Abstract
The increase in air pollution worldwide represents an environmental risk factor that has global implications for the health of humans worldwide. The skin of billions of people is exposed to a mixture of harmful air pollutants, which can affect its physiology and are responsible for cutaneous damage. Some polycyclic aromatic hydrocarbons are photoreactive and could be activated by ultraviolet radiation (UVR). Therefore, such UVR exposure would enhance their deleterious effects on the skin. Air pollution also affects vitamin D synthesis by reducing UVB radiation, which is essential for the production of vitamin D3, tachysterol, and lumisterol derivatives. Ambient air pollutants, photopollution, blue-light pollution, and cigarette smoke compromise cutaneous structural integrity, can interact with human skin microbiota, and trigger or exacerbate a range of skin diseases through various mechanisms. Generally, air pollution elicits an oxidative stress response on the skin that can activate the inflammatory responses. The aryl hydrocarbon receptor (AhR) can act as a sensor for small molecules such as air pollutants and plays a crucial role in responses to (photo)pollution. On the other hand, targeting AhR/Nrf2 is emerging as a novel treatment option for air pollutants that induce or exacerbate inflammatory skin diseases. Therefore, AhR with downstream regulatory pathways would represent a crucial signaling system regulating the skin phenotype in a Yin and Yang fashion defined by the chemical nature of the activating factor and the cellular and tissue context.
Keywords: air pollutants, photopollution, cigarette smoke, AhR, skin diseases
1. Introduction
Environmental pollution is a global health problem associated with growing respiratory [1], cardiovascular [2], cutaneous [3,4], and neurological morbidities [5,6], as well as premature mortality [7,8]. Airborne pollution is defined as contamination by any chemical, physical, or biological agent from biogenic, anthropogenic, or mixed origins that modifies the natural characteristic of the atmosphere. Environmental exposure throughout one’s lifespan may lead to epigenetic changes that vary significantly with different types of air pollutants [9]. The exposure time window is also of great relevance for more severe outcomes at certain ages (e.g., childhood and advanced age). Moreover, air pollution exposure during pregnancy (in utero) may cause reduced fetal growth, pre-term birth, or spontaneous abortions [10]. As a first-line barrier, the human skin, together with the lungs, is the main target organ affected by the harmful insults of air pollution [11]. Billions of people are still exposed to unhealthy ambient air, of which the mixture of pollutants could affect skin physiology either directly by transcutaneous absorption or indirectly by their systemic distribution after inhalation or ingestion. The air pollutants of global concern include particulate matter (PM), polycyclic aromatic hydrocarbons (PAHs), benzene, ground-level ozone (O3) and other gaseous pollutants such as carbon monoxide (CO), nitrogen dioxide (NO2), and sulfur dioxide (SO2), various heavy metals, and volatile organic compounds (VOC).
PM is among the most harmful pollutants, being a heterogeneous mixture of very small particles and liquid droplets composed of organic chemicals, acids, metals, and soil or dust particles. Based on their size, they are subdivided into coarse particles with a diameter of 2.5 to 10 μm (PM10), fine particles with less than or equal to 2.5 μm (PM2.5), and ultrafine particular matter (UFPM) with a diameter under 100 nm (PM0.1), also called nanoparticles [12]. Currently, UFPM is considered the most abundant PM pollutant in the atmosphere of industrial and urban areas. The ambient PM through adhesion to the skin surface can reduce epidermal barrier function [13]. The transdermal penetration of solid particles depends on their size and shape, as well as on the state of the skin barrier. The nanoparticles that are larger than 45 nm cannot penetrate the skin. UFPM with a size between 21 and 45 nm can only penetrate and permeate skin with an impaired barrier in comparison with the smaller 4–20 nm nanoparticles, which can potentially permeate not only damaged skin but intact skin as well. UFPM equal to or smaller than 4 nm can penetrate intact skin [14]. Fine and ultrafine-sized particles (PM2.5 and PM0.1) are respirable and could affect pulmonary function [15]. Additionally, they can potentially reach the alveoli and cross the alveolar-capillary barrier of the lungs, gaining access via blood circulation to various organs [16,17]. In fact, UFPM has a large surface area and the capacity to adsorb PAHs, thus they can reach systemic blood circulation and deep skin, either from lung alveoli or via the skin surface, hair follicles, or eccrine and apocrine glands. Airborne PAHs are widespread and can be found in all human body fluids and hair [18]. PAHs are highly lipophilic, which allows them to easily penetrate the epidermal skin barrier. Moreover, various PAHs are present in cigarette smoke [19], leading to the accumulation of PAH-metabolites in the hair of smokers compared to non-smokers [20]. In fact, cigarette smoke contains several PAHs similar to those defined as air pollutants. Many PAHs can exert mutagenic and cytotoxic effects, and some of them could become phototoxic. Photoactivation of PAH upon ultraviolet A (UVA) light exposure would augment the deleterious effects of PM on the skin [21]. In Europe, PAH levels in the air are estimated via monitoring of the photoreactive benzo(a)pyrene (BaP) (1 ng/m3 per year–standard) [22]. The pro-cancerogenic potency of air pollutant BaP could be accelerated by sunlight exposure [23]. Anthracene, BaP, and naphthalene are direct irritants and sensitizers of the skin.
O3 is a highly reactive pollution oxidant formed by the interaction of VOCs and gaseous NO compounds upon UV-photoactivation. Even though O3 is not a radical species per se, its noxious effects on the epidermis are mediated through the generation of potentially toxic peroxidation products and antioxidant depletion [24]. In fact, it is proven that exposure of human cutaneous tissue to O3 increases lipid peroxidation byproducts: α-β unsaturated aldehyde 4-hydroxynonenal (4HNE) and 8-iso-prostaglandin-F2α(8-iso F2α) [25].
The skin is also a target of another physical stressor represented by UV radiation (UVR). UVR is the most harmful environmental factor that affects skin biology contributing to photodamage on chronically sun-exposed areas, thus accelerating the physiological aging process and increasing skin cancer risk [26,27]. UVR wavelengths of solar radiation reaching the Earth’s surface include UVB (290–320 nm) and UVA (320–400 nm), each having a different mechanism of action on the skin and other tissues exposed to radiation. For example, the biological response to UVB is predominantly dependent on the absorption of its energy by chromophores such as DNA, pyrimidines and purines, aromatic amino acids, indoles, proteins, and biogenic amines, leading to tissue damage and genetic mutations, and to a lower degree, on the generation of reactive oxygen species (ROS). UVA biological activity, on the other hand, is primarily dependent on ROS and reactive nitrogen species (RNS) production with absorption by limited cellular chromophores such as NADH, NADPH, riboflavin, and porphyrins, and being weakly absorbed by DNA [26,28]. Both wavelengths have different levels of skin penetration. For example, UVB primarily penetrates the epidermis and, to a lower degree, the papillary dermis [26,29]. On the other hand, UVA penetrates deeply into the reticular dermis, also reaching the hypodermis [26,29]. UVR also influences the composition of the cutaneous microbiome [30]. Moreover, the co-exposure of air pollutants (PM/PAHs) and UVA, defined as photopollution, causes an additive damaging effect on the skin [31].
Until recently, the deleterious effects of sunlight on the skin were assigned to the UVR. Recently, studies have demonstrated the negative impact of the most energetic light from the visible spectra, blue light, on the skin and the circadian rhythm [32,33]. With the widespread use of electronic devices, the problem of light pollution is becoming increasingly serious for human health. Humans are exposed to blue light from electronic screen devices (456 nm) and light-emitting-diodes (LEDs) during both day- and nighttime in modern society. In comparison with UV rays, blue light has deeper penetration into the subcutaneous tissue [34]. There is convincing evidence for retinal damage and degeneration caused by blue light pollution through the induction of ferroptosis [35]. On the skin, blue light irradiation can cause changes in skin chromophores and can induce hyperpigmentation (in dark skin) as a visible sign of photoaging [36].
2. Molecular Mechanisms of Pollutant-Affected Skin Physiology
Air pollutants and photopollution exert a negative impact on the skin health of the general population. They compromise cutaneous structural integrity, interact with human skin microbiota, and trigger or exacerbate a range of skin diseases through various mechanisms [4,37,38], which are briefly discussed below.
2.1. Skin-A Dynamic Barrier with the Capacity to Maintain Homeostasis
The skin is a complex, multifunctional organ with the capacity to maintain cutaneous and overall body homeostasis, electrolyte and fluid balance, and thermoregulation [39,40,41]. It operates as a fully functional and independent neuroendocrine biofactory producing hormones, neuropeptides, and neurotransmitters [41,42,43,44,45]. On the other hand, the skin serves not only as a source of hormones but also as a target for their activities [39,41,46,47]. In addition, UVB can induce the production of the prohormone vitamin D, which then transforms into biologically active metabolites [48,49]. Of note, vitamin D also plays an important role in epidermal barrier functions and cutaneous homeostasis protection [50] and participates in the modulation of skin immunity [51]. Furthermore, skin possesses an interactive network between the nerves, neuroendocrine signals, and the cutaneous immune system (NICE), securing homeostasis and skin integrity [45,52,53,54,55,56,57,58,59].
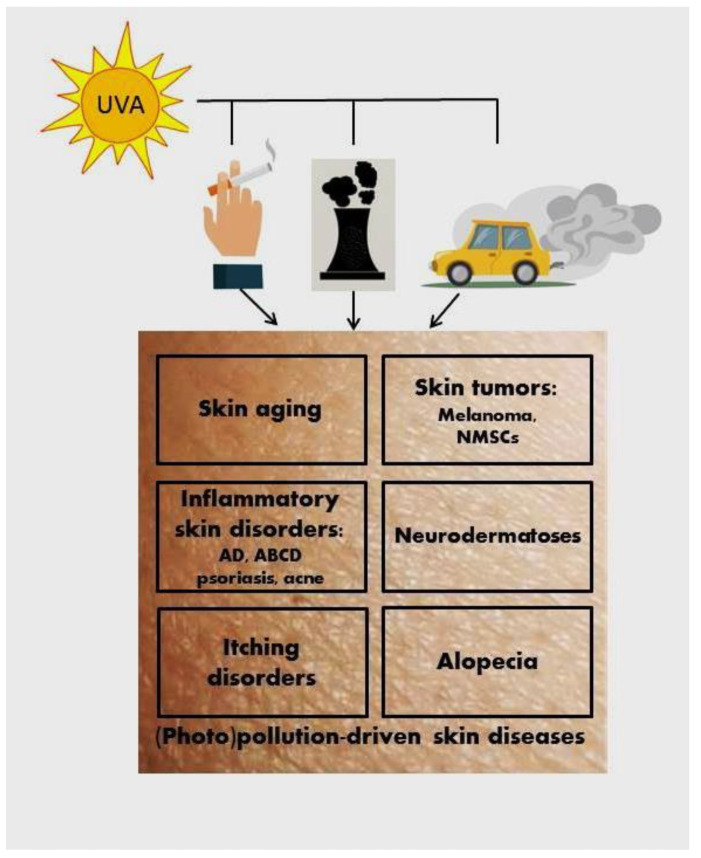
Facing the environment, the skin with its epidermal barrier [60] protects the body from the deleterious insults of its surroundings. Environmental factors trigger cutaneous changes that can imprint immune cells acting as messengers of skin responses to regulate local and systemic homeostasis. Frequently, skin is exposed to a mixture of air pollutants. The impact of air pollutants on the skin might be different depending on their particular characteristics and intensity, and the length of their exposure. The underlying mechanisms of skin damage also differ based on cutaneous contact with the particular pollutant or co-pollutants. Generally, air pollution elicits an oxidative stress response in the skin with the activation of inflammation, which drives the skin and systemic pathologies. These effects on health could be amplified by the deleterious synergic effect of chronic UVR exposure [61]. Air pollution can induce or exacerbate various skin pathological conditions and systemic diseases (Figure 1) such as premature skin aging, skin cancer (cutaneous melanoma, squamous cellular carcinoma (SCC), and basal cell carcinoma (BCC), inflammatory skin diseases (atopic dermatitis (AD), airborne contact dermatitis (ABCD), allergic contact dermatitis, and psoriasis, as examples), acne, alopecia including androgenic alopecia, pigmentary disorders such as vitiligo, melasma, post-inflammatory pigment alteration, different neurodermatoses, itching disorders, etc. [3,38].
Figure 1.
The deleterious synergic effect on the skin of UVA and air pollution. Non-melanoma skin cancer (NMSC); atopic dermatitis (AD); airborne contact dermatitis (ABCD).
2.2. Cutaneous Response to Air Pollutants, Photopollution, and Cigarette Smoke
It is well established that the skin responses to air pollutants, cigarette smoke, and blue light exposure lead to an induction of oxidative stress [62,63]. Several air pollutants, especially those containing PAHs (e.g., PMs, cigarette smoke), which are highly lipophilic, alone or after UVA exposure, by generating ROS/RNS, can significantly impair cellular redox homeostasis [31,64,65]. UFPM, with their small size, could enter the mitochondria via cellular uptake and promote ROS production resulting in mitochondrial impairment from oxidative processes [66]. Moreover, PM-linked mitochondrial DNA (mtDNA) oxidative injury was reported in maternal and umbilical cord blood in women exposed to PMs in various time windows during their pregnancy [67]. Additionally, PMs exhibit oxidative potential from their metal constituents (Fe, Cu, etc.) able to catalyze Fenton-like reactions, triggering ROS-associated oxidative damages [68].
It is well-accepted that oxidative stress leads to lipid peroxidation, protein carbonylation, and genomic and mtDNA oxidative damage. The main product of pollution-driven oxidative stress is the highly reactive compound 4HNE. It results from the non-enzymatic peroxidation of ω-6 polyunsaturated fatty acids (PUFAs) in the biomembranes, such as linolenic acid, which is essential for the skin [69]. 4HNE can be produced directly upon O3 exposure by oxidizing PUFAs present in the upper cutaneous layers, forming unstable peroxides, and indirectly after PMs and cigarette smoke contamination. It is believed that PMs and cigarette smoke trigger 4HNE production via the generation of ROS/RNS [64,70]. Free radicals initiate the oxidation of arachidonic acid leading to the formation of isoprostanes F2α (8-iso-F2α), which can increase phospholipid peroxidation and PUFAs oxidization while increasing the 4HNE concentration [71].
In addition, cutaneous exposure to O3 causes oxidative imbalances in the skin via the depletion of hydrophilic (vitamin C, glutathione, and uric acid) and lipophilic antioxidants (vitamin E) in the upper layers of the epidermis of human [72] and murine skin [73,74]. Of note, the stratum corneum has been identified as a primary target of O3-induced skin damage. The lipids on the skin surface derive from epidermal and sebaceous sources. Squalene is the major sebum-specific human skin lipid serving as a source of lipid peroxide on the skin surface [75]. As a defense against oxidative processes on the skin, vitamin E of nutritional origin is actively secreted from sebaceous glands and presumably co-secreted with squalene [76]. The main environmental stressors, such as O3, long UVA rays, PMs, and tobacco smoke, are able to boost the (per)oxidization process of squalene, resulting in the production of comedogenic molecules and the impairment of cutaneous physiology [77,78]. The biochemical changes in the sebum and corneal layer of the skin indicate pollutant-induced oxidative stress responses in humans living in urban areas, with decreased concentrations of squalene, vitamin E, and ATP and increased levels of carbonylated proteins [79]. In addition, a recent study showed an iron-dependent accumulation of lipid peroxides (ferroptosis) in female skin exposed to cigarette smoke [80].
2.3. AhR Signaling Pathway–A Target of Air Pollutants
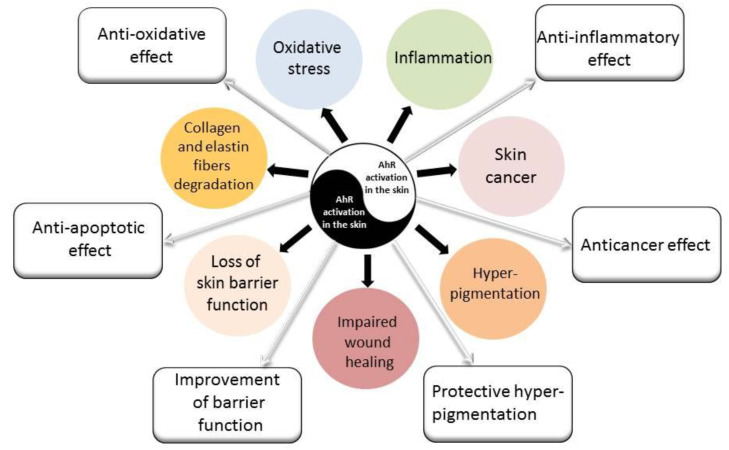
The aryl hydrocarbon receptor (AhR) is expressed in all epidermal and dermal cells and is essential for skin integrity and skin immunity [81,82]. It is widely considered that AhR exerts a dual role in skin physiology and pathology, including the regulation of melanogenesis, inflammatory responses, and skin cancerogenesis [83]. AhR is a sensor for a variety of molecules and its ligands are abundant in the skin. Their nature (endogenous or exogenous sources) determines the phenotypic responses [82]. Solar UVB radiation generates the AhR endogenous ligand from trypthophan called 6-formylindolo[3,2-b]carbazole (FICZ) in the skin. FICZ promotes melanin pigmentation and improves DNA protection [84], similar to melanin [85]. AhR, being a sensor of environment–skin interactions, plays a crucial role in responses to (photo)pollution. Various air pollutants and tobacco smoke contain many synthetic exogenous ligands with very high affinity to AhR, which some used to call the “dioxin-receptor” [86]. PAHs (such as BaP) and dioxins from pollutants are capable of binding and triggering the AhR canonical signaling pathway. Once activated, AhR is translocated to the nucleus, where it dimerizes with the AhR nuclear transporter (ARNT). The protein complex AhR/ARNT binds to the xenobiotic-responsive element (XRE) in promoter regions and then induces the transcription of AhR-responsive genes, such as cytochrome P450 1A1 (CYP1A1) [87]. After the interaction with canonic XRE, AhR is transported back into the cytosol and its ligands are metabolized by CYP1A1. This action of CYP1A1 is linked to the production of a large number of ROS and mutagenic PAH metabolites, which may damage proteins and DNA. Therefore, the canonical pathway activated by AhR may be responsible for premature skin aging, skin cancer, and the inhibition of apoptosis. AhR also promotes the transcription of its own AhR repressor (AhRR) allowing negative feedback regulation [88]. On the other hand, there are opposite data and concepts showing that the activation of AhR can induce anti-oxidative and anti-inflammatory responses and that it can regulate epidermal barrier functions and exhibit anticancerogenic activity [89,90,91,92]. Furthermore, there is a growing body of evidence that the AhR is also a receptor for several compounds such as vitamin D3 hydroxyderivatives [93,94,95], and diverse beneficial effects of active forms of vitamin D are widely recognized.
The altered redox homeostasis from air pollution initiates downstream signaling cascades interplaying between inflammation and oxidative stress products, thus contributing to a vicious circle of skin oxinflammation. Depending on the ligand and context, AhR can generate an oxidative stress response, enhanced expression of pro-inflammatory genes, and apoptotic cell death [96,97,98]. Pollutant-activated AhR can trigger the production of inflammatory and immunosuppressive cytokines in cutaneous keratinocytes and fibroblasts. In vitro studies have demonstrated that airborne fine particles dose-dependently enhanced the release of interleukin-6 (IL-6), IL-8, IL-1α, and IL-1β in the skin [64,65,70,97]. Similarly, BaP from cigarette smoke can induce oxidative stress-associated IL-1α in adults [99] and IL-8 production in human epidermal keratinocytes via the AHR signaling pathway [100]. This study supports the clinical observations that smoking exacerbates IL-8-related inflammatory skin diseases, such as acne and palmoplantar pustulosis [101,102].
PMs and O3 can cause the upregulation of cyclooxygenase-2 (COX-2) expression and the activation of nuclear factor kappa beta (NF-κβ) in keratinocytes and fibroblasts [97,98,103]. The redox-sensitive transcription factor NF-κβ might be additionally connected to a noncanonical AhR inflammatory pathway (interacts directly with AhR in the absence of AhR/ARNT activity) [104]. After binding to AhR, urban PMs can stimulate the phosphorylation of extracellular signal-regulated kinases (ERK)/p38 mitogen-activated protein kinases (MAPKs) and transcription factor c-Jun-N-terminal kinase (JNK) signaling via the nicotinamide adenine dinucleotide phosphate (NADPH)-oxidase (NOX)-generated ROS. It was proposed that NOX/ROS-dependent mechanisms could induce NF-κβ activation and phosphorylation of activator protein-1 (AP-1) [105]. After PM exposure, the phosphorylated dimers of the AP-1 transcription factor, c-Jun, and c-Fos, as well as the p38 kinase, regulate the transcription of IL-1α and IL-1β genes in human keratinocytes [97,105]. Moreover, the activation of p65 (a subunit of NF-κβ) and c-Jun/c-Fos contribute to a significant upregulation of COX-2 expression and PGE2 production induced by PMs [98,105]. In addition to COX-2, IL-1α and IL-1β are capable of regulating matrix metalloproteinase-1 (MMP-1) expression. In an in vitro co-culture model of human keratinocytes and fibroblasts, it was assumed that after PM treatment, keratinocyte-derived IL-1α/1β would increase the levels of MMP-1 and COX-2 in the fibroblasts [97]. Likewise, tobacco smoke extracts can induce MMP-1 mRNA expression in vitro in human skin cells in a dose-dependent manner [106]. Moreover, using a 3D skin model, consisting of an epidermis without a dermis, Lecas S. et al. (2016) demonstrated the noxious effect of tobacco smoke (containing both PM and gas) that resulted in the significant production of inflammatory cytokines (IL-8, IL-1α, IL-18) and MMPs (MMP-1 and MMP-3), as well as an increase in the 4HNE level [107]. The activation of ERK and MAPK p38 from air pollutants and cigarette smoke favor inflammation-induced degradation of the extracellular matrix (ECM) and downregulation of neocollagenesis. MMPs can fully degrade collagen and elastin fibers, thus decreasing the skin’s viscoelasticity. MMP-1 (collagenase) is the major collagenolytic enzyme that contributes to the breakdown of ECM of the skin tissue, primarily initiating the fragmentation of type I and III collagens. Once cleaved by MMP-1, collagen can be further degraded by both MMP-3 and MMP-9 [108]. At the same time, cigarette smoke and air pollutants impair the biosynthesis of collagen types III, IV, and VII, as well as induce the neosynthesis of abnormal elastin fibers [106]. These alterations are responsible for wrinkle formation and premature skin aging [109,110].
The AhR can also contribute to the modulation of growth factors such as epidermal growth factor (EGF) and transforming growth factor-β (TGF-β). EGF is involved in cell differentiation and proliferation. PAHs-induced AhR activation can cause a decrease in skin cell proliferation together with the apoptosis of keratinocytes and fibroblasts [111]. In addition, the treatment of keratinocytes with 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) significantly accelerates the rate of terminal differentiation and cornification [112,113]. EGF through the EGF receptor (EGFR) mediates the opposing effects on gene transcription and cell differentiation in comparison to the TCDD-induced AhR activation in human keratinocytes [112]. On the other hand, active TGF-β plays an essential role in epidermal homeostasis and dermal growth. PAHs, including those in cigarette smoke, have induced the non-functional latent form of TGF-β and the downregulation of the TGF-β1 receptor. These data are consistent with the observations of smoking-associated premature skin aging through the impairment of ECM protein synthesis [114].
Environmental air pollutants exert an important impact on skin quality. Airborne PMs, O3, smoking, VOCs, NO2, and UVR are capable of increasing trans-epidermal water loss (TEWL) and compromising the epidermal barrier function and structural integrity of the skin, which in turn induce or exacerbate various skin diseases [115,116]. In keratinocytes, PMs downregulate the expression of genes of terminal differentiation markers such as filaggrin (FLG) by their COX-2/PGE2 oxidative potential [105]. Filaggrin contributes to the formation of the corneal layer, thus playing an essential role in the barrier function of the skin. Additionally, a tobacco smoke-exposed reconstructed epidermis model showed even slight exposure triggered drastically decreased expression of both types of epidermal structural genes, those encoding cell–cell adhesion (desmoglein 1 (DSG1), desmocollin 1 (DSC1), and corneodesmosin (CDSN)) and terminal differentiation genes (filaggrin (FLG), loricrin (LOR), involucrin (IVL), etc.), and their corresponding proteins. Consequently, skin architecture can be modified by cigarette smoke, exhibiting poor cohesion of the epidermal barrier and accelerated desquamation and cornification [107]. The crucial role of the AhR signaling pathway for skin barrier integrity can be seen in AhR-knockout mice, which display weaker intercellular connectivity in keratinocytes and express lower expression levels of genes associated with the skin barrier function [117].
While we have focused on pollutant-induced AhR signaling pathways’ involvement in epidermal barrier defects, alteration in epidermal cell differentiation and proliferation, hypopigmentation, and the increased production of proinflammatory cytokines, we must also emphasize the opposite effects, e.g., building the epidermal barrier, anti-inflammatory, antioxidative, and anticancer activities, and defining the Yin and Yang mechanism of action of the AhR, which will be dependent on the nature of the ligand and the cellular and biochemical context (Figure 2).
Figure 2.
AhR signaling pathways’ activation and the cutaneous response to air pollutants and smoking. Negative (Yin) and positive (Yang) effects of AhR activation on the skin are marked by black and white arrows, respectively.
2.4. Pollution Affects Vitamin D Production in the Skin
Air photo(pollution), environmental chemicals, and smoking can be important factors for vitamin D deficiency [118]. PMs and O3 can directly affect the cutaneous production of vitamin D [118]. In addition, air pollutants, persistent organic pollutants, and heavy metals can behave as endocrine-disrupting chemicals (EDCs), which may alter vitamin D-hydroxyderivatives levels [119]. Other environmental factors, such as the winter season, inadequate sun exposure, and a high-latitude location, can also predispose one to vitamin D deficiency [120,121]. Exposure to UVB rays accounts for more than 90% of vitamin D production in humans [48,122,123]. Air pollution also affects vitamin D synthesis by reducing UVB energy reaching the surface of the Earth, which is essential for the production of vitamin D3, tachysterol (T3), and lumisterol (L3) derivatives [49,124,125,126]. It should be noted that exposure to air pollutants during the gestational period can decrease vitamin D levels in newborns [127]. The absorption/scattering of UVB radiation caused by tropospheric ozone and PMs is becoming a real concern for human health [128]. The skin serves not only as a primary place for vitamin D3 production but also as a target organ for its action, which is vital in the formation of the skin barrier and hair follicles [125]. Moreover, vitamin D deficiency has been connected to many inflammatory, proliferative, and malignant skin disorders [129,130,131,132]. There is growing experimental evidence demonstrating the photoprotective properties of vitamin D3 and L3 hydroxyderivatives [133,134,135,136,137,138,139]. The classical and novel forms of vitamin D also impact the development and progression of melanoma and non-melanoma skin cancers [140,141,142,143,144,145].
3. Pollution-Induced Skin Pathologies
3.1. Premature Skin Aging
Skin aging is a process driven by the total exposure of both intrinsic and extrinsic factors over the human lifespan (skin exposome), which is responsible for progressive morphological and functional cutaneous alterations [146,147,148]. The most prominent external stressors for the skin, which can result in premature aging, include UVR [149,150], air pollutants [110,151,152], and smoking [153]. They predominantly affect parts exposed to the environment such as the face, head, neck, and back of the hands. Moreover, chronic photopollution exposure of the skin may accelerate the photoaging process and can correlate with enhanced cancer risk [31,154].
The endogenous antioxidant cutaneous capacity decreases with aging, making aged skin more vulnerable to environmental insults. Indeed, human skin aging is primarily induced by oxidative events. In particular, extensive ROS production and insufficient scavenging activity or mitochondrial dysfunction are crucial for premature skin aging [155,156,157]. O3 from smog and PM can trigger ROS generation and induce oxidative stress, contributing to phenotypic features of aging. O3 primarily causes wrinkles formation [148,158], while long-term exposure to fine PM and NO2 is responsible for pigment spots (lentigines) [159] and deep nasolabial folds [160]. Currently, the habit of smoking is considered an aging accelerator, and it is an even greater contributor to facial wrinkling than sun exposure [161,162]. Smoking also increases keratinocyte dysplasia and skin roughness and increases the risk of the development of pathological elastosis [153]. Moreover, long-term secondhand-smoke exposure could also affect skin appearance as shown in a premature skin aging rat model [163].
Cigarette smoke and PMs contain numerous PAHs that trigger premature skin aging via an AhR pathway [164]. Activated AhR can subsequently initiate ERK/MAPK signaling pathways and upregulate the expression of aging-related genes [111]. MMP-1, which degrades collagen, is induced dose-dependently by tobacco smoke extracts in human fibroblasts and keratinocytes through AhR activation [106]. Similarly, in primary human dermal fibroblasts exposed to different concentrations of PMs, the expression of MMP-1, MMP-3, and TGF-β significantly increased and showed changes associated with skin aging [165]. Indeed, senescent fibroblasts are characterized by increased levels of MMP secretion. In addition, PM10 may contribute to premature skin aging and skin inflammation via impaired collagen synthesis [166].
3.2. Skin Cancers
Solar UVR is the primary etiological factor responsible for skin cancer development. It is found that SCC and BCC are dependent on the total dose of UVR exposures, while cutaneous melanoma is also dependent on exposure patterns, with intermittent irradiation being the most harmful [167]. During the last few decades, humans worldwide have been facing the adverse influence of climate change and stratospheric ozone depletion, which are becoming a public health concern [168]. The changes to the O3 layer resulted from global industrialization and ambient pollution, which allow an increased proportion of UVB irradiation to reach the Earth’s surface. This depletion of the O3 layer can impact the dual effects of UVR on skin health [26,169] and likely enhance the risk of skin cancer. Every 1% of O3 layer reduction would increase UVB irradiation by 2%, which may result in a 1 to 2% increase in cutaneous melanoma and a 3 to 4.6% increase in SCC incidence [170]. Nonmelanoma skin cancer (SCCs and BCCs) is the most common type of human cancer, primarily affecting white-skinned individuals. Importantly, the incidences of both melanoma and non-melanoma skin tumors are increasing worldwide [171].
Ambient air pollution alone or simultaneously with UVR may play a crucial role in skin cancer emergence. Many air pollutants are potentially cancerogenic. Among these pollutants, PM10 is believed to be linked to enhanced cancer development of the skin, larynx, lungs, thyroid gland, and bladder. Moreover, it was established that a 10 µg/m3 increase in the PM10 concentration was associated with a 52% higher relative risk of nonmelanoma skin tumors [172]. Moreover, UFPMs including black carbon and PAHs increase the incidence of skin cancer [173]. BaP and other PAHs are photoreactive, and their potential cancerogenic risk seems to be aggravated by UVA radiation [21,174]. In addition, the higher risk of developing SCCs in smokers [175] is mostly attributed to the carcinogen BaP, present as one of the main constituents of cigarette smoke [176]. In the presence of PUFAs (e.g., in biomembranes), BaP undergoes oxidative transformations and the products of BaP oxidation and lipid peroxidation exhibit mutagenic potential and may induce cancerogenesis [177,178].
Chronic exposure of the skin to PAHs and/or UVR may activate the AhR transcription factor and promote downstream epidermal targets, contributing to skin cancerogenesis [179,180]. Other AhR ligands have the potential to increase PAH toxicity through the induction of the CYP1A1 gene. The interaction of pollutants with AhR can induce pro-oxidative mechanisms and oxidative stress-induced genotoxicity [181]. Enhanced ROS formation and reduced antioxidant defense can be correlated with DNA damage, mutations, and cancerogenesis. The critical role of AhR in PM- or BaP-induced cancerogenesis has been indicated by the lack of skin tumors in AhR(−/−) mice continuously exposed to airborne PM or BaP. In this setting, tumor development in AhR(+/+) mice was mediated via CYP1A1 expression induced by PAHs [182,183]. In addition, mice with Langerhans cells (LCs) deletion were protected from cancerogenesis, independent of T cell immunity. LC-deficient mice skin has shown relatively strong resistance to cancer development. LCs, which are skin-specific dendritic cells, metabolize PAHs into a pro-oncogenic intermediate, which increases mutagenesis and facilitates epidermal DNA damage and SCC formation [184].
3.3. Atopic Dermatitis
Atopic dermatitis (AD) is a chronic inflammatory cutaneous disease affecting up to 20% of children and 10% of adults, which is growing globally with prevalence in industrialized countries [185,186]. This disorder has a complex pathogenesis that relies on environmental and genetic factors, epidermal barrier dysfunction, immune dysregulation, cutaneous and gut dysbiosis, and food sensitization [187,188]. Air pollutants, especially those due to industrialization and wildfires, could be independent factors related to increased risk for the development or exacerbation of AD lesions and symptoms in both children and adults [189,190,191]. Moreover, prenatal exposure to PMs (PM2.5 and PM10) and NO2, especially during the first trimester, was linked to a higher risk of infantile AD [192,193,194]. Moreover, smoking, both active and passive, positively correlates with adult AD prevalence [195,196,197]. Several studies have demonstrated that NO2, VOCs, and formaldehyde can increase trans-epidermal water loss (TEWL), which may result in skin barrier damage [198,199,200] and hypersensitization to aeroallergens leading to systemic allergic responses [201,202]. On the other hand, epidermal barrier disruption, especially in AD children’s skin, allows the intracellular penetration of PMs. Repeated PM exposure can cause thickening of the epidermis and dermal inflammation with neutrophil infiltration [203]. Additionally, it was established that the effects of atmospheric particles of various sizes and gaseous air pollutants (e.g., NO2, SO2) on atopic skin could be augmented by meteorological factors, especially dry conditions and high temperatures [204,205]. Furthermore, environmental stressors, including airborne pollutants, may change the skin microbiome composition, thus influencing the epidemiology and severity of AD [206]. It was well documented that AD lesional skin with abnormal cutaneous barrier possesses abundant colonization of Staphylococcus aureus, Corynebacterium, etc. species, which further exacerbate T helper 2 (Th2)-deviated skin inflammation [207].
In vivo and in vitro studies showed that air pollutants contribute to the development and flares of lesions and symptoms of AD via the activation of AhR signaling pathways, promoting oxidative stress, triggering a proinflammatory response, and impairing the skin’s barrier function [208,209]. For example, in an AD mouse model, PM10 application induced/aggravated cutaneous inflammation through differential expression of genes encoding skin barrier integrity and immune responses [210]. At the molecular level, it was found that AD lesions exhibited an elevated expression of AhR and ARNT [211]. Furthermore, the levels of AhR in the serum of patients with AD increased compared to healthy individuals. AhR mRNA expression positively correlates with the severity index score of the disorder and the concentration of IL-6 in the serum of AD patients [212]. Cigarette smoke can additionally affect atopic sensitization via the BaP–AhR interaction. This interaction further causes immune responses including T-cell polarization and LCs migration [213]. In chronically inflamed skin such as in AD, increased levels of noncanonical AhR-partner molecules, such as NF-κB and the signal transducer and activator of transcription-3 (STAT-3), are noted [104].
The activation of AhR in human keratinocytes by air pollutants can induce elevated expression of the neurotrophic factor artemin (ARTN) in the epidermis of patients with AD but not in healthy people [214]. Recently, Hidaka et al. also studied the expression of Arnt in mice expressing constitutively active AHR in keratinocytes (AHR-CA). Those AhR-CA mice overexpress Artn, which, as a target gene of AhR, can induce substantial pruritus during the chronic presence of PAHs, as evaluated by continuous scratching behavior [214].
3.4. Psoriasis
Psoriasis is a common (2–3% worldwide prevalence) chronic inflammatory skin disease with systemic involvement. As an immune-mediated disorder, Th17 cells and IL-17 play a crucial role in its pathogenesis [215]. It is thought that short-term exposure to ambient air pollution may be a trigger factor for psoriasis flares [216,217]. Moreover, cigarette smoke may increase the severity of psoriasis in a dose-dependent manner [218]. Airborne pollutants such as PMs [219] and O3 [220] may play an essential role in Th17 differentiation in an AhR-dependent manner [220,221]. The AhR and ARNT are found co-localized at the lower layer of the epidermis in acute psoriatic lesions, which also suggests the activation of AhR pathways [205]. Moreover, modulated by AhR, autophagy can lead to skin inflammation in human keratinocytes via the p65NF-κβ/p38MAPK signaling pathways, suggesting that AhR signaling and autophagy may contribute to psoriasis-related inflammation [222].
3.5. Acne
Acne vulgaris is a common inflammatory skin disease involving the pilosebaceous unit, with multifactorial etiology where an exposome [223] along with increased sebum production due to hormonal stimulation and genetic factors are very important etiologic factors [224,225]. Ambient pollution is considered one of the exposome factors of the skin. Acne could be either aggravated or developed in highly polluted areas. A relationship between air pollutants and increased acne prevalence has been established [226]. In studies with Chinese subjects, it was found that cutaneous exposure to increased levels of PMs (PM2.5 and PM10) and NO2 were significantly associated with a higher number of acne lesions and increased sebum production (hyperseborrhoea) [226] that resulted in more outpatient visits [227]. Notably, increased concentrations of SO2 showed a negative correlation with the number of acne-related daily visits [227]. This is in accordance with the use of sulfur-containing topical combinations for the treatment of acne vulgaris. Another study demonstrated age- and gender-related effects of short-term exposure to air pollutants on the skin and the risk of increased outpatient visits for teenage and adult acne. [228]. Both SO2 and NO2 were found positively correlated with acne presentation in men and women. SO2 was found to be associated with increased acne visits only in children and young adults in this study, whereas NO2 corresponded to increased acne visits in all age groups [228]. In addition, types of food could affect acne presentation.
The exact mechanism of acne formation in the presence of air pollutants is still not fully clarified. As we discussed above (Section 2.2), air pollution inducing oxidative stress in the skin can cause lipid peroxidation, the carbonylation of proteins, and oxidative DNA damage. Human sebum produced by sebaceous glands during the life cycle of sebocytes is a mixture of triglycerides, wax esters, and squalene. Sebum secretion fuels the lipophilic resident cutaneous flora, primarily comprising Propionibacterium acnes, Staphylococci, and Malassezia species [229]. O3, cigarette smoke, and long UVA rays exhibit the powerful (photo)oxidizing potential of squalene [24,78]. In particular, the overlying lipids on the corneal layer of the epidermis can be modified by air pollutants with increased levels of peroxidized forms of squalene and decreased levels of linoleic acid, thus promoting comedogenesis [78,230]. Moreover, hyperseborrhea and dysseborrhea, which are important etiopathogenetic factors in acne [231], were measured on the forehead of citizens in two highly polluted cities, namely Shanghai and Mexico City [79,232].
Outdoor air pollution could also trigger inflammation of the skin and stimulate the occurrence of inflammatory acne lesions [233]. PAH-activated AhR may further induce skin inflammation via the heightened production of pro-inflammatory cytokines from epidermal keratinocytes such as IL-1α [97,99] and IL-8 [100]. Both cytokines are more prominent in inflamed acne lesions than in normal skin, demonstrating their contribution to the exacerbation of acne [99,230,234]. The colonization of Propionibacterium acnes in areas of the skin with hyperseborrhea additionally drives inflammatory responses in acne vulgaris [235].
In addition, exposure to a high concentration of dioxins via inhalation, ingestion, and transcutaneous absorption induces chloracne, which is classified as an occupational dermatosis [236]. Dioxins have been found to be very potent ligands of AhR and promote accelerated terminal differentiation and hyperkeratinization of the epidermis, and convert sebocytes towards a keratinocytic differentiation lineage, which can result in acneiform eruptions [237].
3.6. Melasma and Other Hyperpigmentations
Melanogenesis and pigmentation are vital in photoprotective responses against DNA damage in epidermal keratinocytes [238]. In fact, photoprotection by tanning can occur even without UVB exposure [239].
AhR is a pleiotropic sensor of environmental factors. UVB-induced, FICZ-mediated activation of AhR is essential for the protection of DNA. Moreover, it was confirmed that AHR-deficient mice exhibit significantly weaker skin tanning in comparison with wild-type mice [84]. The activation of AhR/MAPK signaling in melanocytes in response to other ligands present in air pollutants (PAH, dioxins) promotes the proliferation of melanocytes and stimulates melanogenesis by upregulating the expression of melanogenic enzymes, which leads to hyperpigmentation and the appearance of pigmented spots on the skin [237,240,241].
3.7. Hair Loss
Airborne pollutants such as PMs, VOCs, NOx, and carbon oxides (CO and CO2) may be deposited on the hair and scalp or penetrate into the deeper layer of the skin via hair follicles or transcutaneous absorption [242]. Urban PM nanoparticles were observed inside hair follicles in both intact and barrier-disrupted skin in vivo [203]. Absorbing PAH on their surface, PMs from air pollution may trigger ROS generation and ROS-dependent inflammatory responses in the skin, which may further result in hair shedding [242]. Other data demonstrate that PMs may induce keratinocytes’ apoptosis in ex vivo cultured scalp hair follicles that could impair hair growth [243]. In addition, tobacco smoke containing PAHs is recognized as an oxidizing agent and is implicated in early-onset androgenetic alopecia in men [244]. Similarly, in an animal model, most C57BL/6 mice exposed to cigarette smoke for 3 months developed areas of alopecia and grey hair. The smoke-treated mice skin showed atrophic skin, reduced thickness of the subcutaneous tissue, a scarcity of hair follicles, and massive apoptosis of hair bulb cells at the alopecia edges [245].
4. Preventive and Treatment Options for Air Pollutant-Damaged Skin
4.1. Anti-Pollution Skin Care Strategies
The noxious effects of pollution on the skin with potentially systemic implications stirred interest in developing effective anti-pollution skincare and haircare products [246]. The main preventive and therapeutic strategies against air pollution-driven skin damage should include control of the deposition and penetration of air pollutants through the skin and hair follicles and their removal, repairing skin barrier function and improvement of hydration, control of pigmentation, reduction of oxinflammation by using antioxidants, and the prevention of collagen and elastin degradation [3,11].
The basic pollution protective measures involve the use of protective clothing, rinsing products to wash away the pollutants from the skin (but not overwashing), and barrier creams to preserve or restore the skin barrier [246,247]. Sun protection is essential for the prevention of photo-reactive compounds to cause photopollution skin damage. Therefore, products with broad-spectrum (UVA + UVB) sun protection, sunscreens with the addition of antioxidants (vitamin E, ferulic acid, etc.), and sunscreens and after-sun lotions containing DNA repair enzymes are a promising strategy against cutaneous photodamage [248,249,250]. Additionally, sunscreen with mineral filters containing pigments such as iron oxide and titanium dioxide could be helpful for melasma prevention [251].
Plants extracts and other natural compounds with powerful antioxidant activity can protect and treat air-pollution-related oxidative damage to the skin [63,252,253]. Of note, a comprehensive topical antioxidant mixture (WEL-DS) that combines 19 water-soluble, lipid-soluble, and enzymatic antioxidants, designed to protect skin from the oxidizing effects of UVR and to reduce the visible signs of facial photodamage [254], has diminished oxidative stress promoted by blue light and cigarette smoke exposure [63], as well as the ambient O3-induced oxidative damage in a reconstructed skin model [255].
Another potential candidate for the attenuation or treatment of (photo)pollution-triggered cutaneous damage is melatonin [256,257]. Melatonin, being both synthesized and metabolized in the skin, together with most of its metabolites, works as a potent antioxidant that possesses the capacity to reduce oxidative damage, protect mitochondrial functions, reduce inflammation, and modulate the immune system in the skin [42,258,259,260,261]. It should be noted that melatonin’s antioxidant cascade directly detoxifies many harmful radicals (hydroxyl radical and peroxynitrite), which are not degraded by enzymes in comparison with a single radical scavenge by classical antioxidants (vitamins C and E) [262,263,264]. Melatonin may additionally activate antioxidant enzymes, which are able to degrade the weakly reactive ROS [265,266]. Additionally, melatonin is capable of stimulating SIRT1, which plays an important role in pollution-associated premature skin aging. Thus, the upregulation of SIRT1 could downregulate MMP-1 and MMP-3, which contribute to collagen breakdown and could decrease inflammation via NF-κβ signaling [267]. The (photo)protective potential of topically applied exogenous melatonin has been demonstrated by many studies. For example, the application of night cream containing melatonin, carnosine, and extracts of the Mediterranean flowering plant Helichrysum italicum on skin explants pre-exposed to a mixture of PAHs and heavy metals showed a reduction of the cutaneous irritation and damage, and a significant increase in collagen type I [268]. Moreover, melatonin could reverse the increased lipid peroxidation and might even improve the skin of former smokers [269]. Therefore, formulating new skincare products with melatonin would be a novel approach to the prevention of oxidative damage on the skin caused by air pollutants, heavy metals, and smoking.
4.2. Modulation of AhR in Air Pollution-Induced Skin Diseases
Only a few specific molecules are currently able to prevent or counteract the noxious effects of ambient air pollutants on the skin. The use of AhR modulators has become a new strategy for anti-pollution skin prevention and therapy. Importantly, some AhR ligands can simultaneously activate the master regulator of the antioxidant responses, nuclear factor erythroid 2-related factor 2 (Nrf2) [96,104]. Other antioxidant phytochemicals (e.g., cinnamon derivatives) could activate Nrf2 and independently block the AhR and inhibit CYP1A1 [237,270,271]. The targeting of AhR/Nrf2 could be a potential candidate strategy in the treatment of air pollution-induced skin diseases. Therapeutics that both downregulate ligand-activated AhR signaling and stimulate the Nrf2 antioxidant system are likely the most promising candidates. The stimulation of the Nrf2 transcription factor further triggers the downstream antioxidative signaling pathway, neutralizing oxidative stress and playing a pivotal role in the cytoprotection of the skin [272,273,274].
Additionally, antioxidative AhR/Nrf2 dual agonists can reduce inflammation via the downregulation of proinflammatory cytokines and can regulate the skin barrier protein expression, improving epidermal barrier function [275,276]. Therefore, AhR/Nrf2 represents a potential therapeutic target in the treatment of inflammatory skin disorders such as atopic dermatitis, psoriasis, and other dermatoses [277,278].
Tapinarof is a novel, naturally derived, small-molecule AhR-modulating therapeutic agent, currently under clinical trials for the treatment of atopic dermatitis and psoriasis [279,280,281]. It specifically binds to and activates AhR in the skin, which inhibits cutaneous inflammation in mice and humans. The topical application of tapinarof cream on imiquimod-induced psoriasiform skin lesions in mice has led to a decrease in the cytokines level, as well as a reduction in epidermal thickening and erythema. In contrast, tapinarof has shown no effect on skin inflammation in AhR-deficient mice [282]. In addition, the significant efficacy of tapinarof in psoriasis is attributed to its downregulation of IL-17 and other pro-inflammatory cytokines. Tapinarof also exhibits antioxidative capacity via the activation of Nrf2 and its downstream antioxidative enzymes and downregulates the phosphorylated signal transducer and the activator of transcription 6 (P-STAT6) formation [283].
Topical tapinarof is a safe and promising agent with the ability to attenuate the development of atopic dermatitis and may also be helpful in the treatment of air-pollution-initiated exacerbation of atopic lesions. Tapinarof-treated NHEKs showed the upregulation of epidermal barrier FLG and LOR genes and protein expression via AHR activation. Tapinarof also enhanced the secretion of IL-24, a cytokine-activating Janus kinase (JAK)- STAT axis, which downregulates the expression of FLG and LOR [284]. It should be noted that IL-24 can be stimulated by certain oxidative AhR agonists such as TCDD, BaP, PMs, and UVB radiation [285].
5. Conclusions
The increased level of air pollution worldwide represents an environmental risk factor for skin damage and the development of cutaneous pathologies. Some PAHs are photoreactive and could be activated upon UVA light. Therefore, such UVR exposure would enhance their deleterious effects on the skin.
AhR is a sensor for small molecules such as air pollutants, which are capable of activating oxidative stress responses and triggering inflammatory and immunosuppressive cytokine production in the skin. On the other hand, targeting AhR/Nrf2 is emerging as a novel treatment option for ambient pollutants that induce or exacerbate inflammatory skin diseases such as atopic dermatitis, psoriasis, etc. Therefore, AhR with downstream regulatory pathways would represent a crucial signaling system regulating the skin phenotype in a Yin-and-Yang fashion defined by the chemical nature of the activating factor and the cellular context.
Author Contributions
Conceptualization and original draft preparation, G.B.; writing the manuscript, extensive editing, and revision of the manuscript, R.M.S. and A.T.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data appear in the manuscript. For further inquiries, please contact the first author or corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The writing was supported in part by NIH grants 1R01AR073004-01A1, R01AR071189-01A1, and R21 AI149267-01A1, by VA merit grant 1I01BX004293-01A1, and DOD grant # W81XWH2210689 to ATS.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Guarnieri M., Balmes J.R. Outdoor air pollution and asthma. Lancet. 2014;383:1581–1592. doi: 10.1016/S0140-6736(14)60617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Bont J., Jaganathan S., Dahlquist M., Persson Å., Stafoggia M., Ljungman P. Ambient air pollution and cardiovascular diseases: An umbrella review of systematic reviews and meta-analyses. J. Intern. Med. 2022;291:779–800. doi: 10.1111/joim.13467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Damevska K., Nikolovska S., Kazandjieva J., Kotevska B., Bocheva G. Skin and pollution. In: França K., Lotti T., editors. Advances in Integrative Dermatology. Wiley, J. & Sons, Ltd.; Hoboken, NJ, USA: 2019. pp. 379–392. [Google Scholar]
- 4.Araviiskaia E., Berardesca E., Bieber T., Gontijo G., Sanchez Viera M., Marrot L., Chuberre B., Dreno B. The impact of airborne pollution on skin. J. Eur. Acad. Dermatol. Venereol. 2019;33:1496–1505. doi: 10.1111/jdv.15583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim H., Kim W.H., Kim Y.Y., Park H.Y. Air Pollution and Central Nervous System Disease: A Review of the Impact of Fine Particulate Matter on Neurological Disorders. Front. Public Health. 2020;8:575330. doi: 10.3389/fpubh.2020.575330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costa L.G., Cole T.B., Dao K., Chang Y.C., Coburn J., Garrick J.M. Effects of air pollution on the nervous system and its possible role in neurodevelopmental and neurodegenerative disorders. Pharmacol. Ther. 2020;210:107523. doi: 10.1016/j.pharmthera.2020.107523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee H.W., Kang S.C., Kim S.Y., Cho Y.J., Hwang S. Long-term Exposure to PM10 Increases Lung Cancer Risks: A Cohort Analysis. Cancer Res. Treat. 2022;54:1030–1037. doi: 10.4143/crt.2021.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lelieveld J., Evans J.S., Fnais M., Giannadaki D., Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525:367–371. doi: 10.1038/nature15371. [DOI] [PubMed] [Google Scholar]
- 9.Real Á.D., Santurtún A., Teresa Zarrabeitia M. Epigenetic related changes on air quality. Environ. Res. 2021;197:111155. doi: 10.1016/j.envres.2021.111155. [DOI] [PubMed] [Google Scholar]
- 10.Grippo A., Zhang J., Chu L., Guo Y., Qiao L., Zhang J., Myneni A.A., Mu L. Air pollution exposure during pregnancy and spontaneous abortion and stillbirth. Rev. Environ Health. 2018;33:247–264. doi: 10.1515/reveh-2017-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koohgoli R., Hudson L., Naidoo K., Wilkinson S., Chavan B., Birch-Machin M.A. Bad air gets under your skin. Exp. Dermatol. 2017;26:384–387. doi: 10.1111/exd.13257. [DOI] [PubMed] [Google Scholar]
- 12.Mathew B.B., Singh H., Biju V.G., Krishnamurthy N.B. Classification, Source, and Effect of Environmental Pollutants and Their Biodegradation. J. Environ. Pathol. Toxicol. Oncol. 2017;36:55–71. doi: 10.1615/JEnvironPatholToxicolOncol.2017015804. [DOI] [PubMed] [Google Scholar]
- 13.Pan T.L., Wang P.W., Aljuffali I.A., Huang C.T., Lee C.W., Fang J.Y. The impact of urban particulate pollution on skin barrier function and the subsequent drug absorption. J. Dermatol. Sci. 2015;78:51–60. doi: 10.1016/j.jdermsci.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 14.Larese Filon F., Mauro M., Adami G., Bovenzi M., Crosera M. Nanoparticles skin absorption: New aspects for a safety profile evaluation. Regul. Toxicol. Pharmacol. 2015;72:310–322. doi: 10.1016/j.yrtph.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 15.Loomis D., Grosse Y., Lauby-Secretan B., El Ghissassi F., Bouvard V., Benbrahim-Tallaa L., Guha N., Baan R., Mattock H., Straif K. International Agency for Research on Cancer Monograph Working Group IARC. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013;14:1262–1263. doi: 10.1016/S1470-2045(13)70487-X. [DOI] [PubMed] [Google Scholar]
- 16.Donaldson K., Tran L., Jimenez L.A., Duffin R., Newby D.E., Mills N., MacNee W., Stone V. Combustion-derived nanoparticles: A review of their toxicology following inhalation exposure. Part. Fibre Toxicol. 2005;2:10. doi: 10.1186/1743-8977-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kwon H.S., Ryu M.H., Carlsten C. Ultrafine particles: Unique physicochemical properties relevant to health and disease. Exp. Mol. Med. 2020;52:318–328. doi: 10.1038/s12276-020-0405-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toriba A., Kuramae Y., Chetiyanukornkul T., Kizu R., Makino T., Nakazawa H., Hayakawa K. Quantification of polycyclic aromatic hydrocarbons (PAHs) in human hair by HPLC with fluorescence detection: A biological monitoring method to evaluate the exposure to PAHs. Biomed. Chromatogr. 2003;17:126–132. doi: 10.1002/bmc.222. [DOI] [PubMed] [Google Scholar]
- 19.Hearn B.A., Ding Y.S., Watson C.H., Johnson T.L., Zewdie G., Jeong-Im J.H., Walters M.J., Holman M.R., Rochester C.G. Multi-year Study of PAHs in Mainstream Cigarette Smoke. Tob. Regul. Sci. 2018;4:96–106. doi: 10.18001/TRS.4.3.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Appenzeller B.M., Mathon C., Schummer C., Alkerwi A., Lair M.L. Simultaneous determination of nicotine and PAH metabolites in human hair specimen: A potential methodology to assess tobacco smoke contribution in PAH exposure. Toxicol. Lett. 2012;210:211–219. doi: 10.1016/j.toxlet.2011.11.022. [DOI] [PubMed] [Google Scholar]
- 21.Dimitrov A., Zanini M., Zucchi H., Boudah S., Lima J., Soeur J., Marrot L. Vitamin C prevents epidermal damage induced by PM-associated pollutants and UVA1 combined exposure. Exp. Dermatol. 2021;30:1693–1698. doi: 10.1111/exd.14315. [DOI] [PubMed] [Google Scholar]
- 22.Guerreiro C.B.B., Horálek J., de Leeuw F., Couvidat F. Benzo(a)pyrene in Europe: Ambient air concentrations, population exposure and health effects. Environ. Pollut. 2016;214:657–667. doi: 10.1016/j.envpol.2016.04.081. [DOI] [PubMed] [Google Scholar]
- 23.von Koschembahr A., Youssef A., Béal D., Gudimard L., Giot J.P., Douki T. Toxicity and DNA repair in normal human keratinocytes co-exposed to benzo[a]pyrene and sunlight. Toxicol. In Vitro. 2020;63:104744. doi: 10.1016/j.tiv.2019.104744. [DOI] [PubMed] [Google Scholar]
- 24.Thiele J.J., Traber M.G., Tsang K., Cross C.E., Packer L. In vivo exposure to ozone depletes vitamins C and E and induces lipid peroxidation in epidermal layers of murine skin. Free Radic. Biol. Med. 1997;23:385–391. doi: 10.1016/S0891-5849(96)00617-X. [DOI] [PubMed] [Google Scholar]
- 25.Valacchi G., Pecorelli A., Belmonte G., Pambianchi E., Cervellati F., Lynch S., Krol Y., Oresajo C. Protective Effects of Topical Vitamin C Compound Mixtures against Ozone-Induced Damage in Human Skin. J. Investig. Dermatol. 2017;137:1373–1375. doi: 10.1016/j.jid.2017.01.034. [DOI] [PubMed] [Google Scholar]
- 26.Slominski A.T., Zmijewski M.A., Plonka P.M., Szaflarski J.P., Paus R. How UV Light Touches the Brain and Endocrine System Through Skin, and Why. Endocrinology. 2018;159:1992–2007. doi: 10.1210/en.2017-03230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bernerd F., Passeron T., Castiel I., Marionnet C. The Damaging Effects of Long UVA (UVA1) Rays: A Major Challenge to Preserve Skin Health and Integrity. Int. J. Mol. Sci. 2022;23:8243. doi: 10.3390/ijms23158243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Battie C., Jitsukawa S., Bernerd F., Del Bino S., Marionnet C., Verschoore M. New insights in photoaging, UVA induced damage and skin types. Exp. Dermatol. 2014;23:7–12. doi: 10.1111/exd.12388. [DOI] [PubMed] [Google Scholar]
- 29.Marionnet C., Tricaud C., Bernerd F. Exposure to non-extreme solar UV daylight: Spectral characterization, effects on skin and photoprotection. Int. J. Mol. Sci. 2014;16:68–90. doi: 10.3390/ijms16010068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burns E.M., Ahmed H., Isedeh P.N., Kohli I., Van Der Pol W., Shaheen A., Muza_ar A.F., Al-Sadek C., Foy T.M., Abdelgawwad M.S., et al. Ultraviolet radiation, both UVA and UVB, influences the composition of the skin microbiome. Exp. Dermatol. 2019;28:136–141. doi: 10.1111/exd.13854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Soeur J., Belaïdi J.P., Chollet C., Denat L., Dimitrov A., Jones C., Perez P., Zanini M., Zobiri O., Mezzache S., et al. Photo-pollution stress in skin: Traces of pollutants (PAH and particulate matter) impair redox homeostasis in keratinocytes exposed to UVA1. J. Dermatol Sci. 2017;86:162–169. doi: 10.1016/j.jdermsci.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 32.Nakashima Y., Ohta S., Wolf A.M. Blue light-induced oxidative stress in live skin. Free Radic. Biol. Med. 2017;108:300–310. doi: 10.1016/j.freeradbiomed.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 33.Dong K., Goyarts E.C., Pelle E., Trivero J., Pernodet N. Blue light disrupts the circadian rhythm and create damage in skin cells. Int. J. Cosmet. Sci. 2019;41:558–562. doi: 10.1111/ics.12572. [DOI] [PubMed] [Google Scholar]
- 34.Ouyang X., Yang J., Hong Z., Wu Y., Xie Y., Wang G. Mechanisms of blue light-induced eye hazard and protective measures: A review. Biomed. Pharmacother. 2020;130:110577. doi: 10.1016/j.biopha.2020.110577. [DOI] [PubMed] [Google Scholar]
- 35.Li X., Zhu S., Qi F. Blue light pollution causes retinal damage and degeneration by inducing ferroptosis. J. Photochem. Photobiol. B. 2023;238:112617. doi: 10.1016/j.jphotobiol.2022.112617. [DOI] [PubMed] [Google Scholar]
- 36.Campiche R., Curpen S.J., Lutchmanen-Kolanthan V., Gougeon S., Cherel M., Laurent G., Gempeler M., Schuetz R. Pigmentation effects of blue light irradiation on skin and how to protect against them. Int. J. Cosmet. Sci. 2020;42:399–406. doi: 10.1111/ics.12637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mancebo S.E., Wang S.Q. Recognizing the impact of ambient air pollution on skin health. J. Eur. Acad. Dermatol. Venereol. 2015;29:2326–2332. doi: 10.1111/jdv.13250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abolhasani R., Araghi F., Tabary M., Aryannejad A., Mashinchi B., Robati R.M. The impact of air pollution on skin and related disorders: A comprehensive review. Dermatol. Ther. 2021;34:e14840. doi: 10.1111/dth.14840. [DOI] [PubMed] [Google Scholar]
- 39.Slominski A.T., Zmijewski M.A., Skobowiat C., Zbytek B., Slominski R.M., Steketee J.D. Sensing the environment: Regulation of local and global homeostasis by the skin’s neuroendocrine system. Adv. Anat. Embryol. Cell Biol. 2012;212:1–115. doi: 10.1007/978-3-642-19683-6_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zouboulis C.C. Human skin: An independent peripheral endocrine organ. Horm. Res. 2000;54:230–242. doi: 10.1159/000053265. [DOI] [PubMed] [Google Scholar]
- 41.Slominski A., Wortsman J. Neuroendocrinology of the skin. Endocr. Rev. 2000;21:457–487. doi: 10.1210/er.21.5.457. [DOI] [PubMed] [Google Scholar]
- 42.Slominski A., Wortsman J., Tobin D.J. The cutaneous serotoninergic/melatoninergic system: Securing a place under the sun. FASEB J. 2005;19:176–194. doi: 10.1096/fj.04-2079rev. [DOI] [PubMed] [Google Scholar]
- 43.Slominski A.T., Kim T.K., Kleszczyński K., Semak I., Janjetovic Z., Sweatman T., Skobowiat C., Steketee J.D., Lin Z., Postlethwaite A., et al. Characterization of serotonin and N-acetylserotonin systems in the human epidermis and skin cells. J. Pineal Res. 2020;68:e12626. doi: 10.1111/jpi.12626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Slominski A., Zbytek B., Nikolakis G., Manna P.R., Skobowiat C., Zmijewski M., Li W., Janjetovic Z., Postlethwaite A., Zouboulis C.C., et al. Steroidogenesis in the skin: Implications for local immune functions. J. Steroid Biochem. Mol. Biol. 2013;137:107–123. doi: 10.1016/j.jsbmb.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Slominski A.T., Slominski R.M., Raman C., Chen J.Y., Athar M., Elmets C. Neuroendocrine signaling in the skin with a special focus on the epidermal neuropeptides. Am. J. Physiol. Cell Physiol. 2022;323:C1757–C1776. doi: 10.1152/ajpcell.00147.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Slominski A., Wortsman J., Kohn L., Ain K.B., Venkataraman G.M., Pisarchik A., Chung J.H., Giuliani C., Thornton M., Slugocki G., et al. Expression of hypothalamic-pituitary-thyroid axis related genes in the human skin. J. Investig. Dermatol. 2002;119:1449–1455. doi: 10.1046/j.1523-1747.2002.19617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Slominski A., Wortsman J., Pisarchik A., Zbytek B., Linton E.A., Mazurkiewicz J.E., Wei E.T. Cutaneous expression of corticotropin-releasing hormone (CRH), urocortin, and CRH receptors. FASEB J. 2001;15:1678–1693. doi: 10.1096/fj.00-0850rev. [DOI] [PubMed] [Google Scholar]
- 48.Holick M.F. Ultraviolet B Radiation: The Vitamin D Connection. Adv. Exp. Med. Biol. 2017;996:137–154. doi: 10.1007/978-3-319-56017-5_12. [DOI] [PubMed] [Google Scholar]
- 49.Slominski A., Kim T.K., Zmijewski M.A., Janjetovic Z., Li W., Chen J., Kusniatsova E.I., Semak I., Postlethwaite A., Miller D.D., et al. Novel vitamin D photoproducts and their precursors in the skin. Dermatoendocrinology. 2013;5:7–19. doi: 10.4161/derm.23938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Slominski A.T., Kim T.K., Li W., Yi A.K., Postlethwaite A., Tuckey R.C. The role of CYP11A1 in the production of vitamin D metabolites and their role in the regulation of epidermal functions. J. Steroid Biochem. Mol. Biol. 2014;144:28–39. doi: 10.1016/j.jsbmb.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Charoenngam N., Holick M.F. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients. 2020;12:2097. doi: 10.3390/nu12072097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roosterman D., Goerge T., Schneider S.W., Bunnett N.W., Steinhoff M. Neuronal control of skin function: The skin as a neuroimmunoendocrine organ. Physiol. Rev. 2006;86:1309–1379. doi: 10.1152/physrev.00026.2005. [DOI] [PubMed] [Google Scholar]
- 53.Luger T.A., Paus R., Slominski A., Lipton J. The proopiomelanocortin system in cutaneous neuroimmunomodulation. An introductory overview. Ann. N. Y. Acad. Sci. 1999;885 doi: 10.1111/j.1749-6632.1999.tb08661.x. [DOI] [PubMed] [Google Scholar]
- 54.O’Sullivan R.L., Lipper G., Lerner E.A. The neuro-immuno-cutaneous-endocrine network: Relationship of mind and skin. Arch. Dermatol. 1998;134:1431–1435. doi: 10.1001/archderm.134.11.1431. [DOI] [PubMed] [Google Scholar]
- 55.Slominski A.T., Manna P.R., Tuckey R.C. Cutaneous glucocorticosteroidogenesis: Securing local homeostasis and the skin integrity. Exp. Dermatol. 2014;23:369–374. doi: 10.1111/exd.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Slominski A., Wortsman J., Luger T., Paus R., Solomon S. Corticotropin releasing hormone and proopiomelanocortin involvement in the cutaneous response to stress. Physiol. Rev. 2000;80:979–1020. doi: 10.1152/physrev.2000.80.3.979. [DOI] [PubMed] [Google Scholar]
- 57.Slominski A.T., Zmijewski M.A., Zbytek B., Tobin D.J., Theoharides T.C., Rivier J. Key role of CRF in the skin stress response system. Endocr. Rev. 2013;34:827–884. doi: 10.1210/er.2012-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Slominski A.T., Kleszczyński K., Semak I., Janjetovic Z., Zmijewski M.A., Kim T.K., Slominski R.M., Reiter R.J., Fischer T.W. Local melatoninergic system as the protector of skin integrity. Int. J. Mol. Sci. 2014;15:17705–17732. doi: 10.3390/ijms151017705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Slominski A., Wortsman J., Paus R., Elias P.M., Tobin D.J., Feingold K.R. Skin as an endocrine organ: Implications for its function. Drug Discov. Today Dis. Mech. 2008;5:137–144. doi: 10.1016/j.ddmec.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tončić R.J., Kezić S., Hadžavdić S.L., Marinović B. Skin barrier and dry skin in the mature patient. Clin. Dermatol. 2017;36:109–115. doi: 10.1016/j.clindermatol.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 61.Marrot L. Pollution and Sun Exposure: A Deleterious Synergy. Mechanisms and Opportunities for Skin Protection. Curr. Med. Chem. 2018;25:5469–5486. doi: 10.2174/0929867324666170918123907. [DOI] [PubMed] [Google Scholar]
- 62.Piao M.J., Ahn M.J., Kang K.A., Ryu Y.S., Hyun Y.J., Shilnikova K., Zhen A.X., Jeong J.W., Choi Y.H., Kang H.K., et al. Particulate matter 2.5 damages skin cells by inducing oxidative stress, subcellular organelle dysfunction, and apoptosis. Arch. Toxicol. 2018;92:2077–2091. doi: 10.1007/s00204-018-2197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wortzman M., Nelson D.B. A comprehensive topical antioxidant inhibits oxidative stress induced by blue light exposure and cigarette smoke in human skin tissue. J. Cosmet. Dermatol. 2021;20:1160–1165. doi: 10.1111/jocd.13991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mokrzyński K., Krzysztyńska-Kuleta O., Zawrotniak M., Sarna M., Sarna T. Fine Particulate Matter-Induced Oxidative Stress Mediated by UVA-Visible Light Leads to Keratinocyte Damage. Int. J. Mol. Sci. 2021;22:10645. doi: 10.3390/ijms221910645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Romani A., Cervellati C., Muresan X.M., Belmonte G., Pecorelli A., Cervellati F., Benedusi M., Evelson P., Valacchi G. Keratinocytes oxidative damage mechanisms related to airbone particle matter exposure. Mech. Ageing Dev. 2018;172:86–95. doi: 10.1016/j.mad.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 66.Piao M.J., Kang K.A., Zhen A.X., Fernando P.D.S.M., Ahn M.J., Koh Y.S., Kang H.K., Yi J.M., Choi Y.H., Hyun J.W. Particulate matter 2.5 mediates cutaneous cellular injury by inducing mitochondria-associated endoplasmic reticulum stress: Protective effects of ginsenoside Rb1. Antioxidants. 2019;8:383. doi: 10.3390/antiox8090383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grevendonk L., Janssen B.G., Vanpoucke C., Lefebvre W., Hoxha M., Bollati V., Nawrot T.S. Mitochondrial oxidative DNA damage and exposure to particulate air pollution in mother-newborn pairs. Environ. Health. 2016;15:10. doi: 10.1186/s12940-016-0095-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gao D., Ripley S., Weichenthal S., Godri Pollitt K.J. Ambient particulate matter oxidative potential: Chemical determinants, associated health effects, and strategies for risk management. Free Radic. Biol. Med. 2020;151:7–25. doi: 10.1016/j.freeradbiomed.2020.04.028. [DOI] [PubMed] [Google Scholar]
- 69.Pecorelli A., Woodby B., Prieux R., Valacchi G. Involvement of 4-hydroxy-2-nonenal in pollution-induced skin damage. Biofactors. 2019;45:536–547. doi: 10.1002/biof.1513. [DOI] [PubMed] [Google Scholar]
- 70.Verdin A., Cazier F., Fitoussi R., Blanchet N., Vié K., Courcot D., Momas I., Seta N., Achard S. An in vitro model to evaluate the impact of environmental fine particles (PM0.3–2.5) on skin damage. Toxicol. Lett. 2019;305:94–102. doi: 10.1016/j.toxlet.2019.01.016. [DOI] [PubMed] [Google Scholar]
- 71.Bickers D.R., Athar M. Oxidative stress in the pathogenesis of skin disease. J. Investig. Dermatol. 2006;126:2565–2575. doi: 10.1038/sj.jid.5700340. [DOI] [PubMed] [Google Scholar]
- 72.Valacchi G., Fortino V., Bocci V. The dual action of ozone on the skin. Br. J. Dermatol. 2005;153:1096–1100. doi: 10.1111/j.1365-2133.2005.06939.x. [DOI] [PubMed] [Google Scholar]
- 73.Weber S.U., Jothi S., Thiele J.J. High-pressure liquid chromatography analysis of ozone-induced depletion of hydrophilic and lipophilic antioxidants in murine skin. Methods Enzymol. 2000;319:536–546. doi: 10.1016/s0076-6879(00)19050-0. [DOI] [PubMed] [Google Scholar]
- 74.Weber S.U., Thiele J.J., Cross C.E., Packer L. Vitamin C, uric acid, and glutathione gradients in murine stratum corneum and their susceptibility to ozone exposure. J. Investig. Dermatol. 1999;113:1128–1132. doi: 10.1046/j.1523-1747.1999.00789.x. [DOI] [PubMed] [Google Scholar]
- 75.De Luca C., Valacchi G. Surface lipids as multifunctional mediators of skin responses to environmental stimuli. Mediat. Inflamm. 2010;2010:321494. doi: 10.1155/2010/321494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Thiele J.J., Weber S.U., Packer L. Sebaceous gland secretion is a major physiologic route of vitamin E delivery to skin. J. Investig. Dermatol. 1999;113:1006–1010. doi: 10.1046/j.1523-1747.1999.00794.x. [DOI] [PubMed] [Google Scholar]
- 77.Ekanayake Mudiyanselage S., Hamburger M., Elsner P., Thiele J.J. Ultraviolet a induces generation of squalene monohydroperoxide isomers in human sebum and skin surface lipids in vitro and in vivo. J. Investig. Dermatol. 2003;120:915–922. doi: 10.1046/j.1523-1747.2003.12233.x. [DOI] [PubMed] [Google Scholar]
- 78.Pham D.M., Boussouira B., Moyal D., Nguyen Q.L. Oxidization of squalene, a human skin lipid: A new and reliable marker of environmental pollution studies. Int. J. Cosmet. Sci. 2015;37:357–365. doi: 10.1111/ics.12208. [DOI] [PubMed] [Google Scholar]
- 79.Lefebvre M.A., Pham D.M., Boussouira B., Bernard D., Camus C., Nguyen Q.L. Evaluation of the impact of urban pollution on the quality of skin: A multicentre study in Mexico. Int. J. Cosmet. Sci. 2015;37:329–338. doi: 10.1111/ics.12203. [DOI] [PubMed] [Google Scholar]
- 80.Zhang Q., Tang S., Huang G., Liu H. Cigarettes, a skin killer! Cigarette smoke may cause ferroptosis in female skin. J. Cosmet. Dermatol. 2022;21:3085–3094. doi: 10.1111/jocd.14559. [DOI] [PubMed] [Google Scholar]
- 81.Esser C., Bargen I., Weighardt H., Haarmann-Stemmann T., Krutmann J. Functions of the aryl hydrocarbon receptor in the skin. Semin. Immunopathol. 2013;35:677–691. doi: 10.1007/s00281-013-0394-4. [DOI] [PubMed] [Google Scholar]
- 82.Furue M., Takahara M., Nakahara T., Uchi H. Role of AhR/ARNT system in skin homeostasis. Arch. Dermatol. Res. 2014;306:769–779. doi: 10.1007/s00403-014-1481-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Szelest M., Walczak K., Plech T. A New Insight into the Potential Role of Tryptophan-Derived AhR Ligands in Skin Physiological and Pathological Processes. Int. J. Mol. Sci. 2021;22:1104. doi: 10.3390/ijms22031104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jux B., Kadow S., Luecke S., Rannug A., Krutmann J., Esser C. The aryl hydrocarbon receptor mediates UVB radiation-induced skin tanning. J. Investig. Dermatol. 2011;131:203–210. doi: 10.1038/jid.2010.269. [DOI] [PubMed] [Google Scholar]
- 85.Ahn Y., Lee E.J., Luo E., Choi J., Kim J.Y., Kim S., Kim S.-H., Bae Y.J., Park S., Lee J., et al. Particulate Matter Promotes Melanin Production through Endoplasmic Reticulum Stress-Mediated IRE1α Signaling. J. Investig. Dermatol. 2022;142:1425–1434.e6. doi: 10.1016/j.jid.2021.08.444. [DOI] [PubMed] [Google Scholar]
- 86.Esser C., Lawrence B.P., Sherr D.H., Perdew G.H., Puga A., Barouki R., Coumoul X. Old Receptor, New Tricks-The Ever-Expanding Universe of Aryl Hydrocarbon Receptor Functions. Report from the 4th AHR Meeting, 29–31 August 2018 in Paris, France. Int. J. Mol. Sci. 2018;19:3603. doi: 10.3390/ijms19113603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ye W., Chen R., Chen X., Huang B., Lin R., Xie X., Chen J., Jiang J., Deng Y., Wen J. AhR regulates the expression of human cytochrome P450 1A1 (CYP1A1) by recruiting Sp1. FEBS J. 2019;286:4215–4231. doi: 10.1111/febs.14956. [DOI] [PubMed] [Google Scholar]
- 88.Mimura J., Ema M., Sogawa K., Fujii-Kuriyama Y. Identification of a novel mechanism of regulation of Ah (dioxin) receptor function. Genes Dev. 1999;13:20–25. doi: 10.1101/gad.13.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tan Y.Q., Wang Y.N., Feng H.Y., Guo Z.Y., Li X., Nie X.L., Zhao Y.Y. Host/microbiota interactions-derived tryptophan metabolites modulate oxidative stress and inflammation via aryl hydrocarbon receptor signaling. Free Radic. Biol. Med. 2022;184:30–41. doi: 10.1016/j.freeradbiomed.2022.03.025. [DOI] [PubMed] [Google Scholar]
- 90.Uberoi A., Bartow-McKenney C., Zheng Q., Flowers L., Campbell A., Knight S.A.B., Chan N., Wei M., Lovins V., Bugayev J., et al. Commensal microbiota regulates skin barrier function and repair via signaling through the aryl hydrocarbon receptor. Cell Host Microbe. 2021;29:1235–1248.e8. doi: 10.1016/j.chom.2021.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tsuji G., Takahara M., Uchi H., Matsuda T., Chiba T., Takeuchi S., Yasukawa F., Moroi Y., Furue M. Identification of Ketoconazole as an AhR-Nrf2 Activator in Cultured Human Keratinocytes: The Basis of Its Anti-Inflammatory Effect. J. Investig. Dermatol. 2012;132:59–68. doi: 10.1038/jid.2011.194. [DOI] [PubMed] [Google Scholar]
- 92.Contador-Troca M., Alvarez-Barrientos A., Barrasa E., Rico-Leo E.M., Catalina-Fernández I., Menacho-Márquez M., Bustelo X.R., García-Borrón J.C., Gómez-Durán A., Sáenz-Santamaría J., et al. The dioxin receptor has tumor suppressor activity in melanoma growth and metastasis. Carcinogenesis. 2013;34:2683–2693. doi: 10.1093/carcin/bgt248. [DOI] [PubMed] [Google Scholar]
- 93.Slominski A.T., Kim T.K., Janjetovic Z., Brożyna A.A., Żmijewski M.A., Xu H., Sutter T.R., Tuckey R.C., Jetten A.M., Crossman D.K. Differential and Overlapping Effects of 20,23(OH)2D3 and 1,25(OH)2D3 on Gene Expression in Human Epidermal Keratinocytes: Identification of AhR as an Alternative Receptor for 20,23(OH)2D3. Int. J. Mol. Sci. 2018;19:3072. doi: 10.3390/ijms19103072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Brzeminski P., Fabisiak A., Slominski R.M., Kim T.K., Janjetovic Z., Podgorska E., Song Y., Saleem M., Reddy S.B., Qayyum S., et al. Chemical synthesis, biological activities and action on nuclear receptors of 20S(OH)D3, 20S,25(OH)2D3, 20S,23S(OH)2D3 and 20S,23R(OH)2D3. Bioorg. Chem. 2022;121:105660. doi: 10.1016/j.bioorg.2022.105660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Song Y., Slominski R.M., Qayyum S., Kim T.K., Janjetovic Z., Raman C., Tuckey R.C., Song Y., Slominski A.T. Molecular and structural basis of interactions of vitamin D3 hydroxyderivatives with aryl hydrocarbon receptor (AhR): An integrated experimental and computational study. Pt AInt. J. Biol. Macromol. 2022;209:1111–1123. doi: 10.1016/j.ijbiomac.2022.04.048. [DOI] [PubMed] [Google Scholar]
- 96.Grishanova A.Y., Perepechaeva M.L. Aryl Hydrocarbon Receptor in Oxidative Stress as a Double Agent and Its Biological and Therapeutic Significance. Int. J. Mol. Sci. 2022;23:6719. doi: 10.3390/ijms23126719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kim M., Kim J.H., Jeong G.J., Park K.Y., Lee M.K., Seo S.J. Particulate matter induces pro-inflammatory cytokines via phosphorylation of p38 MAPK possibly leading to dermal inflammaging. Exp. Dermatol. 2019;28:809–815. doi: 10.1111/exd.13943. [DOI] [PubMed] [Google Scholar]
- 98.Magnani N.D., Muresan X.M., Belmonte G., Cervellati F., Sticozzi C., Pecorelli A., Miracco C., Marchini T., Evelson P., Valacchi G. Skin Damage Mechanisms Related to Airborne Particulate Matter Exposure. Toxicol. Sci. 2016;149:227–236. doi: 10.1093/toxsci/kfv230. [DOI] [PubMed] [Google Scholar]
- 99.Yang Y.S., Lim H.K., Hong K.K., Shin M.K., Lee J.W., Lee S.W., Kim N.I. Cigarette smoke-induced interleukin-1 alpha may be involved in the pathogenesis of adult acne. Ann. Dermatol. 2014;26:11–16. doi: 10.5021/ad.2014.26.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tsuji G., Takahara M., Uchi H., Takeuchi S., Mitoma C., Moroi Y., Furue M. An environmental contaminant, benzo(a)pyrene, induces oxidative stress-mediated interleukin-8 production in human keratinocytes via the aryl hydrocarbon receptor signaling pathway. J. Dermatol Sci. 2011;62:42–49. doi: 10.1016/j.jdermsci.2010.10.017. [DOI] [PubMed] [Google Scholar]
- 101.Suvanprakorn P., Tongyen T., Prakhongcheep O., Laoratthaphong P., Chanvorachote P. Establishment of an Anti-acne Vulgaris Evaluation Method Based on TLR2 and TLR4-mediated Interleukin-8 Production. In Vivo. 2019;33:1929–1934. doi: 10.21873/invivo.11687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Skov L., Beurskens F.J., Zachariae C.O., Reitamo S., Teeling J., Satijn D., Knudsen K.M., Boot E.P., Hudson D., Baadsgaard O., et al. IL-8 as antibody therapeutic target in inflammatory diseases: Reduction of clinical activity in palmoplantar pustulosis. J. Immunol. 2008;181:669–679. doi: 10.4049/jimmunol.181.1.669. [DOI] [PubMed] [Google Scholar]
- 103.Valacchi G., Sticozzi C., Belmonte G., Cervellati F., Demaude J., Chen N., Krol Y., Oresajo C. Vitamin C Compound Mixtures Prevent Ozone-Induced Oxidative Damage in Human Keratinocytes as Initial Assessment of Pollution Protection. PLoS ONE. 2015;10:e0131097. doi: 10.1371/journal.pone.0131097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Haarmann-Stemmann T., Esser C., Krutmann J. The Janus-Faced Role of Aryl Hydrocarbon Receptor Signaling in the Skin: Consequences for Prevention and Treatment of Skin Disorders. J. Investig. Dermatol. 2015;135:2572–2576. doi: 10.1038/jid.2015.285. [DOI] [PubMed] [Google Scholar]
- 105.Lee C.W., Lin Z.C., Hu S.C., Chiang Y.C., Hsu L.F., Lin Y.C., Lee I.T., Tsai M.H., Fang J.Y. Urban particulate matter down-regulates filaggrin via COX2 expression/PGE2 production leading to skin barrier dysfunction. Sci. Rep. 2016;6:27995. doi: 10.1038/srep27995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ono Y., Torii K., Fritsche E., Shintani Y., Nishida E., Nakamura M., Shirakata Y., Haarmann-Stemmann T., Abel J., Krutmann J., et al. Role of the aryl hydrocarbon receptor in tobacco smoke extract-induced matrix metalloproteinase-1 expression. Exp. Dermatol. 2013;22:349–353. doi: 10.1111/exd.12148. [DOI] [PubMed] [Google Scholar]
- 107.Lecas S., Boursier E., Fitoussi R., Vié K., Momas I., Seta N., Achard S. In vitro model adapted to the study of skin ageing induced by air pollution. Toxicol. Lett. 2016;259:60–68. doi: 10.1016/j.toxlet.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 108.Birkedal-Hansen H. Catabolism and turnover of collagens: Collagenases. Methods Enzymol. 1987;144:140–171. doi: 10.1016/0076-6879(87)44177-3. [DOI] [PubMed] [Google Scholar]
- 109.Sárdy M. Role of matrix metalloproteinases in skin ageing. Connect. Tissue Res. 2009;50:132–138. doi: 10.1080/03008200802585622. [DOI] [PubMed] [Google Scholar]
- 110.Vierkötter A., Schikowski T., Ranft U., Sugiri D., Matsui M., Krämer U., Krutmann J. Airborne particle exposure and extrinsic skin aging. J. Investig. Dermatol. 2010;130:2719–2726. doi: 10.1038/jid.2010.204. [DOI] [PubMed] [Google Scholar]
- 111.Qiao Y., Li Q., Du H.Y., Wang Q.W., Huang Y., Liu W. Airborne polycyclic aromatic hydrocarbons trigger human skin cells aging through aryl hydrocarbon receptor. Biochem. Biophys. Res. Commun. 2017;488:445–452. doi: 10.1016/j.bbrc.2017.04.160. [DOI] [PubMed] [Google Scholar]
- 112.Sutter C.H., Yin H., Li Y., Mammen J.S., Bodreddigari S., Stevens G., Cole J.A., Sutter T.R. EGF receptor signaling blocks aryl hydrocarbon receptor-mediated transcription and cell differentiation in human epidermal keratinocytes. Proc. Natl. Acad. Sci. USA. 2009;106:4266–4271. doi: 10.1073/pnas.0900874106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kennedy L.H., Sutter C.H., Leon Carrion S., Tran Q.T., Bodreddigari S., Kensicki E., Mohney R.P., Sutter T.R. 2,3,7,8-Tetrachlorodibenzo-p-dioxin-mediated production of reactive oxygen species is an essential step in the mechanism of action to accelerate human keratinocyte differentiation. Toxicol. Sci. 2013;132:235–249. doi: 10.1093/toxsci/kfs325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yin L., Morita A., Tsuji T. Tobacco smoke extract induces age-related changes due to modulation of TGF-beta. Exp. Dermatol. 2003;12:51–56. doi: 10.1034/j.1600-0625.12.s2.8.x. [DOI] [PubMed] [Google Scholar]
- 115.Huang N., Mi T., Xu S., Dadd T., Ye X., Chen G., Du Y., Santhanam U. Traffic-derived air pollution compromises skin barrier function and stratum corneum redox status: A population study. J. Cosmet. Dermatol. 2019;19:1751–1759. doi: 10.1111/jocd.13194. [DOI] [PubMed] [Google Scholar]
- 116.Hieda D.S., Anastacio da Costa Carvalho L., Vaz de Mello B., Oliveira E.A., Romano de Assis S., Wu J., Du-Thumm L., Viana da Silva C.L., Roubicek D.A., Maria-Engler S.S., et al. Air Particulate Matter Induces Skin Barrier Dysfunction and Water Transport Alteration on a Reconstructed Human Epidermis Model. J. Investig. Dermatol. 2020;140:2343–2352.e3. doi: 10.1016/j.jid.2020.03.971. [DOI] [PubMed] [Google Scholar]
- 117.Haas K., Weighardt H., Deenen R., Köhrer K., Clausen B., Zahner S., Boukamp P., Bloch W., Krutmann J., Esser C. Aryl Hydrocarbon Receptor in Keratinocytes Is Essential for Murine Skin Barrier Integrity. J. Investig. Dermatol. 2016;136:2260–2269. doi: 10.1016/j.jid.2016.06.627. [DOI] [PubMed] [Google Scholar]
- 118.Mousavi S.E., Amini H., Heydarpour P., Amini Chermahini F., Godderis L. Air pollution, environmental chemicals, and smoking may trigger vitamin D deficiency: Evidence and potential mechanisms. Environ. Int. 2019;122:67–90. doi: 10.1016/j.envint.2018.11.052. [DOI] [PubMed] [Google Scholar]
- 119.Johns L.E., Ferguson K.K., Meeker J.D. Relationships Between Urinary Phthalate Metabolite and Bisphenol A Concentrations and Vitamin D Levels in U.S. Adults: National Health and Nutrition Examination Survey (NHANES), 2005–2010. J. Clin. Endocrinol. Metab. 2016;101:4062–4069. doi: 10.1210/jc.2016-2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shinkov A., Borissova A.M., Dakovska L., Vlahov J., Kassabova L., Svinarov D. Winter 25-hydroxyvitamin D levels in young urban adults are affected by smoking, body mass index and educational level. Eur. J. Clin. Nutr. 2015;69:355–360. doi: 10.1038/ejcn.2014.163. [DOI] [PubMed] [Google Scholar]
- 121.Kmieć P., Żmijewski M., Waszak P., Sworczak K., Lizakowska-Kmieć M. Vitamin D deficiency during winter months among an adult, predominantly urban, population in Northern Poland. Endokrynol. Pol. 2014;65:105–113. doi: 10.5603/EP.2014.0015. [DOI] [PubMed] [Google Scholar]
- 122.Wacker M., Holick M.F. Sunlight and Vitamin D: A global perspective for health. Dermatoendocrinology. 2013;5:51–108. doi: 10.4161/derm.24494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Slominski A.T., Kim T.K., Shehabi H.Z., Semak I., Tang E.K., Nguyen M.N., Benson H.A., Korik E., Janjetovic Z., Chen J., et al. In vivo evidence for a novel pathway of vitamin D3 metabolism initiated by P450scc and modified by CYP27B1. FASEB J. 2012;26:3901–3915. doi: 10.1096/fj.12-208975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tuckey R.C., Cheng C.Y.S., Slominski A.T. The serum vitamin D metabolome: What we know and what is still to discover. J. Steroid Biochem. Mol. Biol. 2019;186:4–21. doi: 10.1016/j.jsbmb.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bikle D., Christakos S. New aspects of vitamin D metabolism and action—Addressing the skin as source and target. Nat. Rev. Endocrinol. 2020;16:234–252. doi: 10.1038/s41574-019-0312-5. [DOI] [PubMed] [Google Scholar]
- 126.Slominski A.T., Kim T.K., Li W., Tuckey R.C. Classical and non-classical metabolic transformation of vitamin D in dermal fibroblasts. Exp. Dermatol. 2016;25:231–232. doi: 10.1111/exd.12872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Baïz N., Dargent-Molina P., Wark J.D., Souberbielle J.C., Slama R., Annesi-Maesano I., EDEN Mother-Child Cohort Study Group Gestational exposure to urban air pollution related to a decrease in cord blood vitamin d levels. J. Clin. Endocrinol. Metab. 2012;97:4087–4095. doi: 10.1210/jc.2012-1943. [DOI] [PubMed] [Google Scholar]
- 128.Hoseinzadeh E., Taha P., Wei C., Godini H., Ashraf G.M., Taghavi M., Miri M. The impact of air pollutants, UV exposure and geographic location on vitamin D deficiency. Food Chem. Toxicol. 2018;113:241–254. doi: 10.1016/j.fct.2018.01.052. [DOI] [PubMed] [Google Scholar]
- 129.Oda Y., Hu L., Nguyen T., Fong C., Zhang J., Guo P., Bikle D.D. Vitamin D Receptor Is Required for Proliferation, Migration, and Differentiation of Epidermal Stem Cells and Progeny during Cutaneous Wound Repair. J. Investig. Dermatol. 2018;138:2423–2431. doi: 10.1016/j.jid.2018.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Reichrath J., Saternus R., Vogt T. Challenge and perspective: The relevance of ultraviolet (UV) radiation and the vitamin D endocrine system (VDES) for psoriasis and other inflammatory skin diseases. Photochem. Photobiol. Sci. 2017;16:433–444. doi: 10.1039/c6pp00280c. [DOI] [PubMed] [Google Scholar]
- 131.Bocheva G., Slominski R.M., Slominski A.T. The impact of vitamin D on skin aging. Int. J. Mol. Sci. 2021;22:9097. doi: 10.3390/ijms22169097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Reichrath J., Zouboulis C.C., Vogt T., Holick M.F. Targeting the vitamin D endocrine system (VDES) for the management of inflammatory and malignant skin diseases: An historical view and outlook. Rev. Endocr. Metab. Disord. 2016;17:405–417. doi: 10.1007/s11154-016-9353-4. [DOI] [PubMed] [Google Scholar]
- 133.Slominski A.T., Chaiprasongsuk A., Janjetovic Z., Kim T.K., Stefan J., Slominski R.M., Hanumanthu V.S., Raman C., Qayyum S., Song Y., et al. Photoprotective Properties of Vitamin D and Lumisterol Hydroxyderivatives. Cell Biochem. Biophys. 2020;78:165–180. doi: 10.1007/s12013-020-00913-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Scott J.F., Das L.M., Ahsanuddin S., Qiu Y., Binko A.M., Traylor Z.P., Debanne S.M., Cooper K.D., Boxer R., Lu K.Q. Oral Vitamin D Rapidly Attenuates Inflammation from Sunburn: An Interventional Study. J. Investig. Dermatol. 2017;137:2078–2086. doi: 10.1016/j.jid.2017.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tongkao-On W., Carter S., Reeve V.E., Dixon K.M., Gordon-Thomson C., Halliday G.M., Tuckey R.C., Mason R.S. CYP11A1 in skin: An alternative route to photoprotection by vitamin D compounds. J. Steroid Biochem. Mol. Biol. 2015;148:72–78. doi: 10.1016/j.jsbmb.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 136.Chaiprasongsuk A., Janjetovic Z., Kim T.K., Tuckey R.C., Li W., Raman C., Panich U., Slominski A.T. CYP11A1-derived vitamin D3 products protect against UVB-induced inflammation and promote keratinocytes differentiation. Free Radic. Biol. Med. 2020;155:87–98. doi: 10.1016/j.freeradbiomed.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chaiprasongsuk A., Janjetovic Z., Kim T.K., Jarrett S.G., D’Orazio J.A., Holick M.F., Tang E.K.Y., Tuckey R.C., Panich U., Li W., et al. Protective effects of novel derivatives of vitamin D3 and lumisterol against UVB-induced damage in human keratinocytes involve activation of Nrf2 and p53 defense mechanisms. Redox Biol. 2019;24:101206. doi: 10.1016/j.redox.2019.101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Chaiprasongsuk A., Janjetovic Z., Kim T.K., Schwartz C.J., Tuckey R.C., Tang E.K.Y., Raman C., Panich U., Slominski A.T. Hydroxylumisterols, Photoproducts of Pre-Vitamin D3, Protect Human Keratinocytes against UVB-Induced Damage. Int. J. Mol. Sci. 2020;21:9374. doi: 10.3390/ijms21249374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.De Silva W.G.M., Han J.Z.R., Yang C., Tongkao-On W., McCarthy B.Y., Ince F.A., Holland A.J.A., Tuckey R.C., Slominski A.T., Abboud M., et al. Evidence for Involvement of Nonclassical Pathways in the Protection From UV-Induced DNA Damage by Vitamin D-Related Compounds. JBMR Plus. 2021;5:e10555. doi: 10.1002/jbm4.10555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Slominski A.T., Brożyna A.A., Skobowiat C., Zmijewski M.A., Kim T.K., Janjetovic Z., Oak A.S., Jozwicki W., Jetten A.M., Mason R.S., et al. On the role of classical and novel forms of vitamin D in melanoma progression and management. J. Steroid Biochem. Mol. Biol. 2018;177:159–170. doi: 10.1016/j.jsbmb.2017.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Brożyna A.A., Hoffman R.M., Slominski A.T. Relevance of Vitamin D in Melanoma Development, Progression and Therapy. Anticancer Res. 2020;40:473–489. doi: 10.21873/anticanres.13976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Slominski A.T., Janjetovic Z., Kim T.K., Wright A.C., Grese L.N., Riney S.J., Nguyen M.N., Tuckey R.C. Novel vitamin D hydroxyderivatives inhibit melanoma growth and show differential effects on normal melanocytes. Anticancer Res. 2012;32:3733–3742. [PMC free article] [PubMed] [Google Scholar]
- 143.Slominski A.T., Brożyna A.A., Zmijewski M.A., Janjetovic Z., Kim T.K., Slominski R.M., Tuckey R.C., Mason R.S., Jetten A.M., Guroji P., et al. The Role of Classical and Novel Forms of Vitamin D in the Pathogenesis and Progression of Nonmelanoma Skin Cancers. Adv. Exp. Med. Biol. 2020;1268:257–283. doi: 10.1007/978-3-030-46227-7_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Slominski A.T., Brożyna A.A., Kim T.K., Elsayed M.M., Janjetovic Z., Qayyum S., Slominski R.M., Oak A.S.W., Li C., Podgorska E., et al. CYP11A1-derived vitamin D hydroxyderivatives as candidates for therapy of basal and squamous cell carcinomas. Int. J. Oncol. 2022;61:96. doi: 10.3892/ijo.2022.5386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Dixon K.M., Norman A.W., Sequeira V.B., Mohan R., Rybchyn M.S., Reeve V.E., Halliday G.M., Mason R.S. 1α,25(OH)2-vitamin D and a nongenomic vitamin D analogue inhibit ultraviolet radiation-induced skin carcinogenesis. Cancer Prev. Res. 2011;4:1485–1494. doi: 10.1158/1940-6207.CAPR-11-0165. [DOI] [PubMed] [Google Scholar]
- 146.Bocheva G., Slominski R.M., Slominski A.T. Neuroendocrine Aspects of Skin Aging. Int. J. Mol. Sci. 2019;20:2798. doi: 10.3390/ijms20112798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Farage M.A., Miller K.W., Elsner P., Maibach H.I. Intrinsic and extrinsic factors in skin ageing: A review. Int. J. Cosmet. Sci. 2008;30:87–95. doi: 10.1111/j.1468-2494.2007.00415.x. [DOI] [PubMed] [Google Scholar]
- 148.Passeron T., Krutmann J., Andersen M.L., Katta R., Zouboulis C.C. Clinical and biological impact of the exposome on the skin. J. Eur. Acad. Dermatol. Venereol. 2020;34((Suppl. 4)):4–25. doi: 10.1111/jdv.16614. [DOI] [PubMed] [Google Scholar]
- 149.Green A.C., Wallingford S.C., McBride P. Childhood exposure to ultraviolet radiation and harmful skin effects: Epidemiological evidence. Prog. Biophys. Mol. Biol. 2011;107:349–355. doi: 10.1016/j.pbiomolbio.2011.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Vierkötter A., Krutmann J. Environmental influences on skin aging and ethnic-specific manifestations. Dermatoendocrinology. 2012;4:227–231. doi: 10.4161/derm.19858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Parrado C., Mercado-Saenz S., Perez-Davo A., Gilaberte Y., Gonzalez S., Juarranz A. Environmental Stressors on Skin Aging. Mechanistic Insights. Front. Pharmacol. 2019;10:759. doi: 10.3389/fphar.2019.00759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Martic I., Jansen-Dürr P., Cavinato M. Effects of Air Pollution on Cellular Senescence and Skin Aging. Cells. 2022;11:2220. doi: 10.3390/cells11142220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kennedy C., Bastiaens M.T., Bajdik C.D., Willemze R., Westendorp R.G., Bouwes Bavinck J.N. Leiden Skin Cancer Study. Effect of smoking and sun on the aging skin. J. Investig. Dermatol. 2003;120:548–554. doi: 10.1046/j.1523-1747.2003.12092.x. [DOI] [PubMed] [Google Scholar]
- 154.Wondrak G.T., Jacobson M.K., Jacobson E.L. Endogenous UVA-photosensitizers: Mediators of skin photodamage and novel targets for skin photoprotection. Photochem Photobiol Sci. 2006;5:215–237. doi: 10.1039/b504573h. [DOI] [PubMed] [Google Scholar]
- 155.Kammeyer A., Luiten R.M. Oxidation events and skin aging. Ageing Res. Rev. 2015;21:16–29. doi: 10.1016/j.arr.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 156.Zhang R., Wang Y., Ye K., Picard M., Gu Z. Independent impacts of aging on mitochondrial DNA quantity and quality in humans. BMC Genom. 2017;18:890. doi: 10.1186/s12864-017-4287-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Papaccio F., D’Arino A., Caputo S., Bellei B. Focus on the Contribution of Oxidative Stress in Skin Aging. Antioxidants. 2022;11:1121. doi: 10.3390/antiox11061121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Fuks K.B., Hüls A., Sugiri D., Altug H., Vierkötter A., Abramson M.J., Goebel J., Wagner G.G., Demuth I., Krutmann J., et al. Tropospheric ozone and skin aging: Results from two German cohort studies. Environ. Int. 2019;124:139–144. doi: 10.1016/j.envint.2018.12.047. [DOI] [PubMed] [Google Scholar]
- 159.Hüls A., Sugiri D., Fuks K., Krutmann J., Schikowski T. Lentigine formation in caucasian women-interaction between particulate matter and solar UVR. J. Investig. Dermatol. 2018;139:974–976. doi: 10.1016/j.jid.2018.09.034. [DOI] [PubMed] [Google Scholar]
- 160.Peng F., Xue C.H., Hwang S.K., Li W.H., Chen Z., Zhang J.Z. Exposure to fine particulate matter associated with senile lentigo in Chinese women: A cross-sectional study. J. Eur. Acad. Dermatol. Venereol. 2017;31:355–360. doi: 10.1111/jdv.13834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bernhard D., Moser C., Backovic A., Wick G. Cigarette smoke—an aging accelerator? Exp. Gerontol. 2007;42:160–165. doi: 10.1016/j.exger.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 162.Morita A. Tobacco smoke causes premature skin aging. J. Dermatol. Sci. 2007;48:169–175. doi: 10.1016/j.jdermsci.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 163.Chaichalotornkul S., Nararatwanchai T., Narkpinit S., Dararat P., Kikuchi K., Maruyama I., Tancharoen S. Secondhand smoke exposure-induced nucleocytoplasmic shuttling of HMGB1 in a rat premature skin aging model. Biochem. Biophys. Res. Commun. 2015;456:92–97. doi: 10.1016/j.bbrc.2014.11.040. [DOI] [PubMed] [Google Scholar]
- 164.Morita A., Torii K., Maeda A., Yamaguchi Y. Molecular basis of tobacco smoke-induced premature skin aging. J. Investig. Dermatol. Symp. Proc. 2009;14:53–55. doi: 10.1038/jidsymp.2009.13. [DOI] [PubMed] [Google Scholar]
- 165.Reynolds W.J., Hanson P.S., Critchley A., Griffiths B., Chavan B., Birch-Machin M.A. Exposing human primary dermal fibroblasts to particulate matter induces changes associated with skin aging. FASEB J. 2020;34:14725–14735. doi: 10.1096/fj.202001357R. [DOI] [PubMed] [Google Scholar]
- 166.Park S.Y., Byun E.J., Lee J.D., Kim S., Kim H.S. Air pollution, autophagy, and skin aging impact of particulate matter (pm10) on human dermal fibroblasts. Int. J. Mol. Sci. 2018;19:E2727. doi: 10.3390/ijms19092727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Moan J., Grigalavicius M., Baturaite Z., Dahlback A., Juzeniene A. The relationship between UV exposure and incidence of skin cancer. Photodermatol. Photoimmunol. Photomed. 2015;31:26–35. doi: 10.1111/phpp.12139. [DOI] [PubMed] [Google Scholar]
- 168.Lin M.J., Torbeck R.L., Dubin D.P., Lin C.E., Khorasani H. Climate change and skin cancer. J. Eur. Acad. Dermatol. Venereol. 2019;33:e324–e325. doi: 10.1111/jdv.15622. [DOI] [PubMed] [Google Scholar]
- 169.Umar S.A., Tasduq S.A. Ozone Layer Depletion and Emerging Public Health Concerns—An Update on Epidemiological Perspective of the Ambivalent Effects of Ultraviolet Radiation Exposure. Front. Oncol. 2022;12:866733. doi: 10.3389/fonc.2022.866733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Balato N., Megna M., Ayala F., Balato A., Napolitano M., Patruno C. Effects of climate changes on skin diseases. Expert Rev. Anti-Infect. Ther. 2014;12:171–181. doi: 10.1586/14787210.2014.875855. [DOI] [PubMed] [Google Scholar]
- 171.Green A.C., Olsen C.M. Cutaneous squamous cell carcinoma: An epidemiological review. Br. J. Dermatol. 2017;177:373–381. doi: 10.1111/bjd.15324. [DOI] [PubMed] [Google Scholar]
- 172.Datzmann T., Markevych I., Trautmann F., Heinrich J., Schmitt J., Tesch F. Outdoor air pollution, green space, and cancer incidence in Saxony: A semi-individual cohort study. BMC Public Health. 2018;18:715. doi: 10.1186/s12889-018-5615-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Siddens L.K., Larkin A., Krueger S.K., Bradfield C.A., Waters K.M., Tilton S.C., Pereira C.B., Löhr C.V., Arlt V.M., Phillips D.H., et al. Polycyclic aromatic hydrocarbons as skin carcinogens: Comparison of benzo[a]pyrene, dibenzo[def,p]chrysene and three environmental mixtures in the FVB/N mouse. Toxicol. Appl. Pharmacol. 2012;264:377–386. doi: 10.1016/j.taap.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Hopf N.B., Spring P., Hirt-Burri N., Jimenez S., Sutter B., Vernez D., Berthet A. Polycyclic aromatic hydrocarbons (PAHs) skin permeation rates change with simultaneous exposures to solar ultraviolet radiation (UV-S) Toxicol. Lett. 2018;287:122–130. doi: 10.1016/j.toxlet.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 175.Dusingize J.C., Olsen C.M., Pandeya N.P., Subramaniam P., Thompson B.S., Neale R.E., Green A.C., Whiteman D.C. QSkin Study. Cigarette Smoking and the Risks of Basal Cell Carcinoma and Squamous Cell Carcinoma. J. Investig. Dermatol. 2017;137:1700–1708. doi: 10.1016/j.jid.2017.03.027. [DOI] [PubMed] [Google Scholar]
- 176.Bukowska B., Mokra K., Michałowicz J. Benzo[a]pyrene-Environmental Occurrence, Human Exposure, and Mechanisms of Toxicity. Int. J. Mol. Sci. 2022;23:6348. doi: 10.3390/ijms23116348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.McNeill J.M., Wills E.D. The formation of mutagenic derivatives of benzo[a]pyrene by peroxidising fatty acids. Chem. Biol. Interact. 1985;53:197–207. doi: 10.1016/S0009-2797(85)80096-X. [DOI] [PubMed] [Google Scholar]
- 178.Bukowska B., Duchnowicz P. Molecular Mechanisms of Action of Selected Substances Involved in the Reduction of Benzo[a]pyrene-Induced Oxidative Stress. Molecules. 2022;27:1379. doi: 10.3390/molecules27041379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Vogeley C., Rolfes K.M., Krutmann J., Haarmann-Stemmann T. The Aryl Hydrocarbon Receptor in the Pathogenesis of Environmentally-Induced Squamous Cell Carcinomas of the Skin. Front. Oncol. 2022;12:841721. doi: 10.3389/fonc.2022.841721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Andrysík Z., Vondráček J., Marvanová S., Ciganek M., Neča J., Pěnčíková K., Mahadevan B., Topinka J., Baird W.M., Kozubík A., et al. Activation of the aryl hydrocarbon receptor is the major toxic mode of action of an organic extract of a reference urban dust particulate matter mixture: The role of polycyclic aromatic hydrocarbons. Mutat. Res. 2011;714:53–62. doi: 10.1016/j.mrfmmm.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 181.Costa C., Catania S., De Pasquale R., Stancanelli R., Scribano G.M., Melchini A. Exposure of human skin to benzo[a]pyrene: Role of CYP1A1 and aryl hydrocarbon receptor in oxidative stress generation. Toxicology. 2010;271:83–86. doi: 10.1016/j.tox.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 182.Matsumoto Y., Ide F., Kishi R., Akutagawa T., Sakai S., Nakamura M., Ishikawa T., Fujii-Kuriyama Y., Nakatsuru Y. Aryl hydrocarbon receptor plays a significant role in mediating airborne particulate-induced carcinogenesis in mice. Environ. Sci. Technol. 2007;41:3775–3780. doi: 10.1021/es062793g. [DOI] [PubMed] [Google Scholar]
- 183.Shimizu Y., Nakatsuru Y., Ichinose M., Takahashi Y., Kume H., Mimura J., Fujii-Kuriyama Y., Ishikawa T. Benzo[a]pyrene carcinogenicity is lost in mice lacking the aryl hydrocarbon receptor. Proc. Natl. Acad. Sci. USA. 2000;97:779–782. doi: 10.1073/pnas.97.2.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Modi B.G., Neustadter J., Binda E., Lewis J., Filler R.B., Roberts S.J., Kwong B.Y., Reddy S., Overton J.D., Galan A., et al. Langerhans cells facilitate epithelial DNA damage and squamous cell carcinoma. Science. 2012;335:104–108. doi: 10.1126/science.1211600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Otsuka A., Nomura T., Rerknimitr P., Seidel J.A., Honda T., Kabashima K. The interplay between genetic and environmental factors in the pathogenesis of atopic dermatitis. Immunol. Rev. 2017;278:246–262. doi: 10.1111/imr.12545. [DOI] [PubMed] [Google Scholar]
- 186.Bocheva G.S., Slominski R.M., Slominski A.T. Immunological Aspects of Skin Aging in Atopic Dermatitis. Int. J. Mol. Sci. 2021;22:5729. doi: 10.3390/ijms22115729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ständer S. Atopic Dermatitis. N. Engl. J. Med. 2021;384:1136–1143. doi: 10.1056/NEJMra2023911. [DOI] [PubMed] [Google Scholar]
- 188.Luger T., Amagai M., Dreno B., Dagnelie M.A., Liao W., Kabashima K., Schikowski T., Proksch E., Elias P.M., Simon M., et al. Atopic dermatitis: Role of the skin barrier, environment, microbiome, and therapeutic agents. J. Dermatol. Sci. 2021;102:142–157. doi: 10.1016/j.jdermsci.2021.04.007. [DOI] [PubMed] [Google Scholar]
- 189.Kim J., Kim E.H., Oh I., Jung K., Han Y., Cheong H.K., Ahn K. Symptoms of atopic dermatitis are influenced by outdoor air pollution. J. Allergy Clin. Immunol. 2013;132:495–498.e1. doi: 10.1016/j.jaci.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 190.Fadadu R.P., Grimes B., Jewell N.P., Vargo J., Young A.T., Abuabara K., Balmes J.R., Wei M.L. Association of Wildfire Air Pollution and Health Care Use for Atopic Dermatitis and Itch. JAMA Dermatol. 2021;157:658–666. doi: 10.1001/jamadermatol.2021.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Park S.K., Kim J.S., Seo H.M. Exposure to air pollution and incidence of atopic dermatitis in the general population: A national population-based retrospective cohort study. J. Am. Acad. Dermatol. 2022;87:1321–1327. doi: 10.1016/j.jaad.2021.05.061. [DOI] [PubMed] [Google Scholar]
- 192.Lee J.Y., Lamichhane D.K., Lee M., Ye S., Kwon J.H., Park M.S., Kim H.C., Leem J.H., Hong Y.C., Kim Y., et al. Preventive Effect of Residential Green Space on Infantile Atopic Dermatitis Associated with Prenatal Air Pollution Exposure. Int. J. Environ. Res. Public Health. 2018;15:102. doi: 10.3390/ijerph15010102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Deng S., Huang D., Wang W., Yan H., Li S., Xiang H. Associations of gestational and the first year of life exposure to ambient air pollution with childhood eczema in Hubei, China. Environ. Sci. Pollut Res Int. 2019;26:23842–23849. doi: 10.1007/s11356-019-05633-w. [DOI] [PubMed] [Google Scholar]
- 194.Yao T.C., Huang H.Y., Pan W.C., Wu C.Y., Tsai S.Y., Hung C.Y., Lu K.L., Chang-Chien J., Tseng C.L., Wu C.D., et al. Association of prenatal exposure to fine particulate matter pollution with childhood eczema. Allergy. 2021;76:2241–2245. doi: 10.1111/all.14738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Kim S.Y., Sim S., Choi H.G. Atopic dermatitis is associated with active and passive cigarette smoking in adolescents. PLoS ONE. 2017;12:e0187453. doi: 10.1371/journal.pone.0187453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Lee C.H., Chuang H.Y., Hong C.H., Huang S.K., Chang Y.C., Ko Y.C., Yu H.S. Lifetime exposure to cigarette smoking and the development of adult-onset atopic dermatitis. Br. J. Dermatol. 2011;164:483–489. doi: 10.1111/j.1365-2133.2010.10116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Kantor R., Kim A., Thyssen J.P., Silverberg J.I. Association of atopic dermatitis with smoking: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2016;75:1119–1125.e1. doi: 10.1016/j.jaad.2016.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Green M., Kashetsky N., Feschuk A., Maibach H.I. Transepidermal water loss (TEWL): Environment and pollution-A systematic review. Skin Health Dis. 2022;2:e104. doi: 10.1002/ski2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Shamsipour M., Nasrollahi S.A., Hassanvand M.S., Yazdanparast T., Samadi A., Yunesian M., Mahdavi M., Kassir M., Firooz A. Short-term effects of exposure to air pollution on biophysical parameters of skin in a panel of healthy adults. Dermatol. Ther. 2020;33:e14536. doi: 10.1111/dth.14536. [DOI] [PubMed] [Google Scholar]
- 200.Leung M.H.Y., Tong X., Shen Z., Du S., Bastien P., Appenzeller B.M.R., Betts R.J., Mezzache S., Bourokba N., Cavusoglu N., et al. Skin microbiome differentiates into distinct cutotypes with unique metabolic functions upon exposure to polycyclic aromatic hydrocarbons. Microbiome. 2023;11:124. doi: 10.1186/s40168-023-01564-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Lopez D.J., Lodge C.J., Bui D.S., Waidyatillake N.T., Su J.C., Perret J.L., Knibbs L.D., Erbas B., Thomas P.S., Hamilton G.S., et al. Association between ambient air pollution and development and persistence of atopic and non-atopic eczema in a cohort of adults. Allergy. 2021;76:2524–2534. doi: 10.1111/all.14783. [DOI] [PubMed] [Google Scholar]
- 202.Celebi Sozener Z., Özbey Yücel Ü., Altiner S., Ozdel Oztürk B., Cerci P., Türk M., Gorgülü Akin B., Akdis M., Yilmaz I., Ozdemir C., et al. The External Exposome and Allergies: From the Perspective of the Epithelial Barrier Hypothesis. Front. Allergy. 2022;3:887672. doi: 10.3389/falgy.2022.887672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Jin S.P., Li Z., Choi E.K., Lee S., Kim Y.K., Seo E.Y., Chung J.H., Cho S. Urban particulate matter in air pollution penetrates into the barrier-disrupted skin and produces ROS-dependent cutaneous inflammatory response in vivo. J. Dermatol. Sci. 2018;91:175–183. doi: 10.1016/j.jdermsci.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 204.Hu Y., Xu Z., Jiang F., Li S., Liu S., Wu M., Yan C., Tan J., Yu G., Hu Y., et al. Relative impact of meteorological factors and air pollutants on childhood allergic diseases in Shanghai, China. Sci. Total. Environ. 2020;706:135975. doi: 10.1016/j.scitotenv.2019.135975. [DOI] [PubMed] [Google Scholar]
- 205.Guo Q., Xiong X., Liang F., Tian L., Liu W., Wang Z., Pan X. The interactive effects between air pollution and meteorological factors on the hospital outpatient visits for atopic dermatitis in Beijing, China: A time-series analysis. J. Eur. Acad. Dermatol. Venereol. 2019;33:2362–2370. doi: 10.1111/jdv.15820. [DOI] [PubMed] [Google Scholar]
- 206.Isler M.F., Coates S.J., Boos M.D. Climate change, the cutaneous microbiome and skin disease: Implications for a warming world. Int. J. Dermatol. 2023;62:337–345. doi: 10.1111/ijd.16297. [DOI] [PubMed] [Google Scholar]
- 207.Furue M., Iida K., Imaji M., Nakahara T. Microbiome analysis of forehead skin in patients with atopic dermatitis and healthy subjects: Implication of Staphylococcus and Corynebacterium. J. Dermatol. 2018;45:876–877. doi: 10.1111/1346-8138.14486. [DOI] [PubMed] [Google Scholar]
- 208.Fadadu R.P., Abuabara K., Balmes J.R., Hanifin J.M., Wei M.L. Air Pollution and Atopic Dermatitis, from Molecular Mechanisms to Population-Level Evidence: A Review. Int. J. Environ. Res. Public Health. 2023;20:2526. doi: 10.3390/ijerph20032526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Pan Z., Dai Y., Akar-Ghibril N., Simpson J., Ren H., Zhang L., Hou Y., Wen X., Chang C., Tang R., et al. Impact of Air Pollution on Atopic Dermatitis: A Comprehensive Review. Clin. Rev. Allergy Immunol. 2023 doi: 10.1007/s12016-022-08957-7. [DOI] [PubMed] [Google Scholar]
- 210.Woo Y.R., Park S.Y., Choi K., Hong E.S., Kim S., Kim H.S. Air Pollution and Atopic Dermatitis (AD): The Impact of Particulate Matter (PM10) on an AD Mouse-Model. Int. J. Mol. Sci. 2020;21:6079. doi: 10.3390/ijms21176079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Kim H.O., Kim J.H., Chung B.Y., Choi M.G., Park C.W. Increased expression of the aryl hydrocarbon receptor in patients with chronic inflammatory skin diseases. Exp. Dermatol. 2014;23:278–281. doi: 10.1111/exd.12350. [DOI] [PubMed] [Google Scholar]
- 212.Hu Y.Q., Liu P., Mu Z.L., Zhang J.Z. Aryl hydrocarbon receptor expression in serum, peripheral blood mononuclear cells, and skin lesions of patients with atopic dermatitis and its correlation with disease severity. Chin. Med. J. 2020;133:148–153. doi: 10.1097/CM9.0000000000000591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Hong C.H., Lee C.H., Yu H.S., Huang S.K. Benzopyrene, a major polyaromatic hydrocarbon in smoke fume, mobilizes Langerhans cells and polarizes Th2/17 responses in epicutaneous protein sensitization through the aryl hydrocarbon receptor. Int. Immunopharmacol. 2016;36:111–117. doi: 10.1016/j.intimp.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 214.Hidaka T., Ogawa E., Kobayashi E.H., Suzuki T., Funayama R., Nagashima T., Fujimura T., Aiba S., Nakayama K., Okuyama R., et al. The aryl hydrocarbon receptor AhR links atopic dermatitis and air pollution via induction of the neurotrophic factor artemin. Nat. Immunol. 2017;18:64–73. doi: 10.1038/ni.3614. [DOI] [PubMed] [Google Scholar]
- 215.Grän F., Kerstan A., Serfling E., Goebeler M., Muhammad K. Current Developments in the Immunology of Psoriasis. Yale J. Biol. Med. 2020;93:97–110. [PMC free article] [PubMed] [Google Scholar]
- 216.Bellinato F., Adami G., Vaienti S., Benini C., Gatti D., Idolazzi L., Fassio A., Rossini M., Girolomoni G., Gisondi P. Association Between Short-term Exposure to Environmental Air Pollution and Psoriasis Flare. JAMA Dermatol. 2022;158:375–381. doi: 10.1001/jamadermatol.2021.6019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Wu J., Chen H., Yang R., Yu H., Shang S., Hu Y. Short-term exposure to ambient fine particulate matter and psoriasis: A time-series analysis in Beijing, China. Front. Public Health. 2022;10:1015197. doi: 10.3389/fpubh.2022.1015197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Armstrong A.W., Harskamp C.T., Dhillon J.S., Armstrong E.J. Psoriasis and smoking: A systematic review and meta-analysis. Br. J. Dermatol. 2014;170:304–314. doi: 10.1111/bjd.12670. [DOI] [PubMed] [Google Scholar]
- 219.van Voorhis M., Knopp S., Julliard W., Fechner J.H., Zhang X., Schauer J.J., Mezrich J.D. Exposure to atmospheric particulate matter enhances Th17 polarization through the aryl hydrocarbon receptor. PLoS ONE. 2013;8:e82545. doi: 10.1371/journal.pone.0082545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Afaq F., Zaid M.A., Pelle E., Khan N., Syed D.N., Matsui M.S., Maes D., Mukhtar H. Aryl hydrocarbon receptor is an ozone sensor in human skin. J. Investig. Dermatol. 2009;129:2396–2403. doi: 10.1038/jid.2009.85. [DOI] [PubMed] [Google Scholar]
- 221.Guillon C., Meziani M., Abdelli S., Sigaudo Roussel D., Bonod C., Nosbaum A. The aryl hydrocarbon receptor pathway plays a central role in the cutaneous response to pollutants. Eur. J. Dermatol. 2022;32:305–311. doi: 10.1684/ejd.2022.4262. [DOI] [PubMed] [Google Scholar]
- 222.Kim H.R., Kang S.Y., Kim H.O., Park C.W., Chung B.Y. Role of Aryl Hydrocarbon Receptor Activation and Autophagy in Psoriasis-Related Inflammation. Int. J. Mol. Sci. 2020;21:2195. doi: 10.3390/ijms21062195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Dréno B., Bettoli V., Araviiskaia E., Sanchez Viera M., Bouloc A. The influence of exposome on acne. J. Eur. Acad. Dermatol. Venereol. 2018;32:812–819. doi: 10.1111/jdv.14820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Wolkenstein P., Machovcová A., Szepietowski J.C., Tennstedt D., Veraldi S., Delarue A. Acne prevalence and associations with lifestyle: A cross-sectional online survey of adolescents/young adults in 7 European countries. J. Eur. Acad. Dermatol. Venereol. 2018;32:298–306. doi: 10.1111/jdv.14475. [DOI] [PubMed] [Google Scholar]
- 225.Hazarika N. Acne vulgaris: New evidence in pathogenesis and future modalities of treatment. J. Dermatolog. Treat. 2021;32:277–285. doi: 10.1080/09546634.2019.1654075. [DOI] [PubMed] [Google Scholar]
- 226.Krutmann J., Moyal D., Liu W., Kandahari S., Lee G.S., Nopadon N., Xiang L.F., Seité S. Pollution and acne: Is there a link? Clin. Cosmet. Investig. Dermatol. 2017;10:199–204. doi: 10.2147/CCID.S131323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Liu W., Pan X., Vierkötter A., Guo Q., Wang X., Wang Q., Seité S., Moyal D., Schikowski T., Krutmann J. A Time-Series Study of the Effect of Air Pollution on Outpatient Visits for Acne Vulgaris in Beijing. Skin Pharmacol. Physiol. 2018;31:107–113. doi: 10.1159/000484482. [DOI] [PubMed] [Google Scholar]
- 228.Li X., Cao Y., An S.J., Xiang Y., Huang H.X., Xu B., Zhang Y., Li Y.F., Lu Y.G., Cai T.J. The association between short-term ambient air pollution and acne vulgaris outpatient visits: A hospital-based time-series analysis in Xi’an. Environ. Sci. Pollut. Res. Int. 2022;29:14624–14633. doi: 10.1007/s11356-021-16607-2. [DOI] [PubMed] [Google Scholar]
- 229.Mourelatos K., Eady E.A., Cunliffe W.J., Clark S.M., Cove J.H. Temporal changes in sebum excretion and propionibacterial colonization in preadolescent children with and without acne. Br. J. Dermatol. 2007;156:22–31. doi: 10.1111/j.1365-2133.2006.07517.x. [DOI] [PubMed] [Google Scholar]
- 230.Capitanio B., Lora V., Ludovici M., Sinagra J.L., Ottaviani M., Mastrofrancesco A., Ardigò M., Camera E. Modulation of sebum oxidation and interleukin-1α levels associates with clinical improvement of mild comedonal acne. J. Eur. Acad. Dermatol. Venereol. 2014;28:1792–1797. doi: 10.1111/jdv.12431. [DOI] [PubMed] [Google Scholar]
- 231.Zouboulis C.C. Acne and sebaceous gland function. Clin. Dermatol. 2004;22:360–366. doi: 10.1016/j.clindermatol.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 232.Lefebvre M.A., Pham D.M., Boussouira B., Qiu H., Ye C., Long X., Chen R., Gu W., Laurent A., Nguyen Q.L. Consequences of urban pollution upon skin status. A controlled study in Shanghai area. Int. J. Cosmet. Sci. 2016;38:217–223. doi: 10.1111/ics.12270. [DOI] [PubMed] [Google Scholar]
- 233.El Haddad C., Gerbaka N.E., Hallit S., Tabet C. Association between exposure to ambient air pollution and occurrence of inflammatory acne in the adult population. BMC Public Health. 2021;21:1664. doi: 10.1186/s12889-021-11738-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Abd El All H.S., Shoukry N.S., El Maged R.A., Ayada M.M. Immunohistochemical expression of interleukin 8 in skin biopsies from patients with inflammatory acne vulgaris. Diagn. Pathol. 2007;2:4. doi: 10.1186/1746-1596-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.McLaughlin J., Watterson S., Layton A.M., Bjourson A.J., Barnard E., McDowell A. Propionibacterium acnes and Acne Vulgaris: New Insights from the Integration of Population Genetic, Multi-Omic, Biochemical and Host-Microbe Studies. Microorganisms. 2019;7:128. doi: 10.3390/microorganisms7050128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Sorg O., Zennegg M., Schmid P., Fedosyuk R., Valikhnovskyi R., Gaide O., Kniazevych V., Saurat J.H. 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) poisoning in Victor Yushchenko: Identification and measurement of TCDD metabolites. Lancet. 2009;374:1179–1185. doi: 10.1016/S0140-6736(09)60912-0. [DOI] [PubMed] [Google Scholar]
- 237.Furue M., Tsuji G. Chloracne and Hyperpigmentation Caused by Exposure to Hazardous Aryl Hydrocarbon Receptor Ligands. Int. J. Environ. Res. Public Health. 2019;16:4864. doi: 10.3390/ijerph16234864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Slominski R.M., Sarna T., Płonka P.M., Raman C., Brożyna A.A., Slominski A.T. Melanoma, Melanin, and Melanogenesis: The Yin and Yang Relationship. Front. Oncol. 2022;12:842496. doi: 10.3389/fonc.2022.842496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Eller M.S., Gilchrest B.A. Tanning as part of the eukaryotic SOS response. Pigment Cell Res. 2000;13((Suppl. S8)):94–97. doi: 10.1034/j.1600-0749.13.s8.17.x. [DOI] [PubMed] [Google Scholar]
- 240.Roberts W.E. Pollution as a risk factor for the development of melasma and other skin disorders of facial hyperpigmentation—Is there a case to be made? J. Drugs Dermatol. 2015;14:337–341. [PubMed] [Google Scholar]
- 241.Shi Y., Zeng Z., Liu J., Pi Z., Zou P., Deng Q., Ma X., Qiao F., Xiong W., Zhou C., et al. Particulate matter promotes hyperpigmentation via AhR/MAPK signaling activation and by increasing α-MSH paracrine levels in keratinocytes. Environ. Pollut. 2021;278:116850. doi: 10.1016/j.envpol.2021.116850. [DOI] [PubMed] [Google Scholar]
- 242.Rajput R. Understanding Hair Loss due to Air Pollution and the Approach to Management. Hair Transpl. 2015;5:133. [Google Scholar]
- 243.Jun M.S., Kwack M.H., Kim M.K., Kim J.C., Sung Y.K. Particulate Matters Induce Apoptosis in Human Hair Follicular Keratinocytes. Ann. Dermatol. 2020;32:388–394. doi: 10.5021/ad.2020.32.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Salem A.S., Ibrahim H.S., Abdelaziz H.H., Elsaie M.L. Implications of cigarette smoking on early-onset androgenetic alopecia: A cross-sectional Study. J. Cosmet. Dermatol. 2021;20:1318–1324. doi: 10.1111/jocd.13727. [DOI] [PubMed] [Google Scholar]
- 245.D’Agostini F., Balansky R., Pesce C., Fiallo P., Lubet R.A., Kelloff G.J., De Flora S. Induction of alopecia in mice exposed to cigarette smoke. Toxicol. Lett. 2000;114:117–123. doi: 10.1016/S0378-4274(99)00268-4. [DOI] [PubMed] [Google Scholar]
- 246.Mistry N. Guidelines for Formulating Anti-Pollution Products. Cosmetics. 2017;4:57. doi: 10.3390/cosmetics4040057. [DOI] [Google Scholar]
- 247.Lee J., Oh S.J., Park S., Park J.H., Lee J.H. Anti-pollution skincare: Research on effective ways to protect skin from particulate matter. Dermatol. Ther. 2021;34:e14960. doi: 10.1111/dth.14960. [DOI] [PubMed] [Google Scholar]
- 248.Peres D.D., Sarruf F.D., de Oliveira C.A., Velasco M.V.R., Baby A.R. Ferulic acid photoprotective properties in association with UV filters: Multifunctional sunscreen with improved SPF and UVA-PF. J. Photochem. Photobiol. B. 2018;185:46–49. doi: 10.1016/j.jphotobiol.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 249.Krutmann J., Schalka S., Watson R.E.B., Wei L., Morita A. Daily photoprotection to prevent photoaging. Photodermatol. Photoimmunol. Photomed. 2021;37:482–489. doi: 10.1111/phpp.12688. [DOI] [PubMed] [Google Scholar]
- 250.Farris P.K., Valacchi G. Ultraviolet Light Protection: Is It Really Enough? Antioxidants. 2022;11:1484. doi: 10.3390/antiox11081484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Grether-Beck S., Marini A., Jaenicke T., Krutmann J. Effective photoprotection of human skin against infrared A radiation by topically applied antioxidants: Results from a vehicle controlled, double-blind, randomized study. Photochem. Photobiol. 2015;91:248–250. doi: 10.1111/php.12375. [DOI] [PubMed] [Google Scholar]
- 252.Diao P., He H., Tang J., Xiong L., Li L. Natural compounds protect the skin from airborne particulate matter by attenuating oxidative stress. Biomed. Pharmacother. 2021;138:111534. doi: 10.1016/j.biopha.2021.111534. [DOI] [PubMed] [Google Scholar]
- 253.Tran H.M., Yang C.Y., Wu T.H., Yen F.L. Liposomes Encapsulating Morin: Investigation of Physicochemical Properties, Dermal Absorption Improvement and Anti-Aging Activity in PM-Induced Keratinocytes. Antioxidants. 2022;11:1183. doi: 10.3390/antiox11061183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.McDaniel D.H., Waugh J.M., Jiang L.I., Stephens T.J., Yaroshinsky A., Mazur C., Wortzman M., Nelson D.B. Evaluation of the Antioxidant Capacity and Protective Effects of a Comprehensive Topical Antioxidant Containing Water-soluble, Enzymatic, and Lipid-soluble Antioxidants. J. Clin. Aesthet. Dermatol. 2019;12:46–53. [PMC free article] [PubMed] [Google Scholar]
- 255.Pecorelli A., McDaniel D.H., Wortzman M., Nelson D.B. Protective effects of a comprehensive topical antioxidant against ozone-induced damage in a reconstructed human skin model. Arch. Dermatol. Res. 2021;313:139–146. doi: 10.1007/s00403-020-02083-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Bocheva G., Slominski R.M., Janjetovic Z., Kim T.K., Böhm M., Steinbrink K., Reiter R.J., Kleszczyński K., Slominski A.T. Protective Role of Melatonin and Its Metabolites in Skin Aging. Int. J. Mol. Sci. 2022;23:1238. doi: 10.3390/ijms23031238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Kleszczyński K., Bilska B., Stegemann A., Flis D.J., Ziolkowski W., Pyza E., Luger T.A., Reiter R.J., Böhm M., Slominski A.T. Melatonin and its metabolites ameliorate UVR-induced mitochondrial oxidative stress in human MNT-1 melanoma cells. Int. J. Mol. Sci. 2018;19:3786. doi: 10.3390/ijms19123786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Slominski A., Pisarchik A., Semak I., Sweatman T., Wortsman J., Szczesniewski A., Slugocki G., McNulty J., Kauser S., Tobin D.J., et al. Serotoninergic and melatoninergic systems are fully expressed in human skin. FASEB J. 2002;16:896–898. doi: 10.1096/fj.01-0952fje. [DOI] [PubMed] [Google Scholar]
- 259.Slominski A.T., Semak I., Fischer T.W., Kim T.K., Kleszczyński K., Hardeland R., Reiter R.J. Metabolism of melatonin in the skin: Why is it important? Exp. Dermatol. 2017;26:563–568. doi: 10.1111/exd.13208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Manchester L.C., Coto-Montes A., Boga J.A., Andersen L.P., Zhou Z., Galano A., Vriend J., Tan D.X., Reiter R.J. Melatonin: An ancient molecule that makes oxygen metabolically tolerable. J. Pineal. Res. 2015;59:403–419. doi: 10.1111/jpi.12267. [DOI] [PubMed] [Google Scholar]
- 261.Galano A., Tan D.X., Reiter R.J. On the free radical scavenging activities of melatonin’s metabolites, AFMK and AMK. J. Pineal Res. 2013;54:245–257. doi: 10.1111/jpi.12010. [DOI] [PubMed] [Google Scholar]
- 262.Hardeland R. Melatonin, Its Metabolites and Their Interference with Reactive Nitrogen Compounds. Molecules. 2021;26:4105. doi: 10.3390/molecules26134105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Reiter R.J., Rosales-Corral S., Tan D.X., Jou M.J., Galano A., Xu B. Melatonin as a mitochondria-targeted antioxidant: One of evolution’s best ideas. Cell. Mol. Life Sci. 2017;74:3863–3881. doi: 10.1007/s00018-017-2609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Fischer T.W., Slominski A., Zmijewski M.A., Reiter R.J., Paus R. Melatonin as a major skin protectant: From free radical scavenging to DNA damage repair. Exp. Dermatol. 2008;17:713–730. doi: 10.1111/j.1600-0625.2008.00767.x. [DOI] [PubMed] [Google Scholar]
- 265.Kilańczyk E., Bryszewska M. The effect of melatonin on antioxidant enzymes in human diabetic skin fibroblasts. Cell. Mol. Biol. Lett. 2003;8:333–336. [PubMed] [Google Scholar]
- 266.Fischer T.W., Kleszczyński K., Hardkop L.H., Kruse N., Zillikens D. Melatonin enhances antioxidative enzyme gene expression (CAT, GPx, SOD), prevents their UVR-induced depletion, and protects against the formation of DNA damage (8-hydroxy-2′-deoxyguanosine) in ex vivo human skin. J. Pineal Res. 2013;54:303–312. doi: 10.1111/jpi.12018. [DOI] [PubMed] [Google Scholar]
- 267.Bielach-Bazyluk A., Zbroch E., Mysliwiec H., Rydzewska-Rosolowska A., Kakareko K., Flisiak I., Hryszko T. Sirtuin 1 and skin: Implications in intrinsic and extrinsic aging-a systematic review. Cells. 2021;10:813. doi: 10.3390/cells10040813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Granger C., Brown A., Aladren S., Narda M. Night Cream Containing Melatonin, Carnosine and Helichrysum italicum Extract Helps Reduce Skin Reactivity and Signs of Photodamage: Ex Vivo and Clinical Studies. Dermatol. Ther. 2020;10:1315–1329. doi: 10.1007/s13555-020-00443-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Sagan D., Stepniak J., Gesing A., Lewinski A., Karbownik-Lewinska M. Melatonin reverses the enhanced oxidative damage to membrane lipids and improves skin biophysical characteristics in former-smokers—A study in postmenopausal women. Ann. Agric. Environ. Med. 2017;24:659–666. doi: 10.5604/12321966.1235174. [DOI] [PubMed] [Google Scholar]
- 270.Furue M., Uchi H., Mitoma C., Hashimoto-Hachiya A., Chiba T., Ito T., Nakahara T., Tsuji G. Antioxidants for Healthy Skin: The Emerging Role of Aryl Hydrocarbon Receptors and Nuclear Factor-Erythroid 2-Related Factor-2. Nutrients. 2017;9:223. doi: 10.3390/nu9030223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Uchi H., Yasumatsu M., Morino-Koga S., Mitoma C., Furue M. Inhibition of aryl hydrocarbon receptor signaling and induction of NRF2-mediated antioxidant activity by cinnamaldehyde in human keratinocytes. J. Dermatol. Sci. 2017;85:36–43. doi: 10.1016/j.jdermsci.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 272.Schäfer M., Werner S. Nrf2—A regulator of keratinocyte redox signaling. Free Radic. Biol. Med. 2015;88:243–252. doi: 10.1016/j.freeradbiomed.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 273.He F., Ru X., Wen T. NRF2, a Transcription Factor for Stress Response and Beyond. Int. J. Mol. Sci. 2020;21:4777. doi: 10.3390/ijms21134777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Arena A., Romeo M.A., Benedetti R., Gilardini Montani M.S., Santarelli R., Gonnella R., D’Orazi G., Cirone M. NRF2 and STAT3: Friends or foes in carcinogenesis? Discov. Oncol. 2023;14:37. doi: 10.1007/s12672-023-00644-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Furue M. Regulation of Filaggrin, Loricrin, and Involucrin by IL-4, IL-13, IL-17A, IL-22, AHR, and NRF2: Pathogenic Implications in Atopic Dermatitis. Int. J. Mol. Sci. 2020;21:5382. doi: 10.3390/ijms21155382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Kim H.B., Um J.Y., Chung B.Y., Kim J.C., Kang S.Y., Park C.W., Kim H.O. Aryl Hydrocarbon Receptors: Evidence of Therapeutic Targets in Chronic Inflammatory Skin Diseases. Biomedicines. 2022;10:1087. doi: 10.3390/biomedicines10051087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Hwang J., Newton E.M., Hsiao J., Shi V.Y. Aryl hydrocarbon receptor/nuclear factor E2-related factor 2 (AHR/NRF2) signalling: A novel therapeutic target for atopic dermatitis. Exp. Dermatol. 2022;31:485–497. doi: 10.1111/exd.14541. [DOI] [PubMed] [Google Scholar]
- 278.Furue M., Hashimoto-Hachiya A., Tsuji G. Aryl Hydrocarbon Receptor in Atopic Dermatitis and Psoriasis. Int. J. Mol. Sci. 2019;20:5424. doi: 10.3390/ijms20215424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Paller A.S., Stein Gold L., Soung J., Tallman A.M., Rubenstein D.S., Gooderham M. Efficacy and patient-reported outcomes from a phase 2b, randomized clinical trial of tapinarof cream for the treatment of adolescents and adults with atopic dermatitis. J. Am. Acad. Dermatol. 2021;84:632–638. doi: 10.1016/j.jaad.2020.05.135. [DOI] [PubMed] [Google Scholar]
- 280.Peppers J., Paller A.S., Maeda-Chubachi T., Wu S., Robbins K., Gallagher K., Kraus J.E. A phase 2, randomized dose-finding study of tapinarof (GSK2894512 cream) for the treatment of atopic dermatitis. J. Am. Acad. Dermatol. 2019;80:89–98. doi: 10.1016/j.jaad.2018.06.047. [DOI] [PubMed] [Google Scholar]
- 281.Bissonnette R., Stein Gold L., Rubenstein D.S., Tallman A.M., Armstrong A. Tapinarof in the treatment of psoriasis: A review of the unique mechanism of action of a novel therapeutic aryl hydrocarbon receptor-modulating agent. J. Am. Acad. Dermatol. 2021;84:1059–1067. doi: 10.1016/j.jaad.2020.10.085. [DOI] [PubMed] [Google Scholar]
- 282.Smith S.H., Jayawickreme C., Rickard D.J., Nicodeme E., Bui T., Simmons C., Coquery C.M., Neil J., Pryor W.M., Mayhew D., et al. Tapinarof Is a Natural AhR Agonist that Resolves Skin Inflammation in Mice and Humans. J. Investig. Dermatol. 2017;137:2110–2119. doi: 10.1016/j.jid.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 283.Furue M., Nakahara T. Revival of AHR Agonist for the Treatment of Atopic Dermatitis: Tapinarof. Curr. Treat. Options Allergy. 2020;7:414–421. doi: 10.1007/s40521-020-00259-7. [DOI] [Google Scholar]
- 284.Vu Y.H., Hashimoto-Hachiya A., Takemura M., Yumine A., Mitamura Y., Nakahara T., Furue M., Tsuji G. IL-24 Negatively Regulates Keratinocyte Differentiation Induced by Tapinarof, an Aryl Hydrocarbon Receptor Modulator: Implication in the Treatment of Atopic Dermatitis. Int. J. Mol. Sci. 2020;21:9412. doi: 10.3390/ijms21249412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Jin S.H., Choi D., Chun Y.J., Noh M. Keratinocyte-derived IL-24 plays a role in the positive feedback regulation of epidermal inflammation in response to environmental and endogenous toxic stressors. Toxicol. Appl. Pharmacol. 2014;280:199–206. doi: 10.1016/j.taap.2014.08.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data appear in the manuscript. For further inquiries, please contact the first author or corresponding author.