Clinical presentation
A 13-year-old Hispanic female presented with an enlarging, painful plaque on the crown of the scalp that started 1 month prior. On physical examination, there was a 5 cm circular, exophytic, boggy plaque with yellow crust on the crown with a 1 cm erythematous scaly plaque at the superior edge of the larger plaque (Fig 1). A 1 cm tender lymph node on the left occipital scalp was also palpated. The patient’s mother reported having no pets at home and no recent animal contact. Attempted treatments included organic coconut oil and moisturizing cream. We present the reflectance confocal microscopy (RCM) findings of a kerion in a pediatric patient.
Fig 1.
Clinical image. 5 cm erythematous, thickened, boggy plaque covered with yellow, scaly crust on the crown of the scalp.
Dermatoscopic appearance
Dermatoscopic examination showed white scale and hemorrhagic and yellow crust on large ill-defined patches of erythema (Fig 2).
Fig 2.
Dermatoscopic image. White-yellow scale and hemorrhagic spots as well as a yellow crust on large ill-defined patches on an erythematous background and loss of terminal hairs.
Confocal microscopy appearance
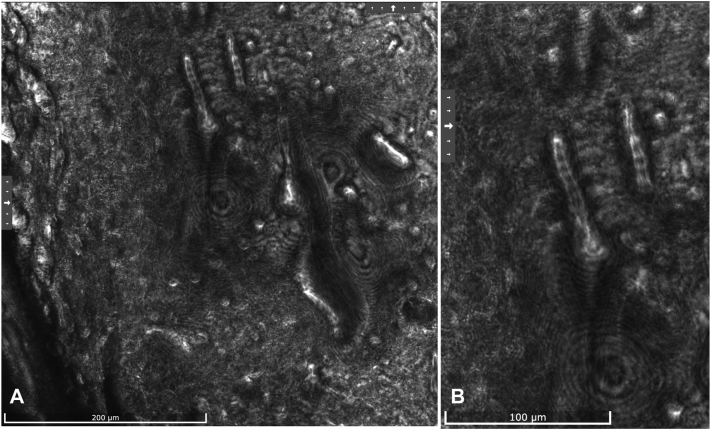
RCM showed bright linear, septate branching structures amongst amorphous fluid in the stratum corneum, consistent with a diagnosis of dermatophyte infection (Fig 3, A and B).1,2 In this case, the hyphae were larger than those commonly visualized in tinea. The organisms had an elongated “cigar” shape, similar to the morphology of the genus trichophyton species based on hyphae and segmental arthroconidia;3 however, the species could not be distinguished. RCM confirmed the clinical suspicion of a kerion, an abscess caused by tinea capitis or fungal infection of the scalp.
Fig 3.
A and B, Reflectance confocal microscopy image. A, Numerous bright linear and branching filamentous structures with segmented arthroconidia representing hyphae amongst an amorphous fluid were observed at the spinous-granular layer of the epidermis. B, Higher magnification shows tubular structures with bright lining and septation corresponding to segmental arthroconidia of fungi surrounded by a darker halo favoring tissue edema.
Diagnosis and treatment
We offered biopsy as an option for the identification of fungus; however, the patient’s mother did not wish to proceed. swabs of lesion crust sent for culture were negative. KOH scrapings were positive for the presence of fungi. In a 2010 pooled analysis, sensitivities of KOH smear and culture were 73.3% (95% CI: 66.3%-79.5%) and 41.7% (34.6%-49.1%), respectively.2 The specificities of culture and KOH smear were 77.7% (72.2%-82.5%) and 42.5% (36.6%-48.6%), respectively. KOH scraping can lead to false positives as it is difficult to distinguish fungal elements from contaminants (ie, hair, cotton/wool fibers). In addition, KOH scraping may lead to false negatives due to sampling error, excess scale in the sample, and inadequate KOH hydrolysis.2 Given this margin for error in traditional bedside examinations of fungus, it is worthwhile to explore an adjunct noninvasive technology that may improve diagnostic accuracy.
Based on the RCM and KOH findings, the patient was treated with prednisone 40 mg daily for 7 days and griseofulvin 20 mL twice daily for 2 months. After 1 month, the nodule size decreased by over 50%, and discomfort resolved. The lesion became flatter and painless, and the erythema had resolved. Repeat dermatoscopic evaluation showed a minimal white and yellow scale (Fig 4).
Fig 4.
Dermatoscopic image. Loss of hair follicles with black dots and white structureless areas with broken hairs consistent with fungal scalp infection at 1-month follow-up.
Key message
RCM presents a potential noninvasive alternative to visualizing fungal hyphae at the bedside without additional sample turnover time and with no discomfort to pediatric patients. Further studies on RCM’s utility in diagnosing fungal infections should include larger study populations and longitudinal therapeutic monitoring.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
Consent: Patient gave consent for their photographs and medical information to be published in print and online with the understanding that this information may be publicly available.
References
- 1.Hui D., Xue-cheng S., Ai-e X. Evaluation of reflectance confocal microscopy in dermatophytosis. Mycoses. 2013;56(2):130–133. doi: 10.1111/j.1439-0507.2012.02222.x. [DOI] [PubMed] [Google Scholar]
- 2.Khan S., Farabi B., Navarrete-Dechent C., Rao B., Safai B. Applications of reflectance confocal microscopy in the diagnosis of fungal infections: a systematic review. J Fungi (Basel) 2022;9(1):39. doi: 10.3390/jof9010039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yazdanparast S.A., Barton R.C. Arthroconidia production in trichophyton rubrum and a new ex vivo model of onychomycosis. J Med Microbiol. 2006;55(11):1577–1581. doi: 10.1099/jmm.0.46474-0. [DOI] [PubMed] [Google Scholar]