Abstract
Purpose:
Innovative methods for delivering cardiac rehabilitation (CR) that provide strategies to circumvent the mounting barriers to traditional CR have the potential to widen access to a well-established secondary prevention strategy. Our study assesses the feasibility and acceptability of a novel virtual world-based CR (VWCR) program, Destination Rehab, as an extension of a conventional center-based CR program.
Methods:
Adult cardiac patients hospitalized at Mayo Clinic hospitals with a diagnosis for CR and ≥1 modifiable, lifestyle risk factor target—sedentary lifestyle (<3 hr physical activity/wk), unhealthy diet (<5 servings fruits and vegetables/d), or current smoking (>1 yr)—were recruited. Patients participated in an 8-wk health education program using a virtual world (VW) platform from a prior proof-of-concept study and a post-intervention focus group. Primary outcome measures included feasibility and acceptability. Secondary outcome measures included changes from baseline to post-intervention in cardiovascular (CV) health behaviors and biometrics, CV health knowledge, and psychosocial factors.
Results:
Of the 30 enrolled patients (age 59.1 ± 9.7 yr; 50% women), 93% attended ≥1 session and 71% attended ≥75% of sessions. The overall VWCR experience received an 8 rating (scale 0-10) and had high acceptability. Clinically relevant trends were noted in CV health behaviors and biometrics, although not statistically significant.
Conclusions:
The VWCR program is a feasible, highly acceptable, and innovative platform to potentially influence health behaviors and CV risk and may increase accessibility to disadvantaged populations with higher CV disease burdens.
Keywords: cardiac rehabilitation, home-based programs, lifestyle, virtual environments
Cardiac rehabilitation (CR) is an evidence-based secondary prevention program incorporating education, health behavior modification, and cardiovascular disease (CVD) risk factor control, as well as exercise assessment and training, to improve outcomes in patients with CVD.1 As such, CR is a class 1 recommendation by the American College of Cardiology/American Heart Association guidelines to improve health-related quality of life and reduce the risk of future hospitalizations and major cardiac events.2–7 Despite this, CR participation remains suboptimal, especially for racial and ethnic minority groups, women and individuals from underserved populations.1,2,8–16
Barriers to CR participation have been described in prior research and include modifiable patient and systemic factors such as inflexible hours, transportation limitations, travel costs, and lack of insurance coverage for CR costs.12,13,17–20 Studies have shown that patients often prefer CR programs that occur at home or in non-clinical settings with more flexible hours, circumventing many of these barriers.19,21,22 To improve CR adherence and effectiveness, the American Heart Association Presidential Advisory Board issued a call for innovative reengineering of the center-based CR (CBCR) model.23 Novel health care delivery methods, focused on mitigating barriers to care, are ever more relevant in the wake of the global COVID-19 pandemic, especially for medically underserved populations.24–29
Over the past 20 yr, home-based CR (HBCR) programs have emerged to alleviate some of the barriers to CR participation and have shown similar effectiveness as CBCR programs.1,30–36 While HBCR programs do mitigate various factors hindering CR participation, current evidence suggests that adherence to HBCR is only slightly better than CBCR.1,30,32 Home-based CR programs inherently lack some critical aspects of face-to-face interventions, which uniquely capitalize on behavioral counseling, cognitive restructuring, accountability, and social support to impact behavioral change, which may account for the limited adherence to HBCR despite increased accessibility.19,37–39 Although not yet validated, utilizing technology tools such as mobile and Internet-based interventions as an adjunct to HBCR is a promising approach to expand its uptake and adherence.1,19,36,40–42
Virtual worlds (VWs) are three-dimensional, immersive computer-based environments that allow patients to interact via online personas, simulate in-person experiences, and engage with a social network.38,43,44 Technology for VW emerged in recent years and has been utilized for a variety of applications including socialization, creativity, education, and more recently, health education and chronic disease management.38,44 A VW provides a space for users to test the potential impact of various health-related behaviors through avatars.43,45 We proposed expanding VW to CR, to widen access to and participation in CR, while narrowing the gap in health outcomes among underserved groups.43
This study aimed to assess the feasibility of delivery and acceptability of a VW-based CR (VWCR) program (Destination Rehab), a program designed to address the education, health behavior modification, and CVD risk factor control components of CR, as an extension of traditional CBCR across multiple clinical sites. We assessed the impact of Destination Rehab on CVD health behaviors (physical activity [PA] and diet) and biometrics (body mass index [BMI], blood pressure [BP], lipids, and hemoglobin A1c), cardiovascular (CV) health knowledge, and psychosocial factors (social support, quality of life, and optimism).
METHODS
CONTEXT AND STUDY DESIGN
The VW-based platform Second Life was utilized to design a VWCR program named Destination Rehab based on principles of self-determination theory.46,47 A prior proof-of-concept study evaluated patient acceptability of the CR program.46 Feedback from this intervention was used to design the refined program used in the current study.
A single-group, nonrandomized, mixed-methods multicenter pilot study was conducted using a refined VWCR program, Destination Rehab, to evaluate the feasibility and acceptability of the intervention. Details of the overall study design are provided in Figure 1. The study was reviewed and approved by the Mayo Clinic Institutional Review Board.
Figure 1.
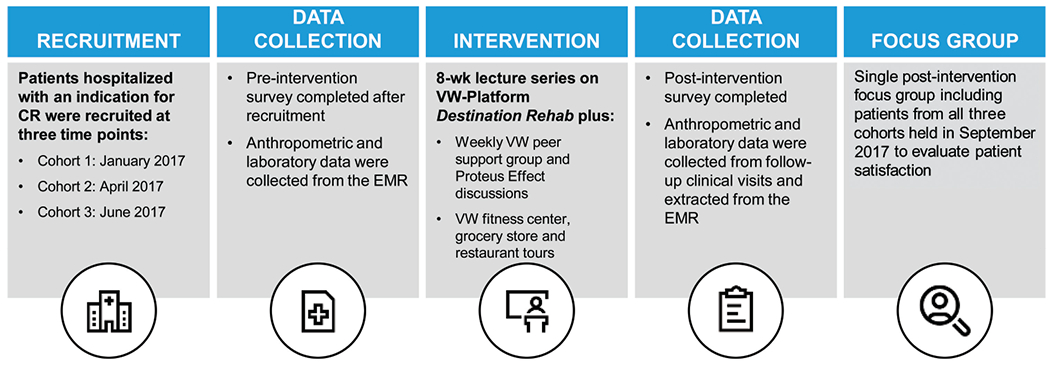
Summary of study design. Abbreviations: CR, cardiac rehabilitation; EMR, electronic medical record; VW, virtual world. This figure is available in color online (www.jcrpjournal.com).
STUDY PARTICIPANTS, SETTING, AND RECRUITMENT
Adult cardiac patients recently hospitalized at Mayo Clinic hospitals in Rochester, MN, Jacksonville, FL, or Scottsdale, AZ with an indication for CR were eligible to participate. Patients were excluded if they were <18 yr, nonfluent in English, or did not have home high-speed Internet access. Though limited by our recruitment settings, patients who historically have more barriers to participation in CR including women and lower socioeconomic status (annual household income <$50 000, education level lower than college graduate) were prioritized for recruitment. A recruitment goal of 30 patients (10/site) with ≥30% women was chosen.
Eligible patients were identified by review of the inpatient cardiology service census within the electronic medical record and the census of patients recently enrolled in CBCR by each site-specific study coordinators. The study coordinators visited eligible patients prior to hospital discharge or contacted them by telephone using a standardized script for recruitment. Patients who expressed interest were shown a brief demo video on VW technology and the VWCR platform. Otherwise, patients were recruited directly from CBCR and viewed the video at a separate recruitment visit. Written informed consent was obtained from patients agreeing to participate. Patients recruited prior to hospital discharge were encouraged to concurrently participate in CBCR for supervised exercise training and those recruited from CBCR were encouraged to continue in-person participation for assessments and contact with CR staff outside of the platform.
INTERVENTION
Three cohorts at the different Mayo Clinic sites attended a hands-on training session where they created Second Life avatars and learned to navigate Destination Rehab (see SDC 1, available at: http://links.lww.com/JCRP/A394). Loaner laptops were provided to patients who did not have access to a personal computer. Following the training session, patients participated in eight weekly educational sessions led by a CVD specialist and a CV nurse educator, both trained in motivational interviewing and the Second Life application. The 90-min sessions included lectures on diet, PA, stress management, CVD risk factors, and CV-related medications.41 Additionally, patients engaged in tours of the virtual fitness center, grocery store, and restaurant and a weekly support group. A trained exercise physiologist led a lecture and tour on exercise and fitness training as a part of the VWCR education curriculum. Participants had the opportunity to simulate a variety of exercise activities via their own avatars (eg, use of a treadmill, swimming, line dancing, and yoga). A registered dietitian provided education on heart healthy diets to promote CV health including DASH (Dietary Approaches to Stop Hypertension) and Mediterranean diets.48,49 The dietitian also led the interactive restaurant and grocery store tours and allowed the participants to proactively engage in “real-world” selection of healthy foods, proper portion sizes, and nutrition label reading. “Proteus effect” reflection discussions were held after each live session, where patients discussed ways in which they have translated healthy behaviors from the VW to the real world.43,44 A virtual library provided patients access to all lecture materials. Also, a bulletin board provided a forum for patient discussion to enhance social networking and user engagement. Technical support staff was present at all sessions to assist with any VW technology challenges. Patients received a 6-mo YMCA membership to minimize barriers to regular PA and a $25 cash card for participation.
DATA COLLECTION
Quantitative assessments were performed at baseline and post-intervention. Patients completed a baseline (pre-intervention) electronic survey collecting sociodemographic information, self-reported health history, perceived health status, health information sources, health care utilization, and outcome measures. The post-intervention survey additionally included an evaluation of intervention acceptability. Available biometrics were extracted from the electronic medical record at baseline and post-intervention (range 6-12 mo). Patient attendance and log-in data were recorded throughout the intervention by the study team.
Qualitative assessment by a single post-intervention focus group including patients from all three cohorts was facilitated on Second Life by an experienced qualitative researcher (J.E.). A semi-structured interview guide (see SDC 2, available at: http://links.lww.com/JCRP/A395) was developed using principles outlined by Krueger and Casey to explore patient perception of the intervention.50 The focus group was audio recorded with patient consent.
PRIMARY OUTCOME MEASURES
Study feasibility was evaluated utilizing metrics including recruitment goal attainment, patient retention, and adherence to the intervention as measured by patient live session attendance and VW platform usage.
Acceptability metrics were included in the post-intervention survey and post-intervention focus group. In the post-intervention survey, patients were asked to rate their overall VWCR experience from poor (0) to excellent (10). They were also asked to rate statements regarding perception of the education sessions, and platform ease of use, appearance, usefulness, and logic of information from strongly disagree (1) to strongly agree (5).
SECONDARY OUTCOME MEASURES
Both CV health behavior measures and biometrics from the electronic medical record were compared pre- and post-intervention.51 The CV health behavior measures included PA and diet, and biometrics included BMI, BP, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and hemoglobin A1c. The International Physical Activity Questionnaire evaluated PA including sedentary time, aerobic exercise, stretching, and resistance exercise.52 Diet was assessed by patient-reported number of servings of fruits and vegetables/d.
Cardiovascular health knowledge was assessed using 15 items from the Heart Disease Knowledge Questionnaire developed by Bergman and colleagues, a previously validated survey demonstrating sound psychometric properties.53 The survey contained true/false questions evaluating five factors of CV health knowledge domains, including dietary factors (two questions), epidemiologic factors (three questions), medical factors (three questions), risk factors (five questions), and symptoms (two questions). Six true/false questions addressing CR effects on CV health were developed by the study team probing additional questions regarding epidemiologic factors (eg, “There are no differences in the rates of heart disease between racial/ethnic groups in the United States”), factors affecting CR participation (eg, “Men are less likely than women to participate in cardiac rehab”), and CVD risk factors (eg, “How you cope with stress can affect your cardiovascular risk”). Three additional multiple-choice questions addressing CV health knowledge were included. The average percent of correct answers on the 24-item survey was tabulated and compared from baseline to post-intervention.53
Psychosocial factors including social support (ENRICHD Social Support Inventory), quality of life (Short Form [SF]-12 Health Survey), and optimism (Revised Life Orientation Test [LOT-R]) were measured using previously validated instruments.54–56
DATA ANALYSIS
Continuous variables are presented as mean ± SD and discrete variables as n (%). Study measures are summarized and compared between groups using the Pearson χ2 test for categorical variables or the Student t test for continuous variables. The changes in measures from baseline to post-intervention are calculated for all participants. These changes were also stratified by sex using paired t tests or McNemar’s tests. Statistical significance is defined as a two-tailed P value < .05. Statistical analyses were performed using SAS Version 9.4 (SAS Institute Inc).
Qualitative analysis of the post-intervention focus group discussion was conducted by an independent experienced qualitative research analyst (J.E.) based on the framework method.57 The focus group discussion took place in the VW platform and was audio-recorded, transcribed verbatim, and entered into a specialized qualitative software, NVivo12 (QRS International) for data management. The transcript was then coded utilizing a generalized inductive approach.58 The coded transcript was subsequently analyzed to identify notable themes and corresponding illustrative quotes.
RESULTS
Patient demographics and baseline characteristics are shown in Table 1. The age of patients was 59.1 ±9.7 yr (50% female). The most common reported sources for obtaining health information included doctors/health care providers (89%) and medical websites (71%). Men had a higher proportion of concurrent enrollment in CBCR than women (79% vs 50%, P = .11).
Table 1.
Patient Baseline Demographics and Characteristics by Sexa
| Variable | All (n = 28) | Men (n = 14) | Women (n = 14) | P Valueb |
|---|---|---|---|---|
| Age, yr | 59.1 ± 9.7 | 57.4 ± 12.0 | 60.8 ± 6.8 | .36 |
| Race | .68 | |||
| American Indian/Alaskan Native | 1 (4) | 1 (7) | 0 (0) | |
| Asian | 3 (11) | 2 (14) | 1 (7) | |
| Black/African American | 2 (7) | 1 (7) | 1 (7) | |
| White | 22 (79) | 10 (71) | 12 (86) | |
| Ethnicity | ||||
| Non-Hispanic/Latino | 28 (100) | 14 (100) | 14 (100) | |
| Marital status | .07 | |||
| Married/committed relationship | 22 (79) | 13 (93) | 9 (64) | |
| Not married/committed relationship | 6 (21) | 1 (7) | 5 (36) | |
| Education level | .22 | |||
| College degree or higher | 9 (32) | 6 (43) | 3 (21) | |
| No college degree | 19 (68) | 8 (57) | 11 (79) | |
| Insurance status | .56 | |||
| Insured | 26 (93) | 12 (86) | 14 (100) | |
| Not insured | 2 (7) | 2 (14) | 0 (0) | |
| Employment status | .7 | |||
| Employed full-time | 13 (46) | 7 (50) | 6 (43) | |
| Not employed full-time | 15 (54) | 7 (50) | 8 (57) | |
| Annual household income | .81 | |||
| ≥$75 000 | 11 (39) | 5 (36) | 6 (43) | |
| <$75 000 | 14 (50) | 7 (50) | 7 (50) | |
| Choose not to disclose | 3 (11) | 2 (14) | 1 (7) | |
| Self-reported medical history | ||||
| Type 2 diabetes | 9 (32) | 3 (21) | 6 (43) | .22 |
| Hypertension | 14 (50) | 5 (36) | 9 (64) | .13 |
| Percutaneous coronary intervention | 19 (68) | 10 (71) | 9 (64) | .69 |
| Coronary artery bypass graft surgery | 4 (14) | 3 (21) | 1 (7) | .28 |
| Heart transplant | 2 (7) | 2 (14) | 0 (0) | .14 |
| Heart assistive device | 2 (7) | 2 (14) | 0 (0) | .16 |
| Defibrillator/pacemaker | 5 (18) | 2 (14) | 3 (21) | .62 |
| Valve surgery | 6 (22) | 3 (23) | 3 (21) | .92 |
| Family history of early coronary artery disease | 12 (44) | 7 (50) | 5 (38) | .55 |
| Cardiac rehabilitation | ||||
| Enrolled | .11 | |||
| Yes | 18 (64) | 11 (79) | 7 (50) | |
| No | 10 (36) | 3 (21) | 7 (50) | |
| Completed | ||||
| Yes | 11 (61)c | 7 (64) | 4 (57) | .78 |
| No | 7 (39)c | 4 (36) | 3 (43) | |
| Health information sources | ||||
| Doctors/health care providers | 25 (89) | 11 (79) | 14 (100) | .07 |
| Virtual world/Second Life | 4 (14) | 2 (14) | 2 (14) | |
| Social media | 2 (7) | 1 (7) | 1 (7) | 1 |
| Medical websites | 20 (71) | 10 (71) | 10 (71) | 1 |
| Nonmedical websites | 4 (14) | 3 (21) | 1 (7) | .28 |
| Cardiovascular health knowledge, % correct | 81.6 ± 8.3 | 81.7 ± 7.1 | 81.6 ± 9.6 | .98 |
Data presented for N = 28 participants (93% of N = 30 enrolled participants) who participated in at least 1 live virtual world-based cardiac rehabilitation session. Data are reported as n (%) or mean ± SD.
P values are based on the Pearson χ2 test for categorical variables or the t test for continuous variables.
Data reported as n (%) among those enrolled.
Patient recruitment and retention are summarized in Figure 2. Of the 44 patients recruited, 30 were enrolled into the study. Twenty-eight connected and participated in ≥1 live session (93%), with 20 patients (71%) attending ≥6 sessions (≥75% of sessions). An average of 79.2 ± 21.1% of patients attended each session, with 83.9 ± 13.1% women in attendance compared with 68.8 ± 8.5% men (P = .02).
Figure 2.
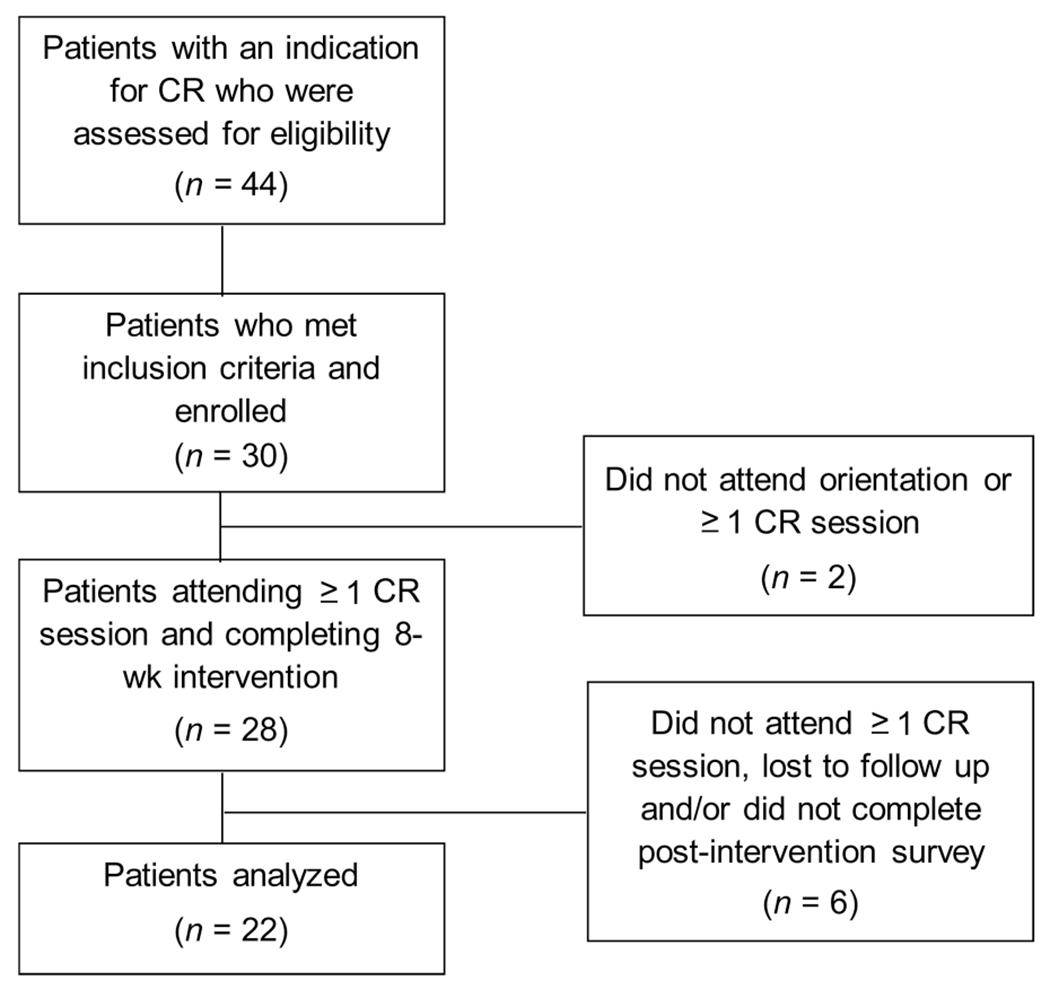
Modified CONSORT flow diagram. Abbreviation: CR, cardiac rehabilitation.
The patients rated their overall experience with the VWCR program an 8 ± 1.7 out of 10 points. They rated the presentations as very good/excellent (>80%) for style, content, and presentation. Patients felt that the platform was easy to use (95%) and easy to learn (95%). They reported that the sessions improved their knowledge about health (100%) and helped them to maintain better health habits (95%). All patients were satisfied with the platform appearance and quality (100%).
CARDIOVASCULAR HEALTH
There were statistically significant improvements in mean time engaged in stretching/flexibility exercises in men (Δ + .9 ± .9 d/wk, P = .05) and mean total cholesterol for all participants (Δ −31.6 ± 46.2 mg/dL, P =.05). Though not statistically significant, there were other positive trends in CV health behaviors from baseline to post-intervention (Table 2) including mean time engaged in vigorous PA. There were notable trends in biometrics including an improvement in mean LDL-C. Among men, there was a reduction in both mean systolic BP and mean diastolic BP, but these did not reach statistical significance. Women had larger improvements, although not statistically significant, in total cholesterol and LDL-C compared with men. Women also lost an average of 3.1 kg versus men who gained an average of 2.4 kg.
Table 2.
Changes in Secondary Outcomes From Baseline to Post-intervention, Within Group by Sexa
| Variable | All | P Valueb | Men | P Valueb | Women | P Valueb |
|---|---|---|---|---|---|---|
| Vigorous PA | .05 | .16 | .16 | |||
| d/wk | 0.29 ± 0.95 | .46 | 0.6 ± 0.9 | .50 | −0.50 ± 0.7 | .50 |
| min/d | 10.7 ± 11.7 | .05 | 13.0 ± 11.5 | .06 | 5.0 ± 14.1 | .70 |
| Moderate PA | .16 | .05 | 1.00 | |||
| d/wk | 1.0 ± 3.0 | .38 | 2.0 ± 2.8 | .50 | −0.7 ± 3.1 | .74 |
| min/d | 7.5 ± 42.0 | .63 | 18.0 ± 40.8 | .75 | −10.0 ± 45.8 | .74 |
| Strength/weight training | .32 | 1.00 | .16 | |||
| min/wk | 26.2 ± 75.4 | .36 | 28.3 ± 88.8 | .47 | 20.0 ± 14.1 | .30 |
| Stretching/flexibility exercises | .03 | .08 | .18 | |||
| d/wk | 0.8 ± 0.8 | .06 | 0.8 ± 0.9 | .05 | 0.5 ± 0.7 | .50 |
| min/wk | 8.3 ± 33.8 | .48 | 20.0 ± 28.4 | .11 | −32.5 ± 3.5 | .05 |
| Weight, kg | −0.4 ± 1.9 | .19 | 2.4 ± 9.9 | .57 | −3.1 ± 9.3 | .30 |
| BMI, kg/m2 | −0.2 ± 9.8 | .53 | 0.8 ± 2.9 | .73 | −1.1 ± 2.6 | .18 |
| Systolic BP, mm Hg | −0.1 ± 2.9 | .52 | −14.1 ± 34.3 | .20 | 1.2 ± 23.1 | .87 |
| Diastolic BP, mm Hg | −6.8 ± 29.8 | .31 | −3.1 ± 13.1 | .45 | 6.8 ± 10.2 | .06 |
| Total cholesterol, mg/dL | 1.6 ± 12.6 | .56 | −16.5 ± 47.4 | .43 | −49.8 ± 42.0 | .06 |
| LDL-C, mg/dL | −31.9 ± 69.9 | .16 | −4.3 ± 28.3 | .72 | −52.0 ± 49.6 | .08 |
| Hemoglobin A1c, % | 0.3 ± 0.8 | .47 | 0.1 ± 0.2 | .47 | 0.6 ± 1.2 | .50 |
| Heart disease knowledge | 0.7 ± 9.4 | .73 | 1.0 ± 7.0 | .63 | 0.36 ± 11.7 | .92 |
| Social Support score | 0.32 ± 3.0 | .77 | −0.36 ± 1.8 | .51 | 1 ± 3.8 | .40 |
| SF-12 score | 0.05 ± 0.11 | .06 | 0.04 ± 0.13 | .33 | 0.06 ± 0.08 | .06 |
| Optimism score | −0.25 ± 3.1 | .72 | −2.0 ± 2.7 | .06 | 1.2 ± 2.6 | .17 |
Abbreviations: BMI, body mass index; BP, blood pressure; LDL-C, low-density lipoprotein cholesterol; PA, physical activity; SF-12, w Suivey.
Data are reported as mean ± SD.
P values are based on McNemar’s test for categorical variables or paired t tests for continuous variables.
At baseline, patients scored 81.6 ± 8.3% on the heart disease knowledge survey, which was unchanged at post-intervention (Table 2).
There were no statistically significant changes in social support, quality of life, or optimism from baseline to post-intervention (Table 2).
FOCUS GROUP RESULTS
Responses by patients indicated that a VWCR program was a highly acceptable method to augment CBCR. Four main themes emerged from the focus group discussion regarding the Destination Rehab program including: (1) complementary to CBCR, (2) convenient modality for CR delivery, (3) educational by providing valuable health information on key CV topics, and (4) social networking beneficial to recovery (Table 3).
Table 3.
Focus Group Salient Themes and Illustrative Quotes
| Theme | Quote |
|---|---|
| Complements center-based cardiac rehabilitation | “I wasn’t able to participate in a lot of the classes or the extra things [in center-based cardiac rehabilitation] and so I got most of that from Second Life.” |
| Convenience | “There were people who were so remote that there was no way they were going to have access to a group, which to me was phenomenal. I think it’s going to be fantastic for a lot of people.” |
| Educational | “We went and did the restaurant ordering and then you went over to the athletic area and they gave you a rundown on how much exercise you’d have to burn for what you just ordered.” |
| Social connection | “The meetings hold you accountable. You’re meeting with a group who will ask questions, we’re going to talk about what we did. So yeah, definitely it just kind of put me on a pattern which I’ve been able to continue.” |
Several patients expressed that Destination Rehab served as a complement to but did not replace CBCR. They emphasized benefits of supervised CBCR but noted that Destination Rehab more conveniently replaced the additional curriculum. Patients agreed that Destination Rehab was a convenient platform for providing an educational experience and a rich social network that otherwise may not be accessible.
Patients acknowledged a perceived improvement in knowledge regarding CV health. One patient explained that their doctor gave an overview of CVD but noted that they appreciated the depth of information in the Anatomy and Physiology lecture. Several patients noted that they appreciated having a deeper understanding of their CV-related medications. They also described the practical knowledge and confidence gained from the interactive VW experience, which they were able to translate into real-world behavior changes.
Patients were comforted by listening to the stories of others and realizing that they are not alone. They enjoyed listening to the experiences of others and even suggested having individuals who have undergone similar experiences share their stories. The social connection fostered a sense of accountability to the group.
DISCUSSION
The VWCR program, Destination Rehab, was shown to be a feasible and highly acceptable method of delivering the educational, health behavior modification, and CVD risk factor control aspects of CR, based on excellent patient recruitment, retention, attendance rates, and patient-reported satisfaction. Additionally, our study demonstrated exemplary intervention adherence in women. While women were less likely to be enrolled in CBCR, they attended more Destination Rehab sessions on average compared with men. Patients were highly satisfied with the intervention and acknowledged that Destination Rehab could be a convenient complement to CBCR, as it can provide the educational component of CR at home, while maintaining the development of social connections that patients felt were essential for their recovery. While there were no statistically significant changes in secondary outcome measures, there were favorable trends in CV risk factors from pre- to post-intervention.
Attendance to our VWCR sessions was comparable to attendance rates previously observed in both HBCR and CBCR. A large meta-analysis conducted by Oosenbrug et al.9 showed that patient attendance to CBCR sessions averages 66.5 ± 18.2%, which is similar to adherence rates noted by additional studies.1,30,32 Though our sample size was small and not directly compared to CBCR, the adherence to our VWCR program was comparable to this previously observed rate. Oosenbrug et al9 also showed that adherence to CBCR in women was consistently lower than that of men, an observation noted in a variety of studies.13,14 While we observed excellent adherence rates in women, there is insufficient data in the literature to compare the adherence rates of women in our study to alternative non-CBCR methods.1,13
Modification of CVD risk factors, one of the cornerstones of CR, is a means by which CR programs achieve improved patient outcomes.1,2 The current literature suggests that alternative CR delivery programs, such as HBCR, demonstrate comparable improvements in clinical, behavioral, and psychosocial risk factors for CVD when compared with traditional CBCR.1,30,33 While this study was inadequately powered to sufficiently detect statistical significance, clinically relevant trends were noted in both CV health and psychosocial outcomes. More research is needed to compare the efficacy of this intervention to CBCR alone and other alternative CR delivery modalities.
Overall, our study supports the promising potential for VWCR programs to reach populations with a high burden of competing demands by combining unique qualities of both HBCR and CBCR. Destination Rehab capitalizes on many advantages of HBCR including flexibility, decreased travel and transportation barriers, and increased privacy, while incorporating critical aspects of CBCR including social support and patient accountability.1 Patients in the focus group asserted better availability to attend Destination Rehab sessions, supporting the notion that the flexible nature of VWCR programs can broaden CR access. Furthermore, our program reduced transportation barriers. In addition, Destination Rehab has advantages that are often absent in other HBCR programs. For example, patients highlighted the weekly support group as an important CR component, as it offered social support and accountability to the group, both important aspects of behavioral modification.19,37–39 Additionally, unique to a VW platform, patients engaged in a hands-on virtual gym, restaurant, and grocery store, which they acknowledged gave them the knowledge and confidence to make informed and healthy choices in the real world. In summary, the unique characteristics inherent to VWs may provide a powerful solution to broaden access to CR and better promote patient participation and retention. More research is needed to directly compare VWCR adherence rates and CVD risk factor modification to CBCR alone and its impact in minority, socioeconomically disadvantaged, and rural populations.
STRENGTHS AND LIMITATIONS
The most important strength of our study is the novel method of CR delivery and its unique features that distinguish it from other forms of HBCR. The intervention and multicenter design were adapted from an initial proof-of-concept study, integrating participant feedback to better meet patient needs. Unlike other HBCR programs, Destination Rehab offers a rich social network that fosters a sense of group accountability, while maintaining anonymity. The Second Life platform offered a reliable network with minimal technological challenges. Our mixed-methods approach granted us insight to not only the impact of this intervention, but also patient perceptions of its advantages and limitations. Furthermore, our study had excellent recruitment and retention of women, an important population to prioritize when considering alternative approaches to CR delivery.
Notably, Destination Rehab does not offer the patient assessment and supervised exercise training components of CR.3 These are important aspects of CR in improving outcomes. Thus, in its current form, Destination Rehab is an extension to, rather than a replacement of CBCR. However, the intervention included opportunities for interaction with and simulated learning from a trained exercise physiologist on proper exercise techniques. Other study limitations include a small sample size limiting statistical power, and variable timing of documentation of post-intervention data in the electronic medical record as well as missing data. The study did not assess changes in prescribing of CV-related medications, medication adherence, or objective functional status measurements. These variables and others not assessed could potentially confound the positive trends noted in biometric changes. The demographics of patients treated within the Mayo Clinic Health System limited the ability to recruit socioeconomically disadvantaged patients. Most patients were White, insured, socioeconomically advantaged, and all had access to an academic medical center, limiting the generalizability of our results to other populations. Plans are currently underway to conduct a larger, randomized clinical trial with inclusion of health care systems serving patients with a high burden to barriers to CR participation.
CONCLUSIONS
Destination Rehab, a VWCR program, is a feasible and highly acceptable modality of delivering CR, suggesting that it could serve as a convenient adjunct to traditional CR. It has the potential to overcome many barriers to traditional CR, especially in populations with limited access to CR, without omitting some of its most critical aspects, including social support and patient accountability. More research is needed to clarify its impact on CVD risk factor modification compared with CBCR.
Supplementary Material
ACKNOWLEDGMENTS
This study was supported by the Mayo Clinic Center for Innovation, Mayo Clinic Center for Translational Science Activities (UL1TR000135), Mayo Clinic Department of Cardiovascular Medicine, and Mayo Clinic Center for Health Equity and Community Engagement Research. Dr Brewer was supported by the Building Interdisciplinary Research Careers in Women’s Health Scholars Program (award number K12 HD065987-07) from the National Institutes of Health (NIH) Office of Research on Women’s Health, Mayo Clinic Women’s Health Research Center, and the National Center for Advancing Translational Sciences (NCATS, Clinical and Translational Science Awards Grant Number KL2 TR002379), a component of the NIH and the American Heart Association-Amos Medical Faculty Development Program (Grant Number 19AMFDP35040005) during implementation and analysis of this work. The authors would like to express gratitude for the on-site study coordinators, Mrs Lorraine Mai, Mrs Isabel Santana, and Mrs Jessica Bauman, for their invaluable contribution to the organization and execution of this study. We would like to thank the patients who enthusiastically participated in the Destination Rehab program. A special thanks to Mrs Dawn Finnie (Kern Center for the Science of Health Care Delivery, Mayo Clinic) for her assistance in organizing and moderating the focus group.
The content of the article is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences, National Institutes of Health, or Centers for Disease Control and Prevention. The funding bodies had no role in study design; in the collection, analysis, and interpretation of data; writing of the manuscript; and in the decision to submit the manuscript for publication.
Footnotes
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jcrpjournal.com).
Contributor Information
LaPrincess C. Brewer, Department of Cardiovascular Medicine, Mayo Clinic College of Medicine, Rochester, Minnesota; Center for Health Equity and Community Engagement Research, Mayo Clinic, Rochester, Minnesota.
Helayna Abraham, Department of Internal Medicine, Mayo Clinic College of Medicine, Rochester, Minnesota.
Brian Kaihoi, Global Products and Services, Mayo Clinic Center for Innovation, Rochester, Minnesota.
Shawn Leth, Department of Cardiovascular Medicine, Mayo Clinic College of Medicine, Rochester, Minnesota.
Jason Egginton, Center for the Science of Health Care Delivery, Mayo Clinic College of Medicine, Rochester, Minnesota.
Joshua Slusser, Department of Quantitative Health Sciences, Division of Clinical Trials and Biostatistics, Mayo Clinic, Rochester, Minnesota.
Christopher Scott, Department of Quantitative Health Sciences, Division of Clinical Trials and Biostatistics, Mayo Clinic, Rochester, Minnesota.
Sumedha Penheiter, Center for Health Equity and Community Engagement Research, Mayo Clinic, Rochester, Minnesota.
Monica Albertie, Center for Health Equity and Community Engagement Research, Mayo Clinic, Jacksonville, Florida.
Ray Squires, Department of Cardiovascular Medicine, Mayo Clinic College of Medicine, Rochester, Minnesota.
Randal Thomas, Department of Cardiovascular Medicine, Mayo Clinic College of Medicine, Rochester, Minnesota.
Robert Scales, Department of Cardiovascular Medicine, Mayo Clinic College of Medicine, Scottsdale, Arizona.
Jorge Trejo-Gutierrez, Department of Cardiovascular Medicine, Mayo Clinic College of Medicine, Jacksonville, Florida.
Stephen Kopecky, Department of Cardiovascular Medicine, Mayo Clinic College of Medicine, Rochester, Minnesota.
REFERENCES
- 1.Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Cardiopulm Rehabil Prev. 2019;39(4):208–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goel K, Lennon RJ, Tilbury RT, Squires RW, Thomas RJ. Impact of cardiac rehabilitation on mortality and cardiovascular events after percutaneous coronary intervention in the community. Circulation. 2011;123(21):2344–2352. [DOI] [PubMed] [Google Scholar]
- 3.Martin BJ, Arena R, Haykowsky M, et al. Cardiovascular fitness and mortality after contemporary cardiac rehabilitation. Mayo Clin Proc. 2013;88(5):455–463. [DOI] [PubMed] [Google Scholar]
- 4.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2018;71(16):1814–1837. [DOI] [PubMed] [Google Scholar]
- 5.Anderson L, Thompson DR, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;2016(1):Cd001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alqahtani MM, Alanazi AMM, Yohannes AM, Smith CE, Goodfellow LT. The effectiveness of cardiopulmonary rehabilitation programs on psychosocial factors in patients with pulmonary and cardiac disease. J Cardiopulm Rehabil Prev. 2021;41(4):271–276. [DOI] [PubMed] [Google Scholar]
- 7.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2018;11(4):e000037. [DOI] [PubMed] [Google Scholar]
- 8.Ozemek C, Lavie CJ, Kaminsky LA. Review of recent cardiac rehabilitation research related to enrollment/adherence, mental health, and other populations. J Cardiopulm Rehabil Prev. 2021;41(5):302–307. [DOI] [PubMed] [Google Scholar]
- 9.Oosenbrug E, Marinho RP, Zhang J, et al. Sex differences in cardiac rehabilitation adherence: a meta-analysis. Can J Cardiol. 2016;32(11):1316–1324. [DOI] [PubMed] [Google Scholar]
- 10.Sun EY, Jadotte YT, Halperin W. Disparities in cardiac rehabilitation participation in the United States: a systematic review and meta-analysis. J Cardiopulm Rehabil Prev. 2017;37(1):2–10. [DOI] [PubMed] [Google Scholar]
- 11.Ritchey MD, Maresh S, McNeely J, et al. Tracking cardiac rehabilitation participation and completion among Medicare beneficiaries to inform the efforts of a national initiative. Circ Cardiovasc Qual Outcomes. 2020;13(1):e005902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castellanos LR, Viramontes O, Bains NK, Zepeda IA. Disparities in cardiac rehabilitation among individuals from racial and ethnic groups and rural communities—a systematic review. J Racial Ethn Health Disparities. 2019;6(1):1–11. [DOI] [PubMed] [Google Scholar]
- 13.Supervia M, Medina-Inojosa JR, Yeung C, et al. Cardiac rehabilitation for women: a systematic review of barriers and solutions [published online ahead of print March 13, 2017]. Mayo Clin Proc. doi: 10.1016/j.mayocp.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Samayoa L, Grace SL, Gravely S, Scott LB, Marzolini S, Colella TJ. Sex differences in cardiac rehabilitation enrollment: a meta-analysis. Can J Cardiol. 2014;30(7):793–800. [DOI] [PubMed] [Google Scholar]
- 15.Ozemek C, Babu AS, Arena R, Bond S. Strategies to achieving the national 70% cardiac rehabilitation enrollment rate. J Cardiopulm Rehabil Prev. 2021;41(5):E14–e15. [DOI] [PubMed] [Google Scholar]
- 16.Mathews L, Brewer LC. A review of disparities in cardiac rehabilitation: evidence, drivers, and solutions. J Cardiopulm Rehabil Prev. 2021;41(6):375–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bakhshayeh S, Sarbaz M, Kimiafar K, Vakilian F, Eslami S. Barriers to participation in center-based cardiac rehabilitation programs and patients’ attitude toward home-based cardiac rehabilitation programs. Physiother Theory Pract. 2021;37(1):158–168. [DOI] [PubMed] [Google Scholar]
- 18.Foster EJ, Munoz SA, Crabtree D, Leslie SJ, Gorely T. Barriers and facilitators to participating in cardiac rehabilitation and physical activity in a remote and rural population: a cross-sectional survey. Cardiol J. 2021;28(5):697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chindhy S, Taub PR, Lavie CJ, Shen J. Current challenges in cardiac rehabilitation: strategies to overcome social factors and attendance barriers. Expert Rev Cardiovasc Ther. 2020;18(11):777–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schopfer DW, Nicosia FM, Ottoboni L, Whooley MA. Patient perspectives on declining to participate in home-based cardiac rehabilitation: a mixed-methods study. J Cardiopulm Rehabil Prev. 2020;40(5):335–340. [DOI] [PubMed] [Google Scholar]
- 21.Grace SL, McDonald J, Fishman D, Caruso V. Patient preferences for home-based versus hospital-based cardiac rehabilitation. J Cardiopulm Rehabil. 2005;25(1):24–29. [DOI] [PubMed] [Google Scholar]
- 22.Tang LH, Kikkenborg Berg S, Christensen J, et al. Patients’ preference for exercise setting and its influence on the health benefits gained from exercise-based cardiac rehabilitation. Int J Cardiol. 2017;232:33–39. [DOI] [PubMed] [Google Scholar]
- 23.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124(25): 2951–2960. [DOI] [PubMed] [Google Scholar]
- 24.Vigorito C, Faggiano P, Mureddu GF. COVID-19 pandemic: what consequences for cardiac rehabilitation? Monaldi Arch Chest Dis. 2020;90(1). [DOI] [PubMed] [Google Scholar]
- 25.Epstein E, Patel N, Maysent K, Taub PR. Cardiac rehab in the COVID Era and beyond: mHealth and other novel opportunities. Curr Cardiol Rep. 2021;23(5):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mureddu GF, Giallauria F, Venturini E, Fattirolli F, Ambrosetti M. Cardiac rehabilitation and secondary prevention programs during the COVID-19 pandemic: what’s “COVID on”? G Ital Cardiol (Rome). 2020;21(7):527–528. [DOI] [PubMed] [Google Scholar]
- 27.Bokolo Anthony J Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fersia O, Bryant S, Nicholson R, et al. The impact of the COVID-19 pandemic on cardiology services. Open Heart. 2020;7(2):e001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shaw J, Brewer L, Veinot T. Health equity and virtual care: a narrative review of recommendations arising from the COVID-19 pandemic. JMIR Form Res. 2021;5(4):e23233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor RS, Dalal H, Jolly K, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev 2015(8):Cd007130. [DOI] [PubMed] [Google Scholar]
- 31.Anderson L, Sharp GA, Norton RJ, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6(6):Cd007130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shanmugasegaram S, Oh P, Reid RD, McCumber T, Grace SL. A comparison of barriers to use of home- versus site-based cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2013;33(5):297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clark RA, Conway A, Poulsen V, Keech W, Tirimacco R, Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015;22(1):35–74. [DOI] [PubMed] [Google Scholar]
- 34.Drwal KR, Wakefield BJ, Forman DE, Wu WC, Haraldsson B, El Accaoui RN. Home-based cardiac rehabilitation: experience from the Veterans Affairs. J Cardiopulm Rehabil Prev. 2021;41(2):93–99. [DOI] [PubMed] [Google Scholar]
- 35.Thomas RJ, Petersen CE, Olson TP, Beatty AL, Ding R, Supervia M. Asynchronous and synchronous delivery models for home-based cardiac rehabilitation: a scientific review. J Cardiopulm Rehabil Prev. 2021;41(6):407–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thomas R, Scales R, Fernandes R. Alternative models to facilitate and improve delivery of cardiac rehabilitation/secondary prevention. In: Rippe JM, ed. Lifestyle Medicine. 3rd ed. Boca Raton, FL: CRC Press; 2019:833–837. [Google Scholar]
- 37.Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. Behavioral Counseling to Promote a Healthful Diet and Physical Activity for Cardiovascular Disease Prevention in Adults Without Known Cardiovascular Disease Risk Factors: Updated Systematic Review for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality (US); 2017. [PubMed] [Google Scholar]
- 38.Johnston JD, Massey AP, Devaneaux CA. Innovation in weight loss programs: a 3-dimensional virtual-world approach. J Med Internet Res. 2012;14(5):e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gold BC, Burke S, Pintauro S, Buzzell P, Harvey-Berino J. Weight loss on the web: a pilot study comparing a structured behavioral intervention to a commercial program. Obesity (Silver Spring). 2007;15(1):155–164. [DOI] [PubMed] [Google Scholar]
- 40.Widmer RJ, Collins NM, Collins CS, West CP, Lerman LO, Lerman A. Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clin Proc. 2015;90(4):469–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. New York, NY: Guilford Press; 2013. [Google Scholar]
- 42.Ades PA, Keteyian SJ, Wright JS, et al. Increasing cardiac rehabilitation participation from 20% to 70%: a road map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92(2):234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brewer LC, Kaihoi B, Zarling KK, Squires RW, Thomas R, Kopecky S. The use of virtual world-based cardiac rehabilitation to encourage healthy lifestyle choices among cardiac patients: intervention development and pilot study protocol. JMIR Res Protoc. 2015;4(2):e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ghanbarzadeh R, Ghapanchi AH, Blumenstein M, Talaei-Khoei A. A decade of research on the use of three-dimensional virtual worlds in health care: a systematic literature review. J Med Internet Res. 2014;16(2):e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yee N, Bailenson J. The Proteus effect: the effects of transformed self-representation on behavior. Hum Commun Res. 2007;33(3):271–290. [Google Scholar]
- 46.Brewer LC, Kaihoi B, Schaepe K, et al. Patient-perceived acceptability of a virtual world-based cardiac rehabilitation program. Digit Health. 2017;3:2055207617705548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. [DOI] [PubMed] [Google Scholar]
- 48.Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378(25):e34. [DOI] [PubMed] [Google Scholar]
- 49.Sukhato K, Akksilp K, Dellow A, Vathesatogkit P, Anothaisintawee T. Efficacy of different dietary patterns on lowering of blood pressure level: an umbrella review. Am J Clin Nutr. 2020;112(6):1584–1598. [DOI] [PubMed] [Google Scholar]
- 50.Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. Singapore: Sage Publications; 2014. [Google Scholar]
- 51.Wu S, An S, Li W, et al. Association of trajectory of cardiovascular health score and incident cardiovascular disease. JAMA Netw Open. 2019;2(5):e194758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim Y, Park I, Kang M. Convergent validity of the International Physical Activity Questionnaire (IPAQ): meta-analysis. Public Health Nutr. 2013;16(3):440–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bergman HE, Reeve BB, Moser RP, Scholl S, Klein WM. Development of a Comprehensive Heart Disease Knowledge Questionnaire. Am J Health Educ. 2011;42(2):74–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vaglio J Jr, Conard M, Poston WS, et al. Testing the performance of the ENRICHD Social Support Instrument in cardiac patients. Health Qual Life Outcomes. 2004;2:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998;51(11):1171–1178. [DOI] [PubMed] [Google Scholar]
- 56.Hinz A, Schulte T, Finck C, et al. Psychometric evaluations of the Life Orientation Test-Revised (LOT-R), based on nine samples. Psychol Health 2021:1–13. [DOI] [PubMed] [Google Scholar]
- 57.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


