Abstract
Background
Persons living in sub-Saharan Africa (SSA) face disproportionate risk from overlapping epidemics of HIV and bacterial sexually transmitted infections (STIs). Pre-exposure prophylaxis (PrEP) for prevention is gradually being scaled up globally including in several settings in SSA, which represents a key opportunity to integrate STI services with HIV pre-exposure prophylaxis (PrEP). However, there is limited literature on how to successfully integrate these services, particularly in the SSA context. Prior studies and reviews on STI and PrEP services have largely focused on high income countries.
Methods
We conducted a scoping review of prior studies of integration of STI and PrEP services in SSA. We searched PubMed, EMBASE, Cochrane, and CINAHL, in addition to grey literature to identify studies that were published between January 2012 and December 2022, and which provided STI and PrEP services in SSA, with or without outcomes reported. Citations and abstracts were reviewed by two reviewers for inclusion. Full texts were then retrieved and reviewed in full by two reviewers.
Results
Our search strategy yielded 1951 records, of which 250 were retrieved in full. Our final review included 61 reports of 45 studies. Most studies were conducted in Southern (49.2%) and Eastern (24.6%) Africa. Service settings included public health clinics (26.2%), study clinics (23.0%), sexual and reproductive care settings (23.0%), maternal and child health settings (8.2%), community based services (11.5%), and mobile clinics (3.3%). A minority (11.4%) of the studies described only syndromic STI management while most (88.6%) included some form of etiological laboratory STI diagnosis. STI testing frequency ranged from baseline testing only to monthly screening. Types of STI tested for was also variable. Few studies reported outcomes related to implementation of STI services. There were high rates of curable STIs detected by laboratory testing (baseline genitourinary STI rates ranged from 5.6–30.8% for CT, 0.0–11.2% for GC, and 0.4–8.0% for TV).
Discussion
Existing studies have implemented a varied range of STI services along with PrEP. This range reflects the lack of specific guidance regarding STI services within PrEP programs. However, there was limited evidence regarding implementation strategies for integration of STI and PrEP services in real world settings.
Keywords: STIs—sexually transmitted infections, PrEP (pre-exposure prophylaxis), sub sahara Africa, service integration, HIV prevention, STI prevention
Introduction
Persons living in sub-Saharan Africa face disproportionate risk from overlapping epidemics of HIV and bacterial STIs. Specifically, young African women face a disproportionate risk of HIV acquisition, accounting for more than half of new infections on that continent, with incidence rates that are often more than double that of their male age-mates (1). At the same time, African women also face a disproportionate burden of sexually transmitted infections (STIs). Globally, the World Health Organization (WHO) estimates that 358 million new cases of four curable sexually transmitted infections with the greatest burden in low- and middle-income countries (2). The overlapping epidemics of HIV and bacterial STIs in Africa have been recognized since the earliest days of the HIV epidemic.
The WHO has recommended greater bi-directional integration of STI and PrEP programs, by both incorporating STI services into PrEP programs and targeting STI clients as potential PrEP clients. Furthermore, they recommend moving beyond a syndromic approach to diagnostic STI testing and treatment, given concerns related to missed diagnoses and overtreatment (2). National PrEP guidelines in a number of countries in SSA that have rolled out PrEP recommend STI screening at baseline and in follow up; this is largely done via syndromic management due to limited resources (3–5). A number of barriers exist to implementation of STI testing and service delivery in SSA, including financial, logistical and time constraints. Despite the need for innovative approaches to providing combined STI and PrEP services, limited literature exists around models of integration of STI and PrEP programs (6, 7).
We sought to investigate the evidence around integration of PrEP services with STI services in the SSA context via a scoping review of the literature. Specifically, we aimed to better understand in what contexts STI and PrEP integration had been studied, what types of STI services had been integrated with PrEP, and what evidence existed around barriers and best practices for integration of these services.
Methods
We conducted scoping review to evaluate the evidence base for integration of PrEP and STI services in SSA. We used a systematic approach, following Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (8). A study protocol was drafted and filed prior to the search, and is available online via figshare (9).
A full electronic search strategy covered all studies published between January 2012 and December 2022. Studies prior to 2012 were not included due to the lack of PrEP implementation in SSA during that period. Key words were generated to describe the scoping review concepts using index articles as well as the authors’ background knowledge. Initial search strategies were developed using PubMed advanced search builder, which was then followed by an exploratory search. The final search strategy included four core concepts: (HIV) AND (Pre-Exposure Prophylaxis) AND (Sexually Transmitted Infections) AND (Sub-Saharan Africa). This search strategy was subsequently adopted to search other databases that included EMBASE, Cochrane, and CINAHL. We also searched conference proceedings and abstracts from major international HIV and STI conferences (i.e., IAS, CROI, ISTDR, INTEREST, Adherence) and the grey literature for reports focused on PrEP and STI services delivery in SSA from World Health Organization (WHO), non-governmental organizations (NGO), and intergovernmental organizations (IGO) that were available on the following databases: Union of International Associations IGO Search, IGO/NGO custom search engines, WHO Institutional Repository for Information Sharing (IRIS), and WHO Library Database. A full description of the search strategy is provided in Supplementary Appendix I.
Following the search, all identified citations were collated and uploaded into Rayyan, a collaborative software for systematic reviews, and duplicates were removed (10). English-language records with a focus on PrEP and STI service delivery were included. In line with the review question, we included studies which described provision of PrEP and STI services as well as the outcomes of these services. PrEP services were defined as provision of PrEP as well as clinical follow-up. Studies that only described promotion, education, counseling, HIV risk assessment or referral related to oral PrEP without any provision of PrEP were not included. We limited our review to oral daily PrEP as it is the current available modality of PrEP that has been approved to use in SSA. STI services were considered to include promotion, education, consulting, diagnosis (e.g., syndromic diagnosis, laboratory diagnostics, and point of care testing), treatment, or partner services. PrEP and STI outcomes included any quantitative and qualitative outcomes reported regarding these services. Because the overall goal of this scoping review was to describe existing models of STI and PrEP service integration, we also included protocols of ongoing studies that described integration of these services, even if no outcomes were available.
Titles and abstracts were independently screened by two reviewers (PA, LW) for inclusion in the review and potentially relevant articles were then retrieved in full and assessed for inclusion. If only the abstract was available, effort was made to search for a full text article related to the abstract; if none was available, the abstract was included in our review. Full text records were subsequently screened by two independent reviewers for inclusion. Information on study design, context, target population, PrEP and STI services, relevant outcomes, and conclusions were extracted by one reviewer and reviewed by a second reviewer using a data extraction sheet. Disagreements at each step were resolved through discussion between the two reviewers.
Results
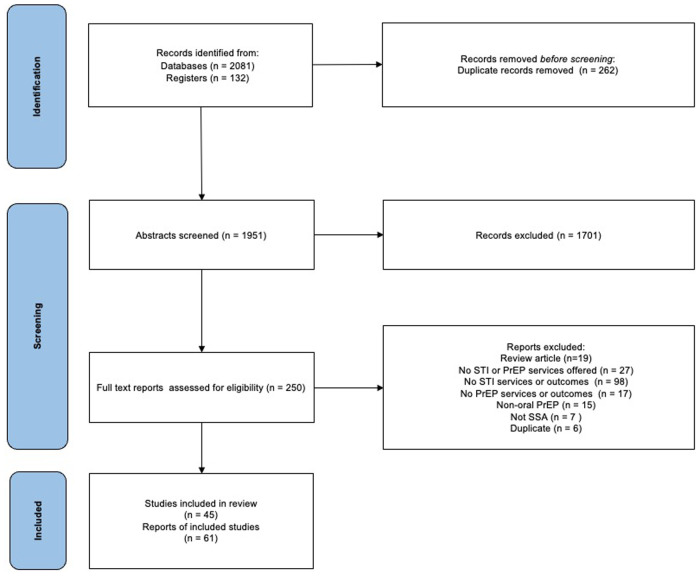
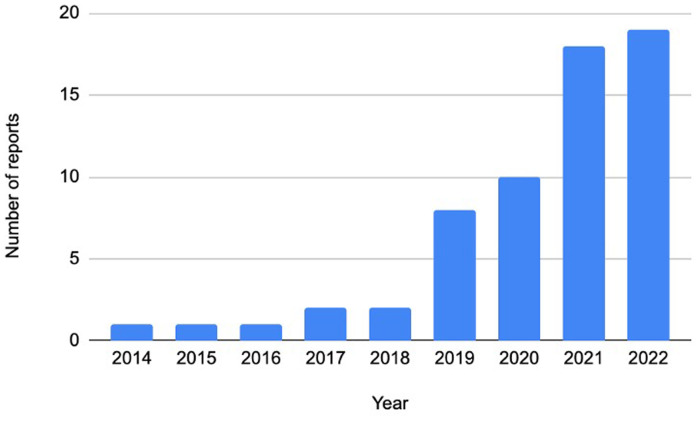
After removal of duplicates, the search strategy yielded a total of 1951 records for abstract review, of which 250 were retrieved in full. Of these, 61 reports of 45 studies were selected for inclusion. Of these, 42 (68.9%) were full text reports, 10 (16.4%) were abstracts and 9 (14.8%) were protocols. Details of the records reviewed, including reasons for exclusion at the full text stage, are provided in Figure 1. The majority of papers were published in 2019 or later (88.5%), reflecting the relatively new rollout of PrEP in SSA (Figure 2).
Figure 1.
PRISMA flow diagram of study inclusion.
Figure 2.
Distribution of year of publication.
Table 1 shows the characteristics of included reports and type of services and direction of integration. Most papers described cohort studies (34/61, 55.7%), including real-world cohorts and single-arm demonstration studies; randomized control trials (RCTs) comprised a smaller proportion of the included reports (12/61, 19.7%) Consistent with the actual implementation of PrEP in SSA, most studies were conducted in Southern (49.2%) and Eastern (24.6%) Africa, with Western Africa (19.7%) representing a smaller portion of the included reports.
Table 1.
Summary of included studies.
| Study features | N (%) |
|---|---|
| Study Design | |
| RCT (including cluster RCT) | 12 (19.7%) |
| Cohort | 34 (55.7%) |
| Cross-sectional | 4 (6.6%) |
| Case report | 1 (1.6%) |
| Qualitative | 1 (1.6%) |
| Protocol only | 9 (14.8%) |
| Year of publication | |
| 2022 | 18 (29.5%) |
| 2021 | 18 (29.5%) |
| 2020 | 10 (16.3%) |
| 2019 | 8 (13.1%) |
| 2018 | 2 (3.3%) |
| 2017 | 2 (3.3%) |
| 2016 | 1 (1.6%) |
| 2015 | 1 (1.6%) |
| 2014 | 1 (1.6%) |
| Region | |
| Southern | 30 (49.2%) |
| Eastern | 15 (24.6%) |
| Western | 12 (19.7%) |
| Multiple | 4 (6.6%) |
| Population studied | |
| AGYW | 20 (32.8%) |
| Women | 8 (13.1%) |
| PBFW | 3 (4.9%) |
| Couples | 6 (9.8%) |
| FSW | 7 (11.5%) |
| MSM | 7 (11.5%) |
| Trangender women | 1 (1.6%) |
| Multiple | 4 (6.6%) |
| Youth | 2 (3.3%) |
| Other/General | 3 (4.9%) |
| Context | |
| Public health/primary care | 16 (26.2%) |
| Sexual and reproductive health | 14 (23.0%) |
| Study clinic | 14 (23.0%) |
| Community based | 7 (11.5%) |
| Maternal and child health | 5 (8.2%) |
| Mobile clinic/venue-based | 2 (3.3%) |
| Multiple | 3 (4.9%) |
| Integration direction | |
| Both services integrated into a third context | 34 (55.7%) |
| STI services within PrEP program | 24 (39.3%) |
| PrEP services within STI program | 3 (4.9%) |
| STI services described (n = 44)a | |
| Laboratory testing at baseline | 33 (75.0%) |
| Laboratory testing at follow up | 20 (45.5%) |
| Syphilis testing only | 2 (4.6%) |
| Syndromic management | 13 (29.6%) |
| Referral for treatment | 3 (6.8%) |
| STI treatment | 30 (68.2%) |
| Partner treatment | 2 (4.6%) |
| STIs and related conditions tested (n = 39)b | |
| Chlamydia | 30 (76.9%) |
| Gonorrhea | 31 (79.5%) |
| Trichomonas | 17 (43.6%) |
| Syphilis | 21 (53.9%) |
| Bacterial vaginosis | 4 (10.3%) |
| Candida | 1 (2.6%) |
| Herpes simplex | 3 (7.7%) |
| Mycoplasma genitalum | 2 (5.1%) |
| Hepatitis B | 12 (30.8%) |
| Testing modality (n = 39)c | |
| Syphilis serology | 13 (29.6%) |
| Syphilis rapid test | 8 (18.2%) |
| GC NAAT | 19 (43.2%) |
| Gonorrhea gram stain | 1 (2.3%) |
| TV NAAT | 6 (13.6%) |
| TV rapid test | 4 (9.1%) |
| Wet mount miscroscopy | 2 (4.6%) |
| Mycoplasma genitalum multiplex assay | 1 (2.3%) |
| HBV serology | 7 (15.9%) |
| HbsAg rapid test | 5 (11.4%) |
| Not specified | 11 (25.0%) |
| Routine testing frequency (n = 39)c | |
| Baseline only | 18 (40.9%) |
| Annual | 1 (2.3%) |
| 6 months | 12 (27.3%) |
| 3 months | 6 (13.6%) |
| Monthly | 2 (4.6%) |
| Other | 2 (4.6%) |
GC, N. gonorrheae and C. trachomatis; TV, T. vaginalis; HBV, hepatitis B; HbsAg, hepatitis B surface antigen; NAAT, nucleic acid amplification test; AGYW, adolescent girls and young women; FSW, female sex workers; MSM, men who have sex with men; PBFW, pregnant and breastfeeding women.
Out of 44 unique study reports (excluding duplicates and studies not reporting specific STI results).
Out of 39 unique studies conducting laboratory/etiologic testing for STIs (5 studies reporting syndromic screening only were excluded).
For studies with multiple screening intervals or different screening intervals for different STIs, the shortest interval of screening was used. For example, routine testing at 6, 12 and 24 months was counted as a 6-month interval of screening.
Most papers focused on a particular population at risk for HIV such as adolescent girls and young women (AGYW) (32.8%), female sex workers (FSWs) (11.5%), and men who have sex with men (MSM) (11.5%). Other common populations of focus included women (including peri-conception) (13.1%), pregnant and breastfeeding women (4.9%) and serodiscordant couples (9.8%). Services were implemented in a variety of contexts, including public health clinics (26.2%), study clinics (23.0%), sexual and reproductive care settings (23.0%), maternal and child health settings (8.2%), community based services (11.5%), and mobile clinics (3.3%).
In most cases, both PrEP and STI services were implemented within a third service setting (55.7%). Less frequently, STI services were implemented within a program with a primary focus on PrEP provision, including PrEP RCTs (39.3%). Few studies reported on PrEP services integrated into a primarily STI-focused program (4.9%).
Table 2 provides a summary of data extraction for studies reviewed, including study setting, population, services provides, assays used, and major outcomes. The type of STI services offered varied and often related to the type of study (RCT, demonstration project or real-world implementation). Most studies and study protocols described STI laboratory testing at baseline (75.0%), with fewer describing any follow up laboratory STI testing (45.5%). A quarter described syndromic management, either with or without any etiological testing (29.6%). Type of STIs included in laboratory testing varied. Of 39 studies and protocols that included etiological STI testing, 30 (76.9%) tested for Chlamydia trachomatis (CT), 31 (79.5%) for Neisseria gonorrhoeae (NG), 21 (53.9%) for syphilis, 17 (43.6%) for trichomonas vaginalis (TV), 4 (10.3%) for bacterial vaginosis (BV), 1 (2.6%) for Candida, 2 (5.1%) for Mycoplasma genitalium, and 3 (7.7%) for HSV.
Table 2.
Data extraction and summary of reviewed studies.
| Study/Author | Setting/region | Study population | Context of service point | Integration direction | STI services described | Type of STIs | Assay type used (e.g., ELIZA, NAAT, POC) | Frequency of testing/specimen type | STI outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Benin demonstration project, Mboup et al 2018 | Benin | Adult FSWs at risk for HIV | Public health/primary care | Both services integrated into a third context | syphilis, yeasts, TV, TC, NG, BV testing | syphilis, yeasts, TV, BV, NG, CT | SD Bioline rapid test and the RPR test for syphilis; Vaginal swabs for direct microscopy of yeasts, Trichomonas vaginalis, and bacterial vaginosis; NAAT for genital gonococcal and chlamydia. | All STIs at baseline; genital GC and CT tested on longitudianl cervical swabs no explicit testing frequency | Baseline prevalence in PrEP group, NG 11.2%, CT 6%, BV 59.4%,, candidiasis 4.0%, and TV 0.4%. Chlamydia incidence was 4.8/100 person-years |
| Benin demonstration project, Giguère et al 2019 | Benin | Adult FSWs at risk for HIV | Public health/primary care | Both services integrated into a third context | TV, TC, NG; free STI treatment for positives | TV, NG, CT | microscopy for TV; NAAT for NG, CT | Vaginal swab at baseline and every 6 months. | Of 255 participants, 120 (47.1%) completed followup. Prevalence of STI decreased from 15.8% (95% CI: 11.8% to 21.0%) at baseline to 2.1% (95% Cl: 0.4% to 10.2%) at 24 |
| 3P, Celum et al 2020 | South Africa | HIV-negative non preganant women ages 16 to 25 in a periurban township outside of Capetown | Study clinic | STI services within PrEP program | Test for TV NG, CT | TV, NG, CT | rapid test for TV; NAAT for NG, CT | STI test at baseline with followup testing frequency unspecified | Baseline prevalence of any curable STIs was 32% overall, CT 25%, NG 11%, TV 6%. Only five women (3%) reported STI symptoms. |
| 4YBY, Iwelunmor et al 2022 | Nigeria | Youth aged 14-24 across Nigeria | Public health/primary care | Both services integrated into a third context | HIV self testing with information to link youth to youth-friendly health clinics for STIs testing and treatment | syphilis, NG, CT | NA | NA | NA |
| ANRS 12381 PRINCESSE, Becquet et al 2021 | Cote d’Ivoire | Adult women engaging in sex work in 19 HIV hotspots in Uganda | Mobile clinic/venue-based | Both services integrated into a third context | Syndromic STI screening, dysplasia testing (+ treatment when necessary), STI treatment | Syphilis, NG, CT | NAAT for GC,CT; Syphilis rapid test | Syndromic screening and etiological testing and treatment baseline then quarterly up to 24 months | NA |
| Anza Mapema, Mehta et al 2021 | Kenya, | HIV negative MSM in Kisumu, Kenya | Study clinic | STI services within PrEP program | GC/CT testing and treatment; syndromic management. | Urethral and/or rectal NG, CT | NAAT for NG, CT | Urethral, and/or rectal CT NG at baseline, 6- and 12- months in urine, and rectal swabs; genital and rectal examination for signs of STIs every 3 months | The prevalence of urethral CT and/or NG infection at baseline was 10.3% (95% CI 6.0–16.2%), decreasing to 7.7% at 6 months (95% CI 4.0–13.1%), and increasing to 10.9% (95% CI 6.4–17.1%) at 12 months. Incidence of urethral CT/NG was 18.5 cases/100 person-years; incidence of rectal CT/NG was 19.9 cases/100 PY |
| CohMSM-PrEP, De Baetselier et al 2019 | Mali, Cote d’Ivoire, Burkina Faso, Togo, | Adult MSM at risk for HIV | Public health/primary care | STI services within PrEP program | STI testing | NG, CT in rectal, urine, and pharynx, TV in urine, and Mycoplasma genitalium (MG) in rectal, urine, and pharynx | NG, CT and TV: NAAT; MG: S-DiagMGTV multiplex assay | At baseline | Chlamydia prevalence was 17.9% (12.3% anorectal, 5.7% urethral) anorectal. Gonorrhea prevalence was 15.8% (10.7% anorectal, 5.7% pharyngeal) MG infection was 26.0% for the Lomé and 27.6% for the Ouagadougou site. Only 1 participant was positive for TV. |
| CohMSM-PrEP, Laurent et al 2021 | Mali, Cote d’Ivoire, Burkina Faso, Togo, | Adult MSM at risk for HIV | Public health/primary care | STI services within PrEP program | Screening and treatment, testing for GC, CT, and syphilis; provision of condoms, testing. | Urethra, rectum, and pharynx NG/CT, syphilis | NG, CT: NAAT; syphilis: treponemal and non-treponemal serology assays | GCCT was tested at months 0, 6, and 12 using urine, anorectal, and pharyngeal samples; syphilis every 3 months in the first year of the follow-up, and once a year thereafter | 7% had STI symptoms at baseline; prevalence of gonorrhoea was 12·6% (73 of 578) at month 0, 11·2% (45 of 402) at month 6, and 14·0% (47 of 336) at month 12. The respective figures were 19·3% (65 of 336), 15·9% (37 of 232), and 20·0% (40 of 200) for chlamydia, and 0·2% (1 of 597), 0·2% (1 of 414), and 1·0% (3 of 340) for syphilis. |
| Community PrEP Study, Peters et al 2021 | South Africa, | AGYW at community-based PrEP program in the Eastern Cape, South Africa | Community-based | STI services within PrEP program | STI testing | NG, CT, TV | NAAT for NG, CT | 6-, 12- and 24-months visits; didn’t specific specimen type; | STI test positivity increased from 23 to 30% for Chlamydia trachomatis, 7% to 14% for Neisseria gonorrhoeae, and 8 to 12% for Trichomonas vaginalis |
| DREAMS, Chabata et al 2021 | Zimbabwe, | Young women who sell sex aged 18-24 years | Community-based | Both services integrated into a third context | syndromic management of STIs | NA | NA | NA | Accessed STI treatment services in the past 12 months at the enrollment: 67/74 (90.5) in the intervention area and 75/93 (80.6) in the non-intervention area. STI symptoms in the last 12 months: 188/963 (19.5) in DREAMS cities, 206/896 (23.0) in non-DREAMS cities |
| ECHO, Beesham et al 2020 | Eswatini, Kenya, South Africa and Zambia,Multiple Africa | HIV- women aged 16–35 years seeking long-acting reversible contraception, randomly assigned to copper intra- uterine device, intramuscular depot medroxyprogesterone acetate, or levonorgestrel implant | Sexual and reproductive health | Both services integrated into a third context | STI testing and treatment, offering condoms | Not specified | Not specified | Not specified | Prevelanc in women who initiated PrEP vs those who did not: CT = (127 (20.4%) vs. 475 (15.8%)); NG 121/3004 (4.0%) vs. 33/622 (5.3%) |
| ECHO, Beesham et al 2021 | South Africa, | HIV negative women, aged 16 to 35 years | Sexual and reproductive health | Both services integrated into a third context | STI testing, treatment and partner notification of STIs; condom provision | Not specified | NAAT | endocervical swabs at enrollment and final visit | 25% had chlamydia and 2.3% had gonorrhea detected at enrolment |
| Healthy Families PrEP Study, Chitneni et al 2020 | Uganda | HIV negative women, 18 to 40 years old, in serodicordant relationship or with partner of unknown serostatus, with plans to conceive | Sexual and reproductive health | Both services integrated into a third context | STIs screening and treatment; partner notifications; patient-delivered partner medications; | Syphilis, NG, CT, and TV | syphilis: a rapid immunochromatographic test (ICT) confirmed by RPR; NG, CT and TV: NAAT | syphilis: blood sample; GCCT and TV: vaginal swabs. STIs were tested at enrollment. | 24% had at least 1 STI including 13% with chlamydia, 2% with gonorrhea, 6% with TV, 6% with syphilis, and 3% with STI coinfection. All STI cases received treatment. 96% received partner notification cards, and 84% received patient delivered partner medications |
| HPTN 082, Celum et al 2021 | South Africa and Zimbabwe | HIV negative women aged 16-25 at risk for HIV | Study clinic | STI services within PrEP program | STIs testing and treatment for those who were tested positive. | Syphilis, NG, CT, and TV | syphilis: RPR followed by a treponemal-specific confirmatory assay; NG, CT: NAAT; TV: rapid test (OSOMTrichomonas Test) | syphilis: blood sample; GCCT and TV: vaginal swabs. STIs were tested at enrollment, 6 months and 12 months. | Rates of STIs were 29% for chlamydia, 8% for NG, 7% TV and <1% for syphilis |
| HPTN 082, Delany-Moretlwe et al 2019 | South Africa, Zimbabwe | HIV negative women 16 to 25 years, at risk for HIV | Study clinic | STI services within PrEP program | STIs testing and treatment for those who were tested positive. | Syphilis, NG, CT, and TV | syphilis: RPR followed by a treponemal-specific confirmatory assay; GCCT: NAAT; TV: rapid test (OSOMTrichomonas Test) | syphilis: blood sample; GCCT and TV: vaginal swabs. STIs were tested at enrollment, 6 months and 12 months. | At baseline 9% of women had CT, 8% GC, 7% TV and 2% reactive syphilis serology. STI incidence was 29.5 per 100 PY for CT, 12.2 per 100 PY for GC, and 6.9 per 100 PY for TV |
| IMARA-SA, Donenberg et al 2021 | South Africa | 15–19-year-old Black South African AGYWs and their female caregivers | Study clinic | Both services integrated into a third context | Education on factors that affect HIV/STIs risk; STIs testing and treatment | NG, CT and TV | NA | baseline, 6-, and 12-month | NA |
| MP3, Sullivan et al 2020 | South Africa | MSM and transgender women in Cape Town and Port Elizabeth | Public health/primary care | Both services integrated into a third context | STIs testing and treatment | Syphilis, NG, CT | syphilis by RPR testing and titres and T pallidum particle agglutination; urethral and rectal CT and NG by PCR testing | blood and urine, and rectal swabs collected at baseline, 6- and 12-month visits | - |
| MP3, Jones et al 2020 | South Africa | MSM and transgender women in Cape Town and Port Elizabeth | Public health/primary care | Both services integrated into a third context | STIs testing and treatment | Syphilis, NG, CT | Syphilis RPR testing and titres and T pallidum particle agglutination; urethral and rectal CT and NG by PCR testing | blood and urine, and rectal swabs collected at baseline, 6- and 12-month visits | Baseline: universal acceptance of urethral (292/292; 100%) screening, near-universal acceptance of syphilis (289/292; 99%) screening, and 189 (64.7%) accepted rectal STI screening. Among those screened, 29 (10%) had urethral CT infection and 8 (3%) had urethral NG; 47 (25%) had rectal CT and 30 (16%) had rectal NG, 50 (18%) had prevalent syphilis. Incident urethral CT was 12.8/100 PY and the rate of incident urethral NG was 7.1/ 100 PY. Incident rectal CT: 33.4/100 PY; Incident rectal NG 26.8/100 PY. The rate of incident syphilis infection was 8.2/100 PY. 91%, 95% and 97% of rectal, urethral, and syphilis infections clinically asymptomatic |
| MyPrEP, Seidman et al 2021 | South Africa | HIV negative women between 18 and 25 years at a public health clinic | Public health/primary care | Both services integrated into a third context | STI testing | NG, CT | Not specified | at screening | 37% of participants has NG or CT |
| Partners PrEP, Celum et al 2014 | Kenya and Uganda | HIV- men and women in serodiscordant partnerships | Study clinic | STI services within PrEP program | STIs testing | HSV-2 | EIA | At baseline | |
| Partners Scale-Up, Irungu et al 2021 | Kenya | Patients at 25 public health clinics in Kenya at risk for HIV | Public health/primary care | STI services within PrEP program | medical assessment and syndromic STI evaluation | Not specified | Not specified | Not specified | STI assessment at 87% of follow up visits |
| POWER, Travill et al 2021 | South Africa | young women, ages 16–25, in South Africa |
Mobile clinic/venue-based | Both services integrated into a third context | STI screening and treatment | NG, CT | NAAT | At baseline | 34% had any curable STI, 27% CT, 3% NG and 3% both; 65% with an STI were successfully contacted and treated |
| POWER, Stewart et al 2019; Rousseau et al 2021 | Kenya | AGYW aged 16–25 | Sexual and reproductive health | Both services integrated into a third context | STI screening and treatment | NG, CT | NAAT | Urine sample was tested at baseline and 6 monthly | 48% (259) tested positive for an STI (NG and/or CT. 17% prevalence of CT and 8% of NG at enrollment. At 6 month follow up, 40.0 per 100 PY cases of chlamydia and 12.3 per 100 PY cases of gonorrhea |
| PREP-PP, Joseph Davey et al 2021 | South Africa | HIV- pregnant women >15 years at first ANC visit | Maternal and child health | Both services integrated into a third context | STI testing | NG, CT, TV | NAAT | At baseline | 35% were diagnosed with an STI |
| PrIYA, Kinuthia et al 2020 | Kenya | HIV- women >15 years at MCH clinics in Kenya | Maternal and child health | Both services integrated into a third context | syphilis screening and syndromic STI management | syphilis and other STIs | RPR testing for syphilis; assays for other STI not specified | syphilis at baseline; syndromic STI management | 1.5% of participants had previously been diagnosed with an STI |
| Safer Conception Intervention for Partners, Heffron et al 2019 | Kenya | HIV serodiscordant couples with fertility desires in Kenya | Sexual and reproductive health | Both services integrated into a third context | STI testing and treatment | NG, CT, TV | Hologic Aptima Gen-probe | diagnostic test was provided monthly | 8 people (out of 74 couples) were infected with chlamydia, 2 with gonorrhea and 3 with trichomonas |
| Sakh’umndeni, Schwartz et al 2017 | South Africa | HIV-affected individuals of reproductive age in relationships in which one or both partners are HIV + and who want to have a child within 6 months | Sexual and reproductive health | Both services integrated into a third context | syphilis screening and syndromic STI management; treatment for those positive | syphilis and other STIs | RPR testing for syphilis; assays for other STIs not specified | syphilis was tested at baseline; monthly follow-up visits for syndromic STI management | Prevalence of symptomatic STIs at enrolment was 4% among women and 3% among men |
| Sakh’umndeni, Iyer et al 2019 Sakh’umndeni, Schwartz et al 2019 |
South africa, | Couples with at least one HIV-positive partner desiring pregnancy | Sexual and reproductive health | Both services integrated into a third context | syphilis screening and syndromic STI management; treatment for those positive | syphilis and other STIs | RPR testing for syphilis; assays for other STIs not specified | syphilis was tested at baseline; monthly follow-up visits for syndromic STI management | Reported STI history, baseline and incident STI detection via syndromic diagnosis through follow up for women was 3% (n = 9/334), 3% (n = 11/334) and 12% (n = 21/182) among women retained through six months of follow-up. Syndromically treated STI at enrollment: 11/334 among women, 5/192 among men; Syphilis diagnosis: 3/334 among women, 1/192 among men. No STI outcomes at follow up visits reported |
| Senegal PrEP Demonstration Project Roberts et al 2020; Sarr et al 2020 | Senegal, | Adult HIV-negative women sex workers in Dakar, Senegal | Public health/primary care | Both services integrated into a third context | free condoms, STI testing and treatment, and counseling | syphilis, NG, CT | Abbott Real Time NG/CT assays, and rapid plasma reagin with Treponema pallidum agglutination assay confirmation for syphilis | STIs testing baseline, months 1, 3, 6, 9, and 12. but due to logistical constraints limited STIs testing was conducted | 40% received gonorrhea and chlamydia testing at least once during the study period, 7.5% tested positive for gonorrhea and 7.5% tested positive for chlamydia. 15.4% of 221 tested women had a positive T. pallidum. Prevalence of syphilis was 1.5%, CT 6.1%, and NG.6% |
| TAPS Demonstration Project, Eakle et al 2017 | South Africa | FSWs at two public health clinics | Public health/primary care | Both services integrated into a third context | free condoms, STI testing and treatment, and counseling | syphilis, NG, CT, | NA | Didn’t specify the testing frequency; blood samples for syphilis | STIs were assessed by syndromic management. At baseline, 17/224 participants were diagnosed with an STI. 3, 3, 2 and 5 additional STIs were diagnosed at 3 months, 6 months, 9 months and 12 months of follow up, respectively |
| TDF2 study Gust et al 2016 | Botswana, | Heterosexual men and women at risk for HIV in Botswana | Study clinic | STI services within PrEP program | free condoms, STI testing and treatment, and partner notification | syphilis, HSV2, NG, CT, TV, BV, Candida spp. | syphilis: Determine® Syphilis TP (Abbott); HSV2: HerpeSelect® IgG ELISA (Focus); Wampole® Impact RPR; HSV2: ELISA; hepB: ELISA; GCCT: COBAS® AMPLICOR PCR Analyzer; TV: TV culture Saline Wet Prep; BV: Premixed Gram stain, BVBlue rapid; Candida spp: KOH wet prep |
syphilis: Whole blood from fingerstick at Enrollment visit and annually; HSV2: Whole blood from phlebotomy at Enrollment visit; hepB: Whole blood from phlebotomy at Screening visit; GN, CT, TV: Cervical/vaginal swab (women) or Urine (men) at baseline and every 6 months; Candida spp: Vaginal or penile glans swab. | |
| VOICE, Marrazzo et al 2015 | South Africa, Uganda, and Zimbabwe,Multiple Africa | Women 18-45 years, not pregnant, at risk for HIV | Study clinic | STI services within PrEP program | STI testing, condoms | syphilis, hepB, NG, CT, TV, BV, Candida spp. | NG, CT: strand-displacement amplification assay; TV: OSOM Trichomonas Rapid Test; syphilis: rapid plasma reagin screening test followed by a confirmatory microhemagglutinin assay for Treponema pallidum or a T. pallidum hemagglutination assay for reactive samples; HSV2: Herpe Select 2 enzyme immunoassay; BV: Nugent score | enrollment, annually, and when indicated. Vaginal fluid was collected for BV other didn’t specify. | Baseline revalence: CT 12%; NG 3%, TV 6%, syphilis 1%, HSV-2 46%, BV 40%. 10% chlamydia, 6% trichomonas, 3% gonorrhea, 1% syphilis of reported 10% chlamydia, 6% trichomonas, 3% gonorrhea, 1% syphilis). In the TDF/FTC group: 14% chlamydia, 6% trichomonas, 5% gonorrhea, 1% syphilis among those reporting SAE |
| Peer-Delivered HIVST, STI Self-Sampling and PrEP for Transgender Women in Uganda 2020 | Uganda | Transgender women 14 years or older at risk for HIV | Community-based | Both services integrated into a third context | peer delivered STI Self-Sampling | NA | NA | NA | |
| Kitenge et al 2021 | South Africa | HIV negative women 18 to 35 years old at community HIV testing sites in KwaZulu Natal | Community-based | Both services integrated into a third context | STI screening and treatment | NA | NA | STI testing was conducted at 3-, 6- and 12-month follow-up visits | |
| Heffron et al 2021 | South Africa | 18 and 25 years old, willing to use contraception (condoms included), HIV and Hepatitis B, uninfected,and not pregnant or breastfeeding. | Sexual and reproductive health | Both services integrated into a third context | STI screening and treatment | syphilis, NG, CT | RPR tests for syphilis, and Aptima GenProbe or GeneXpert for GCCT | Blood sample for syphilis and urine sample for GCCT; one time testing | Chlamydia in 18.2%, gonorrhea in 2%, syphilis in 0% |
| Behanzin et al 2021 | Kenya | Women 15-30 years old, receiving care for pregnancy loss at 3 Kenyan facilities | Sexual and reproductive health | Both services integrated into a third context | STI testing | HBV HCV | immuno-chromatographic test was used for detecting HBV surface antigen (HBsAg, active infection) and HCV antibodies in whole blood. Enzyme immunoassays were used for detecting HBV core (anti- HBc) and surface (anti-HBs) antibodies | blood sample was collected once | Prevalence of active and lifetime HBV were 8.8% and 37.7%, respectively. 0.98% of participants were positive for HCV |
| Wahome et al 2020 | Benin | MSM from the community-based PrEP demonstration study in Cotonou, Benin | Community-based | STI services within PrEP program | syndromic STI management | NG, CT, syphilis | Positive RPR titre confirmed by Treponema pallidum haemagglutination assay (TPHA) for syphilis; NG, CT was diagnosed by detection of Gram-nega-tive, intracellular diplococci | baseline and quarterly follow up; blood sample for syphilis and urethral or rectal secretions for NG, CT | Only 1 participant (0.6%) had STI at baseline (testing for syphilis and gonorrhea done) |
| Oluoch et al 2021 | Kenya | AGYW in Kenya | Public health/primary care | STI services within PrEP program | STI testing | NG, CT, TV | NA | quarterly with STI testing | 12% of AGYW tested positive for an STI. |
| Cassidy et al 2021 | Kenya | NA | Public health/primary care | STI services within PrEP program | syndromic STI management and treatment | NA | NA | month 1 and 2 visits, and thereafter returned every two or three months | 10/72 STI positive among enrolled, 19/164 among PrEP initiated; In the first six months of follow-up, 16 women (27.6%) had a syndromic STI, decreasing to 8 (13.8%) in the final six months |
| Masyuko et al 2018 | Kenya | Adult MSM at risk for HIV in Mtwapa town | Study clinic | STI services within PrEP program | NA | NA | NA | NA | The key indicators for routine tracking iin the PrEP monitoring and evaluation program include number diagnosed with STI |
| Medina-Marino et al 2022 | South Africa | AGYW from study clinic | Study clinic | STI into PrEP program | Baseline testing for CT, NG, TV and syphilis | CT, NG, TV, syphilis | CT, NG, TV NAAT, rapid syphilis testing | baseline; vaginal swab | At enrolment, 227 (37.6%) participants had a positive STI test result, of which 134 (59.0%) were asymptomatic. Chlamydia trachomatis (CT, n = 182; 30.6%) accounted for the highest-burden STI, followed by Neisseria gonorrhoeae (NG, n = 59; 10.0%), Trichomonas vaginalis (TV, n = 42; 7.1%) and syphilis (n = 2, 0.3%) |
| Velloza et al 2022 | South Africa | AGYW from youth focused HIV clinic in Johannesburg | Youth-focused HIV clinic | STI into PrEP program | Etiologic testing and treatment of curable STIs (GCCT, syphilis,TV) at enrolment, 6 months and study exit | NG, CT, TV, syphilis | NA | enrolment, 6 months and study exit; specimen type not specified | NA |
| Beesham et al 2022 | Durban, South Africa | AGYW in sexual and reproductive health clinics | Sexual and reproductive health | PrEP/STI into third context | STI testing at baseline | NG, CT | NAAT | At baseline; swabs | At PrEP initaiton, 33 and 3 women were diagnosied with Chlamydia trachomatis and Neisseria gonorrhoea respectively. |
| Stewart et al 2022 | Kenya | HIV negative, non-pregnant young women (18-20 yo) using PrEP research clinic in Kisumu | Research clinic | STI into PrEP program | treatment arm: doxycycline as STI prevention strategy; treatment and control arm: STI screening (Chlamydia trachomatis, Neisseria gonorrhoeae, and Treponema pallidum) and treatment and risk-reduction counseling without dPEP | NG, CT, and Treponema pallidum; for future testing: staphylococcus aureus, bv, MG, and vaginal microbiome | NG, CT & TV: NAAT; syphilis: RPR or fourfold increase in non-treponemal titers; | At baseline, 3 months blood sample; endocervical swabs | NA |
| Davey et al 2022 | South Africa | Pregnant and breastfeeding women Antenatal care | Antenatal care | PrEP/STI into third context | Baseline CT, NG, TV etiologic testing and treatment | GC, CT, TV | Point of care PCR testing | Baseline; vaginal swab | 30% STI diagnosed at baseline; 14% STI diagnosed and treated same day |
| Ndenkeh et al 2022 | Cameroon | FSW and MSM in drop-in centers of the participating community-based organization partners | Community-based organization | STI into PrEP program | monthly STI screening | STI (not specified); syphilis | TPHA and VDRL tests for syphilis | monthly; specimen type not specified | Not being reported |
| Skovdal et al 2022 | Zimbabwe | AGYW in clinics in Eastern Zimbabwe | community in ann urban suburb and a rural village | PrEP/STI into third context | General SRH services | NA | NA | NA not specified | NA |
| Rutstein et al 2022 | Malawi | STI clients that are eligible for PrEP use; STI clinic staff | STI clinic | PrEP into STI program | STI testing and treatment | NG, CT, syphilis | GCCT: NAAT; syphilis: rapid plasma regain, Treponema pallidum particle agglutination; | baseline, 3 months after; urine and blood samples | NA |
| Chidumwa et al 2022 | South Africa | Young men and women aged 16-29 years from public health/primary care; community-based | Community-based public health/primary care clinics | PrEP/STI into third context | Etiologic testing; syndromic management | NG, CT, TV | samples are sent to AHRI laboratories to be processed | baseline; urine and blood samples | NA |
| Moran et al 2022 | South Africa | Pregnant and breastfeeding women Antenatal care | Antenatal care | PrEP/STI into third context | Baseline CT, NG, TV etiologic testing and treatment | NG, CT, TV | Point of care PCR testing | baseline vaginal swab | STI prevalence of CT, NG and/or TV was 35% at first ANC visit |
| Mantell et al 2022 | Kenya | Male clients of female sex workers, HIV negative aged at least 18-year-old in Kisumu County | Clinical reserach site | STI into PrEP program | STI testing at baseline and refered for the treatment | NG, CT, trich | specific method did get specified | baseline; urine sample blood and urine samples | NA |
| Mayanja et al 2022 | Uganda | AGYW from GWHP clinic in Uganda | GWHP clinic serving AGYW in Uganda | STI into PrEP program | STI testing | CT, NG, syphilis | GCCT NAAT, rapid syphilis, HBV serology | 3 months; Endo-cervical swabs | 26.9% STI at enrolment |
| Inghels et al 2022 | Eswatini | Clients visiting 6 public sector healthcare facilities that provide free ART and PrEP servcies | public sector healthcare facilities | PrEP into STI program | existing STI care | Not specified | Not specified | Not specified | Lower PrEP uptake was found for individuals seeking antenatal care (30.5%, 64/210), STI (30.9%, 29/94) and family planning visits (31.0%, 84/271); majority of people seeking STI services preferred PrEP delivery at outpatient services (66.7%) |
| Celum et al 2022 | Kenya and South Africa | AGYW seeking family planning and SRH service and primary care and eligible for PrEP use | family planning clinics, mobile clinics, and public primary healthcare | STI into PrEP program | STI testing and treatment at baseline and 6 months | NG, CT | NAAT | baseline and 6 months; specimen type not specified | 29% had chlamydia and10% gonorrhoea at baseline; The incidence of C. trachomatis and N. gonorrhoeae was 42.9/100 person-years (95% CI 37.2, 49.2)—35.4/100 person-years for C. trachomatis (95% CI 30.3, 41.2) and13.0/100 person-years for N. gonorrhoeae (95% CI10,0,16.7) |
| Mansoor et al 2022 | South Africa | AGYW from study clinic | Study clinic | STI into PrEP program | STIs (NG, CT and TV) and BV testing were performed at enrolment and study exit. STI treatment and contact tracing | CT, NG, TV | NAAT | At baseline and study exit; genital swab | STI in 22.4%, BV in 56.4% |
| Medina-Marino et al 2023 | South Africa | AGYW from study clinic | Study clinic | STI into PrEP program | Baseline testing for CT, NG, TV and syphilis | CT, NG, TV, syphilis | CT, NG, TV NAAT, rapid syphilis testing | At baseline; vaginal swab | At enrolment, 227 (37.6%) participants had a positive STI test result, of which 134 (59.0%) were asymptomatic. Chlamydia trachomatis (CT, n = 182; 30.6%) accounted for the highest-burden STI, followed by Neisseria gonorrhoeae (NG, n = 59; 10.0%), Trichomonas vaginalis (TV, n = 42; 7.1%) and syphilis (n = 2, 0.3%) |
Prevalence of STIs varied between studies. Baseline prevalence of genitourinary CT, NG, TV ranged from 5.6–30.8%, 0.0–11.2%, and 0.4–8.0% respectively. Baseline prevalence of syphilis ranged from 0.0–18.0%. Baseline prevalence of symptomatic STI by syndromic screening ranged from 0.0–11.6%. STIs detected by routine laboratory testing were reported to be frequently asymptomatic. In one study of MSM receiving PrEP, 91%, 95% and 97% of rectal, urethral and syphilis infections were clinically asymptomatic (11). In one study of AGYW receiving PrEP, baseline STI prevalence was 32%, though only 3% reported symptoms (12), while another study of AGYW presenting for HIV testing services reported 38% STI prevalence at baseline, of which 59% were asymptomatic (13). Etiological testing frequency ranged from monthly to baseline testing only.
A few distinct models of integration of STI services with PrEP emerged from our review. These included routine integration of etiologic STI testing within PrEP RCTs, routine integration of syndromic STI management within public health clinics offering PrEP, etiological screening for STIs within PrEP programs targeting at-risk groups, and community outreach and mobile-based approaches. Of these, novel approaches to integration of PrEP and STI services included use of mobile clinics and other youth-focused approaches to increase convenience and acceptability (14, 15), and provision of STI testing results as a tool for improving retention in PrEP (16). However, in most studies STI diagnosis and treatment were offered as part of a standard package of PrEP services without a focus on improving either service through integration.
Few studies described quantitative or qualitative outcomes relating to implementation of integrated PrEP and STI services. Qualitative interviews from one study evaluating mobile provision of sexual and reproductive health services including STI and PrEP services found that AGYW appreciated the practicality of service integration (14). In contrast, healthcare providers in another study cited stigma as a reason not to integrate PrEP with other sexual health services (17). There was some evidence of synergy between PrEP and STI services. One report demonstrated improved uptake of PrEP services when results of STI testing was made available to AGYW (18). Several studies demonstrated an association between positive STI diagnosis and PrEP acceptance (19, 20). Implementation science research relating to STI and PrEP service integration was very limited. One study described logistical constraints limiting availability of laboratory STI testing, but these were not explored in detail (21). One research protocol described a planned study comparing standard of care syndromic management with community-based STI services including etiologic testing, but no results are yet available (22).
Discussion
This scoping review describes existing literature around integration of STI and PrEP services in SSA. Prior literature describing provision of both these services covers a range of implementation settings, from public health clinics, sexual and reproductive health settings, mobile clinics and in the community. Most studies targeted particular at-risk groups, such as AGYW, FSW or MSM. Studies largely occurred within an existing service setting or within a PrEP program, but in nearly all studies, PrEP was the primary focus.
Despite a growing interest and rollout of PrEP in SSA, and an ongoing epidemic of curable STIs, we found limited literature covering the integration of PrEP and STI services from an implementation science perspective. Few studies addressed barriers and facilitators of integration of PrEP and STI programs. Prior qualitative work has demonstrated that challenges facing PrEP implementers in incorporating STI services include financial barriers to laboratory STI testing, logistical barriers to STI treatment in mobile settings, time constraints, lack of equipment and lack of training and capacity building around STI services(7). However, our review found a lack of evidence base addressing these barriers. In addition, while a few studies indicated potential synergies between STI and PrEP services in terms of service uptake and client satisfaction, this was not explored in detail. Most studies reported results of STI testing when offered as part of PrEP services, but did not explore the effect of bundling these services on outcomes such as acceptability or adoption.
Types of STI services offered varied widely between studies and settings, reflecting the different funding and implementation environments between RCTs, demonstration projects, and studies of real-world implementation. Some studies reported diagnostic STI screening only at baseline, while others conducted routine screening at regular intervals, and others only performed syndromic managements of STIs. The intervals of routine screening, when performed, was variable, as were the types of STIs screened. Current national PrEP guidelines in countries such as Kenya, Uganda and South Africa do not offer detailed guidance on how STI screening should be conducted (3–5), including standard guidance regarding which STIs to screen, site and frequency of screening in different populations.
Of note, laboratory diagnostic testing of STIs was mainly limited to well funded clinical studies and demonstration projects, with limited evidence from real-world public health settings. Where reported, STI prevalence and incidence by laboratory testing were high among most PrEP cohorts (11, 14, 17, 19, 23–29), with the exception of two studies of safer conception cohorts, which reported low rates of laboratory-diagnosed STIs (30, 31). In many settings, STIs diagnosed by laboratory screening were asymptomatic (12, 26, 33), reaffirming the pressing need to incorporate etiological diagnostics in STI programs offered within PrEP services.
Our scoping review has limitations. Due to the nature of the scoping review, reviewers did not assess study quality but instead gathered existing knowledge on STI services offered with PrEP programs. The review may not have captured all studies related to this topic, including sources of grey literature beyond NGO and IGO reports searched in our review. Furthermore, studies published in languages other than English were not included. Our review included abstract and study protocols in order to capture emerging literature given the relative novelty of study on the topic of PrEP and STI integration; the data collected from these sources may be less reliable than traditional peer-reviewed articles. Given the rapid emergence of literature around PrEP, our review may have failed to capture most recently published or presented literature on this topic.
Despite growing acknowledgement of the limitations of syndromic management (2), which is currently the standard practice in SSA regarding STI services within PrEP programs, few studies have addressed real-world integration of expanded STI services within PrEP programs in SSA. Future studies should examine how inclusion of additional STI services affects acceptability, adoption, and client satisfaction with both PrEP and STI services. In addition, studies should investigate cost, feasibility, and best practices regarding implementing etiologic STI diagnosis and treatment into PrEP programs in real world settings. Finally, more work in needed to understand practice setting and population-specific needs regarding integration of STI and PrEP services, including what services best suit key populations such as AGYW, MSM, FSW, and heterosexual couples, as well as how to best offer PrEP services within existing STI service contexts.
Conclusions
In this scoping review, we found a range of STI services integrated with PrEP programs in SSA. STIs are common among populations using PrEP in SSA, highlighting the need for integration of these services. There was some evidence that integration of STI and PrEP services improves uptake of and satisfaction with both PrEP and STI services but more rigorous studies are needed to describe synergies, barriers and best practices for integration of PrEP and STI programs in SSA.
Funding Statement
This work was supported by funding from the National Institute of Mental Health of the US National Institutes of Health (grant R01 MH123267 and R00 MH118134). The funders had no role in study design or writing of the report.
Author contributions
PA, LW, and KKM contributed to the conception and design of the review plan; PA and LW conducted the initial literature review and screening process. AP, with LW, prepared the first draft of the manuscript. PA, LW, and KKM contributed to the writing and critical revision of the paper. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2023.944372/full#supplementary-material
References
- 1.UNAIDS. FACT SHEET 2022. Published (2022). Available at: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf (Accessed December 18, 2022).
- 2.WHO. Prevention and Control of Sexually Transmitted Infections (STIs) in the Era of Oral Pre-Exposure Prophylaxis (PrEP) for HIV. (2019). Available at: https://www.who.int/publications/i/item/prevention-and-control-of-stis-in-the-era-of-prep-for-hiv (Accessed March 24, 2022).
- 3.Uganda Ministry of Health. Consolidated guidelines for the prevention and treatment of HIV and aids in Uganda. (2018). Available at: https://elearning.idi.co.ug/pluginfile.php/5675/mod_page/content/19/Uganda%20HIV%20%20Guidelines%20-%20September%202018.pdf (Accessed March 24, 2022).
- 4.National AIDS & STI Control Program (NASCOP). Guidelines on Use of Antiretroviral Drugs for Treating and Preventing HIV Infection in Kenya. (2018). Available at: http://cquin.icap.columbia.edu/wp-content/uploads/2017/04/ICAP_CQUIN_Kenya-ARV-Guidelines-2018-Final_20thAug2018.pdf (Accessed March 24, 2022).
- 5.Bekker LG, Rebe K, Venter F, Maartens G, Moorhouse M, Conradie F, et al. Southern African Guidelines on the safe use of pre-exposure prophylaxis in persons at risk of acquiring HIV-1 infection. South Afr J HIV Med. (2016) 17(1):2–7. 10.4102/SAJHIVMED.V17I1.455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zablotska IB, Baeten JM, Phanuphak N, McCormack S, Ong J. Getting pre-exposure prophylaxis (PrEP) to the people: opportunities, challenges and examples of successful health service models of PrEP implementation. Sex Health. (2018) 15(6):481–4. 10.1071/SH18182 [DOI] [PubMed] [Google Scholar]
- 7.Ong JJ, Fu H, Baggaley RC, Wi TE, Tucker JD, Smith MK, et al. Missed opportunities for sexually transmitted infections testing for HIV pre-exposure prophylaxis users: a systematic review. J Int AIDS Soc. (2021) 24(2):2–7. 10.1002/jia2.25673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169(7):467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 9.Models of integration of pre-exposure prophylaxis and sexually transmitted infection services in sub-Saharan Africa: a scoping review protocol. Available at: https://figshare.com/articles/online_resource/Models_of_integration_of_pre-exposure_prophylaxis_and_sexually_transmitted_infection_services_in_sub-Saharan_Africa_a_scoping_review_protocol/19209396 (Accessed March 24, 2022). [DOI] [PMC free article] [PubMed]
- 10.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5(1):210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones J, Sanchez TH, Dominguez K, Bekker LG, Phaswana-Mafuya N, Baral SD, et al. Sexually transmitted infection screening, prevalence and incidence among South African men and transgender women who have sex with men enrolled in a combination HIV prevention cohort study: the sibanye methods for prevention packages programme (MP3) project. J Int AIDS Soc. (2020) 23(S6):e25594. 10.1002/JIA2.25594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Celum CL, Gill K, Morton JF, Stein G, Myers L, Thomas KK, et al. Incentives conditioned on tenofovir levels to support PrEP adherence among young South African women: a randomized trial. J Int AIDS Soc. (2020) 23(11):e25636. 10.1002/jia2.25636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Medina-Marino A, Bezuidenhout D, Ngwepe P, Bezuidenhout C, Facente SN, Mabandla S, et al. Acceptability and feasibility of leveraging community-based HIV counselling and testing platforms for same-day oral PrEP initiation among adolescent girls and young women in eastern cape, South Africa. J Int AIDS Soc. (2022) 25(7):5. 10.1002/jia2.25968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rousseau E, Bekker LG, Julies RF, Celum C, Morton J, Johnson R, et al. A community-based mobile clinic model delivering PrEP for HIV prevention to adolescent girls and young women in Cape Town, South Africa. BMC Health Serv Res. (2021) 21(1):888. 10.1186/S12913-021-06920-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Travill D, Ndlovu M, Kidoguchi L, Tlou T, Lunika L, Morton J, et al. Integrating STI screening into PrEP services for adolescent girls and young women (AGYW) in two primary health care (PHC) facilities in Johannesburg: lessons from prevention options for women evaluation research (POWER). J Int AIDS Soc. (2021) 24(S1):28–9. [Google Scholar]
- 16.Eakle R, Gomez GB, Naicker N, Bothma R, Mbogua J, Cabrera Escobar MA, et al. HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: results from a prospective observational demonstration project. PLoS Med. (2017) 14(11):e1002444. 10.1371/JOURNAL.PMED.1002444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skovdal M, Magoge-Mandizvidza P, Dzamatira F, Maswera R, Nyamukapa C, Thomas R, et al. Improving access to pre-exposure prophylaxis for adolescent girls and young women: recommendations from healthcare providers in eastern Zimbabwe. BMC Infect Dis. (2022) 22(1):399. 10.1186/s12879-022-07376-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oluoch LM, Roxby A, Mugo N, Wald A, Ngure K, Selke S, et al. Does providing laboratory confirmed STI results impact uptake of HIV pre-exposure prophylaxis (PrEP) uptake among Kenyan adolescents girls and young women? A descriptive analysis. Sex Transm Infect. (2020) 97(6):467–8. 10.1136/sextrans-2020-054637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Celum C, Hosek S, Tsholwana M, Kassim S, Mukaka S, Dye BJ, et al. PrEP uptake, persistence, adherence, and effect of retrospective drug level feedback on PrEP adherence among young women in Southern Africa: results from HPTN 082, a randomized controlled trial. PLoS Med. (2021) 18(6):e1003670. 10.1371/JOURNAL.PMED.1003670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beesham I, Heffron R, Evans S, Baeten JM, Smit J, Beksinska M, et al. Exploring the use of oral Pre-exposure prophylaxis (PrEP) among women from durban, South Africa as part of the HIV prevention package in a clinical trial. AIDS Behav. (2021) 25(4):1112–9. 10.1007/S10461-020-03072-0/TABLES/4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts DA, Hawes SE, Bousso Bao MD, Ndiaye AJ, Gueye D, Raugi DN, et al. Trends in reported sexual behavior and Y-chromosomal DNA detection among female sex workers in the Senegal preexposure prophylaxis demonstration project. Sex Transm Dis. (2020) 47(5):314. 10.1097/OLQ.0000000000001175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chidumwa G, Chimbindi N, Herbst C, Okeselo N, Dreyer J, Zuma T, et al. Isisekelo sempilo study protocol for the effectiveness of HIV prevention embedded in sexual health with or without peer navigator support (Thetha Nami) to reduce prevalence of transmissible HIV amongst adolescents and young adults in rural KwaZulu-Natal: a 2 × 2 factorial randomised controlled trial. BMC Public Health. (2022) 22(1):454. 10.1186/s12889-022-12796-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G, Palanee T, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. (2015) 372(6):509–18. 10.1056/NEJMOA1402269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chitneni P, Bwana MB, Owembabazi M, O'Neil K, Kalyebara PK, Muyindike W, et al. STI Prevalence among women at risk for HIV exposure initiating safer conception care in rural, southwestern Uganda. Sex Transm Dis. (2020) 47(8):e24. 10.1097/OLQ.0000000000001197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Delany-Moretlwe S, Mgodi N, Bekker L-G, Baeten J, Pathak S, Donnell D, et al. O10.3 high curable STI prevalence and incidence among young African women initiating PrEP in HPTN 082. Sex Transm Infect. (2019) 95(Suppl 1):A60–1. 10.1136/SEXTRANS-2019-STI.160 [DOI] [Google Scholar]
- 26.Li C, Tang W, Wang C, Yang B, Peters R, Medina-Marino A, et al. P167 impact of COVID-19 on adolescent girls and young women in a community-based HIV PrEP programme in South Africa. Sex Transm Infect. (2021) 97(Suppl 1):A102. 10.1136/SEXTRANS-2021-STI.268 [DOI] [Google Scholar]
- 27.Laurent C, Dembélé Keita B, Yaya I, Le Guicher G, Sagaon-Teyssier L, Agboyibor MK, et al. HIV pre-exposure prophylaxis for men who have sex with men in West Africa: a multicountry demonstration study. Lancet HIV. (2021) 8(7):e420–8. 10.1016/S2352-3018(21)00005-9 [DOI] [PubMed] [Google Scholar]
- 28.De Baetselier I, Crucitti T, Yaya I, Dembele B, Mensah E, Dah E, et al. Prevalence of STIs among MSM initiating PREP in West-Africa (COHMSM-PREP ANRS 12369-expertise France). Sex Transm Infect. (2019) 95:A245. 10.1136/SEXTRANS-2019-STI.617 [DOI] [Google Scholar]
- 29.Mehta SD, Okall D, Graham SM, N'gety G, Bailey RC, Otieno F. Behavior change and sexually transmitted incidence in relation to PREP use among men who have sex with men in Kenya. AIDS Behav. (2021) 25(7):2219–29. 10.1007/S10461-020-03150-3 [DOI] [PubMed] [Google Scholar]
- 30.Heffron R, Ngure K, Velloza J, Kiptinness C, Quame-Amalgo J, Oluch L, et al. Implementation of a comprehensive safer conception intervention for HIV-serodiscordant couples in Kenya: uptake, use and effectiveness. J Int AIDS Soc. (2019) 22(4):5. 10.1002/JIA2.25261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwartz SR, Bassett J, Holmes CB, Yende N, Phofa R, Sanne I, et al. Client uptake of safer conception strategies: implementation outcomes from the Sakh’umndeni safer conception clinic in South Africa. J Int AIDS Soc. (2017) 20(Suppl 1):46. 10.7448/IAS.20.2.21291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garrett NJ, McGrath N, Mindel A. Advancing STI care in low/middle-income countries: has STI syndromic management reached its use-by date? Sex Transm Infect. (2017) 93(1):4–5. 10.1136/sextrans-2016-052581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaida A, Dietrich JJ, Laher F, Beksinska M, Jaggernath M, Bardsley M, et al. A high burden of asymptomatic genital tract infections undermines the syndromic management approach among adolescents and young adults in South Africa: implications for HIV prevention efforts. BMC Infect Dis. (2018) 18(1):4–5. 10.1186/S12879-018-3380-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.