Abstract
Objectives: We aimed to evaluate the efficacy and safety of low-dose protamine in reducing access site-related complications during Transcatheter Aortic Valve Implantation (TAVI) as compared to full-dose protamine. Background: Access site-related complications represent an independent predictor of poor outcomes of TAVI. Data regarding heparin reversal with protamine and the dosage needed to prevent bleeding complications are scarce among patients undergoing TAVI. Methods: A total of 897 patients were retrospectively included in the study. Patients who underwent percutaneous coronary intervention within 4 weeks before or concomitantly with TAVI (n = 191) were given 0.5 mg protamine for each 100 units of unfractionated heparin. All other patients (n = 706) were considered as a control group and 1 mg protamine for each 100 units of heparin was administered. Results: The combined intra-hospital endpoint of death, life-threatening major bleeding, and major vascular complications were significantly more frequent in patients receiving low-dose protamine [29 (15.2%) vs. 50 (7.1%), p < 0.001]. After propensity matching (n = 130 for each group) for relevant clinical characteristics including anti-platelet therapy [19 (14.6%) vs. 6 (4.6%), p = 0.006], low-dose protamine predicted the combined endpoint (OR 3.54, 95%-CI 1.36–9.17, p = 0.009), and even in multivariable analysis, low-dose protamine continued to be a predictor of the combined endpoint in the matched model (OR 3.07, 95%-CI 1.17–8.08, p = 0.023) alongside baseline hemoglobin. Conclusions: In this propensity-matched retrospective analysis, a low-dose protamine regime is associated with a higher rate of major adverse events compared to a full-dose protamine regime following transfemoral TAVI.
Keywords: transcatheter aortic valve implantation (TAVI), protamine, vascular complications, bleeding
1. Introduction
The prevalence of aortic valve disease and particularly calcific aortic valve disease is increasing due to the aging population [1]. Since its introduction by Alain Cribier and colleagues in 2002 [2], transcatheter aortic valve implantation (TAVI) has become the primary therapeutic strategy for patients with symptomatic severe aortic stenosis who are at higher surgical risk or those older than 75 years [3], as well as for selected patients with severe aortic regurgitation [4].
Compared with surgical access such as the transapical approach, transfemoral access was associated with mortality and morbidity benefits that justify its use as a mainstream strategy [5,6]. However, despite the advancement of percutaneous closure device technology, access site complications (including bleeding and vascular complications) remain a major concern in transfemoral TAVI [7,8]. Vascular access site-related complications and bleeding are also predictors of poor procedural outcomes [7,9,10]. During the procedure, heparin administration is recommended to maintain an activated clotting time (ACT) of 300 s to reduce thromboembolic risk [11]. Heparin reversal, with protamine sulfate, is associated with reduced major and life-threatening bleeding events in the absence of an increase in thromboembolic events in patients undergoing TAVI [12]. However, the routine practice across centers is variable and data defining indications and the optimal dosing regimen of protamine after TAVI are still scarce.
Therefore, our retrospective analysis aimed to evaluate the efficacy and safety of low-dose protamine compared to full-dose protamine in preventing bleeding and vascular complications in patients undergoing transfemoral TAVI.
2. Methods
2.1. Study Population and Inclusion Criteria
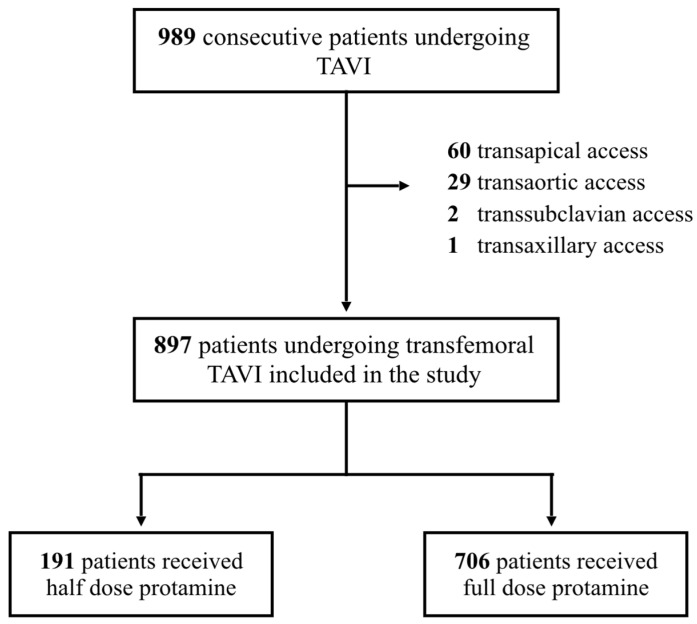
Between January 2015 and December 2020, patients admitted to the Department of Cardiology of the University Hospital of the RWTH Aachen due to severe aortic valve stenosis or severe aortic valve regurgitation who met the criteria for treatment based on the European Society of Cardiology guidelines on valvular heart disease [3] were discussed in our biweekly heart team meeting. The heart team includes an interventional cardiologist, an imaging cardiologist, a cardiovascular surgeon, and an anesthesiologist. Patients were evaluated based upon their medical records, including coronary angiography, pulmonary function, duplex Doppler sonography of the carotid arteries, transthoracic echocardiography, and transoesophageal echocardiography if needed. To estimate the cardiac operative risk, logistic EuroScore, STS-score, and Katz index were documented and patients were subsequently evaluated at the bedside by the heart team. Out of a total of 989 patients accepted for TAVI, 92 were excluded from the current analysis due to non-transfemoral approaches (transapical n = 60, transaortic n = 29, transsubclavian n = 2, transaxillary n = 1). All patients undergoing TAVI via the femoral artery (n = 897) were included in this retrospective study. Further details including patient disposition are demonstrated in Figure 1.
Figure 1.
Study Population.
2.2. Ethical Approval
The protocol for this study as a retrospective analysis of routinely collected data was approved by the local ethics committee (EK 481/21). The study was performed in accordance with the ethical standards defined by the latest version of the Declaration of Helsinki.
2.3. Transcatheter Aortic Valve Implantation (TAVI)
The procedure was carried out by an interventional cardiologist, a cardiothoracic surgeon, and an anesthesiologist. TAVI procedures in our center are carried out under analgesic sedation. Femoral arterial access was guided by using a preoperative computed tomography angiogram of the pelvic vasculature. According to our standard operating procedure, weight-adapted unfractionated heparin was administered before placement of the TAVI introducer sheath. ACT was measured every 20 min and additional heparin was given to maintain ACT above 300. Closure of the access site was performed using either Prostar, Manta, or ProGlide devices. An additional pressure bandage was applied for 12 h following the intervention. Dual anti-platelet therapy was prescribed for 6 months.
2.4. Heparin Reversal
Heparin reversal took place after vascular closure in all patients. The standard dose was 1 mg protamine for every 100 units of unfractionated heparin that were given in the last 30–60 min. In long procedures, 0.75 of protamine was additionally administered per 100 IU of heparin that were given earlier than 60 min. ACT measurements were done both before and after protamine administration. Indications for low-dose protamine included planned PCI during the index procedure or in the 4 weeks prior to the TAVI. ‘Low dose’ protamine was half the usual calculated dose.
2.5. Post-Interventional Care
After the procedure, patients were monitored for 24 h in the intermediate care unit. Transthoracic echocardiography was performed immediately after TAVI and before discharge from our center. All patients underwent a duplex Doppler sonography of the access site of the femoral artery.
2.6. Study Outcomes and Definitions
The classifications of the vascular access site and access-related complications were based on the standardized definitions for important clinical endpoints in TAVI as proposed by the updated consensus document of the Valve Academic Research Consortium from 2012 (VARC-2 criteria) [13]. Primary outcomes were in-hospital (pre-discharge) life-threatening bleeding, major bleeding, major vascular complications, or death from any cause, taken individually or as a combined endpoint. Secondary outcomes consisted of minor bleeding, minor vascular complications, stroke, and myocardial infarction.
2.7. Statistical Analysis
Continuous variables are reported as mean ± standard deviation if normally distributed and median (interquartile ratio) if not normally distributed. Normal distribution was assessed by visual histogram inspection as well as with the Kolgomorov–Smirnov test. Dichotomic variables are reported as a proportion (percentage). The comparison of baseline continuous variables was performed with a t-test for normally distributed variables and with a Mann–Whitney test for non-normally distributed variables; distributions of binary variables were compared with a chi-squared test. In order to assess the association of two different protamine doses with interventional outcomes and complications, we performed a univariable logistic analysis; results are expressed as an odds ratio (OR) with a 95%-confidence interval. In order to adjust for possible confounders, we performed multivariable logistic analysis for the prediction of the combined endpoint, including in the model all variables with p < 0.10 in the univariable analysis (EuroScore, COPD, peripheral artery disease, glomerular filtration rate, hemoglobin levels, LDL levels, coronary artery disease, dual antiplatelet therapy) and then performing backward selection.
To exclude the effects of different baseline characteristics between the two study groups, we performed propensity matching based on sex, age (with a tolerance of ±5 years), and dual antiplatelet therapy. We then repeated our analyses in the matched population.
Analysis was performed with SPSS software. Statistical significance was awarded for p < 0.05.
3. Results
3.1. Baseline Characteristics
A total of 897 patients were included. The median age was 82 (IQR 78-85) years. Men were represented significantly more in the low-dose protamine group at 58.1% (p = 0.005). The average logistic Euroscore, as a predictor for cardiac operative risk and mortality, was significantly higher in patients receiving the low-dose protamine scheme. These patients also had a higher prevalence of coronary artery disease (CAD) (100% vs. 59.5%, p ≤ 0.001) and dual anti-platelet inhibition (40.5% vs. 6.7%, p ≤ 0.001), while other clinical characteristics were comparable between both groups.
Propensity matching was performed on 130 patients from the low-dose protamine group and 130 patients from the full-dose group. After matching, both groups presented similar characteristics regarding the above-mentioned differences, except for CAD which remained higher in the low-dose protamine group. Importantly, no in-between group difference was present regarding anti-coagulatory and anti-platelet therapy. The baseline characteristics of matched patients are presented in Table 1. Patients in both groups received comparable doses of unfractionated heparin (9302 ± 2976 vs. 9024 ± 2471, p = 0.88). In the majority of the patients, A. femoralis was used as an additional vascular access site with no significant difference between both groups (78.8% vs. 83.2%, p = 0.502). There was no difference between the groups in terms of closure device used. (p = 0.574). Further procedural characteristics are presented in Table 2.
Table 1.
Basic Characteristics of Patients Before and After Propensity Matching.
| Before Matching | After Matching | ||||||
|---|---|---|---|---|---|---|---|
| Overall (N = 897) | Protamine full dose (N = 706) | Protamine half dose (N = 191) | p-Value | Protamine full dose (N = 130) | Protamine half dose (N = 130) | p-Value | |
| Median age (IQR)—year | 82 (78–85) | 81 (78–85) | 82 (79–85) | 0.481 | 80 (77–84) | 82 (78–85) | 0.065 |
| Male—no. (%) | 440 (49.1) | 329 (46.6) | 111 (58.1) | 0.005 | 78 (60.0%) | 78 (60.0%) | 1.000 |
| Median logistic EuroSCORE (IQR)—% | 15 (10–23) | 14.5 (10–22) | 18 (11.4–26) | 0.015 | 15.6 (9.6–23.0) | 15.2 (10.5–25.5) | 0.54 |
| COPD—no. (%) | 301 (33.3) | 244 (34.4) | 59 (30.1) | 0.225 | 42 (32.3%) | 44 (33.8%) | 0.301 |
| Diabetes mellitus—no. (%) | 320 (35.7) | 242 (36.1) | 84 (44) | 0.013 | 57 (43.8%) | 44 (33.8%) | 0.098 |
| Hypertension—no. (%) | 709 (79.1) | 560 (79.3) | 149 (78) | 0.787 | 101 (77.7%) | 98 (76.0%) | 0.742 |
| Peripheral artery disease—no. (%) | 140 (15.6) | 98 (13.8) | 42 (22) | 0.006 | 23 (17.7%) | 35 (27.1%) | 0.068 |
| Cerebral artery disease—no. (%) | 273 (30.5) | 207 (29.2) | 67 (35) | 0.121 | 51 (39.2%) | 45 (34.6%) | 0.441 |
| Smoker—no. (%) | 101 (11.3) | 75 (10.6) | 26 (13.6) | 0.246 | 18 (13.8%) | 16 (12.3%) | 0.713 |
| Previous Stroke—no. (%) | 100 (11.1) | 79 (11.1) | 21 (11) | 0.590 | 18 (13.8%) | 18 (13.8%) | 1.000 |
| Median GFR (IQR)—mL/min/1.73 m2 | 56.7 (41–73) | 57 (41–74) | 55.5 (39–69) | 0.757 | 57 (41–71) | 53 (38–69) | 0.527 |
| Median LDL (IQR)—mg/dL | 84 (66–110) | 86.5 (67–112) | 80 (62–101.5) | 0.901 | 85 (63–110) | 78 (61–100) | 0.135 |
| Median Hemoglobin (IQR)—g/dL | 11.9 (11–13) | 11.9 (11–13) | 11.8 (10.3–13) | 0.06 | 12.3 (11.2–13.7) | 11.9 (10.3-13.3) | 0.024 |
| Previous aortic valve replacement—no. (%) | 27 (3) | 23 (3.2) | 4 (2.1) | 0.404 | 3 (2.3%) | 4 (3.1%) | 0.709 |
| Coronary heart disease (CHD)—no. (%) | 609 (67.8) | 420 (59.5) | 189 (100) | <0.001 | 99 (76.2%) | 127 (97.7%) | <0.001 |
| Previous CABG—no. (%) | 83 (9.2) | 71 (10) | 12 (6.3) | 0.11 | 11 (8.5%) | 11 (8.5%) | 1.000 |
| Dual-antiplatelet therapy—no. (%) | 157 (17.5) | 48 (6.8) | 109 (57.1) | <0.001 | 48 (36.9%) | 48 (36.9%) | 1.000 |
| NOAC or VKA—no. (%) | 357 (39.8) | 269 (38.2) | 70 (36.6) | 0.693 | 52 (40.0%) | 42 (32.3%) | 0.197 |
| Indication for NOAC or VKA | <0.001 | ||||||
| Atrial fibrillation—no. (%) | 140 (81.3) | 88 (24.8) | 52 (45.5) | ||||
| Other—no. (%) | 307 (118.7) | 267 (75.2) | 40 (43.5) | ||||
| Concomitant PCI—no. (%) | 60 (31.4) | ||||||
Table 2.
Procedural Characteristics.
| Protamine Full Dose (N = 706) | Protamine Half Dose (N = 191) | p-Value | |
|---|---|---|---|
| UFH (mean ± SD)—IU | 9302 ± 2976 | 9024 ± 2471 | 0.88 |
| Vascular closure device | 0.574 | ||
| Prostar XL—no. (%) | 567 (80.3) | 157 (82.2) | |
| MANTA—no. (%) | 113 (16) | 27 (14.1) | |
| Perclose ProGlide—no. (%) | 5 (0.7) | 1 (0.5) | |
| Stent implantation—no. (%) | 52 (7.4) | 16 (8.4) | 0.629 |
| Additional access site | 0.502 | ||
| A. femoralis—no. (%) | 556 (78.8) | 159 (83.2) | |
| A. radialis—no. (%) | 134 (19) | 29 (15.2) | |
| Transcatheter heart valve | 0.21 | ||
| CoreValve Evolut R/Pro—no. (%) | 619 (88) | 172 (91) | |
| Edwards SAPIEN 3—no. (%) | 46 (6.6) | 8 (42) | |
| Acurate NEO—no. (%) | 31 (5.2) | 9 (4.8) | |
| PCI access site | |||
| A. femoralis—no. (%) | 124 (78) | ||
| A. radialis—no. (%) | 35 (22) |
3.2. Association of Protamine Dose Scheme with Clinical Outcomes
The combined primary intra-hospital endpoint of death, life-threatening major bleeding, and major vascular complications occurred significantly more often in patients receiving low-dose protamine compared to patients treated with full-dose protamine [29 (15.2%) vs. 50 (7.1%), p < 0.001]. In particular, the low-dose protamine group presented a higher incidence of life-threatening [9 (4.7%) vs. 14 (2%), p = 0.034] and major bleeding events [12 (6.3%) vs. 16 (2.3%), p = 0.005]. No significant difference between both groups was observed for stroke and [4 (2.1%) vs. 11 (1.6%), p = 0.608] and myocardial infarction [1 (0.5%) vs. 2 (0.3%), p = 0.610], respectively.
Additional outcomes for both groups are presented in Table 3. A larger blood transfusion volume was observed in patients with low-dose protamine treatment (1.1 ± 3.1 vs. 0.5 ± 1.6 units, p < 0.001).
Table 3.
Primary and Secondary Outcomes Before Propensity Matching.
| Overall (N = 897) | Protamine Full (N = 706) | Protamine Half (N = 191) | p-Value | |
|---|---|---|---|---|
| Primary | ||||
| Combined endpoint | 79 (8.8%) | 50 (7.1%) | 29 (15.2%) | <0.001 |
| In-hospital mortality | 37 (4.1%) | 26 (3.7%) | 11 (5.8%) | 0.200 |
| Life-threatening bleeding | 23 (2.5%) | 14 (2%) | 9 (4.7%) | 0.034 |
| Major bleeding | 28 (3.1%) | 16 (2.3%) | 12 (6.3%) | 0.005 |
| Major vascular complications | 37 (4.1%) | 25 (3.5%) | 12 (6.3%) | 0.091 |
| Secondary | ||||
| Stroke after TAVI | 15 (1.7%) | 11 (1.6%) | 4 (2.1%) | 0.608 |
| Myocardial Infarction | 3 (0.003%) | 2 (0.002%) | 1 (0.005%) | 0.610 |
| Minor bleeding | 124 (13.8%) | 87 (12.2%) | 37 (19.5%) | 0.01 |
| Minor vascular complications | 204 (22.7%) | 157 (22.2%) | 48 (25.1%) | 0.235 |
| In-hospital stay (days) | 17.1 ± 14.1 | 15.9 ± 12.7 | 21.7 ± 17.6 | <0.001 |
| Blood transfusion volume (units) | 0.7 ± 2.0 | 0.5 ± 1.6 | 1.1 ± 3.1 | <0.001 |
Univariable logistic regression analysis was performed to assess the association between low-dose protamine treatment and adverse clinical outcomes. Low-dose protamine treatment significantly predicted the combined endpoint (OR 2.35, 95%-CI 1.44–3.82, p < 0.001) and life-threatening (OR 2.44, 95%-CI 1.04–5.74, p = 0.040) and major bleeding events (OR 2.89, 95%-CI 1.34–6.22, p = 0.007) in Table 4. In univariable logistic regression analysis, EuroScore (OR 1.37 per 10%-variation, 95%-CI 1.13–1.65, p = 0.001) and pre-procedural hemoglobin (OR 0.69 per 1 g/dL, 95%-CI 0.59–0.79, p < 0.001) were able to predict the combined endpoint; details of the univariable analysis are reported in Supplementary Table S1. In multivariable analysis, low-dose protamine treatment remained a significant predictor of adverse outcome (OR 2.07, 95%-CI 1.23–3.47, p = 0.006) alongside with EuroScore and pre-procedural hemoglobin, as reported in Supplementary Table S2.
Table 4.
Univariable Logistic Regression Before Propensity Matching: Low-Dose Protamine Predicted the Combined Endpoint.
| OR (95%-CI) | p-Value | |
|---|---|---|
| Primary Endpoints | ||
| Combined endpoint | 2.35 (1.44–3.82) | <0.001 |
| In-hospital mortality | 1.60 (0.77–3.30) | 0.204 |
| Life-threatening bleeding | 2.44 (1.04–5.74) | 0.040 |
| Major bleeding | 2.89 (1.34–6.22) | 0.007 |
| Major vascular complications | 1.83 (0.90–3.71) | 0.095 |
| Secondary Endpoints | ||
| Stroke after TAVI | 1.35 (0.42–4.29) | 0.609 |
| Minor bleeding | 1.74 (1.14–2.66) | 0.011 |
| Minor vascular complications | 1.14 (0.78–1.66) | 0.488 |
Since the two study groups differed significantly regarding relevant clinical characteristics at baseline, we performed propensity matching of 130 patients from the low-dose protamine group and 130 patients from the full-dose group. Both groups presented with similar characteristics regarding the above-mentioned differences, except for CAD which remained higher in the low-dose protamine group although rates of anticoagulation and anti-platelet therapy were similar. The baseline characteristics of matched patients are presented in Table 1.
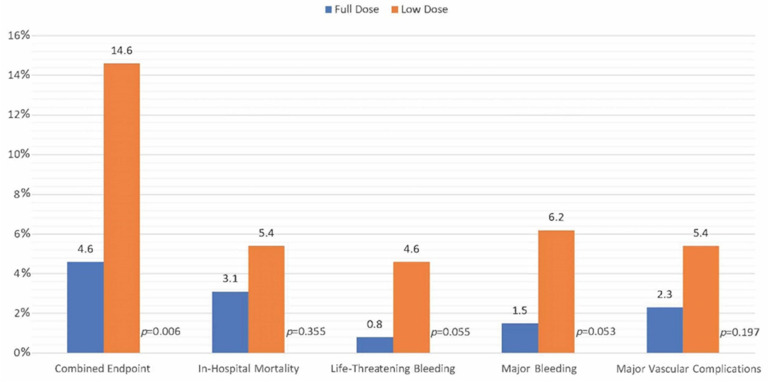
Following propensity matching, low-dose protamine was still significantly associated with a higher incidence of the composite endpoint (OR 3.54, 95%-CI 1.36–9.17, p = 0.009). Details are reported in Figure 2, Table 5 and Table 6. In the univariable logistic regression analysis performed in the matched population, pre-procedural hemoglobin also reached statistical significance as a predictor of the combined endpoint (OR 0.71 per 1 g/dL, 95%-CI 0.56–0.89, p = 0.004); details of this analysis are shown in Supplementary Table S1. Even following propensity matching, in multivariable logistic regression analysis, low-dose protamine remained associated with a higher incidence of the composite endpoint (OR 3.07, 95%-CI 1.17–8.08, p = 0.023) together with pre-procedural hemoglobin (OR 0.73 per 1 g/dl, 95%-CI 0.58–0.93, p = 0.010). Details are shown in Supplementary Table S3.
Figure 2.
Primary and Secondary Outcomes in Matched Model.
Table 5.
Primary and Secondary Outcomes After Propensity Matching.
| Protamine Full (N = 130) | Protamine Half (N = 130) | p-Value | |
|---|---|---|---|
| Primary Endpoints | |||
| Combined endpoint | 6 (4.6%) | 19 (14.6%) | 0.006 |
| In-hospital mortality | 4 (3.1%) | 7 (5.4%) | 0.355 |
| Life-threatening bleeding | 1 (0.8%) | 6 (4.6%) | 0.055 |
| Major bleeding | 2 (1.5%) | 8 (6.2%) | 0.053 |
| Major vascular complications | 3 (2.3%) | 7 (5.4%) | 0.197 |
| Secondary Endpoints | |||
| Stroke after TAVI | 2 (1.5%) | 3 (2.3%) | 0.556 |
| Minor bleeding | 13 (10%) | 27 (20.9%) | 0.015 |
| Minor vascular complications | 32 (24.6%) | 28 (21.5%) | 0.652 |
| In-hospital stay | 15.3 ± 10.2 | 20.3 ± 17.4 | <0.001 |
| Blood transfusion volume (units) | 0.3 ± 0.8 | 1.2 ± 3.2 | 0.003 |
Table 6.
Univariable Logistic Regression After Propensity Matching: Low-Dose Protamine Predicted the Combined Endpoint.
| OR (95%-CI) | p-Value | |
|---|---|---|
| Primary Endpoints | ||
| Combined endpoint | 3.54 (1.36–9.17) | 0.009 |
| In-hospital mortality | 1.79 (0.51–6.28) | 0.361 |
| Life-threatening bleeding | 6.24 (0.74–52.59) | 0.092 |
| Major bleeding | 4.20 (0.87–20.16) | 0.073 |
| Major vascular complications | 2.41 (0.61–9.53) | 0.210 |
| Secondary Endpoints | ||
| Stroke after TAVI | 1.51 (0.25–9.20) | 0.654 |
| Minor bleeding | 2.33 (1.17–4.86) | 0.017 |
| Minor vascular complications | 0.84 (0.47–1.50) | 0.556 |
4. Discussion
Transfemoral TAVI has emerged as an optimal therapy for high-risk patients with aortic stenosis and selected patients with aortic insufficiency. Access site-related complications remain the primary driver of post-interventional morbidity and mortality. In addition to closure devices, heparin reversal by protamine sulfate is an option to reduce access site bleeding, although a standardized dosing scheme during TAVI is lacking. Therefore, the aim of our study was to compare the efficacy of two regularly used doses of protamine in a retrospective analysis.
The major finding of our analysis is that full-dose protamine administration (1:1 protamine/heparin ratio) following transfemoral TAVI was associated with a lower incidence of the combined intra-hospital endpoint of all-cause mortality, major and life-threatening bleeding, as well as major vascular complications when compared with a low-dose protamine scheme (0.5:1 protamine/heparin ratio), mainly due to a significantly lower incidence of major and life-threatening bleeding. First, our data show an overall complication rate mostly comparable to major cohorts [14], especially when outcomes were defined according to VARC-2 criteria [7]. One of the largest registries of aortic stenosis treatment worldwide, the GARY registry, reported in-hospital mortality, major vascular complications, and major bleeding events in 5.2%, 4.1%, and 26.3% of patients following TAVI [15]. The rates of in-hospital mortality and major vascular complications were approximately equal to our data (4.1% for both). However, the rate of life-threatening and major bleeding in the GARY registry was considerably higher than that of our analysis (26.3% vs. 5.6%). It is likely that the difference in rates is accounted for by differences in definitions of major bleeding events. However, overall, our study cohort is representative of real-life data from larger registries.
Although the only existing single-center randomized clinical trial (PS TAVI) on protamine sulfate during TAVI, which was limited by its small sample size (n = 100), provided no evidence for a significant decrease in major and life-threatening bleeding complications among patients who routinely received protamine sulfate as compared to those in the placebo group [16], the use of protamine after cardiac and vascular interventions is routine practice [17,18]. In a meta-analysis of five trials including 6762 patients, protamine was associated with significantly less major bleeding after coronary angioplasty [19]. There also seems to be no greater rate of stent thrombosis after elective PCI when protamine is used [20]. A recent study reported protamine usage to lower significant bleeding and major vascular complications after TAVI without increasing the incidence of thromboembolic events [12]. More robust evidence on the efficacy of routine protamine administration versus selective protamine administration after TAVI is expected when the results of the ongoing ACE PROTAVI randomized double-blind trial are published. Notably, the optimal protamine dose required to prevent major bleeding events after TAVI has not been addressed. Evidence from the field of cardiac surgery suggests that a high dose of protamine sulfate (>1:1) can lead to adverse outcomes with respect to increased bleeding complications due to impaired hemostasis through the downregulation of thrombin generation as well as other side effects of protamine [21,22,23]. On the other hand, a lower dose of protamine (<0.6 mg per 100 IU of heparin) was associated with a reduced need for blood transfusion [20]. A protamine-heparin ratio between 0.6 to 1 was consequently suggested to provide optimal effects on hemostasis and bleeding during cardiothoracic operations [22], with a generally proposed dosing regimen of 1 IU per IU of heparin [24].
Our routine practice of the use of low-dose protamine in patients with recent PCI (0.5:1 protamine/heparin ratio) with the intention of balancing bleeding complications with stent thrombosis offered the opportunity to compare two doses of protamine in a real-world scenario. Patients receiving low-dose protamine experienced a significantly higher rate of the combined intra-hospital endpoint of death, life-threatening major bleeding, and major vascular complications compared with patients receiving full-dose protamine. This was driven by a significantly higher rate of both life-threatening and major bleeding events in the low-dose group, and translated into a higher blood transfusion volume as well as a longer hospital stay.
Whilst it is tempting to speculate that incomplete heparin reversal using the low-dose protamine scheme is insufficient in preventing access site bleeding in patients after TAVI, the conclusion should be tempered by the higher risk profile, as demonstrated by EuroScore and more frequent medication of anti-platelet and anticoagulant agents in those allocated low-dose protamine. In order to control for these baseline differences, we performed propensity matching between both groups, although this was only partially successful given that the primary indication for low-dose protamine was a recent or concurrent coronary intervention. Nevertheless, despite propensity matching, the primary combined endpoint as well as secondary endpoints such as minor bleeding, blood transfusion volume, and the length of hospital stay were still significantly greater in the low-dose group. A multivariable analysis determined that low-dose protamine alongside with EuroScore and baseline hemoglobin predicted the combined endpoint. Even after repeating the same analysis in the matched model, the combined endpoint was predicted only by low-dose protamine and baseline hemoglobin.
With respect to thrombosis, the overall rates of intervention-related stroke and myocardial infarction were extremely low in both study groups. We found no association between stroke rates and the dosage of protamine used. Stent thrombosis was confirmed only in one patient who received low-dose protamine after recent elective PCI, a further two cases of myocardial infarction due to coronary embolism were reported in patients in the full-dose protamine group. Overall, the extremely low rate of thromboembolic complications demonstrates that protamine application, independently of the suggested dosing scheme, seems not to be associated with thrombotic events.
5. Limitations
Despite being the first study assessing two different dosing schemes of protamine following TAVI, the main limitation is the retrospective nature of our analysis and the possible resultant selection bias which partially persists despite propensity matching for relevant clinical characteristics including anti-platelet therapy. Taking this into consideration highlights the role of conducting large randomized clinical trials to validate our results. Furthermore, in spite of the very low incidence of thromboembolic events following protamine administration in our cohort as well as in previous studies, the safety of a high-dose regime in patients who underwent a recent PCI still has to be assessed.
6. Conclusions
In this retrospective propensity-matched study of a large and unselected patient cohort, a low-dose protamine regime (0.5:1 protamine/heparin ratio) was associated with a higher rate of intra-hospital major adverse events compared to a full-dose protamine (1:1 protamine/heparin ratio) after transfemoral TAVI. This may suggest that a complete reversal of the heparin effect is needed to reduce bleeding complications after TAVI. These findings need to be confirmed in a prospective randomized trial.
Abbreviations
| TAVI | Transcatheter Aortic Valve Implantation |
| ACT | Activated Clotting Time |
| STS | Society of Thoracic Surgeons |
| PCI | Percutaneous Coronary Intervention |
| VARC | Valve Academic Research Consortium |
| DAPT | Dual Antiplatelet Therapy |
| CKD | Chronic Kidney Disease |
| BMI | Body Mass Index |
| GARY | German Aortic Valve Registry |
| IU | International Units |
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12134243/s1, Table S1. Univariable Analysis Before and After Matching, Table S2. Multivariable Analysis of the Combined Endpoint, Table S3. Multivariable Analysis of the Combined Endpoint in Matched Models.
Author Contributions
Conceptualization, M.A. and J.S.; methodology, M.A. and K.K.; software, K.K.; validation, K.K. and A.M.; formal analysis, K.K. and A.M.; investigation, J.S.; resources, J.S.; data curation, K.K.; writing—original draft preparation, K.K.; writing—review and editing, K.W., M.L., F.V. and N.M.; visualization, K.K.; supervision, J.S. and M.L.; project administration, K.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by local ethics committee (EK 481/21). The study was performed in accordance with the ethical standards defined by the latest version of the Declaration of Helsinki.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available upon reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
We declare herewith that none of the authors has become funding regarding this article.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Yadgir S., Johnson C.O., Aboyans V., Adebayo O.M., Adedoyin R.A., Afarideh M., Alahdab F., Alashi A., Alipour V., Arabloo J., et al. Global, regional, and national burden of calcific aortic valve and degenerative mitral valve diseases, 1990–2017. Circulation. 2020;141:1670–1680. doi: 10.1161/CIRCULATIONAHA.119.043391. correction in Circulation 2020, 141, e836. [DOI] [PubMed] [Google Scholar]
- 2.Cribier A.G. The odyssey of TAVR from concept to clinical reality. Tex. Heart Inst. J. 2014;41:125–130. doi: 10.14503/THIJ-14-4137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vahanian A., Beyersdorf F., Praz F., Milojevic M., Baldus S., Bauersachs J., Capodanno D., Conradi L., De Bonis M., De Paulis R., et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur. Heart J. 2022;43:561–632. doi: 10.1093/eurheartj/ehab395. [DOI] [PubMed] [Google Scholar]
- 4.Yoon S.-H., Schmidt T., Bleiziffer S., Schofer N., Fiorina C., Munoz-Garcia A.J., Yzeiraj E., Amat-Santos I.J., Tchetche D., Jung C., et al. Transcatheter aortic valve replacement in pure native aortic valve regurgitation. J. Am. Coll. Cardiol. 2017;70:2752–2763. doi: 10.1016/j.jacc.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Blackstone E.H., Suri R.M., Rajeswaran J., Babaliaros V., Douglas P.S., Fearon W.F., Miller D.C., Hahn R.T., Kapadia S., Kirtane A.J., et al. Propensity-matched comparisons of clinical outcomes after transapical or transfemoral transcatheter aortic valve replacement: A placement of aortic transcatheter valves (PARTNER)-I trial substudy. Circulation. 2015;131:1989–2000. doi: 10.1161/CIRCULATIONAHA.114.012525. [DOI] [PubMed] [Google Scholar]
- 6.Gaede L., Blumenstein J., Husser O., Liebetrau C., Dörr O., Grothusen C., Eckel C., Al-Terki H., Kim W.-K., Nef H., et al. Aortic valve replacement in Germany in 2019. Clin. Res. Cardiol. 2021;110:460–465. doi: 10.1007/s00392-020-01788-6. [DOI] [PubMed] [Google Scholar]
- 7.Langouet Q., Martinez R., Saint-Etienne C., Soulami R.B., Harmouche M., Aupart M., Le Breton H., Verhoye J.-P., Bourguignon T. Incidence, predictors, impact, and treatment of vascular complications after transcatheter aortic valve implantation in a modern prospective cohort under real conditions. J. Vasc. Surg. 2020;72:2120–2129.e2. doi: 10.1016/j.jvs.2020.03.035. [DOI] [PubMed] [Google Scholar]
- 8.Ando T., Akintoye E., Telila T., Briasoulis A., Takagi H., Grines C.L., Afonso L. Trends in vascular complications in high-risk patients following transcatheter aortic valve replacement in the United States. Am. J. Cardiol. 2017;119:1433–1437. doi: 10.1016/j.amjcard.2017.01.028. [DOI] [PubMed] [Google Scholar]
- 9.Raju S., Eisenberg N., Montbriand J., Cusimano R.J., Feindel C., Ouzounian M., Horlick E., Osten M., Tsang W., Roche-Nagle G. Vascular complications and procedures following transcatheter aortic valve implantation. Eur. J. Vasc. Endovasc. Surg. 2019;58:437–444. doi: 10.1016/j.ejvs.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 10.Wang J., Yu W., Jin Q., Li Y., Liu N., Hou X., Yu Y. Risk factors for post-TAVI bleeding according to the VARC-2 bleeding definition and effect of the bleeding on short-term mortality: A meta-analysis. Can. J. Cardiol. 2017;33:525–534. doi: 10.1016/j.cjca.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Holmes D.R., Mack M.J., Kaul S., Agnihotri A., Alexander K.P., Bailey S.R., Calhoon J.H., Carabello B.A., Desai M.Y., Edwards F.H., et al. 2012 ACCF/AATS/SCAI/STS expert consensus document on transcatheter aortic valve replacement. J. Am. Coll. Cardiol. 2012;59:1200–1254. doi: 10.1016/j.jacc.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Al-Kassou B., Kandt J., Lohde L., Shamekhi J., Sedaghat A., Tabata N., Weber M., Sugiura A., Fimmers R., Werner N., et al. Safety and efficacy of protamine administration for prevention of bleeding complications in patients undergoing TAVR. JACC Cardiovasc. Interv. 2020;13:1471–1480. doi: 10.1016/j.jcin.2020.03.041. [DOI] [PubMed] [Google Scholar]
- 13.Kappetein A.P., Head S.J., Généreux P., Piazza N., Van Mieghem N.M., Blackstone E.H., Brott T.G., Cohen D.J., Cutlip D.E., Van Es G.-A., et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: The Valve Academic Research Consortium-2 consensus document (VARC-2) Eur. J. Cardiothorac. Surg. 2012;42:S45–S60. doi: 10.1093/ejcts/ezs533. [DOI] [PubMed] [Google Scholar]
- 14.Bendayan M., Messas N., Perrault L.P., Asgar A.W., Lauck S., Kim D.H., Arora R.C., Langlois Y., Piazza N., Martucci G., et al. Frailty and bleeding in older adults undergoing TAVR or SAVR: Insights from the FRAILTY-AVR study. JACC Cardiovasc. Interv. 2020;13:1058–1068. doi: 10.1016/j.jcin.2020.01.238. [DOI] [PubMed] [Google Scholar]
- 15.Walther T., Hamm C.W., Schuler G., Berkowitsch A., Kötting J., Mangner N., Mudra H., Beckmann A., Cremer J., Welz A., et al. Perioperative results and complications in 15,964 transcatheter aortic valve replacements: Prospective data from the GARY registry. J. Am. Coll. Cardiol. 2015;65:2173–2180. doi: 10.1016/j.jacc.2015.03.034. [DOI] [PubMed] [Google Scholar]
- 16.Zbroński K., Grodecki K., Gozdowska R., Ostrowska E., Wysińska J., Rymuza B., Scisło P., Wilimski R., Kochman J., Filipiak K.J., et al. Protamine sulfate during transcatheter aortic valve implantation (PS TAVI)—A single-center, single-blind, randomized placebo-controlled trial. Kardiol. Pol. 2021;79:995–1002. doi: 10.33963/KP.a2021.0070. [DOI] [PubMed] [Google Scholar]
- 17.Stone D.H., Nolan B.W., Schanzer A., Goodney P.P., Cambria R.A., Likosky D.S., Walsh D.B., Cronenwett J.L. Protamine reduces bleeding complications associated with carotid endarterectomy without increasing the risk of stroke. J. Vasc. Surg. 2010;51:559–564.e1. doi: 10.1016/j.jvs.2009.10.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghannam M., Chugh A., Dillon P., Alyesh D., Kossidas K., Sharma S., Coatney J., Atreya A., Yokokawa M., Saeed M., et al. Protamine to expedite vascular hemostasis after catheter ablation of atrial fibrillation: A randomized controlled trial. Heart Rhythm. 2018;15:1642–1647. doi: 10.1016/j.hrthm.2018.06.045. [DOI] [PubMed] [Google Scholar]
- 19.De Luca G., Parodi G., Antoniucci D. Safety and benefits of protamine administration to revert anticoagulation soon after coronary angioplasty. A meta-analysis. J. Thromb. Thrombolysis. 2010;30:452–458. doi: 10.1007/s11239-010-0482-4. [DOI] [PubMed] [Google Scholar]
- 20.Kubota M., Sakakura K., Yamamoto K., Taniguchi Y., Tsukui T., Seguchi M., Wada H., Momomura S.-I., Fujita H. Mid-term clinical outcomes of immediate protamine use following elective percutaneous coronary interventions. Int. Heart J. 2020;61:865–871. doi: 10.1536/ihj.20-126. [DOI] [PubMed] [Google Scholar]
- 21.Meesters M.I., Veerhoek D., de Lange F., de Vries J.-W., de Jong J.R., Romijn J.W.A., Kelchtermans H., Huskens D., van der Steeg R., Thomas P.W.A., et al. Effect of high or low protamine dosing on postoperative bleeding following heparin anticoagulation in cardiac surgery. A randomised clinical trial. Thromb. Haemost. 2016;116:251–261. doi: 10.1160/TH16-02-0117. [DOI] [PubMed] [Google Scholar]
- 22.Boer C., Meesters M.I., Veerhoek D., Vonk A.B.A. Anticoagulant and side-effects of protamine in cardiac surgery: A narrative review. Br. J. Anaesth. 2018;120:914–927. doi: 10.1016/j.bja.2018.01.023. [DOI] [PubMed] [Google Scholar]
- 23.Kunz S.A., Miles L.F., Ianno D.J., Mirowska-Allen K.L., Matalanis G., Bellomo R., Seevanayagam S. The effect of protamine dosing variation on bleeding and transfusion after heparinisation for cardiopulmonary bypass. Perfusion. 2018;33:445–452. doi: 10.1177/0267659118763043. [DOI] [PubMed] [Google Scholar]
- 24.Society of Thoracic Surgeons Blood Conservation Guideline Task Force. Ferraris V.A., Brown J.R., Despotis G.J., Hammon J.W., Reece T.B., Saha S.P., Song H.K., Clough E.R., Shore-Lesserson L.J., et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. Ann. Thorac. Surg. 2011;91:944–982. doi: 10.1016/j.athoracsur.2010.11.078. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request to the corresponding author.