Abstract
Background/Objective
Adults with asthma who experience difficulties in emotion regulation are prone to developing psychopathological symptoms that may affect their self-management activities and symptom control. The current research investigated the role of psychological flexibility and cognitive emotion regulation strategies in relation to mental health outcomes (psychological distress and quality of life) among patients with asthma in Pakistan.
Method
A sample of 200 adults, diagnosed with asthma (32% men, 68% women; Mage = 42.32, SDage = 16.99), completed the acceptance and action questionnaire (AAQ-II) cognitive emotion regulation questionnaire (CERQ), depression, anxiety, stress scale-21 (DASS-21), asthma-related quality of life questionnaire (AQLQ) and a self-structured demographic sheet.
Results
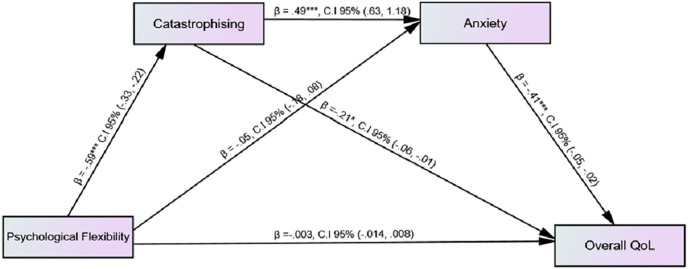
Results of Pearson product moment correlation showed that most of the adaptive cognitive emotion regulation strategies (positive refocusing, refocus on planning, and positive reappraisal) were positively correlated with psychological flexibility and quality of life, whereas negatively correlated with psychological distress. All the maladaptive strategies of cognitive emotion regulation had a significant inverse relationship with psychological flexibility and quality of life, while positively correlated with psychological distress. Results of serial mediation analysis through PROCESS MACRO showed that catastrophising and anxiety fully mediated the relationship between psychological flexibility and asthma-related quality of life.
Conclusion
Evidence-based interventions should focus on developing psychological flexibility and identifying maladaptive patterns of cognitive emotion regulation strategies for improved mental health and quality of life outcomes for adults with asthma.
Keywords: Asthma, Psychological flexibility, Cognitive emotion regulation, Mental health, Psychological distress, Quality of life
Introduction
Asthma is a multi-factorial chronic respiratory illness, characterized by wheezing, coughing, shortness of breath and chest tightness (World Health Organization, 2023; Global Initiative for Asthma, 2023). The World Health Organization (2023) estimates that there were 383,000 casualties of asthma caused in 2015 around the globe. By 2025, the number of patients suffering from asthma is likely to increase up to 400 million (Global Initiative for Asthma, 2023). Pakistan is the 6th most populated country and more than twenty million individuals are facing asthmatic difficulties (Chiesi Respiratory Diseases Center, 2016).
People suffering from any chronic illness like diabetes, chronic pain, multiple sclerosis osteoporoses, and asthma etc., reported a high level of psychological distress (Mort & Philip, 2014) and lower quality of life (Trost et al., 2015; Preis et al., 2018). Several researches indicated that almost in all three stages of asthma: onset, progression, and exacerbation (Edwards et al., 2017), people suffering from asthma had reported a low level of happiness, well-being, more psychological distress (anxiety, depression, & stress), and poorer quality of life in contrast to healthy controls (Brumpton et al., 2013; Ampon et al., 2005) and were at more risk of having asthma-related emergency room visits (Ahmedani et al., 2013). In a study conducted by Pickles et al. (2018), asthma was found to be correlated with poor quality of life, exhaustion, restrictions in doing daily life activities effectively, adverse impacts on well-being, as well as with reduced productivity. Findings of studies conducted in Pakistan indicated that 15% of the asthmatic patients experienced depressive symptoms (Motiani, Haidri & Rizvi, 2011) especially, the women suffering from asthma (Malik et al., 2017b). Studies further showed that emotional problems related to physical illness could be considered a serious threat to a patient’s quality of life (Saleem, Mahmood & Naeem, 2016). In Pakistan adults with asthma experience poor health-related quality of life but with the help of better medical facilities it can be improved (Malik et al., 2017a).
Certain factors could be associated with psychopathology and poorer quality of life including perception or acceptance of illness such as personality dispositions (Monique Van De Ven & Engels, 2011), psychological flexibility (Guerrini Usubini et al., 2021; Bergman & Keitel, 2020), and coping strategies (Li et al., 2015; Kristofferzon, Engström & Nilsson, 2018). Psychological flexibility is the most important variable of acceptance and commitment therapy (ACT) and emerged as a significant determinant of emotional well-being and behavioral value (Bond, Lloyd & Guenole, 2013). Psychological flexibility as an ability to build up a strong contact with the present moment in the presence of emotionally interfering thoughts (Hayes et al., 2006; Moran, 2015), has been significantly related to greater well-being (Dawson & Golijani-Moghaddam, 2020), a better quality of life and reduced psychological distress (Wersebe et al., 2018). Previous researches suggested that psychological flexibility proved to be a very useful intervention for a wide range of psychological disorders such as post-traumatic stress disorder, depression, anxiety, stress (Powers, Vörding & Emmelkamp, 2009), and for individuals suffering from any physical chronic illness (Prevedini et al., 2011). Psychological flexibility is significantly associated with higher well-being among people with obesity and enables them to make interventions for healthy living (Guerrini Usubini et al., 2021). Karimzadeh & Latifi (2015) identified psychological flexibility as a strong predictor of improved quality of life and reduced negative emotional consequences of asthma.
Psychological flexibility also cope with stress resulting from chronic illness and enhanced resilience against chronic disease (Gentili et al., 2019; Vowles et al., 2014) might be helpful in the selection of adaptive coping strategies and related behaviors. Adaptive cognitive emotion regulation strategies like acceptance, putting into perspective, refocus on planning, positive refocusing, positive reappraisal (as cited in Garnefski, Kraaij & Spinhoven (2001)) and psychological flexibility had a positive impact on the quality of life of the people suffering from any chronic illness and enable people to cope effectively with their disease (Li et al., 2015; Momeniarbat et al., 2017). In contrast to psychological flexibility, inflexibility is particularly known as experiential avoidance (tendency to escape from challenging experiences, thoughts, feelings, and situations (Hayes et al., 2006) has found to be related to maladaptive coping and poorer quality of life, well-being and impaired psychological/emotional outcomes such as depression, anxiety, stress (Fergus, Bardeen & Orcutt, 2013; Nielsen, Sayal & Townsend, 2018). Maladaptive cognitive emotion regulation strategies including self-blame, rumination, catastrophising, and blaming others (as cited in Garnefski, Kraaij & Spinhoven (2001)) might also act as a central part in the perception of illness and also in the quality of life of the individuals suffering from chronic physical illness such cancer (Postolica et al., 2017). Catastrophising has been reportedly linked with psychological outcomes of physical illness such as poorer quality of life (Sherwin, Leary & Henderson, 2017). In an Iranian sample of asthma patients, it was revealed that catatstrophising proved to be a strong mediator between alexithymia and physical symptoms of asthma (Ghorbani et al., 2017). So, it can be seen that when a person suffers from any physiological disease, it will affect his/her quality of life and develop psychological distress among them. If the psychological flexibility is high then it will play an important role in maintaining a better quality of life and decreasing emotional distress. That is why it is very important to know how to cope with disease so that the quality of life will be maintained. Literature provides that no study was found, that focused on the association between cognitive-emotional regulation strategies and psychological flexibility with psychological distress and quality of life in patients living with asthma. Thus the current research intends (a) to check the association among cognitive emotion regulation coping techniques (adaptive, maladaptive), psychological/emotional flexibility, and mental health outcomes (psychological distress & asthma-related quality of life) among individuals suffering from asthma; (b) to explore the mediating effect of psychological distress and catastrophising on the association between psychological flexibility and health-related quality of life in patients with asthma.
Method
Participants and procedure
After getting ethical approval the procedure of data collection was started. This manuscript is the sub session of MS dissertation which was approved from board of studies at the Department of Applied Psychology Government College University Faisalabad, Pakistan (reference no. Psy/206). Both men and women diagnosed with asthma since one year at least and receiving treatment at the time of research, were included. Patients with any other physiological co-morbidity (diabetes, heart failure, kidney failure etc.) and mental health problems were excluded. After seeking permission from the hospital authorities and clinics, written informed consent was obtained from patients diagnosed with asthma and their caregivers to fulfill the ethical requirement. Participants were instructed about the questionnaires and asked to complete cognitive emotion regulation questionnaire (CERQ), acceptance and action questionnaire-II (AAQ-II) depression, anxiety stress scale-21 (DASS-21), and asthma quality of life questionnaire (AQLQ). Authors have permission to use these instruments from copy right holders (permissions attached in Supplemental Files). Besides these questionnaires, a demographic information sheet was also used to record the essential demographics of the participants. At first 235 questionnaires were distributed from which 15 participants refused to participate in research; nine did not provide essential demographic information and 11 participants did not meet the inclusion criteria. Finally, a total sample of 200 individuals (Mage = 42.32, SDage = 16.99) above 18 years, both men (n = 63; Mage = 48.84, SDage = 18.97) and women (n = 137; Mage = 39.32, SDage = 15.16) diagnosed with asthma since one year at least and receiving treatment at the time of research, were drawn from pulmonology unit of different public/private sector hospitals and clinics of Faisalabad (Pakistan). Purposive sampling technique and correlational research design were followed. It was made sure that all information was kept confidential and used only for research purposes.
Instruments
Cognitive emotional regulation questionnaire (CERQ; Garnefski, Kraaij & Spinhoven, 2002). CERQ is a multi-dimensional self-report instrument containing 36 items, measures nine adaptive and maladaptive cognitive emotion regulation coping strategies on five points Likert scale. Five subscales measure adaptive strategies (acceptance, putting into perspective, positive refocusing, refocus on planning, & positive reappraisal) while, four subscales (catastrophising, rumination, self-blame & other blame) are categorized as maladaptive cognitive emotion regulation strategies. Each subscale has four items. Researches on cognitive emotion regulation questionnaire confirmed that each subscale showed good reliability coefficient (0.68 to 0.86); (Garnefski, Kraaij & Spinhoven, 2002). In current study Urdu version of CERQ (Butt et al., 2016) was used with adequate Chronbach alpha reliability (α = 0.71).
Acceptance and action questionnaire (AAQ-II; Bond et al., 2011). Acceptance and action questionnaire (AAQ) is a measure of psychological flexibility/experiential avoidance. It is seven points Likert scale high scores indicate higher levels of psychological inflexibility or experiential avoidance, while low scores indicate psychological flexibility (Bond et al., 2011). It has been widely used in health-related psychological studies and showed good psychometric properties (Bond et al., 2011; Zhang et al., 2014; Paladines-Costa et al., 2021). For present study Urdu Version of AAQ-II consist of seven items (Khawar & Aslam, 2018) was used.
Depression anxiety stress scale (DASS–21; Lovibond & Lovibond, 1995). Depression anxiety stress scale was developed to measure the adverse impacts of three negative emotions including depression, anxiety and stress (Lovibond & Lovibond, 1995). The measure originally consists of 42 items on four point Likert scale. Its short-form called DASS-21 consists of 21 items; seven items for each subscale (Lovibond & Lovibond, 1995) having sound psychometric properties (Pezirkianidis et al., 2018; Coker, Coker & Sanni, 2018; Bibi et al., 2020). In current research, Urdu version of DASS-21 was used (Farooqi & Habib, 2010).
Asthma quality of life questionnaire (AQLQ; Juniper et al., 1992). Asthma quality of life questionnaire was used to assess the practical issues (psychological/emotional, physical, social and everyday work-related) experienced by the patients of asthma. There are 32 questions in AQLQ divided into four subscales including symptoms of asthma, limitations in daily life activities, emotional functions and environmental stimuli. The instrument provides an overall score for means of all items and mean scores for each domain (Bateman et al., 2015). Participants are instructed to complete this scale about how they have been experienced the last 14 days and to answer each of the 32 items on a seven point scale (7 = not impaired at all to 1 = severely impaired). It has excellent test-retest reliability (r = 0.95) (Juniper et al., 1992). For current research translated Urdu version of AQLQ with.87 Chronbach alpha reliability, was used.
Demographic information sheet. Demographic information (age, gender, education, number of family size, family system, monthly income, and duration of illness) of the adults with asthma was also obtained.
Results
The data were analyzed through the IBM statistical package for social sciences version 22 (SPSS, Inc., Chicago, IL, USA). The data were interpreted in the form of two sections, section I is labeled as “Descriptive Statistics” containing all the demographic information of the sample; while section II is named as “Inferential Statistics” consisting of correlation analysis, mediation, etc. A significance level of 0.05 was used for analysis.
Table 1 showed the demographic information of the sample such as; age, area of residence, marital status, education, duration of illness etc.
Table 1. Demographic characteristics of study sample (N = 200).
| Gender | ||||
|---|---|---|---|---|
| Variables | Groups | Men | Women | Total |
| f (%) | f (%) | f (%) | ||
| Age | 18–35 years | 19 (9.5) | 71 (35.5) | 90 (45) |
| 36–55 years | 16 (8.0) | 42 (21.0) | 58 (29) | |
| 56–80 years | 28 (14.0) | 24 (12.0) | 52 (26) | |
| Total | 63 (31.5) | 137 (68.5) | 200 (100) | |
| Marital status | Single | 6 (3.0) | 13 (6.5) | 19 (9.5) |
| Married | 48 (24.0) | 101 (50.5) | 149 (74.5) | |
| Separated | 3 (1.5) | 7 (3.5) | 10 (5.0) | |
| Widowed/Widower | 6 (3.0) | 16 (8.0) | 22 (11.0) | |
| Total | 63 (31.5) | 137 (68.5) | 200 (100) | |
| Area of residence | Rural | 24 (12.0) | 63 (30.0) | 84 (42) |
| Urban | 39 (19.5) | 77 (38.5) | 116 (58) | |
| Total | 63 (31.5) | 137 (68.5) | 200 (100) | |
| Family type | Nuclear | 38 (19.0) | 98 (49.0) | 136 (68) |
| Joint/Extended | 25 (12.5) | 39 (19.5) | 64 (32) | |
| Total | 63 (31.5) | 137 (68.5) | 200 (100) | |
| Monthly income | 10,000–50,000 | 50 (25.0) | 116 (58.0) | 116 (83) |
| 51,000–100,000 | 12 (6.0) | 18 (9.0) | 30 (15) | |
| 101,000–150,000 | 1 (0.5) | 3 (1.5) | 4 (2) | |
| Total | 63 (31.5) | 137 (68.5) | 200 (100) | |
| Education | Illiterate | 2 (1.0) | 20 (10) | 22 (11) |
| Middle and below | 30 (15.0) | 53 (26.5) | 83 (41.5) | |
| Secondary/Higher Secondary | 19 (9.5) | 40 (20) | 59 (29.5) | |
| Graduation and above | 12 (6.0) | 24 (12.0) | 36 (18.0) | |
| Total | 63 (31.5) | 137 (68.5) | 200 (100) | |
| Duration of illness | 1–5 years | 39 (19.5) | 91 (45.5) | 139 (65) |
| 6–10 years | 14 (7.0) | 30 (15.0) | 44 (22) | |
| 11–15 years | 10 (5.0) | 16 (8.0) | 26 (13) | |
| Total | 63 (31.5) | 137 (68.5) | 200 (100) | |
Table 2 shows the descriptive statistics and reliability coefficients for all the study measures and their subscales. Data are normally distributed as per criteria for social sciences (skewness & kurtosis ± 2) defined by Gravetter & Wallnau (2014), and that is suitable for parametricstatistics.
Table 2. Descriptives statistics and alpha level of all the study measures and their subscales.
| Variables | M | SD | Skewness | Kurtosis | α |
|---|---|---|---|---|---|
| AAQ-II | 22.60 | 6.97 | 0.68 | 0.12 | 0.89 |
| CERQ | 0.71 | ||||
| Positive refocusing | 11.41 | 3.42 | 0.52 | −0.48 | 0.80 |
| Acceptance | 12.68 | 2.53 | −0.11 | −0.33 | 0.68 |
| Positive reappraisal | 11.25 | 3.09 | 0.66 | −0.23 | 0.76 |
| Refocus on planning | 13.63 | 2.65 | 0.12 | −0.07 | 0.73 |
| Putting into perspective | 12.91 | 2.08 | −0.08 | 1.15 | 0.45 |
| Self–blame | 11.68 | 2.35 | −0.29 | −0.27 | 0.57 |
| Rumination | 13.09 | 1.95 | −0.81 | 1.67 | 0.49 |
| Catastrophising | 14.18 | 3.24 | −0.27 | −0.35 | 0.81 |
| Other blame | 11.46 | 2.41 | −0.12 | 0.92 | 0.69 |
| DASS-21 total | 68.66 | 14.63 | 0.12 | 0.00 | 0.82 |
| Depression | 22.05 | 6.63 | −0.21 | 0.12 | |
| Anxiety | 22.85 | 6.02 | 0.14 | −0.11 | |
| Stress | 23.76 | 4.84 | 0.23 | 0.60 | |
| AQLQ total | 3.07 | 0.52 | −0.70 | 0.34 | 0.87 |
| Activity limitations | 3.53 | 0.68 | −0.35 | −0.16 | |
| Symptoms | 3.22 | 0.61 | −0.71 | 0.89 | |
| Emotional function | 2.76 | 0.73 | 0.17 | 0.24 | |
| Environmental stimuli | 3.41 | 0.73 | 0.08 | 0.59 |
Table 3 showed the results of Pearson Product Moment correlation between all the study variables. Both adaptive and maladaptive cognitive emotion regulation coping techniques were significantly correlated with psychological flexibility, psychological distress and domains of asthma related quality of life (p < 0.001, p < 0.01, p < 0.05). All adaptive cognitive emotion regulation strategies except acceptance and putting into perspective were positively correlated with psychological flexibility and quality of life; while all maladaptive strategies and two adaptive strategies (putting into perspective & acceptance) had a significant negative association with psychological flexibility and quality of life.
Table 3. Inter-correlation among psychological flexibility, adaptive and maladaptive cognitive emotion regulation strategies, psychological distress and quality of life (N = 200).
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Psychological flexibility | 1 | |||||||||||||||||
| 2. Acceptance | −0.44*** | 1 | ||||||||||||||||
| 3. Positive refocusing | 0.44*** | −0.54*** | 1 | |||||||||||||||
| 4. Refocus on planning | 0.20** | −0.32*** | 0.69*** | 1 | ||||||||||||||
| 5. Positive reappraisal | 0.41*** | −0.44*** | 0.82*** | 0.68*** | 1 | |||||||||||||
| 6. Putting into perspective | −0.28*** | 0.16* | 0.048 | 0.15* | 0.12 | 1 | ||||||||||||
| 7. Self-blame | −0.47*** | 0.51*** | −0.42*** | −0.18* | −0.38*** | 0.25*** | 1 | |||||||||||
| 8. Rumination | −0.50*** | 0.31*** | −0.12 | 0.15* | −0.15* | 0.30*** | 0.44*** | 1 | ||||||||||
| 9. Catastrophising | −0.59*** | 0.63*** | −0.64*** | −0.35*** | −0.56*** | 0.28*** | 0.60*** | 0.49*** | 1 | |||||||||
| 10. Other blame | −0.46*** | 0.42*** | −0.42*** | −0.34*** | −0.37*** | 0.27*** | 0.45*** | 0.34*** | 0.58*** | 1 | ||||||||
| 11. Activity limitations AQLQ | 0.17* | −0.19** | 0.35*** | 0.27*** | 0.34*** | −0.06 | −0.21 | −0.10 | −0.32*** | −0.30*** | 1 | |||||||
| 12. Symptoms AQLQ | 0.24** | −0.29*** | 0.36*** | 0.33*** | 0.33*** | −0.22** | −0.22 | −0.12 | −0.40*** | −0.30*** | 0.71*** | 1 | ||||||
| 13. Emotional function AQLQ | 0.19** | −0.25*** | 0.40*** | 0.36*** | 0.33*** | −0.13 | −0.24 | −0.07 | −0.36*** | −0.32*** | 0.61*** | 0.75*** | 1 | |||||
| 14. Environmental stimuli AQLQ | 0.08 | −0.10 | 0.04 | 0.11 | 0.02 | −0.02 | −0.09 | −0.02 | −0.03 | −0.22** | −0.10 | 0.10 | 0.11 | 1 | ||||
| 15. AQLQ total | 0.23** | −0.28*** | 0.40*** | 0.35*** | 0.36*** | −0.17* | −0.25*** | −0.11 | −0.40*** | −0.36*** | 0.17* | 0.24** | 0.19** | 0.08 | 1 | |||
| 16. Depression | −0.49*** | 0.57*** | −0.55*** | −0.39*** | −0.51*** | 0.15* | 0.54*** | 0.30*** | 0.60*** | 0.49*** | −0.30*** | −0.40*** | −0.38*** | −0.11 | −0.49*** | 1 | ||
| 17. Anxiety | −0.34*** | 0.43*** | −0.51*** | −0.44*** | −0.47*** | 0.11 | 0.36*** | 0.12 | 0.52*** | 0.34*** | −0.44*** | −0.49*** | −0.43*** | −0.01 | −0.35*** | 0.65*** | 1 | |
| 18. Stress | −0.48*** | 0.32*** | −0.41*** | −0.28*** | −0.40*** | 0.22** | 0.47*** | 0.31*** | 0.52*** | 0.46*** | −0.25*** | −0.31*** | −0.29*** | −0.12 | −0.48*** | 0.55*** | 0.39** | 1 |
Notes:
p < 0.001.
p < 0.01.
p < 0.05.
AQLQ, Asthma related quality of life questionnaire.
Figure 1 showed the serial mediation analysis to identify the effect of psychological flexibility on quality of life through catastrophising and anxiety; while gender and duration of diagnosis of illness were taken as covariates and none of them were found to be significant. Serial mediation analysis (Model 6) was performed by estimating 5,000 bootstrap sample through PROCESS MACRO (Hayes, 2022). Findings indicated that total effect of psychological flexibility on quality of life was significant (b = 0.017, p < 0.01; 95% CI [0.007–0.027]) while direct effect was non-significant (b = –0.003, 95% CI [−0.014-0.008]). On the other hand, indirect effect by assuming 95% CI were as follows: psychological flexibility catastrophising quality of life (b = 0.124, 95% CI [0.022–0.232]), psychological flexibility anxiety quality of life (b = 0.023, 95% CI [−0.039-0.087]), psychological flexibility catastrophising anxiety quality of life (b = 0.120, 95% CI [0.068–0.184]) (see Table S1). Total indirect effect of psychological flexibility on quality of life was 28%. The overall findings indicated that catastrophising and anxiety serially, fully mediated the relationship between psychological flexibility and quality of life. Findings showed that an increase in psychological flexibility predicted the low level of catastrophising while by increasing catastrophising an increase in anxiety was shown. Moreover, an increase in anxiety predicted a decrease in quality of life among patients with asthma.
Figure 1. Mediating effect of catastrophising and anxiety on the association among psychological flexibility and quality of life.
Table S1 showed the total, direct and indirect effects of psychological flexibility on quality of life.
Discussion
Although the current study has provided significant contributions to the field of health psychology, but the following limitations were observed: in the present research, the sample was obtained from few hospitals of Faisalabad. In future the data would be collected from different cities in exchange for generalizability. There is no control group in this study that is a major limitation. A control group would yield the more degree of evidence for results. The sample size was restricted due to the shortage of time and reduces the chances of generalization of current research. Some participants showed hesitation in giving their personal information. A qualitative analysis should be incorporated due to the subjectivity of many factors involved. The findings of current research would be implicated in health psychology and counseling for patients with asthma.
The findings of current study showed that psychologically flexibility is significantly correlated with lower levels of psychological distress (including depression, anxiety and stress on DASS 21) and health-related quality of life (activity limitation, physical symptoms and emotional function on AQLQ). This association was however stronger for depression and quality of life based on physical symptoms. Previous studies illustrated that psychological flexibility has been constantly related to lower psychological distress and better emotional or psychological well-being among individuals suffering from chronic illness (Tyndall et al., 2020; Wersebe et al., 2018). Psychological flexibility could also be helpful in better disease management and leads toward a better quality of life among patients suffering from chronic respiratory disease in Hong Kong (Cheung & Mak, 2016). The underline mechanism of this positive association was further explored in terms of cognitive emotion regulation strategies.
Positive link between psychological flexibility, adaptive cognitive emotion regulation strategies, lower level of distress and higher quality of life found in present study. Findings showed that psychological flexibility and adaptive cognitive emotion regulation strategies are significantly positively correlated with each other and psychological flexibility serves as a buffer against psychological distress. Literature proved that psychological flexibility could reduce the negative effects of current life stressors on mental health and well-being (Gloster, Meyer & Lieb, 2017; Fonseca et al., 2020). Current study indicated that maladaptive cognitive emotion regulation coping techniques and psychological flexibility were inversely correlated with each other. AAQ-II in terms of high scores is considered as an instrument for measuring experiential avoidance (Bond et al., 2011). In our study experiential avoidance/inflexibility had been particularly linked with catastrophising and rumination. Both of these cognitive emotion regulation strategies are not only considered maladaptive coping (Garnefski & Kraaij, 2018) but also have a significant role in general cognitive distortions (Mahaffey et al., 2013). Rueda & Valls (2020) revealed that psychological flexibility had an indirect impact on distress and well-being mediated through avoidant coping techniques which indicated that by using avoidant/maladaptive coping strategies the effect of psychological flexibility turns into inflexibility and had adverse impacts on quality of life.
Cognitive emotion regulation strategies have been significantly linked with psychological problems such as depression, anxiety, stress (Garnefski & Kraaij, 2006, 2007; Gross & Jazaieri, 2014; Liu & Thompson, 2017) and quality of life (Li et al., 2015, Kanwa & Iftikhar, 2019). Our results indicated that adaptive cognitive emotion regulation strategies especially positive refocusing, refocus on planning, and positive reappraisal were significantly negatively associated with psychological distress (depression, anxiety, stress) and positively linked with asthma related quality of life. Current research also highlighted the significant positive correlation between maladaptive cognitive emotion regulation coping (rumination, catastrophising, self-blame, & other blame) and psychological distress. Literature provides significant verdicts for these findings that more use of adaptive strategies such as positive reappraisal, refocus on planning and positive refocusing was negatively associated with anxiety and depression (Min et al., 2013; Barberis et al., 2017) while positively linked with better quality of life (Li et al., 2015) among patients with chronic illness. Rumination and self-blaming were found to be directly associated with depression; catastrophising and other-blame were exclusively related to more anxious signs and symptoms (Garnefski & Kraaij, 2018). Literature proved that the person who uses maladaptive cognitive coping experienced more psychological problems like depression, anxiety, stress; and poor emotional well-being (Bahrami et al., 2017; Garnefski, Hossain & Kraaij, 2017). In a study conducted in Serbian breast cancer patients’ support our findings that catastrophising and rumination are significant maladaptive cognitive coping strategies which would be helpful in changing the intensity of psychological distress and reflected in person’s health related quality of life (Kovač et al., 2020).
Further, it was revealed that an increase in acceptance was highly significantly linked with an increase in depression, anxiety, stress and poorer quality of life, which is consistent with previous literature (Domaradzka & Fajkowska, 2018; Dubey, Podder & Pandey, 2020; Manju, 2017). Although acceptance is an adaptive strategy, few studies suggested that acceptance should be treated as maladaptive (Martin & Dahlen, 2005, Tuna & Bozo, 2012). As in acceptance subscale, some items (“I think I cannot change anything”, “I must learn to live with this situation”, etc.) appeared as maladaptive and may provide a sense of hopelessness or helplessness for current research. Moreover, our results also showed that increased use of putting into perspective as an adaptive coping strategy was significantly related to high level of depression and stress and poor quality of life. Previous research also showed negative relationship between this strategy and quality of life (Li et al., 2015). It may cause due to an uncertain situation of disease as when individuals suffer from chronic illness it was very difficult for them to focus on thinking and planning positive events or situations in their lives and it becomes more stressful. Hence, it was revealed by our findings that the more one fails to put less emphasis on stressful things or situations and tries to accept his/her physical illness, the more it will be depressing, stressful and helpless for him/her; the more one tries to focus on positive and pleasant things in life, engaging in thinking positive aspects of the situation instead of the negative situation, and making plans about deciding what steps should be taken to overcome the stress, the more sense of worth he/she will develop.
Results of serial mediation analysis using PROCESS MACRO (Hayes, 2022) revealed catastrophising (maladaptive cognitive emotion regulation strategy) and anxiety mediated the link between psychological flexibility and quality of life. When we introduce catastrophising as mediator the effect of psychological flexibility on quality of life was diminished because the higher catastrophising lowers the impact of psychological flexibility/higher experiential avoidance and leads towards the poorer quality of life. Psychological flexibility as a personality trait has shown greater openness in accepting life stressors and carrying valued living. In this way, psychological flexibility is positively associated with greater individual well-being and quality of life (Berghoff et al., 2014; Ramaci et al., 2019). Psychological flexibility also minimized emotional distress and enhanced better psychological health of patients with asthma (Karimzadeh & Latifi, 2015). It was found in previous researches that coping and psychological distress (anxiety) was significantly mediated between personality traits and health-related quality of life (Pereira-Morales et al., 2018). Literature supports our findings that quality of life among patients suffering from asthma was mediated through cognitive coping techniques (Van Lieshout & MacQueen, 2012). Previous researches provide strong verdicts that among cognitive emotion regulation strategies just catastrophising, plays a mediating role among alexithymia subscales and physical symptoms among asthmatics patients, in this way catastrophizing intensifies the asthmatic symptoms and leads toward greater psychological distress and poorer quality of life (Rieffe et al., 2010). In another study, it was found that catastrophising and psychological distress significantly mediated the link between pain-related fear and quality of life among people with chronic low back pain (Marshall, Schabrun & Knox, 2017). Catastrophising is directly related to psychological distress and in this way more emotional issues are related to this coping style.
Conclusion
The present study provides one of the first looks at the role of different cognitive emotion regulation strategies (adaptive, maladaptive) and gives an insight into the frequency of these strategies, psychological flexibility, and their impacts on quality of life. This study will prove to be a significant addition in literature not only for health psychology as well as for better asthma management in medical sciences and provide strong foundations for further researches regarding this issue.
Supplemental Information
Acknowledgments
We acknowledge all the participants who took part in research.
Funding Statement
The authors received no funding for this work.
Additional Information and Declarations
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Samavia Hussain conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, and approved the final draft.
Rabia Khawar conceived and designed the experiments, performed the experiments, analyzed the data, authored or reviewed drafts of the article, and approved the final draft.
Rizwana Amin performed the experiments, analyzed the data, authored or reviewed drafts of the article, and approved the final draft.
Asma Hamdani conceived and designed the experiments, prepared figures and/or tables, and approved the final draft.
Asma Majeed performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the article, and approved the final draft.
Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
Institutional Review Board Government College University Faisalabad. The Board of Studies Department of Applied Psychology, Government College University Faisalabad Pakistan approved the study (Reference No. Psy/206).
Data Availability
The following information was supplied regarding data availability:
Raw data is available in the Supplemental Files.
This file contain raw data of all variables included in study.
References
- Ahmedani et al. (2013).Ahmedani BK, Peterson EL, Wells KE, Williams LK. Examining the relationship between depression and asthma exacerbations in a prospective follow-up study. Psychosomatic Medicine. 2013;75(3):305–310. doi: 10.1097/PSY.0b013e3182864ee3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ampon et al. (2005).Ampon RD, Williamson M, Correll PK, Marks GB. Impact of asthma on self-reported health status and quality of life: a population based study of Australians aged 18-64. Thorax. 2005;60(9):735–739. doi: 10.1136/thx.2005.040311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahrami et al. (2017).Bahrami B, Mashhadi A, Kareshki H, Bahrami A. Role of mediating cognitive Emotion regulation strategies and goal adjustment in relationship between personality characteristics and quality of life of patients with cancer. International Journal of Cancer Management. 2017;10(12):1447. doi: 10.5812/ijcm.9317. [DOI] [Google Scholar]
- Barberis et al. (2017).Barberis N, Cernaro V, Costa S, Montalto G, Lucisano S, Larcan R, Buemi M. The relationship between coping, emotion regulation, and quality of life of patients on dialysis. The International Journal of Psychiatry in Medicine. 2017;52(2):111–123. doi: 10.1177/0091217417720893. [DOI] [PubMed] [Google Scholar]
- Bateman et al. (2015).Bateman ED, Esser D, Chirila C, Fernandez M, Fowler A, Moroni-Zentgraf P, FitzGerald JM. Magnitude of effect of asthma treatments on asthma quality of life questionnaire and asthma control questionnaire scores: systematic review and network meta-analysis. Journal of Allergy and Clinical Immunology. 2015;136(4):914–922. doi: 10.1016/j.jaci.2015.03.023. [DOI] [PubMed] [Google Scholar]
- Berghoff et al. (2014).Berghoff CR, Forsyth JP, Ritzert TR, Sheppard SC. Comparing paths to quality of life: contributions of ACT and cognitive therapy intervention targets in two highly anxious samples. Journal of Contextual Behavioral Science. 2014;3(2):89–97. doi: 10.1016/j.jcbs.2014.04.001. [DOI] [Google Scholar]
- Bergman & Keitel (2020).Bergman M, Keitel MA. Navigating Life Transitions for Meaning. Cambridge: Academic Press; 2020. At the heart of meaning-making: an acceptance and commitment approach to developing adaptive meaning following acute cardiac events; pp. 145–164. [Google Scholar]
- Bibi et al. (2020).Bibi A, Lin M, Zhang XC, Margraf J. Psychometric properties and measurement invariance of depression, anxiety and stress scales (DASS-21) across cultures. International Journal of Psychology. 2020;55(6):916–925. doi: 10.1002/ijop.12671. [DOI] [PubMed] [Google Scholar]
- Bond et al. (2011).Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Waltz T, Zettle RD. Preliminary psychometric properties of the acceptance and action questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy. 2011;42(4):676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Bond, Lloyd & Guenole (2013).Bond FW, Lloyd J, Guenole N. The work-related acceptance and action questionnaire: initial psychometric findings and their implications for measuring psychological flexibility in specific contexts. Journal of Occupational and Organizational Psychology. 2013;86(3):331–347. doi: 10.1111/joop.12001. [DOI] [Google Scholar]
- Brumpton et al. (2013).Brumpton BM, Leivseth L, Romundstad PR, Langhammer A, Chen Y, Camargo CA, Jr, Mai XM. The joint association of anxiety, depression and obesity with incident asthma in adults: the HUNT study. International Journal of Epidemiology. 2013;42(5):1455–1463. doi: 10.1093/ije/dyt151. [DOI] [PubMed] [Google Scholar]
- Butt et al. (2016).Butt M, Khawar R, Saeed S, Malik F, Islam S. Psychometric evaluation of cognitive emotional regulation questionnaire Urdu version (CERQ-U). Paper Presented in International Conference on Current trends in Psychology. 31st March, 2016; Multan, Pakistan: Department of Applied Psychology, Bahauddin Zakariya University; 2016. [Google Scholar]
- Cheung & Mak (2016).Cheung KW, Mak YW. Association between psychological flexibility and health beliefs in the uptake of influenza vaccination among people with chronic respiratory diseases in Hong Kong. International Journal of Environmental Research and Public Health. 2016;13(2):155. doi: 10.3390/ijerph13020155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesi Respiratory Diseases Center (2016).Chiesi Respiratory Diseases Center Prevalence of asthma in Pakistan. 2016. http://www.chiesipakistan.com http://www.chiesipakistan.com
- Coker, Coker & Sanni (2018).Coker AO, Coker OO, Sanni D. Psychometric properties of the 21-item depression anxiety stress scale (DASS-21) African Research Review. 2018;12(2):135–142. doi: 10.4314/afrrev.v12i2.13. [DOI] [Google Scholar]
- Dawson & Golijani-Moghaddam (2020).Dawson DL, Golijani-Moghaddam N. COVID-19: psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science. 2020;17(3):126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domaradzka & Fajkowska (2018).Domaradzka E, Fajkowska M. Cognitive emotion regulation strategies in anxiety and depression understood as types of personality. Frontiers in Psychology. 2018;9:856. doi: 10.3389/fpsyg.2018.00856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubey, Podder & Pandey (2020).Dubey N, Podder P, Pandey D. Knowledge of COVID-19 and its influence on mindfulness, cognitive emotion regulation and psychological flexibility in the Indian community. Frontiers in Psychology. 2020;11:589365. doi: 10.3389/fpsyg.2020.589365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards et al. (2017).Edwards MR, Saglani S, Schwarze J, Skevaki C, Smith JA, Ainsworth B, Almond M, Andreakos E, Belvisi MG, Chung KF, Cookson W, Cullinan P, Hawrylowicz C, Lommatzsch M, Jackson D, Lutter R, Marsland B, Moffatt M, Thomas M, Virchow JC, Xanthou G, Edwards J, Walker S, Johnston SL. Addressing unmet needs in understanding asthma mechanisms: from the European asthma research and innovation partnership (EARIP) work package (WP) 2 collaborators. European Respiratory Journal. 2017;49(5):1602448. doi: 10.1183/13993003.02448-2016. [DOI] [PubMed] [Google Scholar]
- Farooqi & Habib (2010).Farooqi Y, Habib M. Gender differences in anxiety, depression and stress among survivors of suicide bombing. Pakistan Journal of Social and Clinical Psychology. 2010;8(2):145–153. [Google Scholar]
- Fergus, Bardeen & Orcutt (2013).Fergus TA, Bardeen JR, Orcutt HK. Experiential avoidance and negative emotional experiences: the moderating role of expectancies about emotion regulation strategies. Cognitive Therapy and Research. 2013;37(2):352–362. doi: 10.1007/s10608-012-9469-0. [DOI] [Google Scholar]
- Fonseca et al. (2020).Fonseca S, Trindade IA, Mendes AL, Ferreira C. The buffer role of psychological flexibility against the impact of major life events on depression symptoms. Clinical Psychologist. 2020;24(1):82–90. doi: 10.1111/cp.12194. [DOI] [Google Scholar]
- Garnefski, Hossain & Kraaij (2017).Garnefski N, Hossain S, Kraaij V. Relationships between maladaptive cognitive emotion regulation strategies and psychopathology in adolescents from Bangladesh. Archives of Depression and Anxiety. 2017;3(2):23–29. doi: 10.17352/2455-5460.000019. [DOI] [Google Scholar]
- Garnefski & Kraaij (2006).Garnefski N, Kraaij V. Relationships between cognitive emotion regulation strategies and depressive symptoms: a comparative study of five specific samples. Personality and Individual Differences. 2006;40(8):1659–1669. doi: 10.1016/j.paid.2005.12.009. [DOI] [Google Scholar]
- Garnefski & Kraaij (2007).Garnefski N, Kraaij V. The cognitive emotion regulation questionnaire: psychometric features and prospective relationships with depression and anxiety in adults. European Journal of Psychological Assessment. 2007;23(3):141–149. doi: 10.1027/1015-5759.23.3.141. [DOI] [Google Scholar]
- Garnefski & Kraaij (2018).Garnefski N, Kraaij V. Specificity of relations between adolescents’ cognitive emotion regulation strategies and symptoms of depression and anxiety. Cognition and Emotion. 2018;32(7):1401–1408. doi: 10.1080/02699931.2016.1232698. [DOI] [PubMed] [Google Scholar]
- Garnefski, Kraaij & Spinhoven (2001).Garnefski N, Kraaij V, Spinhoven P. Negative life events, cognitive emotion regulation and emotional problems. Personality and Individual Differences. 2001;30(8):1311–1327. doi: 10.1016/S0191-8869(00)00113-6. [DOI] [Google Scholar]
- Garnefski, Kraaij & Spinhoven (2002).Garnefski N, Kraaij V, Spinhoven P. Manual for the use of the cognitive emotion regulation questionnaire. Leiderdorp, The Netherlands: DATEC; 2002. [Google Scholar]
- Gentili et al. (2019).Gentili C, Rickardsson J, Zetterqvist V, Simons LE, Lekander M, Wicksell RK. Psychological flexibility as a resilience factor in individuals with chronic pain. Frontiers in Psychology. 2019;10:2016. doi: 10.3389/fpsyg.2019.02016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghorbani et al. (2017).Ghorbani F, Khosravani V, Ardakani RJ, Alvani A, Akbari H. The mediating effects of cognitive emotion regulation strategies on the relationship between alexithymia and physical symptoms: evidence from Iranian asthmatic patients. Psychiatry Research. 2017;247(1):144–151. doi: 10.1016/j.psychres.2016.11.015. [DOI] [PubMed] [Google Scholar]
- Global Initiative for Asthma (2023).Global Initiative for Asthma Global strategy for asthma management and prevention. 2023. https://ginasthma.org/gina-reports/ https://ginasthma.org/gina-reports/
- Gloster, Meyer & Lieb (2017).Gloster AT, Meyer AH, Lieb R. Psychological flexibility as a malleable public health target: evidence from a representative sample. Journal of Contextual Behavioral Science. 2017;6(2):166–171. doi: 10.1016/j.jcbs.2017.02.003. [DOI] [Google Scholar]
- Gravetter & Wallnau (2014).Gravetter FJ, Wallnau LB. 8th edition. USA: Wadsworth; 2014. Essentials of statistics for the behavioral sciences. [Google Scholar]
- Gross & Jazaieri (2014).Gross JJ, Jazaieri H. Emotion, emotion regulation, and psychopathology: an affective science perspective. Clinical Psychological Science. 2014;2(4):387–401. doi: 10.1177/2167702614536164. [DOI] [Google Scholar]
- Guerrini Usubini et al. (2021).Guerrini Usubini A, Varallo G, Granese V, Cattivelli R, Consoli S, Bastoni I, Volpi C, Castelnuovo G, Molinari E. The impact of psychological flexibility on psychological well-being in adults with obesity. Frontiers in Psychology. 2021;12:777. doi: 10.3389/fpsyg.2021.636933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes (2022).Hayes AF. 3rd edition. New York: Guilford Publications; 2022. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Hayes et al. (2006).Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Juniper et al. (1992).Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax. 1992;47(2):76–83. doi: 10.1136/thx.47.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanwa & Iftikhar (2019).Kanwa S, Iftikhar R. Cognitive emotion regulation, optimism and quality of life in blood cancer patients. Journal of Behavioural Sciences. 2019;29(1):13–24. [Google Scholar]
- Karimzadeh & Latifi (2015).Karimzadeh J, Latifi Z. Effectiveness of acceptance and commitment therapy (ACT) on anxiety, depression, and flexibility of patients with asthma. MAGNT Research Report. 2015;3(1):1357–1367. [Google Scholar]
- Khawar & Aslam (2018).Khawar R, Aslam Z. Addaptive/Maladaptive emotion regulation processes and psychopathological outcomes of infertility: a study of gender differences. 2018. Unpublished Disseartion. Department of Applied Psychology, Government College University, Faisalabad, Pakistan.
- Kovač et al. (2020).Kovač A, Tovilović S, Bugarski-Ignjatović V, Popović-Petrović S, Tatić M. The role of cognitive emotion regulation strategies in health related quality of life of breast cancer patients. Vojnosanitetski Pregled. 2020;77(10):1032–1040. doi: 10.2298/VSP180205178K. [DOI] [Google Scholar]
- Kristofferzon, Engström & Nilsson (2018).Kristofferzon ML, Engström M, Nilsson A. Coping mediates the relationship between sense of coherence and mental quality of life in patients with chronic illness: a cross-sectional study. Quality of Life Research. 2018;27(7):1855–1863. doi: 10.1007/s11136-018-1845-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2015).Li L, Zhu X, Yang Y, He J, Yi J, Wang Y, Zhang J. Cognitive emotion regulation: characteristics and effect on quality of life in women with breast cancer. Health and Quality of Life Outcomes. 2015;13(1):1–10. doi: 10.1186/s12955-015-0242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu & Thompson (2017).Liu DY, Thompson RJ. Selection and implementation of emotion regulation strategies in major depressive disorder: an integrative review. Clinical Psychology Review. 2017;57(2):183–194. doi: 10.1016/j.cpr.2017.07.004. [DOI] [PubMed] [Google Scholar]
- Lovibond & Lovibond (1995).Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Mahaffey et al. (2013).Mahaffey BL, Wheaton MG, Fabricant LE, Berman NC, Abramowitz JS. The contribution of experiential avoidance and social cognitions in the prediction of social anxiety. Behavioural and Cognitive Psychotherapy. 2013;41(1):52–65. doi: 10.1017/S1352465812000367. [DOI] [PubMed] [Google Scholar]
- Malik et al. (2017a).Malik M, Khan A, Hussain A, Hashmi A. Assessment of health-related quality of life among asthmatic patients: the need for structured pharmaceutical care delivery system in Pakistan. Journal of Pharmacy & Bio-Allied Sciences. 2017a;9(4):272. doi: 10.4103/JPBS.JPBS_185_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik et al. (2017b).Malik M, Khan A, Hussain A, Hashmi A. Prevalence of depression among asthmatic patients in Pakistan: challenges for integrated team care. International Journal of Pharmaceutical Research & Allied Sciences. 2017b;6(4):8–16. [Google Scholar]
- Manju (2017).Manju HK. Cognitive regulation of emotion and quality of life. Journal of Psychosocial Research. 2017;12(1):1–10. [Google Scholar]
- Marshall, Schabrun & Knox (2017).Marshall PW, Schabrun S, Knox MF. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLOS ONE. 2017;12(7):e0180788. doi: 10.1371/journal.pone.0180788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin & Dahlen (2005).Martin RC, Dahlen ER. Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Personality and Individual Differences. 2005;39(7):1249–1260. doi: 10.1016/j.paid.2005.06.004. [DOI] [Google Scholar]
- Min et al. (2013).Min JA, Yu JJ, Lee CU, Chae JH. Cognitive emotion regulation strategies contributing to resilience in patients with depression and/or anxiety disorders. Comprehensive Psychiatry. 2013;54(8):1190–1197. doi: 10.1016/j.comppsych.2013.05.008. [DOI] [PubMed] [Google Scholar]
- Momeniarbat et al. (2017).Momeniarbat F, Karimi J, Erfani N, Kiani J. The role of neuroticism and psychological flexibility in chronic fatigue and quality of life in patients with type 2 diabetes. Romanian Journal of Diabetes Nutrition and Metabolic Diseases. 2017;24(2):137–148. [Google Scholar]
- Monique Van De Ven & Engels (2011).Monique Van De Ven MO, Engels RC. Quality of life of adolescents with asthma: the role of personality, coping strategies, and symptom reporting. Journal of Psychosomatic Research. 2011;71(3):166–173. doi: 10.1016/j.jpsychores.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Moran (2015).Moran DJ. Acceptance and commitment training in the workplace. Current Opinion in Psychology. 2015;2(3):26–31. doi: 10.1016/j.copsyc.2014.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mort & Philip (2014).Mort AJ, Philip LJ. Social isolation and the perceived importance of in-person care amongst rural older adults with chronic pain: a review and emerging research Agenda. Journal of Pain Management. 2014;7(1):13–21. [Google Scholar]
- Motiani, Haidri & Rizvi (2011).Motiani B, Haidri FR, Rizvi N. Frequency of depression in chronic obstructive pulmonary disease (COPD) patients. Pakistan Journal of Medical Sciences. 2011;27(5):1112–1115. [Google Scholar]
- Nielsen, Sayal & Townsend (2018).Nielsen E, Sayal K, Townsend E. Correction: exploring the relationship between experiential avoidance, coping functions and the frequency and frequency of self-harm. PLOS ONE. 2018;13(2):e0192795. doi: 10.1371/journal.pone.0192795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paladines-Costa et al. (2021).Paladines-Costa B, López-Guerra V, Ruisoto P, Vaca-Gallegos S, Cacho R. Psychometric properties and factor structure of the Spanish version of the acceptance and action questionnaire-II (AAQ-II) in Ecuador. International Journal of Environmental Research and Public Health. 2021;18(6):2944. doi: 10.3390/ijerph18062944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira-Morales et al. (2018).Pereira-Morales AJ, Adan A, Lopez-Leon S, Forero DA. Personality traits and health-related quality of life: the mediator role of coping strategies and psychological distress. Annals of General Psychiatry. 2018;17(1):1–9. doi: 10.1186/s12991-018-0196-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pezirkianidis et al. (2018).Pezirkianidis C, Karakasidou E, Lakioti A, Stalikas A, Galanakis M. Psychometric properties of the depression, anxiety, stress scales-21 (DASS-21) in a Greek sample. Psychology. 2018;9(15):2933–2950. doi: 10.4236/psych.2018.915170. [DOI] [Google Scholar]
- Pickles et al. (2018).Pickles K, Eassey D, Reddel HK, Locock L, Kirkpatrick S, Smith L. “This illness diminishes me. What it does is like theft”: a qualitative meta-synthesis of people’s experiences of living with asthma. Health Expectations. 2018;21(1):23–40. doi: 10.1111/hex.12605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postolica et al. (2017).Postolica R, Iorga M, Petrariu FD, Azoicai D. Cognitive-behavioral coping, illness perception, and family adaptability in oncological patients with a family history of cancer. BioMed Research International. 2017;2017(1):1–11. doi: 10.1155/2017/8104397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers, Vörding & Emmelkamp (2009).Powers MB, Vörding MBZVS, Emmelkamp PM. Acceptance and commitment therapy: a meta-analytic review. Psychotherapy and Psychosomatics. 2009;78(2):73–80. doi: 10.1159/000190790. [DOI] [PubMed] [Google Scholar]
- Preis et al. (2018).Preis E, Franz K, Siegert E, Makowka A, March C, Riemekasten G, Cereda E, Norman K. The impact of malnutrition on quality of life in patients with systemic sclerosis. European Journal of Clinical Nutrition. 2018;72(4):504–510. doi: 10.1038/s41430-018-0116-z. [DOI] [PubMed] [Google Scholar]
- Prevedini et al. (2011).Prevedini AB, Presti G, Rabitti E, Miselli G, Moderato P. Acceptance and commitment therapy (ACT): the foundation of the therapeutic model and an overview of its contribution to the treatment of patients with chronic physical diseases. Giornale Italiano di Medicina del Lavoro ed Ergonomia. 2011;33(1 Suppl A):A53–A63. [PubMed] [Google Scholar]
- Ramaci et al. (2019).Ramaci T, Bellini D, Presti G, Santisi G. Psychological flexibility and mindfulness as predictors of individual outcomes in hospital health workers. Frontiers in Psychology. 2019;10:1302. doi: 10.3389/fpsyg.2019.01302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieffe et al. (2010).Rieffe C, Oosterveld P, Terwogt MM, Novin S, Nasiri H, Latifian M. Relationship between alexithymia, mood and internalizing symptoms in children and young adolescents: evidence from an Iranian sample. Personality and Individual Differences. 2010;48(4):425–430. doi: 10.1016/j.paid.2009.11.010. [DOI] [Google Scholar]
- Rueda & Valls (2020).Rueda B, Valls E. Is the effect of psychological inflexibility on symptoms and quality of life mediated by coping strategies in patients with mental disorders? International Journal of Cognitive Therapy. 2020;13(2):112–126. doi: 10.1007/s41811-020-00069-4. [DOI] [Google Scholar]
- Saleem, Mahmood & Naeem (2016).Saleem S, Mahmood Z, Naeem F. Health related quality of life in female patients with bronchial asthma and post-menopausal (osteoporosis: a comparative study) Journal of Pakistan Psychiatric Society. 2016;13(3):20–23. [Google Scholar]
- Sherwin, Leary & Henderson (2017).Sherwin LB, Leary E, Henderson WA. The association of catastrophizing with quality-of-life outcomes in patients with irritable bowel syndrome. Quality of Life Research. 2017;26(8):2161–2170. doi: 10.1007/s11136-017-1554-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trost et al. (2015).Trost Z, Agtarap S, Scott W, Driver S, Guck A, Roden-Foreman K, Reynolds M, Foreman ML, Warren AM. Perceived injustice after traumatic injury: associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabilitation Psychology. 2015;60(3):213–221. doi: 10.1037/rep0000043. [DOI] [PubMed] [Google Scholar]
- Tuna & Bozo (2012).Tuna E, Bozo Ö. The cognitive emotion regulation questionnaire: factor structure and psychometric properties of the Turkish version. Journal of Psychopathology and Behavioral Assessment. 2012;34(4):564–570. doi: 10.1007/s10862-012-9303-8. [DOI] [Google Scholar]
- Tyndall et al. (2020).Tyndall I, Waldeck D, Pancani L, Whelan R, Roche B, Pereira A. Profiles of psychological flexibility: a latent class analysis of the acceptance and commitment therapy model. Behavior Modification. 2020;44(3):365–393. doi: 10.1177/0145445518820036. [DOI] [PubMed] [Google Scholar]
- Van Lieshout & MacQueen (2012).Van Lieshout RJ, MacQueen GM. Relations between asthma and psychological distress: an old idea revisited. Allergy and the Nervous System. 2012;98:1–13. doi: 10.1159/issn.0079-6034. [DOI] [PubMed] [Google Scholar]
- Vowles et al. (2014).Vowles KE, McCracken LM, Sowden G, Ashworth J. Psychological flexibility in coping with chronic pain: further examination of the brief pain coping inventory-2. The Clinical Journal of Pain. 2014;30(4):324–330. doi: 10.1097/AJP.0b013e31829ea187. [DOI] [PubMed] [Google Scholar]
- Wersebe et al. (2018).Wersebe H, Lieb R, Meyer AH, Hofer P, Gloster AT. The link between stress, well-being, and psychological flexibility during an acceptance and commitment therapy self-help intervention. International Journal of Clinical and Health Psychology. 2018;18(1):60–68. doi: 10.1016/j.ijchp.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2023).World Health Organization Asthma. 2023. https://www.who.int/news-room/fact-sheets/detail/asthma https://www.who.int/news-room/fact-sheets/detail/asthma
- Zhang et al. (2014).Zhang CQ, Chung PK, Si G, Liu JD. Psychometric properties of the acceptance and action questionnaire-II for Chinese college students and elite Chinese athletes. Measurement and Evaluation in Counseling and Development. 2014;47(4):256–270. doi: 10.1177/0748175614538064. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The following information was supplied regarding data availability:
Raw data is available in the Supplemental Files.
This file contain raw data of all variables included in study.