Nationwide Study. J Korean Med Sci. 2022;37:e130. doi: 10.3346/jkms.2022.37.e130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park TY, Jung JW, Choi JC, et al. Epidemiological trend of pulmonary thromboembolism at a tertiary hospital in Korea. Korean J Intern Med. 2017;32:1037–1044. doi: 10.3904/kjim.2016.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jimenez D, de Miguel-Diez J, Guijarro R, et al. Trends in the management and outcomes of acute pulmonary embolism: analysis from the RIETE Registry. J Am Coll Cardiol. 2016;67:162–170. doi: 10.1016/j.jacc.2015.10.060. [DOI] [PubMed] [Google Scholar]
- 9.Smith SB, Geske JB, Kathuria P, et al. Analysis of national trends in admissions for pulmonary embolism. Chest. 2016;150:35–45. doi: 10.1016/j.chest.2016.02.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) Eur Heart J. 2020;41:543–603. doi: 10.1093/eurheartj/ehz405. [DOI] [PubMed] [Google Scholar]
- 11.Jaff MR, McMurtry MS, Archer SL, et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011;123:1788–1830. doi: 10.1161/CIR.0b013e318214914f. [DOI] [PubMed] [Google Scholar]
- 12.Ortel TL, Neumann I, Ageno W, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv. 2020;4:4693–4738. doi: 10.1182/bloodadvances.2020001830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afonso L, Sood A, Akintoye E, et al. A Doppler echocardiographic pulmonary flow marker of massive or submassive acute pulmonary embolus. J Am Soc Echocardiogr. 2019;32:799–806. doi: 10.1016/j.echo.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Torbicki A, Kurzyna M, Ciurzynski M, et al. Proximal pulmonary emboli modify right ventricular ejection pattern. Eur Respir J. 1999;13:616–621. doi: 10.1183/09031936.99.13361699. [DOI] [PubMed] [Google Scholar]
- 15.Grifoni S, Olivotto I, Cecchini P, et al. Utility of an integrated clinical, echocardiographic, and venous ultrasonographic approach for triage of patients with suspected pulmonary embolism. Am J Cardiol. 1998;82:1230–1235. doi: 10.1016/s0002-9149(98)00612-2. [DOI] [PubMed] [Google Scholar]
- 16.Kurzyna M, Torbicki A, Pruszczyk P, et al. Disturbed right ventricular ejection pattern as a new Doppler echocardiographic sign of acute pulmonary embolism. Am J Cardiol. 2002;90:507–511. doi: 10.1016/s0002-9149(02)02523-7. [DOI] [PubMed] [Google Scholar]
- 17.Lodato JA, Ward RP, Lang RM. Echocardiographic predictors of pulmonary embolism in patients referred for helical CT. Echocardiography. 2008;25:584–590. doi: 10.1111/j.1540-8175.2008.00665.x. [DOI] [PubMed] [Google Scholar]
- 18.Jackson RE, Rudoni RR, Hauser AM, Pascual RG, Hussey ME. Prospective evaluation of two-dimensional transthoracic echocardiography in emergency department patients with suspected pulmonary embolism. Acad Emerg Med. 2000;7:994–998. doi: 10.1111/j.1553-2712.2000.tb02090.x. [DOI] [PubMed] [Google Scholar]
- 19.Ceccarelli E, Masotti L, Barabesi L, Forconi S, Cappelli R. Pulmonary embolism in very old patients. Aging Clin Exp Res. 2003;15:117–122. doi: 10.1007/BF03324488. [DOI] [PubMed] [Google Scholar]
- 20.Chen JY, Chao TH, Guo YL, et al. A simplified clinical model to predict pulmonary embolism in patients with acute dyspnea. Int Heart J. 2006;47:259–271. doi: 10.1536/ihj.47.259. [DOI] [PubMed] [Google Scholar]
- 21.Dresden S, Mitchell P, Rahimi L, et al. Right ventricular dilatation on bedside echocardiography performed by emergency physicians aids in the diagnosis of pulmonary embolism. Ann Emerg Med. 2014;63:16–24. doi: 10.1016/j.annemergmed.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 22.Tuzovic M, Adigopula S, Amsallem M, et al. Regional right ventricular dysfunction in acute pulmonary embolism: relationship with clot burden and biomarker profile. Int J Cardiovasc Imaging. 2016;32:389–398. doi: 10.1007/s10554-015-0780-1. [DOI] [PubMed] [Google Scholar]
- 23.Casazza F, Bongarzoni A, Capozi A, Agostoni O. Regional right ventricular dysfunction in acute pulmonary embolism and right ventricular infarction. Eur J Echocardiogr. 2005;6:11–14. doi: 10.1016/j.euje.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 24.McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996;78:469–473. doi: 10.1016/s0002-9149(96)00339-6. [DOI] [PubMed] [Google Scholar]
- 25.Kurnicka K, Lichodziejewska B, Goliszek S, et al. Echocardiographic pattern of acute pulmonary embolism: analysis of 511 consecutive patients. J Am Soc Echocardiogr. 2016;29:907–913. doi: 10.1016/j.echo.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 26.Daley J, Grotberg J, Pare J, et al. Emergency physician performed tricuspid annular plane systolic excursion in the evaluation of suspected pulmonary embolism. Am J Emerg Med. 2017;35:106–111. doi: 10.1016/j.ajem.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 27.Lobo JL, Holley A, Tapson V, et al. Prognostic significance of tricuspid annular displacement in normotensive patients with acute symptomatic pulmonary embolism. J Thromb Haemost. 2014;12:1020–1027. doi: 10.1111/jth.12589. [DOI] [PubMed] [Google Scholar]
- 28.Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 29.Park JH, Park YS, Park SJ, et al. Midventricular peak systolic strain and Tei index of the right ventricle correlated with decreased right ventricular systolic function in patients with acute pulmonary thromboembolism. Int J Cardiol. 2008;125:319–324. doi: 10.1016/j.ijcard.2007.02.030. [DOI] [PubMed] [Google Scholar]
- 30.Sugiura E, Dohi K, Onishi K, et al. Reversible right ventricular regional non-uniformity quantified by speckle-tracking strain imaging in patients with acute pulmonary thromboembolism. J Am Soc Echocardiogr. 2009;22:1353–1359. doi: 10.1016/j.echo.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 31.Nazeyrollas P, Metz D, Jolly D, et al. Use of transthoracic Doppler echocardiography combined with clinical and electrocardiographic data to predict acute pulmonary embolism. Eur Heart J. 1996;17:779–786. doi: 10.1093/oxfordjournals.eurheartj.a014946. [DOI] [PubMed] [Google Scholar]
- 32.Goldhaber SZ. Thrombolysis for pulmonary embolism. N Engl J Med. 2002;347:1131–1132. doi: 10.1056/NEJMp020107. [DOI] [PubMed] [Google Scholar]
- 33.Bova C, Greco F, Misuraca G, et al. Diagnostic utility of echocardiography in patients with suspected pulmonary embolism. Am J Emerg Med. 2003;21:180–183. doi: 10.1016/s0735-6757(02)42257-7. [DOI] [PubMed] [Google Scholar]
- 34.Mori S, Nakatani S, Kanzaki H, et al. Patterns of the interventricular septal motion can predict conditions of patients with pulmonary hypertension. J Am Soc Echocardiogr. 2008;21:386–393. doi: 10.1016/j.echo.2007.05.037. [DOI] [PubMed] [Google Scholar]
- 35.Azarian R, Wartski M, Collignon MA, et al. Lung perfusion scans and hemodynamics in acute and chronic pulmonary embolism. J Nucl Med. 1997;38:980–983. [PubMed] [Google Scholar]
- 36.Currie PJ, Seward JB, Chan KL, et al. Continuous wave Doppler determination of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients. J Am Coll Cardiol. 1985;6:750–756. doi: 10.1016/s0735-1097(85)80477-0. [DOI] [PubMed] [Google Scholar]
- 37.Firdous N, Nasa P, Bansal A, Juneja D, Kanwar MS, Bera ML. Comparison of non-invasive diagnostic tests to multi-detector CT pulmonary angiography for the diagnosis of pulmonary embolism. J Cardiovasc Dis Res. 2013;4:40–43. doi: 10.1016/j.jcdr.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nazeyrollas P, Metz D, Chapoutot L, et al. Diagnostic accuracy of echocardiography-Doppler in acute pulmonary embolism. Int J Cardiol. 1995;47:273–280. doi: 10.1016/0167-5273(94)02196-p. [DOI] [PubMed] [Google Scholar]
- 39.Kjaergaard J, Schaadt BK, Lund JO, Hassager C. Quantitative measures of right ventricular dysfunction by echocardiography in the diagnosis of acute nonmassive pulmonary embolism. J Am Soc Echocardiogr. 2006;19:1264–1271. doi: 10.1016/j.echo.2006.04.037. [DOI] [PubMed] [Google Scholar]
- 40.Casazza F, Bongarzoni A, Centonze F, Morpurgo M. Prevalence and prognostic significance of right-sided cardiac mobile thrombi in acute massive pulmonary embolism. Am J Cardiol. 1997;79:1433–1435. doi: 10.1016/s0002-9149(97)00162-8. [DOI] [PubMed] [Google Scholar]
- 41.Torbicki A, Galie N, Covezzoli A, et al. Right heart thrombi in pulmonary embolism: results from the International Cooperative Pulmonary Embolism Registry. J Am Coll Cardiol. 2003;41:2245–2251. doi: 10.1016/s0735-1097(03)00479-0. [DOI] [PubMed] [Google Scholar]
- 42.Chartier L, Bera J, Delomez M, et al. Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999;99:2779–2783. doi: 10.1161/01.cir.99.21.2779. [DOI] [PubMed] [Google Scholar]
- 43.Fields JM, Davis J, Girson L, et al. Transthoracic echocardiography for diagnosing pulmonary embolism: a systematic review and meta-analysis. J Am Soc Echocardiogr. 2017;30:714–723. doi: 10.1016/j.echo.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 44.Vieillard-Baron A, Page B, Augarde R, et al. Acute cor pulmonale in massive pulmonary embolism: incidence, echocardiographic pattern, clinical implications and recovery rate. Intensive Care Med. 2001;27:1481–1486. doi: 10.1007/s001340101032. [DOI] [PubMed] [Google Scholar]
- 45.Konstantinides SV, Torbicki A, Agnelli G, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033–3069. doi: 10.1093/eurheartj/ehu283. [DOI] [PubMed] [Google Scholar]
- 46.Koonin LM, MacKay AP, Berg CJ, Atrash HK, Smith JC. Pregnancy-related mortality surveillance: United States, 1987–1990. MMWR CDC Surveill Summ. 1997;46:17–36. [PubMed] [Google Scholar]
- 47.Sultan AA, West J, Tata LJ, Fleming KM, Nelson-Piercy C, Grainge MJ. Risk of first venous thromboembolism in and around pregnancy: a population-based cohort study. Br J Haematol. 2012;156:366–373. doi: 10.1111/j.1365-2141.2011.08956.x. [DOI] [PubMed] [Google Scholar]
- 48.Wattanakit K, Cushman M, Stehman-Breen C, Heckbert SR, Folsom AR. Chronic kidney disease increases risk for venous thromboembolism. J Am Soc Nephrol. 2008;19:135–140. doi: 10.1681/ASN.2007030308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reid JH, Coche EE, Inoue T, et al. Is the lung scan alive and well?: facts and controversies in defining the role of lung scintigraphy for the diagnosis of pulmonary embolism in the era of MDCT. Eur J Nucl Med Mol Imaging. 2009;36:505–521. doi: 10.1007/s00259-008-1014-8. [DOI] [PubMed] [Google Scholar]
- 50.Grupa Robocza Europejskiego Towarzystwa Kardiologicznego (ESC) do spraw rozpoznawania i postepowania w ostrej zatorowosci plucnej. Konstantinides S, Torbicki A, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Kardiol Pol. 2014;72:997–1053. doi: 10.5603/KP.2014.0211. [DOI] [PubMed] [Google Scholar]
- 51.Wan S, Quinlan DJ, Agnelli G, Eikelboom JW. Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta-analysis of the randomized controlled trials. Circulation. 2004;110:744–749. doi: 10.1161/01.CIR.0000137826.09715.9C. [DOI] [PubMed] [Google Scholar]
- 52.Grifoni S, Vanni S, Magazzini S, et al. Association of persistent right ventricular dysfunction at hospital discharge after acute pulmonary embolism with recurrent thromboembolic events. Arch Intern Med. 2006;166:2151–2156. doi: 10.1001/archinte.166.19.2151. [DOI] [PubMed] [Google Scholar]
- 53.Aujesky D, Obrosky DS, Stone RA, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med. 2005;172:1041–1046. doi: 10.1164/rccm.200506-862OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ozsu S, Abul Y, Orem A, et al. Predictive value of troponins and simplified pulmonary embolism severity index in patients with normotensive pulmonary embolism. Multidiscip Respir Med. 2013;8:34. doi: 10.1186/2049-6958-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Elias A, Mallett S, Daoud-Elias M, Poggi JN, Clarke M. Prognostic models in acute pulmonary embolism: a systematic review and meta-analysis. BMJ Open. 2016;6:e010324. doi: 10.1136/bmjopen-2015-010324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Miller GA, Sutton GC, Kerr IH, Gibson RV, Honey M. Comparison of streptokinase and heparin in treatment of isolated acute massive pulmonary embolism. Br Med J. 1971;2:681–684. doi: 10.1136/bmj.2.5763.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goldhaber SZ, Haire WD, Feldstein ML, et al. Alteplase versus heparin in acute pulmonary embolism: randomised trial assessing right-ventricular function and pulmonary perfusion. Lancet. 1993;341:507–511. doi: 10.1016/0140-6736(93)90274-k. [DOI] [PubMed] [Google Scholar]
- 58.Quezada CA, Bikdeli B, Barrios D, et al. Meta-analysis of prevalence and short-term prognosis of hemodynamically unstable patients with symptomatic acute pulmonary embolism. Am J Cardiol. 2019;123:684–689. doi: 10.1016/j.amjcard.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 59.Marti C, John G, Konstantinides S, et al. Systemic thrombolytic therapy for acute pulmonary embolism: a systematic review and meta-analysis. Eur Heart J. 2015;36:605–614. doi: 10.1093/eurheartj/ehu218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients: part II: cardiac ultrasonography. Crit Care Med. 2016;44:1206–1227. doi: 10.1097/CCM.0000000000001847. [DOI] [PubMed] [Google Scholar]
- 61.Fesmire FM, Brown MD, Espinosa JA, et al. Critical issues in the evaluation and management of adult patients presenting to the emergency department with suspected pulmonary embolism. Ann Emerg Med. 2011;57:628–652. doi: 10.1016/j.annemergmed.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 62.Meyer G, Vicaut E, Danays T, et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med. 2014;370:1402–1411. doi: 10.1056/NEJMoa1302097. [DOI] [PubMed] [Google Scholar]
- 63.Goldhaber SZ. PEITHO long-term outcomes study: data disrupt dogma. J Am Coll Cardiol. 2017;69:1545–1548. doi: 10.1016/j.jacc.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 64.Konstantinides SV, Barco S, Lankeit M, Meyer G. Management of pulmonary embolism: an update. J Am Coll Cardiol. 2016;67:976–990. doi: 10.1016/j.jacc.2015.11.061. [DOI] [PubMed] [Google Scholar]
- 65.Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149:315–352. doi: 10.1016/j.chest.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 66.Andrus BW, Welch HG. Medicare services provided by cardiologists in the United States: 1999–2008. Circ Cardiovasc Qual Outcomes. 2012;5:31–36. doi: 10.1161/CIRCOUTCOMES.111.961813. [DOI] [PubMed] [Google Scholar]
- 67.Papolos A, Narula J, Bavishi C, Chaudhry FA, Sengupta PP. U.S. hospital use of echocardiography: insights from the Nationwide Inpatient Sample. J Am Coll Cardiol. 2016;67:502–511. doi: 10.1016/j.jacc.2015.10.090. [DOI] [PubMed] [Google Scholar]
- 68.Coutance G, Cauderlier E, Ehtisham J, Hamon M, Hamon M. The prognostic value of markers of right ventricular dysfunction in pulmonary embolism: a meta-analysis. Crit Care. 2011;15:R103. doi: 10.1186/cc10119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Paczynska M, Sobieraj P, Burzynski L, et al. Tricuspid annulus plane systolic excursion (TAPSE) has superior predictive value compared to right ventricular to left ventricular ratio in normotensive patients with acute pulmonary embolism. Arch Med Sci. 2016;12:1008–1014. doi: 10.5114/aoms.2016.57678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cameron J, Pohlner PG, Stafford EG, O’Brien MF, Bett JH, Murphy AL. Right heart thrombus: recognition, diagnosis and management. J Am Coll Cardiol. 1985;5:1239–1243. doi: 10.1016/s0735-1097(85)80031-0. [DOI] [PubMed] [Google Scholar]
- 71.Koc M, Kostrubiec M, Elikowski W, et al. Outcome of patients with right heart thrombi: the Right Heart Thrombi European Registry. Eur Respir J. 2016;47:869–875. doi: 10.1183/13993003.00819-2015. [DOI] [PubMed] [Google Scholar]
- 72.Casazza F, Becattini C, Guglielmelli E, et al. Prognostic significance of free-floating right heart thromboemboli in acute pulmonary embolism: results from the Italian Pulmonary Embolism Registry. Thromb Haemost. 2014;111:53–57. doi: 10.1160/TH13-04-0303. [DOI] [PubMed] [Google Scholar]
- 73.Barrios D, Rosa-Salazar V, Morillo R, et al. Prognostic significance of right heart thrombi in patients with acute symptomatic pulmonary embolism: systematic review and meta-analysis. Chest. 2017;151:409–416. doi: 10.1016/j.chest.2016.09.038. [DOI] [PubMed] [Google Scholar]
- 74.Platz E, Hassanein AH, Shah A, Goldhaber SZ, Solomon SD. Regional right ventricular strain pattern in patients with acute pulmonary embolism. Echocardiography. 2012;29:464–470. doi: 10.1111/j.1540-8175.2011.01617.x. [DOI] [PubMed] [Google Scholar]
- 75.Vitarelli A, Barilla F, Capotosto L, et al. Right ventricular function in acute pulmonary embolism: a combined assessment by three-dimensional and speckle-tracking echocardiography. J Am Soc Echocardiogr. 2014;27:329–338. doi: 10.1016/j.echo.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 76.Lee K, Kwon O, Lee EJ, et al. Prognostic value of echocardiographic parameters for right ventricular function in patients with acute non-massive pulmonary embolism. Heart Vessels. 2019;34:1187–1195. doi: 10.1007/s00380-019-01340-1. [DOI] [PubMed] [Google Scholar]