Abstract
Gout is a metabolic disorder characterized by hyperuricemia and deposition of monosodium urate crystals in the joint spaces and other extraarticular locations. We report the case of a 40-year-old male who presented for consultation regarding gouty tophi on the phallus, an unusual location for tophi deposition, which was resolved with surgical removal. We provide a brief review of the pathophysiology of gout and its treatment modalities, both medical and surgical.
1. Introduction
Gout is a systemic disorder characterized by recurrent episodes of inflammatory arthritis and elevated serum levels of uric acid leading to the formation and deposition of monosodium urate crystals in intraarticular spaces and less commonly, in extraarticular locations. Long-standing, uncontrolled gout is identified by the presence of subcutaneous lesions known as gouty tophi.1 These tophi commonly occur in specific locations such as the helix or antihelix of the ear, the olecranon bursae, the ligaments around the kneecap, the Achilles tendon, the skin and subcutaneous tissues of the upper and lower extremities. The subcutaneous lesions can vary in number, size, and shape, and typically have a yellowish-white color with a firm, smooth, or ulcerated appearance. We present a case of a patient with gouty tophi located on the phallus, an uncommon occurrence.
2. Case presentation
A 40-year-old male with seronegative rheumatoid arthritis presented to the urology clinic with penile-swelling for the past two years. He endorsed difficulty retracting the foreskin and pain with erections and intercourse. Six weeks earlier, the patient was evaluated by dermatology for similar “skin bumps” in other places of the body. He underwent biopsy of a right upper extremity skin lesion and pathology was consistent with gouty tophi. In the interim, rheumatology started him on allopurinol, prednisone, and colchicine to treat for diagnosis of chronic tophaceous gout. On physical examination, the phallus was uncircumcised with clusters of soft subcutaneous yellow papules at the dorsal foreskin (Fig. 1). The foreskin was minimally retracted due to discomfort (Fig. 2). Given his symptoms, a surgical excision of the penile lesion with circumcision was performed for cosmesis and relief of his symptomatology. The final pathology of the excised fragment/foreskin was consistent with gouty tophus. Additional images of the phallus during exam under anesthesia and after excision of the tophus are shown in Fig. 3.
Fig. 1.
Subcutaneous tophi on surface of penis.
Fig. 2.
Minimal retraction of penile foreskin was possible due to the presence of subcutaneous tophi.
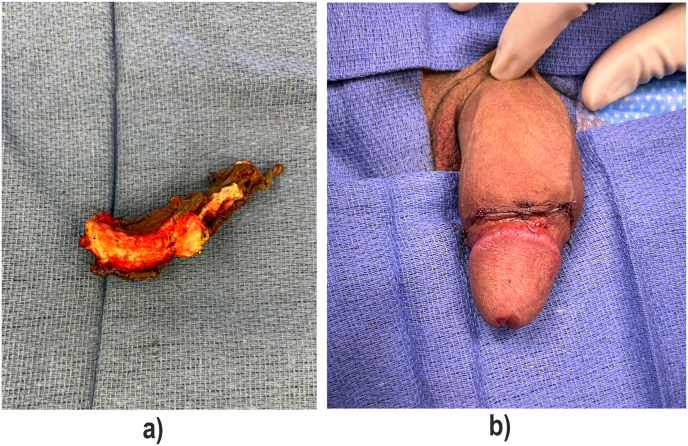
Fig. 3.
Post-op images: Panel A: Excised tophus, Panel B: Surgically repaired phallus.
3. Discussion
Gout is a metabolic disorder characterized by the buildup of monosodium urate crystals in the joints and other tissues. It primarily affects individuals with consistent hyperuricemia, caused either by increased production or decreased excretion of uric acid.1 Gout is more common in men than in women.2,3
Gout has two main clinical phases. The first phase is characterized by intermittent acute attacks of gouty arthritis that spontaneously resolve over a period of seven to ten days. If hyperuricemia goes untreated, transition to the second phase may occur, manifested as chronic tophaceous gout.1 In chronic tophaceous gout, tophi, or masses of urate crystals surrounded by inflammatory cells, begin to develop.4 These tophi, visible under the skin, commonly appear after approximately five years of gouty arthritis development and are typically found in areas such as the olecranon bursa, infrapatellar and Achilles tendons, subcutaneous tissue of the forearms' extensor surfaces, and joints. Infrequently, intradermal tophi may occur on the palms and fingertips.5
Primary treatment for chronic tophaceous gout involves lifestyle modifications such as weight reduction, adopting increasing fluid intake, starting a low-purine diet, reducing alcohol consumption, and discontinuing diuretics. If these measures fail to lower uric acid levels, medications will be necessary. The choice of medication depends on each patient's unique medical history. The use of uricosuric drugs has been shown to reduce tophaceous gout and associated arthritic changes by nearly 50%.2 Probenecid can be used in patients with normal kidney function, while alternative uricosuric drugs or allopurinol are preferred for patients with renal failure or those taking diuretics. In the case discussed, the patient received mainly allopurinol treatment, but the tophi remained uncontrolled.
Surgical intervention may be considered when medical treatments prove ineffective, typically due to inadequate response or functional impairment caused by the compression of surrounding structures, as in this case where retraction of the foreskin had become difficult and painful.
Gouty tophi in the penis is exceptionally rare. Therefore, no specific, standard treatment currently exists. In cases where medical treatment with a uricosuric or allopurinol fails and symptoms persist, surgical removal may be considered as was done in this case.
Ethics statement
This study was approved by institutional ethics committee. The participant has provided written informed consent for publication in this study. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author statement
Mustafa Farooqi: Manuscript Preparation-Original Draft.
Osamah Hasan: Manuscript Editing.
Ryan W. Dobbs: Supervision.
Funding
None.
Declaration of competing interest
The authors declare no conflicts of interest.
Acknowledgements
The authors have no financial or proprietary interest in the subject matter of this article.
Contributor Information
Mustafa Farooqi, Email: mustafa_s_farooqi@rush.edu.
Osamah Hasan, Email: osamah.hasan@midwestern.edu.
Ryan W. Dobbs, Email: ryan.dobbs@cookcountyhhs.org.
References
- 1.Neogi T. Gout. New England J Med. 2021;382(9):866–874. doi: 10.1056/NEJMra1909844. [DOI] [Google Scholar]
- 2.Roddy E., Choi H.K., Dalbeth N. Gout - a disorder of uric acid metabolism. Nat Rev Rheumatol. 2014;10(11):653–662. doi: 10.1038/nrrheum.2014.159. [DOI] [Google Scholar]
- 3.Richette P., Doherty M., Pascual E., et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis. 2017;76(1):29–42. doi: 10.1136/annrheumdis-2016-209707. [DOI] [PubMed] [Google Scholar]
- 4.Choi H.K., Mount D.B. Rationale for considering the kidney as a target for gout therapy. Arthritis Res Ther. 2005;7(1):1–7. doi: 10.1186/ar1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vazquez-Mellado J., Morales E.M., Pacheco-Tena C., Burgos-Vargas R., Hernandez-Cuevas G., Oritz-Franco M. de L. The meaning of gouty tophi and their diagnostic value. J Rheumatol. 1997;24(6):1106–1109. [Google Scholar]