Abstract
Following the post-apartheid era in South Africa, global economic hardships and financial shocks have forced most households to endure various mental and psychological stresses.. This has hindered the achievement of Sustainable Development Goal 3 (SDG-3)—good health and wellbeing—prompting policymakers and academics to search for remedies to mitigate such stresses. Highlighting resilience as a means of improving wellbeing, this paper focuses on financial resilience and constructs an index using a multidimensional framework to investigate its association with mental health disorders. Using the South Africa National Income Dynamic Study alongside several robust estimation techniques, we uncover a negative association between financial resilience and mental health disorders among South Africans. More specifically, financial resilience is associated with an approximately 37% decrease in the occurrence of mental health disorders. The results also reveal disparities in the correlation between financial resilience and mental health disorders across different subgroups. Non-Whites (especially Blacks), urban dwellers, and male household heads are shown to most strongly experience the depression-reducing effect of financial resilience. This paper also shows that life satisfaction and household expenditure mediate the relationship between financial resilience and mental wellbeing. Toward the end of this paper, we discuss the implications of our results and offer some policy recommendations.
Keywords: Multidimensional financial resilience, Mental health disorders, South Africa, Wellbeing, Life satisfaction, Household expenditure
Highlights
-
•
The paper investigates the financial resilience-mental health nexus.
-
•
We develop a multidimensional financial resilience index using the South African NIDS.
-
•
Financial resilience is associated with 37% lower prevalence of mental health disorders.
-
•
The results show disparities among the different subgroups of the population.
-
•
Life satisfaction and household expenditure mediates the FR-mental health nexus.
1. Introduction
Mental and depressive disorders are common across all regions and cultures worldwide. Globally, about 300 million people get depressed each year, with significant fractions of that total attempting and successfully committing suicide (WHO, 2018). These disorders hinder people's ability to earn a living via productive work while costing governments billions in welfare payments and lost revenue (Knapp & Wong, 2020; Layard, 2017). In severe cases, depressive disorders constitute a grave health risk, as affected persons are likely to break down physically and perform poorly in society, family, school, work, sports, and even leisure. Notably, the negative consequences of mental health issues hinder efforts to achieve the United Nations Sustainable Development Goals (SDGs)—especially SDG 3, which focuses on the attainment of good health and wellbeing for all. Hence, addressing mental and depressive disorders is crucial to meet the SDGs by promoting mental health and wellbeing. Notably, some argue that the quest to resolve psychological ailments and boost wellbeing hinges on individuals' ability to effectively manage resources (Kromydas et al., 2021; Nanda & Banerjee, 2021). Considering financial resilience (FR) to be essential in resource accumulation (Nussbaum, 2009), it is appropriate to investigate its implications for mental health. Thus, given that financial resilience is known to protect people from the negative consequences of potential unexpected events (e.g., job loss, natural disasters) and boost their ability to pursue opportunities and investments, we examine its association with mental wellbeing. This is crucial, especially as the United Nations and other international development agencies continue to push the agenda of financial resilience in emerging economies based on SDG 8 with the ultimate aim of ensuring universal access to financial services.
However, the literature on financial resilience's impact on mental wellbeing, especially when it comes to micro-level research, is fairly limited. In fact, there is ongoing debate over the exact relationship between financial resilience and mental health (Duvendack & Mader, 2020). Thus, while some studies view financial resilience as beneficial for mental health, others consider the relationship between the two to be unclear. For instance, using access to finance as a measure of financial resilience, Ajefu et al. (2020) and Ibrahim et al. (2021) show that financial resilience can improve mental health in Nigeria and the United Kingdom, respectively. In contrast, Garman et al. (2022) and Kim (2021) assert that government cash transfers have failed to improve mental health among people in South Africa and the United States, respectively, while Peters et al. (2016) claim that microfinance schemes actually tend to worsen clients' mental wellbeing. This lack of consensus is sometimes attributed simply to the metrics used in one's definition of “financial resilience,” with many previous studies using unidimensional constructs (e.g., access to bank accounts, insurance, credit, access to digital financial services, mortgages, cash transfers) to stand in for financial resilience when analyzing its impact on mental health (Jayasinghe et al., 2020; Ohrnberger et al., 2020; Tahir, Shahid, & Richards, 2022). Salignac et al. (2019) define financial resilience as “the ability to access and draw on internal capabilities and appropriate, acceptable, and accessible external resources and supports in financial adversity.” Their definition points to the importance of considering the multifaceted nature of financial resilience when analyzing the link between financial resilience and mental health.
Importantly, the pathways through which financial resilience affects mental health are typically unaccounted for in the literature. MacKinnon (2012) asserts that neglecting these pathways inevitably biases estimates, hindering the accuracy of conclusions. Hence, researchers must consider these pathways when contributing to the academic literature in order to aid in informed policy work. Moreover, many previous studies have failed to analyze the financial resilience-mental health nexus at decomposed data levels. Reporting such analysis is critical to accurately present the varying implications of financial resilience. With the aim to achieve the SDGs’ central goal to leave no one behind, it is important to analyze data at a detailed level and consider all potential pathways in order to develop effective policies. Based on these assertions, our study examines the relationship between (a multidimensional view of) financial resilience and mental health while considering the channels through which this association may occur and assessing how this relationship may differ across different population subgroups using the South African National Income Dynamics Study (NIDS).
This research contributes the following insights to the existing body of knowledge. First, we contribute to the mental health literature on the determinants of mental wellbeing by determining the implications of financial resilience on depression. Second, unlike previous studies (e.g., Aguila et al., 2016; Ibrahim et al., 2021; Ohrnberger et al., 2020; Schreiter et al., 2020), we contribute to the literature on financial resilience by employing a multidimensional framework that accounts for households’ reliance on support mechanisms, financial inclusion, and financial literacy to raise and manage their income and expenditures. This framework also encompasses savings, debt management, and other measures described by Salignac et al. (2019). Third, we contribute to the literature by detailing the pathways through which financial resilience can affect mental health. While Tahir, Shahid, & Richards, 2022 reveal that non-impulsive behavior and financial satisfaction constitute intermediaries between financial resilience and life satisfaction, they urge future research to explore other ways in which financial resilience could affect mental health to better understand the link and inform policy decisions. Lastly, this study contributes to the literature by using micro-level data from a developing country to explore the financial resilience-mental health nexus. This data enables us to present the differential relationship between financial resilience and wellbeing based on population subgroups. With South Africa known to have a high degree of racial disparities and income inequality (Chatterjee et al., 2022; van Breda & Theron, 2018), presenting this financial resilience-mental health nexus from a disaggregated perspective will undoubtedly aid in policy development.
Our study is structured as follows. In Section 2, we summarize the relevant literature and the hypotheses that we have tested. Sections 3, 4 present our methods and findings, respectively. In Section 5, we discuss the results. Finally, Section 6 presents our conclusions and discusses their policy implications.
2. Literature review
A review of the available evidence suggests that access to and the use of financial resources may have varying impacts on mental health. Using panel data analysis, Aguila et al. (2016) show that bank account ownership is positively correlated with mental wellbeing among older Hispanics in the US. Similarly, Schreiter et al. (2020) demonstrate that a lack of bank account access and ownership is associated with mental health disorders among psychiatric patients in Germany. Boyas et al. (2009) show that owning savings and checking accounts is positively linked to mental and general wellbeing among Latinos in the US. Access to insurance products covering households against unexpected shocks has also been shown to reduce mental stresses and improve general wellbeing through increased financial stability in the US and Ghana (Finkelstein et al., 2012; Gyasi et al., 2020). Anand et al. (2021) claim that financial literacy improved the mental and financial wellbeing of Indian households during the COVID-19 pandemic. Furthermore, Zheng et al. (2021) show that financial literacy has improved the mental health and general wellbeing of urban residents in China. Regarding social capital, Tachibana et al. (2019) assert that, following the 2015 Nepal earthquake, households that received financial support from their family and friends exhibited less psychological distress. Similarly, government financial support greatly reduced depressive and mental stressors among both Chinese and Australian citizens during the COVID-19 pandemic (Botha et al., 2022; Wang et al., 2020). Based on a panel study, Ohrnberger et al. (2020) show that cash transfers have improved the mental health of South Africans.
Importantly, however, results from relevant studies have been somewhat inconsistent. Some show that access to and the use of financial resources actually deteriorate mental health or simply have an insignificant effect. One study by Orton et al. (2016) asserts that participation in microfinance schemes does not necessarily result in improved mental wellbeing among women in low- or middle-income countries. Wind et al. (2011) show that social support for flood-affected towns in England has an insignificant impact on residents' mental and depressive symptoms. Using household data from South Asia, Gopalaswamy et al. (2016) and Brody et al. (2017) show that micro-savings and access to finance have no significant effect on mental wellbeing. Duvendack et al.’s (2011) literature review indicates that microfinance has no significant impact on general wellbeing. In addition, Peters et al. (2016) claim that microfinance schemes ultimately worsen mental health due to debt-induced stress. According to Garman et al. (2022), social support (in the form of government cash transfers) has actually harmed the mental health of South African youth.
Overall, the existing research has some limitations. First, the results are highly inconsistent, likely due to the prevalent use of unidimensional metrics to represent financial resilience (Duvendack & Mader, 2020). In other words, individual metrics like access to bank accounts, financial literacy, and government financial assistance are inadequate when it comes to capturing financial resilience—they are mere components of a more complex whole. Given the current economic hardships stemming in large part from the COVID-19 pandemic, financial resilience is critical to ensuring financial stability, reducing emotional and psychological stress, and improving overall wellbeing. Therefore, to contribute to the literature on the association between financial resilience and mental wellness, it is crucial to employ a framework that properly incorporates the multifaceted nature of financial resilience. Second, the literature has largely failed to consider the potential channels or pathways through which financial resilience affects mental health. Neglecting these channels inevitably leads to biased estimates and improper conclusions (Kenny, 2021; MacKinnon, 2012). Hence, it is appropriate for us to consider these pathways in order to add to the academic literature in a way that informs future policy development. Again, the extant literature has failed to consider variations in the effect of financial resilience on mental health. With the SDGs’ aim to ensure that no one is left behind, it is important to examine the data at decomposed levels to aid in the development of appropriate targeted policies.
2.1. Conceptual framework and hypotheses
In conceptualizing the financial resilience-mental health nexus, we follow the Grossman (1972) model of health demand, which asserts that individuals' initial health stock, which depreciates over time, can be augmented by investments in health. Thus, by determining people's health-related behavior via investment in health care and lifestyle choices, they tend to improve the stock of their health capital and, ultimately, increase their lifespan (Anderson & Grossman, 2009). Research indicates that investments in education (Hartwig & Sturm, 2018) and exercise, among other lifestyle factors (Fu et al., 2016), positively influence health based on the Grossman (1972) model. Financial resilience is known to represent an investment that protects and increases people's ability to handle unexpected expenses or financial emergencies (Lusardi et al., 2011), reduces stress and financial insecurity (Marjolin et al., 2017), and enables people to pursue greater opportunities (Hall, 2021). Based on previous studies that have observed unidimensional measures of financial resilience (e.g., Jayasinghe et al., 2020; Ohrnberger et al., 2020; Tahir, Shahid, & Richards, 2022), it has the ability to improve people's mental health. Especially given the United Nations' current “principles of responsible banking” focused on setting ambitious targets to boost financial inclusion and financial wellbeing (UNEP FI, 2022), mental health is likely to steadily improve moving forward. Based on the Grossman (1972) model, previous empirical studies, and the agenda of the United Nations, we propose the following hypothesis.
Hypothesis 1
Financial resilience is negatively associated with the prevalence of mental health disorders.
2.2. How does financial resilience transmit to mental wellbeing
From a conceptual perspective, financial resilience has the potential to affect mental health through various pathways. This study specifically assesses life satisfaction and household expenditure, detailed below, as two potential pathways.
2.2.1. Life satisfaction
The link between financial resilience and mental wellbeing may be partially explained by the significant role of life satisfaction as a mediator. This assertion is supported by established theories and empirical studies that have demonstrated a robust association between these variables. Maslow's Hierarchy of Needs theory (McLeod, 2007) proposes that individuals have diverse needs ranging from basic physiological needs to needs pertaining to self-actualization and that financial resources are essential for meeting these basic physiological needs. Once individuals' basic needs are met, they can focus on higher-level needs, boosting their life satisfaction (Diener & Oishi, 2000). Thus, financial resilience is critical to the fulfillment of basic needs and, in turn, the improvement of life satisfaction. Empirical studies have also shown that being financially resilient positively and significantly enhances life satisfaction (Sommet & Spini, 2022). In Australia, for example, Jayasinghe et al. (2020) show that financial resources are a major determinant of life satisfaction. Similarly, Fergusson et al. (2015) reveal that financial resources have been essential in the promotion of life satisfaction among New Zealanders.
Notably, some have argued that improvements in life satisfaction promote mental wellbeing. Two theories underlying this claim are cognitive dissonance theory (Cooper, 2019; Festinger, 1957) and self-determination theory (Ng et al., 2012; Ryan & Deci, 2000). The former proposes that individuals who are satisfied with their lives experience less mental distress. Similarly, the latter posits that individuals who feel a sense of autonomy, competence, and relatedness and are more content with their lives experience stronger mental wellbeing. Therefore, these theories suggest that individuals with greater control over their lives, confidence in their abilities, and meaningful relationships are more likely to experience positive mental health outcomes. Empirical evidence supports these claims. For example, Bellis et al. (2012) demonstrate a positive correlation between life satisfaction and mental wellbeing in England, while Sun and Shek (2012) provide evidence that life satisfaction is inversely related to mental health problems among people in China. Fergusson et al. (2015) demonstrate that life satisfaction is negatively correlated with depression, anxiety, and social stress among adults in New Zealand. Ruggeri et al. (2020) also show that life satisfaction is positively associated with mental wellbeing using European Social Survey 2006–2012 data from 21 countries. Evidently, financial resilience tends to enhance mental wellbeing via improvements in life satisfaction. Thus, we propose the following hypothesis.
Hypothesis 2
Life satisfaction acts as an intermediary between financial resilience and mental wellbeing.
2.2.2. Household expenditure
Evidence points to a positive correlation between financial resilience and household expenditure. Thus, financially resilient households are more likely to allocate their expenditures to optimize their consumption structure. Using data from the US, O’Neill and Xiao (2012) show that households with higher expenditures generally have greater access to financial services. Similarly, Hasler et al. (2018) demonstrate that financially resilient households have higher consumption expenditures than their financially fragile counterparts. Notably, several studies indicate that financially resilient individuals and households are able to smooth out their consumption during economic shocks due to their ability to draw on financial assets—in stark contrast to individuals and households that lack financial resilience (e.g., Clark & Mitchell, 2022; Lusardi et al., 2011). To mitigate the impact of unexpected shortfalls in their ability to consume amid economic shocks, people with high financial resilience may leverage their savings or insurance coverage to shape their consumption behaviors and lifestyle, as emphasized by the permanent income hypothesis (Friedman, 1957). For instance, amid severe flooding, affected households may take advantage of credit-market transactions (e.g., loans, savings, insurance coverage) to smooth their consumption (Sawada, 2013; Sawada & Shimizutani, 2011).
On the other hand, an increase in household expenditure enhances mental wellbeing. Several theories suggest a link between household expenditure and mental health. One such theory is the social comparison theory (Festinger, 1954), which asserts that individuals compare themselves with others when it comes to their financial status, material possessions, and standard of living. The theory proposes that, when people perceive themselves as being materially worse off than their colleagues, they experience feelings of jealousy, inferiority, and anxiety. These negative emotions can contribute to the onset of mental health problems, such as depression and stress. Another theory that links household expenditure to mental health is the stress-buffering hypothesis (Cohen & Wills, 1985). This theory posits that social support can act as a buffer against stress and protect against the onset of mental health problems. With regard to household expenditure, this theory suggests that individuals who spend more money on social activities (e.g., socializing with relatives, leisure activities, community events) are more likely to experience positive mental health outcomes. Thus, increases in household expenditure, such as investment in health, create the conditions necessary for improving people's emotional health, living habits, and quality of life by reducing depressive symptoms and mental disorders. Empirical evidence also supports the link between household expenditure and mental health. Using data on British households, Lewis (2014) reports that the psychological wellbeing of British people rises alongside their household expenditure. Similarly, Noll and Weick (2015) assert, based on data from the German Socio-Economic Panel Study, that an individual's mental wellbeing is positively correlated with their household expenditure. Similarly, Wang et al. (2019) demonstrate, using data from the China Family Panel Studies, that household consumption expenditure positively influences mental wellbeing. Based on these points, we hypothesize that financial resilience reduces the prevalence of mental health disorders via increased household consumption expenditure. Therefore, we formally propose the following hypothesis.
Hypothesis 3
Household expenditure acts as an intermediary between financial resilience and mental wellbeing.
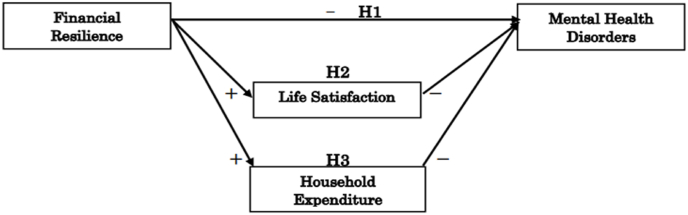
Subject to the abovementioned hypotheses, we present an analytical framework that analyzes the relationship between financial resilience and mental health disorders, as shown in Fig. 1. H1 (which represents hypothesis 1) illustrates financial resilience is negatively associated with the prevalence of mental health disorders, thereby improving wellbeing. Furthermore, the framework illustrates financial resilience as positively correlated with an individual's life satisfaction, reducing the prevalence of mental health disorders (H2). It is evident from the framework that there is a positive relationship between financial resilience and household expenditure, implying that financially resilient households rationally allocate their expenses to optimize their consumption structure amid financial shocks. Ultimately, households optimizing their consumption expenditures ensures that they are not predisposed to financial stress in terms of their ability to provide for their needs, thereby reducing prevalence of mental health disorders (H3). It is important to acknowledge the possibility of other mediating variables, such as food security, that could affect the relationship between financial resilience and mental health disorders. However, due to data limitations pertaining to this variable, this framework only examines life satisfaction and household expenditure.
Fig. 1.
Analytical framework for the relationship between financial resilience and mental health.
2.3. Chronology of the measures of financial resilience
Several metrics have been used in the literature to assess financial resilience. Amid the 2008 financial crisis, Lusardi et al. (2011) employed an early measure of financial resilience based on households' ability to confidently raise $2000 within the next 30 days in the event of an unexpected financial shock. In Indonesia, for instance, DeLoach and Smith-Lin (2018) show that households' access to formal credit and savings is a critical element of their resilience to shocks. In a study on Bangladesh, Belayeth Hussain et al. (2019) operationalize financial resilience as an individual's potential to come up with one-twentieth of the country's GNI per capita within the next month. However, one's ability to raise a set amount of money in the face of adversity does not fully capture financial resilience, especially when it is defined to encompass economic resources (e.g., savings, living expenditure, debt management), financial resources (e.g., access to bank accounts, insurance coverage, credit facility), financial literacy, and social capital (e.g., government support, family support) (Salignac et al., 2019). This complexity has resulted in a debate over the multifaceted nature of financial resilience and the use of a multidimensional framework to conceptualize and compute it. Emphasizing financial behaviors, Kass-Hanna et al. (2022) consider savings, borrowing capacity, and risk-management behaviors to measure financial resilience in Sub-Saharan Africa and South Asia. Moreover, McKnight and Rucci (2020, p. 219) measure European households' financial resilience by considering their income, assets, and debts. However, the multidimensional indices employed by these studies have not been exhaustive, often focusing on financial resilience's economic resources and financial resources dimensions without considering financial literacy or social capital. These studies have failed to account for indicators that reflect current happenings in the financial sector. For example, while they have considered access to bank credit and insurance coverage, they have neglected access to credit cards and other modern financial instruments, including trusts, stocks, and shares. Hence, with financial resilience defined as a household's ability to leverage resources and support mechanisms to bounce back amid financial adversity, it is appropriate to account for the other dimensions of financial resilience while considering indicators that define current trends. Our study, therefore, employs a definition of financial resilience based on Alkire and Foster's (2011) framework (hereafter referred to as the AF methodology), which considers four dimensions—economic resources, financial resources, financial literacy, and social capital—alongside 11 sub-indicators. This AF methodology acknowledges that resilience is a multidimensional concept that must be computed using latent variables/dimensions or other aggregation procedures and data-reduction techniques by combining several variables into a composite measure to craft a resilience index. Moreover, it can be applied to both ordinal and binary datasets (Crentsil et al., 2019), and allows for various cut-offs in the index to help investigate different dynamics in the sample or data.
3. Methods
3.1. Data
For our analysis, we use data from the South African National Income Dynamics Study (NIDS). The NIDS is the national household panel study in South Africa that examined the livelihoods of individuals and households over time from 2008 to 2017. It is important to note that certain variables of interest, especially those pertaining to financial resilience, were concentrated in the study's fifth wave, restricting this study to only the 2017 data. A total of 13,719 households were sampled for the study's fifth wave. After processing the data, we ultimately rely on data from 9359 households for the analysis. The data also provides information about household expenditure, consumption, access to and use of financial products and services, financial literacy, government support, grant receipt, labor market participation, and economic activity. Other themes in the data include poverty status, wellbeing, vulnerability and social capital, and racial demographics, among other household variables. Detailed information on the data can be found in Brophy et al. (2018).
3.2. Choice of the South African context
The apartheid era in South Africa (1948–1994) was characterized by racial segregation and the restriction of economic, health, and educational resources and opportunities to the minority White population to the detriment of the majority Black population. Despite the end of apartheid over since 1994, socio-economic and racial inequalities continue to persist in South Africa. Chatterjee et al. (2022) show that wealth inequality in post-apartheid South Africa is among the most severe in the world, with the top 10% of the population owning nearly 90% of the country's wealth. Orthofer (2016) also highlights the prevalence of racial disparities in terms of economic resources, further exacerbating wealth inequality in favor of the White minority. Evidence indicates that disadvantaged households—which are disadvantaged as a result of these racial and wealth inequalities—are more likely to suffer from mental disorders, including post-traumatic stress disorder (PTSD), in South Africa (Burns et al., 2017; Das-Munshi et al., 2016; Harriman et al., 2021; Lund et al., 2010).
The current situation in South Africa presents major challenges for its citizens in the form of economic difficulties and subsequent mental health problems. As of the fourth quarter of 2021, the unemployment rate in South Africa is 35.3%,1 the highest it has been since 2008, and the country has the third-highest crime rate globally (78.8 per 100,000 people)2 in large part due to the country's high levels of poverty and inequality, which also contribute to households' deteriorating mental health conditions. According to Jack et al. (2014), depression represents the second-highest disease-based burden (behind HIV) and the most common mental and neurological disorder in South Africa. It is estimated that 2.4 million and 7 million people in South Africa suffer from depressive and mental disorders, respectively (IHME, 2019). Thus, it is imperative for policymakers, academics, and even ordinary citizens to address this major mental health concern. However, information on mental health interventions in South Africa is limited. Research by Fernald et al. (2008) shows that men with access to credit show fewer depressive symptoms, though this was not observed among women. Kaminer et al. (2018), after reviewing mental health treatments, assert that only a few interventions have been evaluated for their impact on mitigating depression and anxiety. Given these limitations, it is important to adopt a comprehensive approach to addressing mental health disorders in South Africa that considers both financial and non-financial support mechanisms. The country's high levels of inequality, unemployment, and crime make it a useful case study for other countries seeking to tackle mental health problems related to economic difficulties.
3.3. Measurement of key variables
3.3.1. Mental health
We determine the mental health status of respondents using the Kessler psychological distress scale (Kessler et al., 2002), which assesses experiences of psychological and emotional distress. The scale comprises ten itemized questions focused on restlessness, sadness, fatigue, hopelessness, fear, loneliness, relapse, lack of focus, anxiety, and depression. With a four-level response scale (for which 1 signifies “rarely or none of the time” and 4 signifies “all the time”), respondents scored their own emotional health surveys (see Table A1 in the Appendix) within a range of 10–40. The higher the score, the more distressed and mentally unhealthy the respondent (Lin & Okyere, 2020).
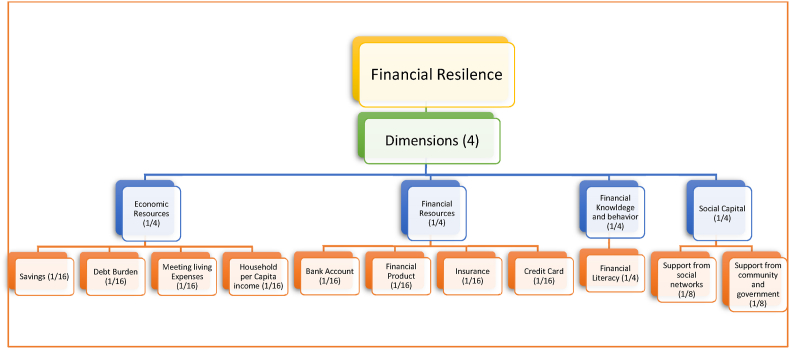
3.3.2. Financial resilience
Previous studies have used several variables to assess financial resilience. For this study, we developed a multidimensional financial resilience index based on Alkire and Foster's (2011) framework. A significant advantage of this framework is its applicability to both ordinal and binary datasets (Crentsil et al., 2019). This framework is a two-step methodology, the two steps being identification and aggregation. More specifically, it identifies financially resilient respondents via the established indicators based on a defined cut-off and aggregates these conditions into a general score through weighting and summation. This study considers four dimensions of financial resilience: economic resources, financial resources, financial literacy, and social capital. These dimensions, which are shown in Figure A1 in the appendix, align with Salignac et al. (2019). The dimensions comprise 11 indicators with binary responses, with 1 representing the possession of a specific resource and 0 indicating the lack of that resource. In line with the AF methodology, we accord weights to the indicators to arrive at a resilience score, as presented in equation (1):
| (1) |
Where is the household's financial resilience score, if a household is financially resilient in terms of indicator , otherwise, and is the weight assigned to indicator with . Although no weighting style is faultless (Ssennono et al., 2021), we allotted a uniform weighting scheme of 1/4 to all dimensions, in line with Alkire et al. (2020), as shown in Table 1. On a continuous scale, our financial resilience score ranges from 0 to 1, where 1 indicates that a respondent is financially resilient from a multidimensional standpoint and 0 indicates that they are not. Aside from the resilience score, we employ a predetermined threshold of 0.3, in line with Nawaz and Iqbal (2021) and Nussbaumer et al. (2012), to classify households as multidimensionally financially resilient. Thus, a household is categorized as 1—meaning financially resilient—if its resilience score equals 0.3 or higher but 0 if its resilience score falls below 0.3. This variable is aptly referred to as financial resilience (FR; cut-off = 0.3).
Table 1.
Dimensions and indicators of the financial resilience index.
| Dimension | Indicator | Financially resilient … | Weight | Reference |
|---|---|---|---|---|
| Economic Resources | Savings | If a household's savings can cover the value of 3 months' expenditure | 1/16 | (McKnight & Rucci, 2020; Salignac et al., 2019) |
| Debt Burden/Management | If a household can manage at least 70% of its debt using the debt-to-asset ratio measure | 1/16 | (Albacete & Lindner, 2013; Bankowska et al., 2015; McKnight & Rucci, 2020) | |
| Meet Living Expenses | If a household's income directly equals its expenditure based on the expenditure-income ratio | 1/16 | (Nguyen et al., 2019; Sabelhaus & Groen, 2000) | |
| Household Per Capita Income | If a household's income meets the national per capita income | 1/16 | Salignac et al. (2019) | |
| Financial Resources | Access to Bank Account | If a household has a bank account | 1/16 | (Bharadwaj et al., 2019; Kass-Hanna et al., 2022; Salignac et al., 2019) |
| Access to Financial Products | If a household has access to financial products, including credit facilities | 1/16 | ||
| Access to Insurance | If a household has access to any insurance coverage | 1/16 | ||
| Access to Credit Card | If a household has access to and uses credit cards | 1/16 | ||
| Financial Knowledge and Behavior | Financially Literate | If a household successfully answers at least 3 out of 4 questions about financial knowledge and behavior | 1/4 | (Kass-Hanna et al., 2022; Salignac et al., 2019; Xiao & Porto, 2017) |
| Social Capital | Support from social networks | If a household receives support from their social networks (family, friends, employer) | 1/8 | (Salignac et al., 2019; Tachibana et al., 2019) |
| Support from the community and government | If a household receives support from its community and government | 1/8 | ||
Source: Adapted from Salignac et al. (2019).
3.3.3. Covariates
The study controls for households’ characteristics, following previous studies on financial resilience (Jayasinghe et al., 2020; Ohrnberger et al., 2020; Sakyi-Nyarko et al., 2022; Salignac et al., 2019; Stevenson et al., 2022; Tahir, Shahid, & Richards, 2022). We control for education, age, sex, household assets, marital status, household size, and location (rural/urban and provincial dummies). Table 2 presents the summary statistics and variable descriptions.
Table 2.
Description and summary statistics.
| Variable | Description | Mean | SD |
|---|---|---|---|
| MHD | Multidimensional measure of mental health disorders indicating mental stresses and depressive symptoms | 12.788 | 8.125 |
| FR Index | Multidimensional measure of financial resilience | 0.294 | 0.153 |
| FR (Cut-Off = 0.3) | Cut-off for measure of financial resilience (1 = If financial resilience score is 0.3 or higher; 0 = Otherwise) | 0.355 | 0.478 |
| Age | Age of head of household | 41.72 | 17.31 |
| Education | Level of education | 1.921 | 0.928 |
| Sex | Sex of head of household (1 = Female; 0 = Otherwise) | 1.587 | 0.492 |
| Household Size | Number of people in household | 3.679 | 2.710 |
| Household Asset (Log) | Log of total household assets (a proxy for wealth/income) | 11.454 | 1.781 |
| Marital Status (Married) | Marital status of head of household | ||
| Consensual | Marital status (1 = Consensual; 0 = Otherwise) | 0.070 | 0.256 |
| Widow | Marital status (1 = Widow; 0 = Otherwise) | 0.127 | 0.333 |
| Divorced/Separated | Marital status (1 = Divorced; 0 = Otherwise) | 0.039 | 0.195 |
| Single | Marital status (1 = Single; 0 = Otherwise) | 0.485 | 0.499 |
| Location | Location (1 = Urban; 0 = Rural) | 0.589 | 0.491 |
| Province (Western Cape) | Province of residence | ||
| Eastern Cape | Province (1 = Eastern Cape; 0 = Otherwise) | 0.119 | 0.324 |
| Northern Cape | Province (2 = Northern Cape; 0 = Otherwise) | 0.068 | 0.252 |
| Free State | Province (3 = Free State; 0 = Otherwise) | 0.060 | 0.237 |
| KwaZulu-Natal | Province (4 = KwaZulu-Natal; 0 = Otherwise) | 0.258 | 0.437 |
| North West | Province (5 = North West; 0 = Otherwise) | 0.062 | 0.241 |
| Gauteng | Province (6 = Gauteng; 0 = Otherwise) | 0.161 | 0.368 |
| Mpumalanga | Province (7 = Mpumalanga; 0 = Otherwise) | 0.074 | 0.262 |
| Limpopo | Province (8 = Limpopo; 0 = Otherwise) | 0.082 | 0.274 |
| Life Satisfaction | Life satisfaction score ranging from 1 (completely dissatisfied) to 10 (completely satisfied) | 5.540 | 2.446 |
| Household Expenditure (Log) | Log of household monthly expenditure | 8.336 | 1.016 |
3.4. Estimation strategy
We estimate the following equation:
| (2) |
Where is the mental health disorders of the i-th household head; is the multidimensional financial resilience score for household ; is a characteristics vector for the i-th household head that includes education level, age, sex, household assets, size, and marital status; is the randomly distributed error term; represents the coefficients of the regressors; and is the constant term. First, we estimate equation (2) using the ordinary least squares (OLS) method. Subsequently, we employ several variant techniques to prove the robustness of the results.
3.4.1. Issues with endogeneity
Using the OLS method to make inferences in research may lead to erroneous conclusions stemming from endogeneity issues. To address this issue, researchers typically employ instrumental variables (IVs). However, some challenge the exogeneity assumption of classical IVs on the basis of a lack of empirical verification of their validity (e.g., Liu et al., 2022). We employ an alternative identification strategy to overcome this challenge: the Lewbel (2012) two-stage least squares (2SLS). This technique internally generates instruments based on the heteroscedasticity in the error terms to resolve endogeneity issues. The Lewbel technique is commonly used by researchers in situations in which there are no valid external instruments as well as in conjunction with accurate external instruments (Essel-Gaisey & Chiang, 2022; Indriyani et al., 2022; Lin & Okyere, 2021; Liu et al., 2022; Zhang et al., 2021). By utilizing the Lewbel technique, we can address endogeneity issues in our research robustly and reliably. Below, we provide further details of the Lewbel technique and its implementation in our study:
| (3) |
Where represents the outcome variable (MHD); denotes the endogenous regressor, financial resilience; is the vector of regressors; and and are the error terms. This technique utilizes an identification strategy reliant on information contained in the heteroscedasticity of to solve endogeneity problems without external instruments. The method assumes that is non-singular, , and , where equals a subset of the elements of ; then, the instruments are estimated as , where is the mean of . The key assumption in this technique is that there should be no correlation between regressors and heteroscedastic errors. This is tested using the Cragg-Donald weak identification Wald test.
This study also employs the kinky least-squares (KLS) approach to ensure robustness, as it is impossible to test exclusion restrictions when applying the instrumental variable technique (Kripfganz & Kiviet, 2021). The KLS approach leverages prior information that the researcher may possess on the relationship between the variable of interest (in this case, financial resilience) and the model's error term. This prior information may be based on the researcher's understanding of omitted variables or unmodelled economic mechanisms that cause the variable to be concurrently determined with the error term. The KLS approach specifies a range of plausible values for the correlation between the endogenous regressor (financial resilience) and the error term, referred to as the “kink.” By focusing on economically plausible parts of the parameter space for the correlation coefficient between the endogenous variable and the error term, the KLS estimator allows for endogeneity-robust and instrument variable-free inference. The KLS estimator then calculates the coefficient estimates and confidence intervals for the regression model within this kink range. Following Kripfganz and Kiviet (2021), the confidence bands obtained from the KLS estimator may be more informative than confidence intervals obtained from IV estimations, particularly when the instruments are weak, as confirmed by other studies (Churchill & Smyth, 2022; Dovì et al., 2021). Moreover, the KLS approach enables a sensitivity analysis of the exclusion restrictions used in IV estimation. For more detailed information on the technique, see Kripfganz and Kiviet (2021) and Kiviet (2020).
The issue of sample selection bias has long been a concern in empirical research, as it has the potential to compromise the validity of causal inference. To address this concern, we employ propensity score matching (PSM), originally developed by Rosenbaum and Rubin (1983), as an additional robustness check. PSM is a non-parametric statistical technique that helps to mitigate endogeneity issues in the selection of treatment groups. The method assumes that treatment and outcome variables are independent and conditional on the observed covariates. To use this method, we estimate the propensity score for each individual, or the conditional probability of being assigned to the treatment group given the observed covariates. Using this score, individuals are matched between the treatment and control groups based on similar covariate values rather than randomization. This study categorizes financially resilient individuals as the treatment group and financially fragile/vulnerable individuals as the control group. The PSM method is used to achieve balance with regard to the covariates of these groups. Specifically, we estimate the average treatment effect of being financially resilient on mental health disorders. This approach allows us to investigate the relationship between financial resilience and mental health disorders while controlling for the associated endogeneity concerns of sample selection bias. The average treatment effect is estimated as follows:
| (4) |
| (5) |
| (6) |
Where indicates the average effect of the treatment; denotes our dependent variable (mental health disorders); and represents the dummy variable (1 if the household head is financially resilient and 0 otherwise). The control variables are represented by , which is a vector of pre-treatment variables. Following this expression, the propensity score is characterized as the probability of being financially resilient given the covariates. In line with the literature (e.g., Essel-Gaisey & Chiang, 2022; Kowaleski-Jones et al., 2018; Lin & Okyere, 2022), we use various matching techniques that support the application of such variant matching methods to ascertain robustness. Thus, we employ the regression adjustment and augmented inverse-probability weighting matching algorithms.
3.5. Possible channels of the underlying mechanism
This section employs the mediation analysis technique proposed by Baron and Kenny (1986), utilizing linear regression models to estimate the total, direct, and indirect effects of the independent variable (FR) on the dependent variable (MHD) through the mediator variable (M). The analysis yields valuable insights into causal mechanisms, explaining observed relationships and identifying potential intervention targets. By controlling for confounding variables and considering alternative explanations, the analysis enhances the accuracy and validity of the research findings (Zhao et al., 2010). Moreover, it contributes to theory development by offering evidence supporting or challenging proposed causal pathways. However, it is crucial to acknowledge the limitations of this method, including susceptibility to bias due to assumptions like linearity, normality, and absence of measurement error, which may not hold in practical contexts (Agler & De Boeck, 2017; Bullock & Green, 2021). Additionally, this method may overlook other variables that impact the relationship between the independent and dependent variables, potentially resulting in biased estimates of the indirect effect (Agler & De Boeck, 2017). Nevertheless, this study's findings provide valuable insights into potential mediating variables influencing the relationship between financial resilience and mental health disorders, contributing to a comprehensive understanding of their complex interplay. Such insights will facilitate the development of targeted interventions and policies aimed at supporting individuals in maintaining their mental well-being amid financial challenges.
As noted in the conceptual framework, financial resilience can, both directly and indirectly, influence mental health disorders via life satisfaction and household expenditure. Therefore, as specified by Baron and Kenny's (1986) stepwise regression method, the following describes the mediation analysis:
| (7) |
| (8) |
Where represents the mediating variables (life satisfaction and household expenditure). In line with Baron and Kenny (1986), Churchill and Smyth (2020), and Lin and Okyere (2022), the basis for judging as a mediator is as follows. First, the coefficient of should be statistically significant in equation (7). Second, the inclusion of in equation (8) should render the coefficient of FR in equation (8) statistically insignificant. This indicates a complete mediating effect (Gan et al., 2020). However, in a situation where FR is significant in equation (8), can be called a mediator if is less than (in equation (2)). However, this indicates a partial mediating effect. As an additional robustness check, we employ the Sobel, Delta, and Monte Carlo tests to justify the validity of the mediators.
4. Results
4.1. Baseline estimates
Table 3 presents the results of the baseline estimates. Columns 1 and 2 report the results using the financial resilience score and 0.3 cut-offs, respectively. The F-statistics show that the explanatory variables jointly explain mental health disorders at the 1% significance level. The coefficient of financial resilience is negative and significant in both columns. Column 1 shows a statistically significant negative association between financial resilience and mental health disorders, indicating that a 1% increase in financial resilience is associated with an approximately 7% reduction in the prevalence of mental health disorders. As shown in column 2, there is a statistically significant coefficient indicating that financially resilient households have less prevalence of mental health disorders by about 2.2% compared to their financially vulnerable counterparts. However, making causal inferences with these results may be erroneous due to the endogeneity issue; hence, we must also test the validity of the estimates using other robust techniques.
Table 3.
Mental health disorders and financial resilience.
| Variables | Mental Health Disorders |
|
|---|---|---|
| (1) | (2) | |
| Financial Resilience | −0.071*** (0.018) | |
| FR = 0.3 Cut Off | −0.022*** (0.005) | |
| Age | 0.007*** (0.000) | 0.007*** (0.000) |
| Age Squared | −0.000*** (0.000) | −0.000*** (0.000) |
| Education | −0.023*** (0.003) | −0.023*** (0.003) |
| Sex (Female) | 0.025*** (0.005) | 0.024*** (0.005) |
| Household Size | 0.001 (0.001) | 0.001 (0.001) |
| Household Asset | −0.012*** (0.001) | −0.012*** (0.001) |
| Marital Status | 0.015*** (0.001) | 0.015*** (0.001) |
| Location (Urban) | −0.018*** (0.005) | −0.018*** (0.005) |
| Constant | 2.701 (0.001) | 2.697*** (0.030) |
| Provincial Fixed Effect |
Yes |
Yes |
| F-Statistics | 49.48*** | 49.70*** |
| R-Squared | 0.050 | 0.050 |
| Observation | 9359 | 9359 |
Robust standard errors in parentheses; ***p < 0.01, **p < 0.05, *p < 0.1.
4.2. Robustness checks
Table 4 shows the results of using the Lewbel (2012) 2SLS method to evaluate the robustness of the model via internally generated instruments. The Craig-Donald Wald F-statistic surpasses the 10 thresholds, signifying the significance and absence of weak relationship in the internal instruments with financial resilience (Stock & Yogo, 2005). Furthermore, this study's findings encompass the Hansen J test of overidentifying restrictions, an essential procedure for overidentified models estimated using the Lewbel technique (Baum et al., 2012). This test examines whether the internally generated instruments are correlated with the endogenous variable but uncorrelated with the error term, assuming the validity of the instruments. With a J statistic value of 7.13 and a non-significant p-value of 0.523, we fail to reject the null hypothesis, indicating the validity of the internally generated instruments derived from heteroscedastic errors. Consequently, the Lewbel estimate is deemed valid. These results highlight a valuable aspect of the Lewbel method, namely its ability to perform tests of overidentifying restrictions and enhance efficiency, as emphasized by Baum (2013). Based on the statistical analysis, a 1% increase in financial resilience is associated with a substantial 36.8% reduction in the prevalence of mental health disorders at the 1% significance level. Moreover, the KLS results complement the previous estimates and consistently show that financial resilience is negatively correlated with mental health disorders among households. In Table 5, we provide additional estimates using the PSM technique to reinforce the fact that our estimates are unbiased. We use various matching methods to ensure robustness for different thresholds of financial resilience. The average treatment effect on the treatment group (financially resilient) is significant and consistent with the baseline, the Lewbel method, and the KLS results. Thus, restricting the financial resilience score to varying cut-offs (0.2, 0.3, and 0.4) and employing variant matching algorithms of the PSM shows that financial resilience is negatively related to mental health disorders. Although estimates from these robust methods vary, it is clear that the endogeneity results in a downward bias relative to the baseline estimates (Table 3). These differences can be attributed to the assumptions that each of these estimation techniques makes. For instance, the Lewbel (2012) method assumes the presence of a valid instrument that is correlated with financial resilience but uncorrelated with the error term. The KLS technique assumes a nonlinear relationship between financial resilience and mental health disorders with a kink at a certain threshold level. Finally, the PSM technique assumes that the treatment and control groups are comparable in terms of their observable characteristics. Hence, despite the different assumptions, all three of these techniques suggest that the baseline estimates are biased downward, in line with previous empirical studies (e.g., Churchill & Smyth, 2022; Lin & Okyere, 2023). Therefore, we can conclude that the evidence from the Lewbel 2SLS, KLS, and PSM estimates consistently demonstrates a negative association between financial resilience and mental health disorders.
Table 4.
Lewbel 2SLS and KLS.
| Panel A: Lewbel 2SLS with internal instruments | MHD |
|---|---|
| Financial Resilience | −0.368*** (0.138) |
| Household x'tics | Yes |
| Individual x'tics | Yes |
| Location | Yes |
| Diagnostics | |
| Craig-Donald Wald F-Statistics | 20.192 |
| Hansen J statistic | 7.13 |
| jp | 0.523 |
| Observation |
9359 |
| Panel B – Kinky Regression | |
| Financial Resilience | −0.665*** |
| Covariates | Yes |
| Postulated Endogeneity of FR | 0.3 |
| Observation | 9359 |
Robust standard errors in parentheses; ***p < 0.01, **p < 0.05, *p < 0.1.
Table 5.
Propensity score matching with varying cut-offs for financial resilience.
| Matching Technique | ATT for FR = 0.2 | ATT for FR = 0.3 | ATT for FR = 0.4 |
|---|---|---|---|
| Augmented Inverse-Probability Weighting | −0.018*** (0.006) | −0.023*** (0.005) | −0.013** (0.006) |
| Regression Adjustment |
−0.018*** | −0.023*** | −0.013** |
| (0.005) |
(0.005) |
(0.006) |
|
| Observation | 9359 | 9359 | 9359 |
Robust standard errors in parentheses; ***p < 0.01, **p < 0.05, *p < 0.1.
4.3. Estimates for variant techniques
Here, we present variant estimation techniques to further demonstrate the robustness of our results. In Table 6, we adopt the multinomial and ordinal logistic regression technique since our dependent variable can be classified into four categories. Depending on the number and severity of symptoms exhibited by the respondent, a depressive occurrence can be categorized as mild, moderate, or severe. Following Andrews and Slade (2001), the MHD scores were categorized as follows: with a score below 16, respondents are likely to be well; with a score of 16–20, respondents are likely to have a mild mental disorder; with a score of 21–24, respondents are likely to have a moderate mental disorder; with a score above 24, respondents are likely to have a severe mental illness. The results indicate that the level of financial resilience is significantly correlated with a reduction of approximately 13% and 40% in households experiencing mild and moderate mental health problems, respectively, at the 10% significance level. The ordinal regression tells a similar story, indicating a statistically significant negative correlation between financial resilience and mental health problems with a reduction of approximately 39% at the 1% significance level. Additionally, the probit model's estimates reveal a statistically significant negative correlation between financial resilience and household mental health problems, suggesting a reduction in the prevalence of mental health disorder by about 19%.
Table 6.
Mental health disorders and financial resilience: Multinomial, ordinal, and probit regression.
| Variables | Mental Health Disorders |
||||
|---|---|---|---|---|---|
| Multinomial Regression |
Ordinal | Probit | |||
| Mild | Moderate | Severe | |||
| FR | −0.127 (0.166) | −0.401* (0.220) | −1.000*** (0.327) | −0.392*** (0.136) | −0.188** (0.089) |
| Household x'tics | Yes | Yes | Yes | Yes | Yes |
| Individual x'tics | Yes | Yes | Yes | Yes | Yes |
| Location |
Yes |
Yes |
Yes |
Yes |
Yes |
| Wald Chi-Sq. | 411.73*** | 411.73*** | 411.73*** | 378.28*** | 336.62*** |
| R-Square | 0.020 | 0.020 | 0.020 | 0.018 | 0.026 |
| Observation | 9450 | 9450 | 9450 | 9450 | 9450 |
Robust standard errors in parentheses; ***p < 0.01, **p < 0.05, *p < 0.1.
The results in Table 7 show three separate estimates: beta, Tobit, and quantile regression. We present the beta results to show the coefficients of financial resilience when we ignore the extreme cases of the dependent variable. For the Tobit estimates, we set the upper limit (40) and lower limit (10) of the raw scores in the dependent variable. The results are consistent with previous estimates in that financial resilience is negatively correlated with mental health disorders. More specifically, according to the beta and Tobit estimates, a statistically significant negative correlation exists between financial resilience and mental health problems, with a 1% increase in financial resilience resulting in 13% and 64% reductions in mental health disorders, respectively. In addition, we employ quantile regression to estimate the relationship between financial resilience and different groups of mental health disorders based on their socioeconomic characteristics (Koenker & Hallock, 2001). Thus, we simultaneously regress the multidimensional financial resilience score on the 25th, 50th, and 75th quantile distributions of mental health disorders, as presented in Table 7. Up to the 25th quantile, the association between financial resilience and mental health problems is insignificant. That is, the most financially resilient households do not experience deteriorations in their mental health. Again, families in the highest quantiles experience significantly lower prevalence in mental health disorders as their level of financial resilience increases. There is a statistically significant negative correlation between financial resilience and mental health disorders, with a reduction of approximately 81% between the 50th and 75th quantiles as a result of a 1% increase in financial resilience. The study also presents estimates on the financial resilience-mental health nexus with regard to the various dimensions of financial resilience. Estimates from Table 8 reveal that access to economic resources, financial resources, and financial literacy are negatively correlated with mental health disorders using the KLS technique. The results presented in Table 6, Table 7, Table 8 all affirm the baseline results and confirm Hypothesis 1.
Table 7.
Mental health disorders and financial resilience: Variant estimates.
| Variables | Mental Health Disorders |
||||
|---|---|---|---|---|---|
| Beta | Tobit | Quantile Regression |
|||
| 25th Percentile | 50th Percentile | 75th Percentile | |||
| FR | −0.130*** (0.031) | −0.640* (0.333) | 0.321 (0.352) | −0.759** (0.338) | −1.586*** (0.468) |
| Household x'tics | Yes | Yes | Yes | Yes | Yes |
| Individual x'tics | Yes | Yes | Yes | Yes | Yes |
| Location |
Yes |
Yes |
Yes |
Yes |
Yes |
| Chi-Sq./F.Stat | 462.94*** | 496.34*** | |||
| R-Squared | 0.009 | 0.028 | 0.022 | 0.031 | |
| Observation | 9359 | 9450 | 9450 | 9450 | 9450 |
Robust standard errors in parentheses; ***p < 0.01, **p < 0.05, *p < 0.1.
Table 8.
Dimensions of financial resilience on mental health disorders.
| Dimensions | MHD |
|---|---|
| Economic Resources | −0.288*** (0.011) |
| Financial Resources/Products | −0.296*** (0.009) |
| Financial Literacy | −0.196*** (0.006) |
| Social Capital | 0.248*** (0.007) |
Robust standard errors in parentheses; ***p < 0.01, **p < 0.05, *p < 0.1.
4.4. Subgroup analysis
We also decompose the analysis into subgroups to show the varying associations between financial resilience and mental health disorders across different demographic groups (Table 9). First, since racial disparities are particularly pronounced in South Africa, it is important to consider variance across racial subgroups. Notably, the results show that financial resilience significantly reduces the prevalence of mental health disorders among non-Whites (including Africans, Asians, and Indians) relative to Whites. Thus, a statistically significant negative association exists between financial resilience and mental health disorders among non-Whites, indicating that 1% increase in financial resilience among non-Whites lowers the prevalence of mental health disorders by about 5.9% than it does among their White counterparts. Geographic differences in crisis severity also play a critical role in changes to psychological or mental distress. Thus, household location matters. The estimates reveal a statistically significant negative association between financial resilience and mental health issues among urban households, with a reduction in the prevalence of mental health disorders by about 9% stemming from a 1% increase in financial resilience. As men and women are known to experience psychological distress differently, we also present subgroup analysis based on the sex of the head of the household. Table 9 shows that a statistically significant negative association exists between financial resilience and depressive symptoms, with males and females experiencing a reduction of roughly 11% and 4%, respectively, alongside 1% increases in their level of financial resilience. Although these estimates re-enforce our claim that financial resilience is negatively associated with mental health disorders, they also demonstrate that the relationship varies across different population sub-groups.
Table 9.
Mental health disorders and financial resilience by race, location, and gender.
| Variable | Mental Health Disorders |
|||||
|---|---|---|---|---|---|---|
| Panel A: Race |
Panel B: Location |
Panel C: Gender |
||||
| Whites | Non-Whites | Rural | Urban | Male | Female | |
| FR | −0.105 (0.075) | −0.059*** (0.018) | −0.042 (0.027) | −0.089*** (0.024) | −0.105*** (0.028) | −0.040* (0.023) |
| Covariates |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
| Observation | 588 | 8769 | 3838 | 5521 | 3859 | 5500 |
Robust standard errors in parentheses; ***p < 0.01, **p < 0.05, *p < 0.1.
4.5. Potential mechanisms
The evidence provided above proves that our results are robust. Here, we detail the potential channels through which financial resilience may enhance mental wellbeing. The results in Table 10 confirm Hypotheses 2 and 3—that life satisfaction and household expenditure mediate the relationship between financial resilience and mental health disorders. Table 10 shows the role of life satisfaction and household expenditure across multiple models. Columns 1 and 3 show the positive relationship between financial resilience and the mediating variables. The results in column 2 indicate that financially resilient households are likely to see an increase in their life satisfaction (which negatively correlates to mental health problems) by about 7%. Similarly, financial resilience significantly boosts household expenditure (which is negatively associated with mental health disorders) by about 4.3%, as shown in column 4. Interestingly, the inclusion of these mediators minimizes the magnitude of financial resilience in columns 2 and 4 compared to its magnitude in column 1 of the baseline regression (Table 3). This indicates a partial mediation effect, as discussed above. The Sobel, Delta, and Monte Carlo tests validate the assertion that life satisfaction and household expenditure significantly mediate the relationship between financial resilience and mental health disorders. From the estimates in column 2, it is clear that the effect of financial resilience on mental health disorders with and without life satisfaction as a mediator (direct and indirect effect) is 7% and 1.2%, respectively. Hence, the mediated effect (RID), or the effect of financial resilience on mental health disorders via life satisfaction, is about 0.2 times as large as the direct effect. The RIT, which indicates the ratio of the indirect effect to the total effect, also reveals that life satisfaction mediates nearly 15% of the relationship between financial resilience and mental health disorders. Similarly, financial resilience's direct and indirect effects on mental health disorders with household expenditure as a mediator are about 4.3% and 6.1%, respectively. Thus, the mediated effect of financial resilience on mental health disorders through household expenditure is about 1.4—as large as the direct effect. On the other hand, RIT shows that 59% of the effect of financial resilience on mental health disorders is partially mediated by household expenditure.
Table 10.
Mediation analysis.
| Variable | (1) |
(2) |
(3) |
(4) |
|---|---|---|---|---|
| Life Satisfaction | MHD | Household Expenditure | MHD | |
| FR | 0.410** (0.165) | −0.070*** (0.017) | ||
| Life Satisfaction | −0.029*** (0.001) | |||
| FR | 1.313*** (0.062) | −0.043** (0.018) | ||
| Household Expenditure | −0.046*** (0.004) | |||
| Diagnostics | ||||
| Direct Effect | 0.070 | 0.043 | ||
| Indirect Effect | 0.012 | 0.061 | ||
| Total Effect | 0.083 | 0.104 | ||
| Delta Test | −0.012** | −0.061*** | ||
| Sobel Test | −0.012** | −0.061*** | ||
| Monte Carlo Test | −0.012** | −0.061*** | ||
| RIT (Indirect Effect/Total Effect) | 0.147 | 0.587 | ||
| RID (Indirect Effect/Direct Effect) | 0.173 | 1.423 | ||
Note: Household expenditure has been logarithmically transformed. Robust standard errors in parentheses; ***p < 0.01, **p < 0.05, *p < 0.1.
5. Discussion
The results show that financial resilience is negatively associated with the prevalence of mental health disorders. This finding is consistent with Hypothesis 1, the Grossman model of health demand, and previous studies that have found financial resources to improve mental wellbeing (e.g., Ajefu et al., 2020; Ohrnberger et al., 2020; Schreiter et al., 2020). This is explained by the fact that financially resilient households and individuals can build up savings, manage debt, meet daily expenses, access and use financial services and products, be financially literate, and invest in their own healthcare, reducing their chances of experiencing mental health disorders. Moreover, the analysis of the various dimensions of financial resilience using the KLS technique is presented in Table 8. Specifically, our findings indicate that the dimensions of access to economic resources, financial resources, and financial literacy are associated with enhanced mental wellbeing, consistent with prior research (Anand et al., 2021; Boyas et al., 2009; Clayton et al., 2015; Schreiter et al., 2020; Taft et al., 2013). One plausible explanation for this pattern of findings is rooted in the notion that individuals who possess a broad array of economic resources, such as savings, adept debt management skills, ample income, access to financial products and services, and financial literacy, are better equipped to effectively manage financial stressors and preserve their mental well-being as argued by Jayasinghe et al. (2020), Nanda and Banerjee (2021) and Stevenson et al. (2022). In contrast, our analysis revealed a positive association between the social capital dimension of financial resilience and mental health disorders, which aligns with recent studies by Garman et al. (2022) and Kim (2021). One potential explanation is that households' reliance on social support may inadvertently increase their susceptibility to mental health disorders, mainly attributed to the social stigma and discrimination that comes with such support. Notably, certain instances have emerged where beneficiaries of monetary transfers have encountered discriminatory treatment based on their racial background, especially in South Africa (Das-Munshi et al., 2016; Gaarder et al., 2010; Garman et al., 2022; Lin & Okyere, 2023), culminating in feelings of shame, humiliation, and diminished self-esteem. These experiences can have detrimental effects on overall mental well-being. The divergent outcomes observed across these dimensions offer further evidence of the inconclusive findings in previous research on the relationship between financial resilience and mental health, emphasizing the necessity of analyzing financial resilience from a multidimensional perspective (Salignac et al., 2019, 2022).
The estimates from the subgroup analysis show that financial resilience is negatively correlated with mental health problems among non-Whites more than it is among Whites. This may be attributable to the fact that non-Whites, especially Africans, generally experience higher levels of mental distress than Whites (Harriman et al., 2021). Again, White South Africans, who constitute a minority group in the country, have access to far more economic resources than non-Whites due to the wealth inequality stemming from apartheid (Chatterjee et al., 2022; Orthofer, 2016). Hence, they are more financially resilient than their non-White counterparts. Notably, we found that there are also differences in the link between financial resilience and mental health outcomes based on household location. The negative association between financial resilience and mental health disorders was stronger among urban households. One key reason for this is that most financial services in South Africa are concentrated in urban areas (Mlachila et al., 2013), giving these folks an edge over their rural counterparts to be more financially resilient. Current statistics indicate that there are 54% more financial institutions offering financial services to South Africans in urban localities than in rural areas (FSCA, 2022; Mtyapi, 2021).
In line with Hypothesis 2, our mediation analysis revealed that life satisfaction serves as a pathway through which financial resilience is negatively associated with the prevalence of mental health disorders. More specifically, being able to raise adequate funds amid crises and having access to financial services enhances life satisfaction by reducing the negative emotions associated with psychological and financial stresses. This finding is consistent with previous research conducted in South Africa, which has established a positive link between financial inclusion and life satisfaction. For example, a recent empirical investigation by BusinessTech (2019) shows that South African households with access to financial services exhibit higher levels of life satisfaction. Similarly, Posel and Casale (2011) and Kollamparambil (2020) report that access to financial resources can boost life satisfaction by more than 2.5% among South Africans, hence reducing the prevalence of mental health disorders, as supported by cognitive dissonance theory and self-determination theory. These theories suggest that individuals who are satisfied with their lives feel a sense of autonomy, competence, and relatedness and, as a result, are content with their lives, leading to a lower likelihood of experiencing mental distress. In essence, evidence indicates that financial resilience indirectly enhances mental wellbeing by improving life satisfaction.
Furthermore, confirming Hypothesis 3, we found that household expenditure mediates the relationship between financial resilience and mental health. In other words, financially resilient households are more likely to make rational expenditure decisions, optimizing their consumption and effectively managing their spending habits. This finding is consistent with previous studies on South Africa showing that financially literate households enhance their overall consumption expenditure patterns due to their ability to efficiently allocate their financial resources (Roberts et al., 2012). In addition, financially included households have been shown to increase their expenditure on consumables due to greater access to financial resources (Gummerson & Schneider, 2013; Mhlanga & Denhere, 2020). Evidently, financially resilient individuals tend to regulate their consumption behaviors and lifestyle, helping them to cope with unforeseen shortfalls in consumption expenditure, including that pertaining to health care. As a result, an increase in household spending translates into an improvement in mental wellbeing, as affirmed by the social comparison theory and the stress-buffering hypothesis. These theories suggest that, as individuals spend more money on their material needs and standard of living, they are more likely to experience positive mental health outcomes. Hence, our findings support the claim that household consumption expenditure enhances wellbeing (Noll & Weick, 2015; Wang et al., 2019). Ample evidence suggests that household consumption expenditure mediates the relationship between financial resilience and mental health disorders.
6. Conclusions and implications
The COVID-19 pandemic and other economic shocks have had severe consequences for the global economy and have made most households, particularly those in the Global South, experience varied forms of mental and psychological stress, including depressive symptoms. These mental stresses have had large detrimental effects on people's mental health and general wellbeing, hindering the achievement of the United Nations' SDGs. This has prompted governments, policymakers, academics, and all other actors in the policymaking space to study this issue and develop holistic policy prescriptions. Our paper focused solely on financial resilience as an effective way to deal with mental health disorders. We considered a measure of financial resilience with four main dimensions—economic resources, financial resources, financial literacy, and social capital—and various sub-dimensions, estimating its association with mental health disorders based on Kessler's psychological distress scale. This study relied on the Grossman model of health demand with a focus on a developing country in Sub-Saharan Africa to investigate the relationship between financial resilience and mental health disorders. We examined this relationship using data from the fifth wave of the South African NIDS. Through the use of robust variant techniques, we found that financial resilience is negatively associated with mental health disorders among households in South Africa, meaning that it enhances their wellbeing. Notably, we identified a similar pattern across all considered subgroups: Whites and non-Whites, urban and rural households, and males and females. We also found that life satisfaction and household expenditure mediate the relationship between financial resilience and mental health disorders.
The results of this study have implications for both policy and research. First, from a policy perspective, this study has implications for actors working toward meeting the United Nations’ SDGs 3 and 8 (those pertaining to good health and wellbeing and sustained, inclusive, and sustainable economic growth). Additionally, our findings are relevant to public health policy, as they present an effective strategy for reducing mental distress, anxiety, and depressive symptoms, especially among households in the Global South. Therefore, we recommend incorporating the provision of financial resources into mental health policies. Second, the mediation analysis that found life satisfaction and household expenditure to explain the financial resilience-mental health nexus implies that the relationship between these two factors can be indirect. Hence, it is important for academics to consider these channels when pursuing a comprehensive understanding of the financial resilience-mental health nexus. Third, the use of a multidimensional framework to capture financial resilience accounted for the multifaceted nature of financial resilience. Our success demonstrates the need for researchers to analyze financial resilience from a multidimensional perspective in order to precisely identify the association between financial resilience and mental health. Our subgroup analysis also showed the varying implications of financial resilience, echoing the need for researchers to analyze these issues at disaggregated dataset levels. Finally, the results showcase many policy-relevant disparities that must be addressed to ensure fair and inclusive development.
7. Limitations and future research
Our analysis was based solely on the fifth wave of the South African NIDS data, as the questions used to compute the multidimensional financial resilience score were concentrated in that wave. Hence, we encourage future studies to consider panel datasets that consist of these or similar questions if and when they become available. Again, we urge researchers to consider other dimensions of health despite our focus on mental wellbeing. Finally, our study identified life satisfaction and household expenditure as potential mediating variables, but we urge future studies to explore other potential mediating variables behind this relationship.
Ethical statement
-
1)
This material is the authors' own original work, which has not been previously published elsewhere.
-
2)
The paper is not currently being considered for publication elsewhere.
-
3)
The paper reflects the authors' own research and analysis in a truthful and complete manner.
-
4)
The paper properly credits the meaningful contributions of co-authors and co-researchers.
-
5)
The results are appropriately placed in the context of prior and existing research.
-
6)
All sources used are properly disclosed (correct citation). Literally copying of text must be indicated as such by using quotation marks and giving proper reference.
-
7)
All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content.
Author contribution
Tsun-Feng Chiang: Conceptualization, Methodology, Original draft, Writing- Original draft preparation, Formal analysis.
Felix Essel-Gaisey: Conceptualization, Methodology, Original draft, Data Curation, Writing- Original draft preparation, Formal analysis.
Michael Adu Okyere: Conceptualization, Methodology, Original draft, Data Curation Writing- Original draft preparation, Formal analysis.
Richmond Forson: Methodology, Writing- Original draft preparation, Resources.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Contributor Information
Felix Essel-Gaisey, Email: pkwesh@gmail.com.
Michael Adu Okyere, Email: papaokyere70@gmail.com.
Richmond Forson, Email: richmondforson6@gmail.com.
Tsun-Feng Chiang, Email: tschiang@mail.ncyu.edu.tw.
Appendices.
Table A1.
Questions from the Kessler psychological distress scale
| Please state how often you have felt this way during the past week. | Rarely or none of the time (less than a day) (Score 1) | Some or little of the time (1–2 days) (Score 2) | Occasionally or moderate amount of time (3–4 days) (Score 3) | All of the time (5–7 days) (Score 4) |
|---|---|---|---|---|
| I was bothered by things that usually don't bother me | ||||
| I had trouble keeping my mind on what I was doing | ||||
| I felt depressed | ||||
| I felt that everything I did was an effort | ||||
| I felt hopeful about the future | ||||
| I felt fearful | ||||
| My sleep was restless | ||||
| I was happy | ||||
| I felt lonely | ||||
| I could not “get going" |
Fig. A1.
Composition of multidimensional financial resilience index
Source: South Africa NIDS Wave 5 (2017)
Data availability
we use the data open to the public
References
- Agler R., De Boeck P. On the interpretation and use of mediation: Multiple perspectives on mediation analysis. Frontiers in Psychology. 2017;8:1984. doi: 10.3389/fpsyg.2017.01984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguila E., Angrisani M., Blanco L.R. Ownership of a bank account and health of older Hispanics. Economics Letters. 2016;144:41–44. doi: 10.1016/j.econlet.2016.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajefu J.B., Demir A., Haghpanahan H. The impact of financial inclusion on mental health. SSM-Population Health. 2020;11 doi: 10.1016/j.ssmph.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albacete N., Lindner P. Household vulnerability in Austria–A microeconomic analysis based on the household finance and consumption survey. Financial Stability Report. 2013;25:57–73. [Google Scholar]
- Alkire S., Foster J. Counting and multidimensional poverty measurement. Journal of Public Economics. 2011;95(7–8):476–487. [Google Scholar]
- Alkire S., Kanagaratnam U., Suppa N. Vol. 49. Oxford Poverty and Human Development; 2020. (The global multidimensional poverty index (MPI) 2020. OPHI MPI methodological note). [Google Scholar]
- Anand S., Mishra K., Verma V., Taruna T. Financial literacy as a mediator of personal financial health during COVID-19: A structural equation modelling approach. Emerald Open Research. 2021;2:59. [Google Scholar]
- Anderson R., Grossman M. Health and the household. Review of Economics of the Household. 2009;7:219–226. [Google Scholar]
- Andrews G., Slade T. Interpreting scores on the Kessler psychological distress scale (K10) Australian & New Zealand Journal of Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842x.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Bankowska K., Lamarche P., Osier G., Pérez-Duarte S. Vol. 39. IFC Bulletins Chapters; 2015. (Measuring household debt vulnerability in the euro area). [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Baum C.F. Vol. 9. Mexican Stata Users’ Group Meetings; 2013. (Implementing new econometric tools in Stata). [Google Scholar]
- Baum C.F., Lewbel A., Schaffer M.E., Talavera O. Vol. 7. United Kingdom Stata User’s Group Meetings; 2012. (Instrumental variables estimation using heteroskedasticity-based instruments). [Google Scholar]
- Belayeth Hussain A.H.M., Endut N., Das S., Chowdhury M.T.A., Haque N., Sultana S., et al. Does financial inclusion increase financial resilience? Evidence from Bangladesh. Development in Practice. 2019;29(6):798–807. [Google Scholar]
- Bellis M.A., Lowey H., Hughes K., Deacon L., Stansfield J., Perkins C. Variations in risk and protective factors for life satisfaction and mental wellbeing with deprivation: A cross-sectional study. BMC Public Health. 2012;12(1):1–17. doi: 10.1186/1471-2458-12-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharadwaj P., Jack W., Suri T. National Bureau of Economic Research; 2019. Fintech and household resilience to shocks: Evidence from digital loans in Kenya. [Google Scholar]
- Botha F., Butterworth P., Wilkins R. Protecting mental health during periods of financial stress: Evidence from the Australian Coronavirus Supplement income support payment. Social Science & Medicine. 2022;306 doi: 10.1016/j.socscimed.2022.115158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyas J., Shobe M.A., Hannam H.M. Examining the association between race, ethnicity, and health status: Do assets matter? Journal of Evidence-Based Social Work. 2009;6(4):401–420. doi: 10.1080/15433710903126604. [DOI] [PubMed] [Google Scholar]
- van Breda A.D., Theron L.C. A critical review of South African child and youth resilience studies, 2009–2017. Children and Youth Services Review. 2018;91:237–247. [Google Scholar]
- Brody C., Hoop T.D., Vojtkova M., Warnock R., Dunbar M., Murthy P., et al. Can self-help group programs improve women's empowerment? A systematic review. Journal of Development Effectiveness. 2017;9(1):15–40. [Google Scholar]
- Brophy T., Branson N., Daniels R.C., Leibbrandt M., Mlatsheni C., Woolard I. University of Cape Town, Southern Africa Labour and Development Research Unit; 2018. National income dynamics study panel user manual. Technical note release. [Google Scholar]
- Bullock J.G., Green D.P. The failings of conventional mediation analysis and a design-based alternative. Advances in Methods and Practices in Psychological Science. 2021;4(4) [Google Scholar]
- Burns J.K., Tomita A., Lund C. Income inequality widens the existing income-related disparity in depression risk in post-apartheid South Africa: Evidence from a nationally representative panel study. Health & Place. 2017;45:10–16. doi: 10.1016/j.healthplace.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BusinessTech . 2019. https://businesstech.co.za/news/banking/308214/the-most-satisfied-banking-customers-in-south-africa-and-who-the-unhappy-ones-are-switching-to/ (2019 banking survey). [Google Scholar]
- Chatterjee A., Czajka L., Gethin A. Wealth inequality in South Africa, 1993–2017. The World Bank Economic Review. 2022;36(1):19–36. [Google Scholar]
- Churchill S.A., Smyth R. Ethnic diversity, energy poverty and the mediating role of trust: Evidence from household panel data for Australia. Energy Economics. 2020;86 [Google Scholar]
- Churchill S.A., Smyth R. Local area crime and energy poverty. Energy Economics. 2022;114 [Google Scholar]
- Clark R.L., Mitchell O.S. Americans' financial resilience during the pandemic. Financial Planning Review. 2022 [Google Scholar]
- Clayton M., Liñares-Zegarra J., Wilson J.O. Does debt affect health? Cross country evidence on the debt-health nexus. Social Science & Medicine. 2015;130:51–58. doi: 10.1016/j.socscimed.2015.02.002. [DOI] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310. [PubMed] [Google Scholar]
- Cooper J. Cognitive dissonance: Where we’ve been and where we’re going. International Review of Social Psychology. 2019;32(1) [Google Scholar]
- Crentsil A.O., Asuman D., Fenny A.P. Assessing the determinants and drivers of multidimensional energy poverty in Ghana. Energy Policy. 2019;133 [Google Scholar]
- Das-Munshi J., Lund C., Mathews C., Clark C., Rothon C., Stansfeld S. Mental health inequalities in adolescents growing up in post-apartheid South Africa: Cross-sectional survey, SHaW study. PLoS One. 2016;11(5) doi: 10.1371/journal.pone.0154478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLoach S.B., Smith-Lin M. The role of savings and credit in coping with idiosyncratic household shocks. Journal of Development Studies. 2018;54(9):1513–1533. [Google Scholar]
- Diener E., Oishi S. Money and happiness: Income and subjective well-being across nations. Culture and Subjective Well-Being. 2000:185–218. [Google Scholar]
- Dovì M.-S., Koester G., Nickel C. 2021. Addressing the endogeneity of slack in phillips curves. [Google Scholar]
- Duvendack M., Mader P. Impact of financial inclusion in low-and middle-income countries: A systematic review of reviews. Journal of Economic Surveys. 2020;34(3):594–629. [Google Scholar]
- Duvendack M., Palmer-Jones R., Copestake J.G., Hooper L., Loke Y., Rao N. 2011. What is the evidence of the impact of microfinance on the well-being of poor people? [Google Scholar]
- Essel-Gaisey F., Chiang T.-F. 2022. Turning the tide on environmental poverty in Ghana: Does financial inclusion matter? Sustainable Production and consumption. [Google Scholar]
- Fergusson D.M., McLeod G.F.H., Horwood L.J., Swain N.R., Chapple S., Poulton R. Life satisfaction and mental health problems (18 to 35 years) Psychological Medicine. 2015;45(11):2427–2436. doi: 10.1017/S0033291715000422. [DOI] [PubMed] [Google Scholar]
- Fernald L.C., Hamad R., Karlan D., Ozer E.J., Zinman J. Small individual loans and mental health: A randomized controlled trial among South African adults. BMC Public Health. 2008;8(1):1–14. doi: 10.1186/1471-2458-8-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Festinger L. A theory of social comparison processes. Human Relations. 1954;7(2):117–140. [Google Scholar]
- Festinger L. Row; Evanston, IL: 1957. A theory of cognitive dissonance. (Peterson) [Google Scholar]
- Financial Sector Conduct Authority . 2022. https://www.fsca.co.za/Documents/FSCA%20Financial%20Sector%20Outlook%20Study%202022.pdf (Financial sector outlook study 2022). [Google Scholar]
- Finkelstein A., Taubman S., Wright B., Bernstein M., Gruber J., Newhouse J.P., et al. The Oregon health insurance experiment: Evidence from the first year. Quarterly Journal of Economics. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman M. A theory of the consumption function. Princeton University Press; 1957. The permanent income hypothesis; pp. 20–37. [Google Scholar]
- Fu R., Noguchi H., Suga K. A revisit to the grossman model with endogenous health depreciation. Economics Bulletin. 2016;36(4):2405–2412. [Google Scholar]
- Gaarder M.M., Glassman A., Todd J.E. Conditional cash transfers and health: Unpacking the causal chain. Journal of Development Effectiveness. 2010;2(1):6–50. [Google Scholar]
- Gan T., Liang W., Yang H., Liao X. The effect of Economic Development on haze pollution (PM2. 5) based on a spatial perspective: Urbanization as a mediating variable. Journal of Cleaner Production. 2020;266 [Google Scholar]
- Garman E.C., Eyal K., Avendano M., Evans-Lacko S., Lund C. Cash transfers and the mental health of young people: Evidence from South Africa's child support grant. Social Science & Medicine. 2022;292 doi: 10.1016/j.socscimed.2021.114631. [DOI] [PubMed] [Google Scholar]
- Gopalaswamy A.K., Babu M.S., Dash U. EPPI-Centre, Social Science Research Unit, UCL Institute of Education, University College London; London: 2016. Systematic review of quantitative evidence on the impact of microfinance on the poor in South Asia. [Google Scholar]
- Grossman M. On the concept of health capital and the demand for health. Journal of Political Economy. 1972;80(2):223–255. [Google Scholar]
- Gummerson E., Schneider D. Eat, drink, man, woman: Gender, income share and household expenditure in South Africa. Social Forces. 2013;91(3):813–836. [Google Scholar]
- Gyasi R.M., Phillips D.R., Buor D. The role of a health protection scheme in health services utilization among community-dwelling older persons in Ghana. The Journals of Gerontology: Serie Bibliographique. 2020;75(3):661–673. doi: 10.1093/geronb/gby082. [DOI] [PubMed] [Google Scholar]
- Hall C.C. Promoting savings for financial resilience: Expanding the psychological perspective. Current Directions in Psychological Science. 2021;30(1):49–54. [Google Scholar]
- Harriman N.W., Williams D.R., Morgan J.W., Sewpaul R., Manyaapelo T., Sifunda S., et al. Racial disparities in psychological distress in post-apartheid South Africa: Results from the SANHANES-1 survey. Social Psychiatry and Psychiatric Epidemiology. 2021;1–15 doi: 10.1007/s00127-021-02175-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartwig J., Sturm J.-E. Testing the Grossman model of medical spending determinants with macroeconomic panel data. The European Journal of Health Economics. 2018;19(8):1067–1086. doi: 10.1007/s10198-018-0958-2. [DOI] [PubMed] [Google Scholar]
- Hasler A., Lusardi A., Oggero N. The George Washington University School of Business; Washington, DC: 2018. Financial fragility in the US: Evidence and implications. Global financial literacy excellence center. [Google Scholar]
- Ibrahim F., McHugh N., Biosca O., Baker R., Laxton T., Donaldson C. Microcredit as a public health initiative? Exploring mechanisms and pathways to health and wellbeing. Social Science & Medicine. 2021;270 doi: 10.1016/j.socscimed.2020.113633. [DOI] [PubMed] [Google Scholar]
- Indriyani W., Yudhistira M.H., Sastiono P., Hartono D. The relationship between the built environment and respiratory health: Evidence from a longitudinal study in Indonesia. SSM-Population Health. 2022;19 doi: 10.1016/j.ssmph.2022.101193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Health Metrics . GBD Results Tool | GHDx; 2019. https://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/d780dffbe8a381b25e1416884959e88b (Global health data exchange (GHDx) and evaluation). [Google Scholar]
- Jack H., Wagner R.G., Petersen I., Thom R., Newton C.R., Stein A., et al. Closing the mental health treatment gap in South Africa: A review of costs and cost-effectiveness. Global Health Action. 2014;7(1) doi: 10.3402/gha.v7.23431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayasinghe M., Selvanathan E.A., Selvanathan S. The financial resilience and life satisfaction nexus of Indigenous Australians. Economic Papers: A Journal of Applied Economics and Policy. 2020;39(4):336–352. [Google Scholar]
- Kaminer D., Owen M., Schwartz B. Systematic review of the evidence base for treatment of common mental disorders in South Africa. South African Journal of Psychology. 2018;48(1):32–47. [Google Scholar]
- Kass-Hanna J., Lyons A.C., Liu F. Building financial resilience through financial and digital literacy in South Asia and Sub-Saharan Africa. Emerging Markets Review. 2022;51 [Google Scholar]
- Kenny D.A. 2021. https://davidakenny.net/cm/mediate.htm (Mediation). [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.-L., et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kim D. Financial hardship and social assistance as determinants of mental health and food and housing insecurity during the COVID-19 pandemic in the United States. SSM-Population Health. 2021;16 doi: 10.1016/j.ssmph.2021.100862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiviet J.F. Testing the impossible: Identifying exclusion restrictions. Journal of Econometrics. 2020;218(2):294–316. [Google Scholar]
- Knapp M., Wong G. Economics and mental health: The current scenario. World Psychiatry. 2020;19(1):3–14. doi: 10.1002/wps.20692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenker R., Hallock K.F. Quantile regression. The Journal of Economic Perspectives. 2001;15(4):143–156. [Google Scholar]
- Kollamparambil U. Happiness, happiness inequality and income dynamics in South Africa. Journal of Happiness Studies. 2020;21:201–222. [Google Scholar]
- Kowaleski-Jones L., Zick C., Smith K.R., Brown B., Hanson H., Fan J. Walkable neighborhoods and obesity: Evaluating effects with a propensity score approach. SSM-Population Health. 2018;6:9–15. doi: 10.1016/j.ssmph.2017.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripfganz S., Kiviet J.F. kinkyreg: Instrument-free inference for linear regression models with endogenous regressors. STATA Journal. 2021;21(3):772–813. [Google Scholar]
- Kromydas T., Thomson R.M., Pulford A., Green M.J., Katikireddi S.V. Which is most important for mental health: Money, poverty, or paid work? A fixed-effects analysis of the UK household longitudinal study. SSM-Population Health. 2021;15 doi: 10.1016/j.ssmph.2021.100909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layard R. IZA World of Labor; 2017. The economics of mental health. [Google Scholar]
- Lewbel A. Using heteroscedasticity to identify and estimate mismeasured and endogenous regressor models. Journal of Business & Economic Statistics. 2012;30(1):67–80. [Google Scholar]
- Lewis J. Income, expenditure and personal well-being, 2011/12 research report. UK Office for National Statistics. 2014 www.ons.gov.uk/ons/dcp171766_365207.pdf [Google Scholar]
- Lin B., Okyere M.A. Multidimensional energy poverty and mental health: Micro-level evidence from Ghana. International Journal of Environmental Research and Public Health. 2020;17(18):6726. doi: 10.3390/ijerph17186726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin B., Okyere M.A. Does energy poverty affect the well-being of people: Evidence from Ghana. Sustainable Production and Consumption. 2021;28:675–685. [Google Scholar]
- Lin B., Okyere M.A. Are people energy poor because of their prosocial behavior? Evidence from Ghana. Energy. 2022;239 [Google Scholar]
- Lin B., Okyere M.A. Race and energy poverty: The moderating role of subsidies in South Africa. Energy Economics. 2023;117 [Google Scholar]
- Liu Y., Zhao J., Zhong H. Grandparental care and childhood obesity in China. SSM-Population Health. 2022;17 doi: 10.1016/j.ssmph.2021.101003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C., Breen A., Flisher A.J., Kakuma R., Corrigall J., Joska J.A., et al. Poverty and common mental disorders in low and middle income countries: A systematic review. Social Science & Medicine. 2010;71(3):517–528. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lusardi A., Schneider D.J., Tufano P. National Bureau of Economic Research; 2011. Financially fragile households: Evidence and implications. [Google Scholar]
- MacKinnon D.P. Routledge; 2012. Introduction to statistical mediation analysis. [Google Scholar]
- Marjolin A., Muir K., Ramia I., Powell A. Centre for Social Impact (CSI) at UNSW Sydney for National Australia Bank; 2017. Why is financial stress on the rise? Financial Resilience in Australia 2016 (Part 1. [Google Scholar]
- McKnight A., Rucci M. Center for Analysis of Social Exclusion, LSE, Case Paper; 2020. The financial resilience of households: 22 country study with new estimates, breakdowns by household characteristics and a review of policy options. [Google Scholar]
- McLeod S. Maslow's hierarchy of needs. Simply Psychology. 2007;1(1–18) [Google Scholar]
- Mhlanga D., Denhere V. Determinants of financial inclusion in southern Africa. Studia Universitatis Babes-Bolyai, Oeconomica. 2020;65(3) [Google Scholar]
- Mlachila M., Dykes D., Zajc S., Aithnard P.-H., Beck T., Ncube M., et al. Banking in sub-saharan Africa: Challenges and opportunities. Regional Studies and Roundtables. 2013 [Google Scholar]
- Mtyapi S. 2021. Investigating financial inclusion in rural households: A South African case. [Google Scholar]
- Nanda A.P., Banerjee R. Consumer's subjective financial well-being: A systematic review and research agenda. International Journal of Consumer Studies. 2021;45(4):750–776. [Google Scholar]
- Nawaz S., Iqbal N. How cash transfers program affects environmental poverty among ultra-poor? Insights from the BISP in Pakistan. Energy Policy. 2021;148 [Google Scholar]
- Ng J.Y., Ntoumanis N., Thøgersen-Ntoumani C., Deci E.L., Ryan R.M., Duda J.L., et al. Self-determination theory applied to health contexts: A meta-analysis. Perspectives on Psychological Science. 2012;7(4):325–340. doi: 10.1177/1745691612447309. [DOI] [PubMed] [Google Scholar]
- Nguyen G.T.H., White B., Ma C. When faced with income and asset shocks, do poor rural households in Vietnam smooth food consumption or assets? Journal of Development Studies. 2019;55(9):2008–2023. [Google Scholar]
- Noll H.-H., Weick S. Consumption expenditures and subjective well-being: Empirical evidence from Germany. International Review of Economics. 2015;62(2):101–119. [Google Scholar]
- Nussbaum M.C. Creating capabilities: The human development approach and its implementation. Hypatia. 2009;24(3):211–215. [Google Scholar]
- Nussbaumer P., Bazilian M., Modi V. Measuring energy poverty: Focusing on what matters. Renewable and Sustainable Energy Reviews. 2012;16(1):231–243. [Google Scholar]
- Ohrnberger J., Anselmi L., Fichera E., Sutton M. The effect of cash transfers on mental health: Opening the black box–A study from South Africa. Social Science & Medicine. 2020;260 doi: 10.1016/j.socscimed.2020.113181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill B., Xiao J.J. Financial behaviors before and after the financial crisis: Evidence from an online survey. Journal of Financial Counseling and Planning. 2012;23(1) [Google Scholar]
- Orthofer A. Vol. 15. Income Distribution & Inclusive Growth; 2016. Wealth inequality in South Africa: Evidence from survey and tax data. Research Project on Employment. [Google Scholar]
- Orton L., Pennington A., Nayak S., Sowden A., White M., Whitehead M. Group-based microfinance for collective empowerment: A systematic review of health impacts. Bulletin of the World Health Organization. 2016;94(9):694. doi: 10.2471/BLT.15.168252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M.D.J., Lockwood C., Munn Z., Moola S., Mishra R.K. EPPI-Centre. Social Science Research Unit, UCL Institute of Education, University College London; London: 2016. People's views and experiences of participating in microfinance interventions: A systematic review of qualitative evidence. 978–1. [Google Scholar]
- Posel D.R., Casale D.M. Relative standing and subjective well-being in South Africa: The role of perceptions, expectations and income mobility. Social Indicators Research. 2011;104:195–223. [Google Scholar]
- Roberts B., Struwig J., Gordon S., Viljoen J., Wentzel M. Financial Services Board; Pretoria: 2012. Financial literacy in South Africa: Results of a baseline national survey. [Google Scholar]
- Rosenbaum P.R., Rubin D.B. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- Ruggeri K., Garcia-Garzon E., Maguire Á., Matz S., Huppert F.A. Well-being is more than happiness and life satisfaction: A multidimensional analysis of 21 countries. Health and Quality of Life Outcomes. 2020;18(1):1–16. doi: 10.1186/s12955-020-01423-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wind T., Fordham M., Komproe I. Social capital and post-disaster mental health. Global Health Action. 2011;4(1):6351. doi: 10.3402/gha.v4i0.6351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan R.M., Deci E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55(1):68. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Sabelhaus J., Groen J.A. Can permanent-income theory explain cross-sectional consumption patterns? The Review of Economics and Statistics. 2000;82(3):431–438. [Google Scholar]
- Sakyi-Nyarko C., Ahmad A.H., Green C.J. The gender-differential effect of financial inclusion on household financial resilience. Journal of Development Studies. 2022:1–21. [Google Scholar]
- Salignac F., Hanoteau J., Ramia I. Financial resilience: A way forward towards economic development in developing countries. Social Indicators Research. 2022;160(1):1–33. [Google Scholar]
- Salignac F., Marjolin A., Reeve R., Muir K. Conceptualizing and measuring financial resilience: A multidimensional framework. Social Indicators Research. 2019;145(1):17–38. [Google Scholar]
- Sawada Y. Vol. 250. The Economic Impacts of Natural Disasters; 2013. (The economic impact of earthquakes on households). [Google Scholar]
- Sawada Y., Shimizutani S. Changes in durable stocks, portfolio allocation, and consumption expenditure in the aftermath of the Kobe earthquake. Review of Economics of the Household. 2011;9(4):429–443. [Google Scholar]
- Schreiter S., Bermpohl F., Schouler-Ocak M., Krausz M.R., Rössler W., Heinz A., et al. Bank account ownership and access among in-patients in psychiatric care in Berlin, Germany—a cross-sectional patient survey. Frontiers in Psychiatry. 2020;11:508. doi: 10.3389/fpsyt.2020.00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommet N., Spini D. Financial scarcity undermines health across the globe and the life course. Social Science & Medicine. 2022;292 doi: 10.1016/j.socscimed.2021.114607. [DOI] [PubMed] [Google Scholar]
- Ssennono V.F., Ntayi J.M., Buyinza F., Wasswa F., Aarakit S.M., Mukiza C.N. Energy poverty in Uganda: Evidence from a multidimensional approach. Energy Economics. 2021;101 [Google Scholar]
- Stevenson C., Wakefield J.R., Bowe M., Kellezi B., Jones B., McNamara N. Weathering the economic storm together: Family identification predicts future well-being during COVID-19 via enhanced financial resilience. Journal of Family Psychology. 2022;36(3):337. doi: 10.1037/fam0000951. [DOI] [PubMed] [Google Scholar]
- Stock J.H., Yogo M. Testing for weak instruments in linear IV regression. Identification and Inference for Econometric Models: Essays in Honor of Thomas Rothenberg. 2005;80(4.2):1. [Google Scholar]
- Sun R.C., Shek D.T. Positive youth development, life satisfaction and problem behaviour among Chinese adolescents in Hong Kong: A replication. Social Indicators Research. 2012;105(3):541–559. doi: 10.1007/s11205-011-9786-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tachibana T., Goto R., Sakurai T., Rayamajhi S., Adhikari A., Dow W.H. Do remittances alleviate negative impacts of disaster on mental health? A case of the 2015 Nepal earthquake. Social Science & Medicine. 2019;238 doi: 10.1016/j.socscimed.2019.112460. [DOI] [PubMed] [Google Scholar]
- Taft M.K., Hosein Z.Z., Mehrizi S.M.T., Roshan A. The relation between financial literacy, financial wellbeing and financial concerns. International Journal of Business and Management. 2013;8(11):63. [Google Scholar]
- Tahir M.S., Shahid A.U., Richards D.W. The role of impulsivity and financial satisfaction in a moderated mediation model of consumer financial resilience and life satisfaction. International Journal of Bank Marketing. 2022;40(4):773–790. [Google Scholar]
- UNEP FI . 2022. https://www.unepfi.org/industries/banking/guidance-on-financial-inclusion-and-financial-health-target-setting/ (Guidance on financial health & inclusion target setting 2.0). [Google Scholar]
- Wang H., Cheng Z., Smyth R. Consumption and happiness. Journal of Development Studies. 2019;55(1):120–136. [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2018. WHO (2018) global health estimates 2016. [Google Scholar]
- Xiao J.J., Porto N. Financial education and financial satisfaction: Financial literacy, behavior, and capability as mediators. International Journal of Bank Marketing. 2017;35(5):805. [Google Scholar]
- Zhang Q., Appau S., Kodom P.L. Energy poverty, children's wellbeing and the mediating role of academic performance: Evidence from China. Energy Economics. 2021;97 [Google Scholar]
- Zhao X., Lynch J.G., Jr., Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37(2):197–206. [Google Scholar]
- Zheng Q., Peng Z., Ding S. Financial literacy, health engagement, and residents' health: Evidence from China. International Journal of Environmental Research and Public Health. 2021;18(8):4202. doi: 10.3390/ijerph18084202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
we use the data open to the public