Abstract
Vasovagal syncope (VVS) is common in young adults and is attributed to cerebral hypoperfusion. However, during active stand (AS) testing, only peripheral and not cerebral hemodynamic responses are measured. We sought to determine whether cerebral oxygenation responses to an AS test were altered in young VVS patients when compared to the young healthy controls. A sample of young healthy adults and consecutive VVS patients attending a Falls and Syncope unit was recruited. Continuous beat-to-beat blood pressure (BP), heart rate, near-infrared spectroscopy (NIRS)-derived tissue saturation index (TSI), and changes in concentration of oxygenated/deoxygenated Δ[O2Hb]/Δ[HHb] hemoglobin were measured. BP and NIRS-derived features included nadir, peak, overshoot, trough, recovery rate, normalized recovery rate, and steady-state. Multivariate linear regression was used to adjust for confounders and BP. In total, 13 controls and 27 VVS patients were recruited. While no significant differences were observed in the TSI and Δ[O2Hb], there was a significantly smaller Δ[HHb] peak-to-trough and faster Δ[HHb] recovery rate in VVS patients, independent of BP. A higher BP steady-state was observed in patients but did not remain significant after multiple comparison correction. Young VVS patients demonstrated a similar cerebral circulatory response with signs of altered peripheral circulation with respect to the controls, potentially due to a hyper-reactive autonomic nervous system. This study sets the grounds for future investigations to understand the role of cerebral regulation during standing in VVS.
Keywords: syncope, cerebral oxygenation, standing, near-infrared spectroscopy, orthostatic, young
1. Introduction
Syncope is defined as a transient loss of consciousness due to cerebral hypoperfusion that resolves in a rapid and spontaneous manner [1], with vasovagal syncope (VVS) being its most common form in teenagers and young adults, who rarely experience cardiac syncope [2]. Exaggerated orthostatic cardiovascular responses have been recently observed in patients with VVS, a behavior that has been attributed to a hyper-reactive autonomic nervous system, and hypothesized to bring the body closer to its physiological limit, increasing an individual’s susceptibility to VVS during episodes of hypotension [3,4].
The European Society of Cardiology recommends that patients investigated for VVS undergo the active stand (AS) test with concurrent peripheral hemodynamics monitoring to identify potential syncope-related conditions such as orthostatic hypotension (OH), delayed blood pressure recovery, or postural orthostatic tachycardia syndrome (POTS) [1,5,6].
In complex VVS cases, a head-up tilt (HUT) test is performed [1]. Two recent studies from our group have demonstrated that VVS diagnosis can be predicted from AS cardiovascular responses [5,6]. Despite the obvious differences in these test protocols (AS and HUT), these studies reveal an overlap in the physiological mechanisms that they trigger, suggesting that the AS test might be sufficient to unveil abnormalities in such mechanisms and might assist more in the diagnosis of VVS than currently considered.
In standard practice, cerebral circulation is not directly assessed during the AS and the HUT tests, and only inferred from peripheral signals and orthostatic intolerance symptoms, often being poor surrogates [7,8]. Near-infrared spectroscopy (NIRS) has emerged as a potential tool for the clinical evaluation of syncope [9,10,11], providing measures of cerebral tissue oxygenation. While cerebral oxygenation responses to a HUT test have been characterized in VVS patients, scarce data can be found on the responses to an AS test, with available literature focusing on healthy young individuals [12,13,14], patients with autonomic failure [15] and orthostatic intolerance [16,17], and children with OH, delayed OH, POTS, and VVS [18,19,20]. Despite the crucial role of the AS test in VVS assessment and the increasing interest in the use of NIRS in this context, an important gap can be identified: cerebral oxygenation responses to an AS are yet to be investigated in young patients with VVS.
The aim of this study is to investigate the following research questions: Are there differences in cerebral oxygenation and peripheral hemodynamics measured during an AS test, between young patients with VVS and the healthy controls? Based on previous research [5,6], we hypothesize that VVS patients will have an exaggerated peripheral hemodynamics response to an AS test. Similarly, we hypothesize that a distinctive cerebral oxygenation response will be found in VVS patients as compared to the healthy controls. Differences in the peripheral and cerebral responses to an AS test might represent important biomarkers to identify patients with VVS, further our understanding of their pathophysiology, and aid in their assessment and management.
2. Materials and Methods
2.1. Setting and Participants
Consecutive patients were recruited prospectively from a National Falls and Syncope Unit at St James’s Hospital, Dublin, Ireland. Patients were referred for investigation of suspected syncope or presyncope and had a history of presyncope and/or syncope.
A sample of young healthy community-dwelling controls was also prospectively recruited. The study had ethical approval from the Tallaght University Hospital/St. James’s Hospital Joint Research Ethics Committee, and informed consent was written and signed by all participants.
2.2. Inclusion and Exclusion Criteria
Patients and controls were aged 18–30 years. Patients had a clinical diagnosis of VVS, determined by a clinical expert in syncope. Controls with a history of syncope, cardiovascular disease, or other comorbidities were excluded. All controls were physically fit and were not taking any cardioactive medication. Participants were excluded if they were not able to stand up from a lying position and stay standing for at least 2 min. Women self-reporting pregnancy were excluded.
2.3. Active Stand Testing
2.3.1. Protocol
Participants underwent an AS test as per international guidelines [1,21]. Participants lay supine for 5–10 min until hemodynamic stabilization and were then instructed to stand up as quickly as possible and remain standing quietly for 3 min. Assistance was provided during the stand if necessary.
2.3.2. Equipment
During AS testing, frontal lobe cerebral oxygenation was monitored using NIRS (Portalite, Artinis Medical Systems B.V., Elst, The Netherlands) to derive the values of the tissue saturation index (TSI) (units of percentage (%)) and changes in the concentration of oxyhemoglobin (Δ[O2Hb]) and deoxyhemoglobin (Δ[HHb]) (in µmol/L). The sensor was placed on the left side of the forehead, centered at 3 cm lateral and 3.5 cm above the nasion [22]. An opaque head bandage was applied to provide ambient light protection and minimize sensor motion artifact.
Continuous beat-to-beat blood pressure (BP) (systolic BP (SBP) and diastolic BP (DBP)) and HR were also measured using a Finometer NOVA (Finometer NOVA, Finapres Medical Systems, Amsterdam, The Netherlands). A finger cuff was attached to the middle phalanx of a finger of the left hand, and a height correction unit was applied to correct hydrostatic effects. The Finometer signal was further calibrated using Physiocal™ and brachial calibration based on the average of two oscillometric BP measurements recorded during the resting period. Physiocal™ was turned off on standing to avoid data loss.
2.3.3. Cohort Clinical Characteristics
A comprehensive medical history was recorded and included the following information: anthropometrics (age (years), gender, weight (kg), height (m), cardiovascular diseases, neurological diseases, vestibular disorders, psychological disorders, vertigo and vestibular disorders, obstructive sleep apnea, chronic obstructive airway disease, and endocrine diseases. Behavioral health including smoking status (non-smoker, current smoker, or ex-smoker) and history of excess alcohol intake (>14 units/weeks for women, >21 units/weeks for men) was also recorded. A detailed medication record was also taken at the time of testing.
2.4. Data Analysis
2.4.1. Signal Processing
Custom code was developed in MATLAB R2020a (The Math Works, Inc., MATLAB, Version 2020a, Natick, MA, USA) to process the multimodal physiological data collected as previously described [23,24]. The following biosignals were analyzed: SBP, DBP, HR and TSI, Δ[O2Hb], and Δ[HHb], with a standardized process applied to all biosignals, described in detail in our recent article [25]. A description of the features extracted is detailed in Table 1 and depicted in Figure 1 (Table A1 for an expanded version of features definition). Features extracted included baseline, nadir (or peak in case of Δ[HHb], as it presents an inverted morphology), overshoot (or trough in the case of Δ[HHb]), maximum recovery rate between nadir and overshoot, and steady-state. In NIRS-derived signals (TSI/Δ[O2Hb]/Δ[HHb]), a recovery rate normalized by SBP changes was also derived.
Table 1.
Definitions, units, description of variables used in the analyses.
| Biosignal (Units) | Variable | Description |
|---|---|---|
| SBP (mmHg), HR (bpm), TSI (%) | Baseline | Mean value 30–60 s before standing |
| SBP (mmHg), TSI (%) | Nadir | Largest trough after standing (in first 30 s) |
| SBP (mmHg) | Overshoot | First peak found between SBP nadir time +5 s and 60 s after standing |
| TSI (%) | Overshoot | First peak found between TSI nadir time +2 s and 60 s after standing |
| SBP (mmHg), TSI (%) | Steady-state | Mean value 60–120 s after standing |
| SBP (mmHg), TSI (%) | Delta | Nadir—Baseline |
| SBP (mmHg), TSI (%) | Nadir to overshoot | Overshoot—Nadir |
| SBP (mmHg), TSI (%) | Steady-state change | Steady-state—Baseline |
| SBP (mmHg/s), TSI (%/s) | Maximum recovery rate | Largest difference between consecutive points divided by the time between points (within the time interval between the nadir and overshoot) |
| TSI/SBP (%/mmHg) | Normalized TSI recovery rate | Maximum TSI recovery rate/maximum SBP recovery rate |
HR: heart rate (units: beats per minute (bpm)), SBP: systolic blood pressure (units: mmHg); TSI: tissue saturation index (units: %).
Figure 1.
Features extracted from TSI and SBP responses to an active stand test in a selected participant. Features extracted from the Finometer and NIRS signals (i.e., baseline, nadir, recovery rate, overshoot, and steady—state) are indicated in both graphs. The standing moment is indicated by a black vertical line at t = 0. The baseline value is indicated by a gray dashed line across the graph. SBP = systolic blood pressure, TSI = tissue saturation index.
Duration of supine rest was estimated from the duration of the Finometer recording prior to standing. Speed of standing was obtained by processing the height correction signal to identify the start and stop of the standing maneuver [23].
OH was defined as a sustained (for the duration of the stand) drop from baseline larger than 20 mmHg in SBP and/or a drop larger than 10 mmHg DBP.
2.4.2. Statistical Analysis
Statistical analysis was performed using Rstudio (RStudio Team, 2016, Rstudio: Integrated Development for R. Rstudio, Inc., Boston, MA, USA). All data were assessed for normality using histograms, Q-Q plots, and the Shapiro–Wilk test. Differences in baseline characteristics between healthy participants and patients were assessed using a Mann–Whitney U test to account for the relatively small number of subjects in the study and deviations from normality. A Chi-squared test was used for binary variables. Values are reported as median and interquartile range (IQR). Linear regression was employed to evaluate unadjusted differences in SBP and cerebral oxygenation (Model 1) features between the two groups. Multivariate linear regression was used to adjust for a number of covariates as part of three adjusted models, described in Table 2. Outliers were identified by inspection for abnormal values, incomplete and noisy data, and/or standardized residual greater than 3 [26] Based on this, four outliers were identified, and after sensitivity analyses they were removed from the final analysis. A false discovery rate (FDR) procedure was used to correct for multiple testing comparisons [27]. Differences were considered to be statistically significant for p-value < 0.05.
Table 2.
Correction for covariates in SBP, TSI, Δ[O2Hb], and Δ[HHb] regression analyses.
| Covariates | |
|---|---|
| Model 1 | None |
| Model 2 | Age + Gender |
| Model 3 | Age + Gender + BMI + HR baseline |
| Model 4 | Age + Gender + BMI + HR baseline + SBP concurrent feature * |
* Model 4 only applicable for NIRS variables (TSI, Δ[O2Hb], and Δ[HHb]): e.g., when the dependent variable was “TSI nadir”, then “SBP nadir” was used as a covariate in the model. BMI: body mass index, SBP: systolic blood pressure, TSI: tissue saturation index, Δ[O2Hb]: concentration of oxygenated hemoglobin, Δ[HHb]: concentration of deoxygenated hemoglobin.
Post hoc sensitivity analyses were performed to assess the robustness of the above results to the following factors: (1) adjustment for the effects of standing speed and duration of lying; (2) definition of recovery rate and normalized recovery rate as averaged rates between nadir and overshoot rather than local maxima rates, (3) age and gender matching of a subset of patients to the group of the controls.
3. Results
3.1. Patients’ Characteristics
A total of 40 participants were recruited: 27 patients and 13 controls. A summary of the participants characteristics is presented in Table 3. Participants did not present significant differences in demographic and baseline hemodynamic characteristics, except for the baseline HR, which was significantly higher in VVS patients (76 (14) vs. 66 (16), p = 0.039). There was a higher proportion of women in the patient vs. the control group (78% vs. 54%, p = 0.122). VVS patients presented with different comorbidities (cardiovascular diseases, cholesterol, chronic obstructive airway disease, migraine, depression/anxiety) with eight taking medications. The controls did not have any comorbidities. All patients had either a history of syncope or presyncope in the last year, with 59% and 41% having a history of recurrent syncope and presyncope, respectively.
Table 3.
Participants’ Characteristics.
| Controls (n = 13) |
Patients (n = 27) |
p-Value | |
|---|---|---|---|
| Age (years) | 22 (1) | 21 (6) | 0.220 |
| Female, % (n) | 54 (7) | 78 (21) | 0.122 |
| Weight (kg) | 75 (15) | 69 (17) | 0.496 |
| Height (cm) | 174 (11) | 168 (13) | 0.310 |
| BMI (kg/m2) | 23 (3) | 23 (5) | 0.806 |
| SBP baseline (mmHg) | 132 (22) | 130 (27) | 0.479 |
| DBP baseline (mmHg) | 81 (5) | 77 (18) | 0.875 |
| MAP baseline (mmHg) | 101 (11) | 102 (23) | 0.977 |
| HR baseline (bpm) | 66 (16) | 76 (14) | 0.039 * |
| Cardiovascular diseases, % (n) | 0 | 4 (1) | - |
| Cholesterol, % (n) | 0 | 4 (1) | - |
| Chronic obstructive airway disease, % (n) | 0 | 15 (4) | - |
| Migraine, % (n) | 0 | 15 (4) | - |
| Depression/anxiety, % (n) | 0 | 30 (8) | - |
| Current smokers, % (n) | 23 (3) | 15 (4) | 0.519 |
| Previous smokers, % (n) | 0 | 0 | - |
| History of syncope, % (n) | 0 | 85 (23) | - |
| History of recurrent syncope, % (n) * | 0 | 59 (16) | - |
| History of presyncope, % (n) | 0 | 52 (14) | - |
| History of recurrent presyncope, % (n) * | 0 | 41 (11) | - |
| Presence of OH on standing | 8 (1) | 0 | - |
| Beta-blockers, % (n) | 8 (1) | 4 (1) | - |
| Antidepressants, % (n) | 8 (1) | 11 (3) | - |
| Antihypertensives, % (n) | 0 | 0 | - |
Values expressed as median (interquartile range). * p < 0.05. SBP, DBP, MAP, and HR values were derived from the Finometer measurements, which are calibrated using an oscillometric arm-cuff-based brachial calibration process. Recurrent syncope/presyncope is defined as a history of two or more syncope/presyncope episodes. BMI: body mass index, DBP: diastolic blood pressure, HR: heart rate, MAP: mean arterial pressure, SBP: systolic blood pressure, OH: orthostatic hypotension.
3.2. Univariate Analyses
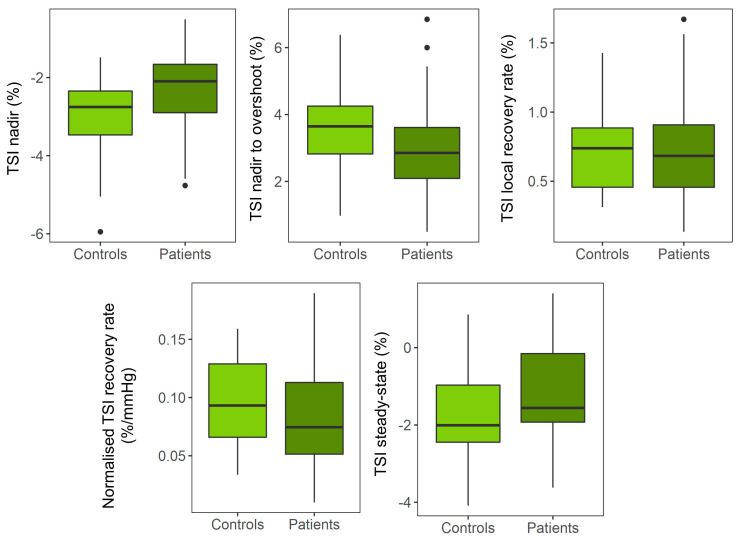
Ensemble average responses are depicted in Figure 2 for both patients and the controls. Analyses revealed a significantly smaller TSI nadir (β: 0.93, CI: [0.12 1.74], p = 0.026) (Table 4, Figure 3) and Δ[O2Hb] nadir (β: 3.62, CI: [0.05 7.19], p = 0.047) (Table A2), which were not significant after FDR correction. VVS patients had an attenuated Δ[HHb] response, both in terms of the peak magnitude (β: −1.09, CI: [2.07 −0.12], p = 0.019) and recovery rate (β: 0.29, CI: [0.09 0.48], p = 0.005) (Table A3). Patients recovered to a higher SBP steady-state value above baseline when compared to the controls (β: 10.80, CI: [3.42–18.17], p = 0.005), which remained significant after correcting for multiple testing (Table A4).
Figure 2.
Average TSI and SBP responses for VVS patients and controls. Average (5% trimmed mean and interquartile range) traces for SBP (mmHg) and TSI (%) relative to baseline for VVS patients (dark color, solid line) and controls (light color, dashed line). Stand occurred at t = 0, indicated by a black vertical line. VVS patients presented a higher SBP value during steady—state (average value during 60–120 s) and smaller initial drop after standing than controls. SBP = systolic blood pressure, TSI = tissue saturation index, VVS = vasovagal syncope.
Table 4.
Univariate (model 1) and multivariate analyses of the effects of group (patients vs. controls (reference)) on TSI responses to active stand testing.
| β Coefficient (CI) | p-Value | FDR Corrected p-Value |
|
|---|---|---|---|
| Model 1 | |||
| TSI nadir (%) | 0.93 (0.12 1.74) | 0.026 * | 0.130 |
| TSI nadir to overshoot difference (%) | −0.53 (−1.55 0.49) | 0.300 | 0.500 |
| Maximum TSI recovery rate (%/s) | −0.04 (−0.30 0.23) | 0.790 | 0.790 |
| Normalized TSI recovery rate (%/mmHg) | −0.01 (−0.04 0.02) | 0.426 | 0.532 |
| TSI baseline to steady-state change (%) | 0.72 (−0.27 1.71) | 0.148 | 0.370 |
| Model 2 | |||
| TSI nadir (%) | 0.84 (0.00 1.68) | 0.050 | 0.250 |
| TSI nadir to overshoot difference (%) | −0.62 (−1.68 0.44) | 0.242 | 0.318 |
| Maximum TSI recovery rate (%/s) | −0.06 (−0.33 0.22) | 0.688 | 0.688 |
| Normalized TSI recovery rate (%/mmHg) | −0.02 (−0.05 0.01) | 0.254 | 0.318 |
| TSI baseline to steady-state change (%) | 0.66 (−0.37 1.69) | 0.202 | 0.318 |
| Model 3 | |||
| TSI nadir (%) | 0.84 (−0.13 1.80) | 0.088 | 0.401 |
| TSI nadir to overshoot difference (%) | −0.77 (−1.98 0.45) | 0.208 | 0.401 |
| Maximum TSI recovery rate (%/s) | −0.15 (−0.46 0.16) | 0.324 | 0.401 |
| Normalized TSI recovery rate (%/mmHg) | −0.02 (−0.05 0.02) | 0.401 | 0.401 |
| TSI baseline to steady-state change (%) | −0.15 (−0.46 0.16) | 0.324 | 0.401 |
| Model 4 | |||
| TSI nadir (%) | 0.73 (−0.27 1.72) | 0.147 | 0.314 |
| TSI nadir to overshoot difference (%) | −0.86 (−2.06 0.35) | 0.157 | 0.314 |
| Maximum TSI recovery rate (%/s) | −0.17 (−0.47 0.14) | 0.282 | 0.376 |
| Normalized TSI recovery rate (%/mmHg) | - | - | - |
| TSI baseline to steady-state change (%) | 0.45 (−0.84 1.73) | 0.484 | 0.484 |
Model 1: univariate, Model 2: model 1 + gender, Model 3: model 2 + gender + body mass index + HR baseline, Model 4: model 3 + corresponding SBP variable. HR: heart rate, SBP: systolic blood pressure, TSI: tissue saturation index. * p < 0.05.
Figure 3.
Differences in TSI between patients and controls for the TSI features analyzed. TSI nadir, TSI nadir to overshoot, maximum TSI recovery rate, normalized TSI recovery rate, and TSI nadir steady—state. None of the differences were significant after correction for multiple testing (see Table 4). TSI = tissue saturation index.
3.3. Multivariate Analyses
A smaller drop was observed in the TSI nadir when correcting for gender, BMI, and baseline HR (Model 3: β: 0.84, CI: [−0.13 1.80], p = 0.080) (Table 4). No associations were observed when further adjusting for the concurrent SBP variable in Model 4. A slower Δ[O2Hb] recovery rate was also observed in patients (β: −0.37, CI: [−0.72 −0.01], p = 0.046), which did not hold significant after the FDR adjustment (Table A2). In the case of Δ[HHb], multivariate analysis yielded similar results to the univariate analysis (Table A3).
Regarding SBP, a significantly higher steady-state value was present in patients after correcting for gender, BMI, and HR baseline (β: 8.37, CI: [0.44 16.30], p = 0.039), which was not significant after the FDR adjustment (Table A4).
3.4. Sensitivity Analyses
Correction for the duration of lying and speed of standing slightly strengthened the TSI association at the nadir (Table A5). Defining the recovery and normalized recovery rates as averaged rates did not impact the associations detected (Table A6). Furthermore, when repeating the analysis with a subset of patients matched with the controls in age and gender, the differences in cerebral oxygenation and SBP were in a similar direction but somewhat reduced (Table A7 and Table A8).
4. Discussion
This study led to the following novel observations: (1) the AS initial cerebral tissue oxygenation response in patients diagnosed with VVS is similar to that of the healthy controls, (2) standing steady-state SBP is higher in VVS patients.
VVS patients presented with an attenuated initial Δ[HHb] response when compared to the controls. These effects were reduced in the age and gender matched subset comparison. Furthermore, no significant associations were observed in the TSI or Δ[O2Hb] responses. To our knowledge, this is the first study that compares AS cerebral oxygenation responses between young VVS patients and the controls. From a group of healthy young adults, Kim et al. observed that those who reported symptoms of orthostatic intolerance during a squat-to-stand test had a slower and more delayed drop rate in total hemoglobin with respect to asymptomatic participants [16]. Lower Δ[O2Hb] initial drops and steady-state values were also reported in children with abnormal (e.g., orthostatic hypotension, VVS) peripheral hemodynamic responses to an AS as compared to a control group [19]. The first study has a similar population to ours, although their squat-to-stand-based protocol may have elicited stronger hemodynamic waves [16], potentially explaining the differences with the current study. The second study investigated a heterogeneous population of children with different orthostatic conditions, which poses a challenge when comparing to our study.
Cerebral oxygenation patterns in patients with VVS have also been studied during the HUT test [9,10,11,28]. These studies have typically demonstrated prolonged lower levels of cerebral oxygenation as measured by NIRS in patients with a positive HUT response when compared to the healthy controls [9,28]. In our study, the primary NIRS changes occurred in the first 30 s after standing while changes during HUT usually occurred over longer windows of time and are at slower rates. These differences are most likely attributed to the differences in the physiological mechanisms triggered by the AS and the HUT, with one involving active muscle contraction and a rapid change in posture and the other one representing a passive and slower orthostatic challenge, respectively.
An alternative method to NIRS to measure cerebral circulation during standing is transcranial doppler (TCD) ultrasonography, which provides a measure of cerebral blood flow velocity (CBFv) in the brain arteries as a surrogate for cerebral blood flow [29]. To the best of the authors’ knowledge, no studies have investigated transient changes in CBFv during active standing in adult patients with VVS. One study performed AS tests in children with syncope symptoms, observing no differences in the orthostatic response between patients and the controls [30]. However, the values were averaged over a 5 min period, and therefore comparison to our study is challenging. Other studies investigating TCD responses to standing in patients with other orthostatic syndromes (POTS and diabetes accompanied by OH) have reported decreases in CBFv associated with symptoms of orthostatic intolerance and decreases in BP [31,32]. Differences in the severity and pathophysiological mechanisms leading to syncope, POTS, and diabetes-related OH might explain the differences with our study.
The shape of the cerebral perfusion response depends on different factors, including the passive effect of the underlying BP waveform and the active modulation of CA. Differences in the initial Δ[HHb] response observed might indicate differences in brain activation between the two cohorts [33], with patients potentially having a less pronounced activation. However, these differences were not reflected in the TSI, with only the drop at the nadir demonstrating a smaller value in patients univariately (β ~1%). When correcting for covariates, despite the association being no longer significant, its magnitude was still relatively large (β ≥ 0.8%), considering that a 5%–10% drop can cause syncope. Therefore, the current study might motivate future research with larger sample sizes to investigate this potential difference. Nevertheless, the current results do not provide enough evidence to support that the overall cerebral tissue oxygenation (TSI) is affected in VVS patients with respect to the healthy controls.
Interestingly, a higher SBP steady-state was observed in patients. Our group previously reported an exaggerated peripheral hemodynamic response to standing in patients with VVS vs. the controls both in young [6] and older adults [5]. This led to the novel hypothesis that patients with VVS may have a hyper-reactive autonomic nervous system [5,6]. Similarly, recent evidence from Brignole et al. demonstrated that VVS patients presented increased resting HR and DBP [34]. The authors proposed that the decreased venous return and stroke volume observed may have led to chronic compensatory increased sympathetic outflow. Here, higher resting HR and exaggerated BP responses were observed in the VVS patient group vs. the controls. These responses may seem protective during an AS, although they might be a sign of potentially enhanced compensatory mechanisms that bring the neurocardiovascular system closer to its physiological limit, requiring a smaller orthostatic challenge to activate the vasovagal reflex and cause VVS (i.e., hyper-reactivity). The lack of correspondence between cerebral oxygenation and SBP might indicate that cerebral autoregulation (CA) is preserved in patients with VVS, although further research is required to better understand whether CA and other regulators of cerebral oxygenation such as PaCO2 could be altered in VVS patients [10].
4.1. Limitations
Firstly, NIRS interpretation is challenging, as the arterial/venous/capillaries proportion of the NIRS signal is unclear, although venous circulation is believed to be the main contributor [10]. Furthermore, NIRS does not provide a global measure; therefore, other regions of the cerebral circulation are not captured. Extracerebral contamination, differences in tissue morphology captured, thickness of extracerebral layers, and susceptibility to motion artifacts are also methodological limitations to consider in NIRS [35,36,37]. Lastly, CO2 is one of the strongest vasoactive molecules that affect the cerebrovasculature and CA [10,38], with PaCO2 correlating to cerebral blood flow. Thus, it remains unclear whether the results found could be attributed to changes in PaCO2 as a result of postural hyperventilation [39,40].
4.2. Strengths
An AS was used instead of the commonly utilized head-up tilt test to study a population with syncope, which provides a simpler and faster way of assessing cerebrovascular regulation upon an orthostatic challenge [41]. The presented application of NIRS is novel and provides a wider picture of an individual’s physiology. Correction for BP has also been applied and allowed investigating the extent of its driving effect. Relative changes from the baseline were investigated, a more accurate and reliable measure when compared to the absolute values of NIRS-derived signals. Furthermore, the influence of the duration of lying and speed of standing was examined, which have been previously demonstrated to influence the responses to an AS [23], but did not alter the results obtained.
5. Conclusions
This study furthers our understanding of transient cerebral and peripheral hemodynamics of VVS patients during standing. Our results suggest cerebral oxygenation is similar while BP demonstrates an exaggerated response, supporting previous evidence of a hyper-reactive autonomic nervous system. The incorporation of new emerging technologies such as NIRS in this clinical context can provide a wider integrative view of the patients beyond traditional approaches, help us better understand their physiology, and further personalize their management.
Acknowledgments
The authors would like to acknowledge participation of all the individuals involved in this study and the contribution of the healthcare professionals at the Falls and Syncope Unit and the Medical Physics and Bioengineering department at St. James’s Hospital, Dublin, Ireland.
Appendix A
Table A1.
Table 1 expanded with all features extracted and calculation method detailed.
| Variable | Units | Description | Calculation Method |
|---|---|---|---|
| SBP baseline | mmHg | Mean SBP 30–60 s before standing | |
| DBP baseline | mmHg | Mean DBP 30–60 s before standing | |
| HR baseline | bpm | Mean HR 30–60 s before standing | |
| TSI baseline | % | Mean TSI 30–60 s before standing | |
| Δ[O2Hb] baseline | µmol/L | Mean Δ[O2Hb] 30–60 s before standing | |
| Δ[HHb] baseline | µmol/L | Mean Δ[HHb] 30–60 s before standing | |
| SBP nadir | mmHg | Largest trough in SBP after standing (within 30 s) |
|
| TSI nadir | % | Largest trough in TSI after standing (within 30 s) |
|
| Δ[O2Hb] nadir | µmol/L | Largest trough in Δ[O2Hb] after standing (within 30 s) |
|
| Δ[HHb] peak | µmol/L | Largest peak in Δ[HHb] after standing (within 30 s) |
|
| SBP overshoot | mmHg | First peak found between 5 s after SBP nadir and 60 s after standing |
|
| TSI overshoot | % | First peak found between 2 s after TSI nadir and 60 s after standing |
|
| Δ[O2Hb] overshoot | µmol/L | First peak found between 2 s after Δ[O2Hb] nadir and 60 s after standing | |
| Δ[HHb] trough | µmol/L | First trough found between 2 s after Δ[HHb] peak and 60 s after standing | |
| SBP steady-state | mmHg | Mean SBP 60–120 s after standing | |
| TSI steady-state | mmHg | Mean TSI 60–120 s after standing | |
| Δ[O2Hb] steady-state | µmol/L | Mean Δ[O2Hb] 60–120 s after standing | |
| Δ[HHb] steady-state | µmol/L | Mean Δ[HHb] 60–120 s after standing | |
| Delta SBP | mmHg | SBP baseline—SBP nadir | SBPB − SBPN |
| Delta TSI | % | TSI baseline—TSI nadir | TSIB − TSIN |
| Delta Δ[O2Hb] | µmol/L | Δ[O2Hb] baseline—Δ[O2Hb] nadir | Δ[O2Hb]B − Δ[O2Hb]N |
| Delta Δ[HHb] | µmol/L | Δ[HHb] baseline—Δ[HHb]peak | Δ[HHb]B − Δ[HHb]P |
| SBP nadir to overshoot difference | mmHg | SBP overshoot—SBP nadir | SBPO − SBPN |
| TSI nadir to overshoot difference | % | TSI overshoot—TSI nadir | TSIO − TSIN |
| Δ[O2Hb] nadir to overshoot difference | µmol/L | Δ[O2Hb] overshoot—Δ[O2Hb] nadir | Δ[O2Hb]O − Δ[O2Hb]N |
| Δ[HHb] peak to through difference | µmol/L | Δ[HHb] trough—Δ[HHb] peak | Δ[HHb]T − Δ[HHb]P |
| SBP steady-state change | mmHg | SBP baseline—SBP steady-state | SBPB − SBPSS |
| TSI steady-state change | % | TSI baseline—TSI steady-state | TSIB − TSISS |
| Δ[O2Hb] steady-state change | µmol/L | Δ[O2Hb] baseline—Δ[O2Hb] steady-state | Δ[O2Hb]B − Δ[O2Hb]SS |
| Δ[HHb] steady-state change | µmol/L | Δ[HHb] baseline—Δ[HHb] steady-state | Δ[HHb]B − Δ[HHb]SS |
| Maximum SBP recovery rate | mmHg/s | In the range between SPB nadir and SBP overshoot: largest difference between consecutive points/time between points | Max((SBPi+1 − SBPi)/(1/fs)), i = nadir index,…, overshoot index |
| Maximum TSI recovery rate | %/s | In the range between TSI nadir and TSI overshoot: largest difference between consecutive points/time between points | Max((TSIi+1 − TSIi)/(1/fs)), i = nadir index,…, overshoot index |
| Δ[O2Hb] maximum recovery rate | µmol/L/s | In the range between Δ[O2Hb] nadir and Δ[O2Hb] overshoot: largest difference between consecutive points/time between points | Max((Δ[O2Hb]i+1 − Δ[O2Hb]i)/(1/fs)), i = nadir index,…, overshoot index |
| Δ[HHb] maximum recovery rate | µmol/L/s | In the range between Δ[HHb] nadir and Δ[HHb] overshoot: largest difference between consecutive points/time between points | Max((Δ[HHb] i+1 − Δ[HHb] i)/(1/fs)), i = nadir index,…, overshoot index |
| Normalized TSI recovery rate | %/mmHg | Maximum TSI recovery rate/maximum SBP recovery rate | TSIRR/SBPRR |
| Normalized Δ[O2Hb] recovery rate | µmol/L/mmHg | Δ[O2Hb] maximum recovery rate/maximum SBP recovery rate | Δ[O2Hb]RR/SBPRR |
| Normalized Δ[HHb] recovery rate | µmol/L/mmHg | Δ[HHb] maximum recovery rate/maximum SBP recovery rate | Δ[HHb]RR/SBPRR |
DBP = diastolic blood pressure, Δ[HHb] = concentration of deoxygenated hemoglobin, HR = heart rate, Δ[O2Hb] = concentration of oxygenated hemoglobin, SBP = systolic blood pressure, TSI = tissue saturation index.
Table A2.
Univariate (model 1) and multivariate analyses of the effects of group (patients vs. controls (reference)) on Δ[O2Hb] responses to active stand testing.
| β Coefficient (CI) | p -Value |
FDR
p -Value |
|
| Model 1 | |||
| Δ[O2Hb] nadir (µmol/L) | 3.62 (0.05 7.19) | 0.047 * | 0.235 |
| Δ[O2Hb] nadir-overshoot difference (µmol/L) | 0.07 (−1.33 1.47) | 0.919 | 0.919 |
| Maximum Δ[O2Hb] recovery rate (µmol/L/s) | −0.10 (−0.47 0.26) | 0.572 | 0.715 |
| Normalized Δ[O2Hb] recovery rate (µmol/L·mmHg) | −0.02 (−0.06 0.02) | 0.292 | 0.487 |
| Δ[O2Hb] baseline to steady-state change (µmol/L) | 2.38 (−2.05 6.82) | 0.284 | 0.487 |
| Model 2 | |||
| Δ[O2Hb] nadir (µmol/L) | 2.87 (−0.60 6.35) | 0.102 | 0.432 |
| Δ[O2Hb] nadir-overshoot difference (µmol/L) | −0.17 (−1.56 1.23) | 0.810 | 0.810 |
| Maximum Δ[O2Hb] recovery rate (µmol/L/s) | −0.14 (−0.52 0.23) | 0.441 | 0.684 |
| Normalized Δ[O2Hb] recovery rate (µmol/L·mmHg) | −0.03 (−0.06 0.01) | 0.173 | 0.432 |
| Δ[O2Hb] baseline to steady-state change (µmol/L) | 1.33 (−3.09 5.74) | 0.547 | 0.684 |
| Model 3 | |||
| Δ[O2Hb] nadir (µmol/L) | 3.24 (−0.67 7.15) | 0.101 | 0.168 |
| Δ[O2Hb] nadir-overshoot difference (µmol/L) | −0.68 (−2.13 0.77) | 0.346 | 0.432 |
| Maximum Δ[O2Hb] recovery rate (µmol/L/s) | −0.37 (−0.72 −0.01) | 0.046 * | 0.168 |
| Normalized Δ[O2Hb] recovery rate (µmol/L·mmHg) | −0.04 (−0.08 0.00) | 0.070 | 0.168 |
| Δ[O2Hb] baseline to steady-state change (µmol/L) | 1.77 (−3.27 6.81) | 0.481 | 0.481 |
| Model 4 | |||
| Δ[O2Hb] nadir (µmol/L) | 2.53 (−1.38 6.45) | 0.197 | 0.263 |
| Δ[O2Hb] nadir-overshoot difference (µmol/L) | −0.88 (−2.22 0.46) | 0.191 | 0.263 |
| Maximum Δ[O2Hb] recovery rate (µmol/L/s) | −0.38 (−0.74 −0.02) | 0.042 * | 0.168 |
| Normalized Δ[O2Hb] recovery rate (µmol/L·mmHg) | - | - | |
| Δ[O2Hb] baseline to steady-state change (µmol/L) | 1.54 (−4.02 7.10) | 0.577 | 0.577 |
Model 1: univariate, Model 2: model 1 + gender Model 3: model 2 + body mass index + HR baseline, Model 4: model 3 + corresponding SBP variable. * p < 0.05. HR = heart rate, Δ[O2Hb] = concentration of oxygenated hemoglobin, SBP = systolic blood pressure.
Table A3.
Univariate (model 1) and multivariate analyses of the effects of group (patients vs. controls (reference)) on Δ[HHb] responses to active stand testing.
| β Coefficient (CI) | p-Value | FDR p-Value |
|
|---|---|---|---|
| Model 1 | |||
| Δ[HHb] peak (µmol/L) | −1.09 (−2.07 −0.12) | 0.029 * | 0.036 * |
| Δ[HHb] peak-to-trough difference (µmol/L) | 0.93 (0.16 1.71) | 0.019 * | 0.032 * |
| Maximum Δ[HHb] recovery rate (µmol/L/s) | 0.29 (0.09 0.48) | 0.005 ** | 0.013 * |
| Normalized Δ[HHb] recovery rate (µmol/L·mmHg) | 0.05 (0.02 0.08) | 0.002 * | 0.010 * |
| Δ[HHb] baseline to steady-state change (µmol/L) | 0.34 (−1.85 2.52) | 0.756 | 0.756 |
| Model 2 | |||
| Δ[HHb] peak (µmol/L) | −1.20 (−2.19 −0.21) | 0.019 * | 0.024 * |
| Δ[HHb] peak-to-trough difference (µmol/L) | 1.02 (0.23 1.805) | 0.013 * | 0.022 * |
| Maximum Δ[HHb] recovery rate (µmol/L/s) | 0.30 (0.10 0.495) | 0.004 ** | 0.010 * |
| Normalized Δ[HHb] recovery rate (µmol/L·mmHg) | 0.05 (0.03 0.083) | 0.001 ** | 0.005 ** |
| Δ[HHb] baseline to steady-state change (µmol/L) | −0.26 (−2.40 1.876) | 0.807 | 0.807 |
| Model 3 | |||
| Δ[HHb] peak (µmol/L) | −0.85 (−1.94 0.24) | 0.123 | 0.154 |
| Δ[HHb] peak-to-trough difference (µmol/L) | 1.24 (0.36 2.12) | 0.007 ** | 0.012 * |
| Maximum Δ[HHb] recovery rate (µmol/L/s) | 0.38 (0.18 0.60) | 0.001 ** | 0.002 ** |
| Normalized Δ[HHb] recovery rate (µmol/L·mmHg) | 0.06 (0.03 0.09) | 0.001 ** | 0.002 ** |
| Δ[HHb] baseline to steady-state change (µmol/L) | −0.17 (−2.6 2.27) | 0.891 | 0.891 |
| Model 4 | |||
| Δ[HHb] peak (µmol/L) | −0.93 (−2.06 0.21) | 0.106 | 0.141 |
| Δ[HHb] peak-to-trough difference (µmol/L) | 1.21 (0.32 2.11) | 0.009 ** | 0.018 * |
| Maximum Δ[HHb] recovery rate (µmol/L/s) | 0.39 (0.17 0.60) | 0.001 ** | 0.004 ** |
| Normalized Δ[HHb] recovery rate (µmol/L·mmHg) | - | - | - |
| Δ[HHb] baseline to steady-state change (µmol/L) | 0.09 (−2.59 2.76) | 0.949 | 0.949 |
Model 1: univariate, Model 2: model 1 + gender Model 3: model 2 + body mass index + HR baseline, Model 4: model 3 + corresponding SBP variable. * p < 0.05, ** p < 0.01. HR = heart rate, Δ[HHb] = concentration of deoxygenated hemoglobin, SBP = systolic blood pressure.
Table A4.
Univariate (model 1) and multivariate analyses of the effects of group (patients vs. controls (reference)) on SBP responses to active stand testing.
| β Coefficient (CI) | p-Value | FDR Corrected p-Value | |
|---|---|---|---|
| Model 1 | |||
| Delta SBP nadir (mmHg) | 5.67 (−4.13 15.47) | 0.249 | 0.249 |
| Delta SBP nadir to overshoot (mmHg) | 5.51 (−3.19 14.20) | 0.207 | 0.249 |
| Maximum SBP recovery rate (mmHg/s) | 1.22 (−0.70 3.14) | 0.205 | 0.249 |
| Delta SBP steady-state (mmHg) | 10.80 (3.42 18.17) | 0.005 * | 0.020 * |
| Model 2 | |||
| Delta SBP nadir (mmHg) | 3.36 (−6.40 13.12) | 0.490 | 0.490 |
| Delta SBP nadir to overshoot (mmHg) | 7.63 (−1.00 16.25) | 0.081 | 0.127 |
| Maximum SBP recovery rate (mmHg/s) | 1.63 (−0.30 3.56) | 0.095 | 0.127 |
| Delta SBP steady-state (mmHg) | 9.34 (1.88 16.80) | 0.016 | 0.064 |
| Model 3 | |||
| Delta SBP nadir (mmHg) | 4.99 (−5.52 15.49) | 0.342 | 0.438 |
| Delta SBP nadir to overshoot (mmHg) | 4.15 (−4.30 12.61) | 0.326 | 0.438 |
| Maximum SBP recovery rate (mmHg/s) | 0.60 (−0.95 2.15) | 0.438 | 0.438 |
| Delta SBP steady-state (mmHg) | 8.37 (0.44 16.30) | 0.039 * | 0.156 |
Model 1: univariate; Model 2: model 1 + gender; Model 3: model 2 + body mass index + HR baseline. * p < 0.05. HR = heart rate, SBP = systolic blood pressure.
Table A5.
Sensitivity analysis to lying duration and speed of standing.
| β Coefficient (CI) | p-Value | FDR Corrected p-Value | |
|---|---|---|---|
| Delta TSI nadir (%) | 1.00 (0.05 1.94) | 0.039 * | 0.195 |
| Delta TSI nadir to overshoot (%) | −0.95 (−2.17 0.27) | 0.121 | 0.258 |
| Maximum TSI recovery rate (%/s) | −0.20 (−0.50 0.11) | 0.203 | 0.258 |
| Normalized TSI recovery rate (%/mmHg) | −0.02 (−0.06 0.02) | 0.283 | 0.283 |
| Delta TSI baseline to steady-state (%) | 0.76 (−0.44 1.95) | 0.206 | 0.258 |
Model: patients vs. healthy + gender + body mass index + HR baseline + lying duration + speed of standing + SBP corresponding feature (for all features except for the normalized TSI recovery rate). HR = heart rate, SBP = systolic blood pressure, TSI = tissue saturation index. * p < 0.05.
Table A6.
Univariate (model 1) and multivariate analyses of the effects of group (patients vs. controls (reference)) on TSI responses to active stand testing using averaged rates for TSI recovery rate and normalized TSI recovery rate.
| β Coefficient (CI) | p-Value | FDR Corrected p-Value |
|
|---|---|---|---|
| Model 1 | |||
| TSI nadir (%) | 0.93 (0.12 1.74) | 0.026 * | 0.130 |
| TSI nadir to overshoot difference (%) | −0.53 (−1.55 0.49) | 0.300 | 0.375 |
| Average TSI recovery rate (%/s) | −0.04 (−0.19 0.11) | 0.587 | 0.587 |
| Normalized TSI recovery rate (%/mmHg) | −0.02 (−0.06 0.02) | 0.285 | 0.375 |
| TSI baseline to steady-state change (%) | 0.72 (−0.27 1.71) | 0.148 | 0.370 |
| Model 2 | |||
| TSI nadir (%) | 0.84 (0.00 1.68) | 0.050 | 0.250 |
| TSI nadir to overshoot difference (%) | −0.62 (−1.68 0.44) | 0.242 | 0.302 |
| Average TSI recovery rate (%/s) | −0.05 (−0.21 0.10) | 0.483 | 0.483 |
| Normalized TSI recovery rate (%/mmHg) | −0.03 (−0.07 0.01) | 0.116 | 0.290 |
| TSI baseline to steady-state change (%) | 0.66 (−0.37 1.69) | 0.202 | 0.302 |
| Model 3 | |||
| TSI nadir (%) | 0.84 (−0.13 1.80) | 0.088 | 0.240 |
| TSI nadir to overshoot difference (%) | −0.77 (−1.98 0.45) | 0.208 | 0.260 |
| Average TSI recovery rate (%/s) | −0.12 (−0.284 0.05) | 0.167 | 0.260 |
| Normalized TSI recovery rate (%/mmHg) | −0.04 (−0.08 0.01) | 0.096 | 0.240 |
| TSI baseline to steady-state change (%) | −0.15 (−0.46 0.16) | 0.324 | 0.324 |
| Model 4 | |||
| TSI nadir (%) | 0.73 (−0.27 1.72) | 0.147 | 0.209 |
| TSI nadir to overshoot difference (%) | −0.86 (−2.06 0.35) | 0.157 | 0.209 |
| Average TSI recovery rate (%/s) | −0.13 (−0.30 0.04) | 0.132 | 0.209 |
| Normalized TSI recovery rate (%/mmHg) | - | - | - |
| TSI baseline to steady-state change (%) | 0.45 (−0.84 1.73) | 0.484 | 0.484 |
Model 1: univariate, Model 2: model 1 + gender, Model 3: model 2 + gender + body mass index + SBP baseline, Model 4: model 3 + corresponding SBP variable. HR = heart rate, SBP = systolic blood pressure, TSI = tissue saturation index. TSI recovery rate is calculated as: (TSI overshoot − TSI nadir)/(TSI overshoot time − TSI nadir time). Normalized TSI recovery rate is calculated as: ((TSI overshoot − TSI nadir)/(TSI overshoot time − TSI nadir time))/((SBP overshoot − SBP nadir)/(SBP overshoot time − SBP nadir time)). HR = heart rate, SBP = systolic blood pressure, TSI = tissue saturation index. * p < 0.05.
Table A7.
Univariate (model 1) and multivariate analyses of the effects of group (patients vs. controls(reference)) on TSI responses to active stand testing using a subcohort of patients matched by age and gender to the controls.
| β Coefficient (CI) | p-Value | FDR Corrected p-Value |
|
|---|---|---|---|
| Model 1 | |||
| Delta TSI (%) | 0.81 (−0.22 1.846) | 0.117 | 0.454 |
| TSI nadir-overshoot difference (%) | −0.61 (−1.95 0.742) | 0.363 | 0.454 |
| TSI recovery rate (%/s) | −0.00 (−0.36 0.350) | 0.981 | 0.981 |
| Normalized TSI recovery rate (%/mmHg) | −0.02 (−0.06 0.020) | 0.343 | 0.454 |
| TSI baseline to steady-state change (%) | 0.54 (−0.58 1.655) | 0.333 | 0.454 |
| Model 3 | |||
| Delta TSI (%) | 0.73 (−0.52 1.98) | 0.238 | 0.697 |
| TSI nadir-overshoot difference (%) | −0.66 (−2.29 0.97) | 0.411 | 0.697 |
| TSI recovery rate (%/s) | −0.08 (−0.50 0.34) | 0.697 | 0.697 |
| Normalized TSI recovery rate (%/mmHg) | −0.01 (−0.05 0.03) | 0.647 | 0.697 |
| TSI baseline to steady-state change (%) | 0.51 (−0.86 1.88) | 0.445 | 0.697 |
| Model 4 | |||
| Delta TSI (%) | 0.68 (−0.62 1.98) | 0.287 | 0.614 |
| TSI nadir-overshoot difference (%) | −0.84 (−2.50 0.83) | 0.307 | 0.614 |
| TSI recovery rate (%/s) | −0.14 (−0.57 0.29) | 0.498 | 0.663 |
| Normalized TSI recovery rate (%/mmHg) | - | - | - |
| TSI baseline to steady-state change (%) | 0.32 (−1.19 1.83) | 0.663 | 0.663 |
Model 1: univariate, Model 3: model 1 + body mass index + HR baseline, Model 4: model 3 + corresponding SBP variable. SBP = systolic blood pressure, TSI = tissue saturation index.
Table A8.
Univariate (model 1) and multivariate analyses of the effects of group (patients vs. controls (reference)) on SBP responses to active stand testing using a subcohort of patients matched by gender to the controls.
| β Coefficient (CI) | p-Value | FDR Corrected p-Value |
|
|---|---|---|---|
| Model 1 | |||
| Delta SBP (%) | 1.25 (−11.92 14.41) | 0.847 | 0.847 |
| SBP nadir-overshoot difference (%) | 10.31 (−0.73 21.35) | 0.066 | 0.088 |
| SBP recovery rate (%/s) | 2.53 (0.14 4.92) | 0.039 * | 0.088 |
| SBP baseline to steady-state change (%) | 9.05 (−0.48 18.58) | 0.062 | 0.088 |
| Model 3 | |||
| Delta SBP (%) | 2.87 (−11.56 17.30) | 0.684 | 0.684 |
| SBP nadir-overshoot difference (%) | 6.65 (−4.44 17.75) | 0.227 | 0.303 |
| SBP recovery rate (%/s) | 1.36 (−0.64 3.36) | 0.173 | 0.303 |
| SBP baseline to steady-state change (%) | 7.83 (−2.56 18.21) | 0.132 | 0.303 |
Model 1: univariate, Model 3: model 1 + body mass index + HR baseline. * p < 0.05. SBP = systolic blood pressure, TSI = tissue saturation index.
Author Contributions
Conceptualization, L.P.-D., R.A.K. and C.F.; methodology, L.P.-D., P.C., A.O., M.D.-O., C.R., R.A.K. and C.F.; formal analysis, L.P.-D.; writing—original draft preparation, L.P.-D.; writing—review and editing, L.P.-D., R.A.K. and C.F. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Tallaght University Hospital/St. James’s Hospital Joint Research Ethics Committee (REC:2018-08, CA,16, date of approval: 31 August 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
C.F. is funded by Endotronix as part of an Industrial Partnership grant. All other authors report no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
The authors would also like to acknowledge the sources of funding: LPD is supported by the Irish Research Council: Government of Ireland Postgraduate Scholarship Programme 2018 (Grant No: GOIPG/2018/134), Dublin, Ireland and the Fundació Universitària Agustí Pedro i Pons, Universitat de Barcelona, Barcelona, Spain; CF holds Science Foundation Ireland and Irish Research Council grants; Grant No: 19/IFA/7409 and Grant No: GOIPG/2018/134, Dublin, Ireland.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Brignole M., Moya A., de Lange F.J., Deharo J.C., Elliott P.M., Fanciulli A., Fedorowski A., Furlan R., Kenny R.A., Martin A., et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur. Heart J. 2018;39:1883–1948. doi: 10.1093/eurheartj/ehy037. [DOI] [PubMed] [Google Scholar]
- 2.Colman N., Nahm K., Ganzeboom K.S., Shen W.K., Reitsma J., Linzer M., Wieling W., Kaufmann H. Epidemiology of reflex syncope. Clin. Auton. Res. 2004;14((Suppl. S1)):9–17. doi: 10.1007/s10286-004-1003-3. [DOI] [PubMed] [Google Scholar]
- 3.Carmody M., Finucane C., Nolan H., Kenny R.A. Combining the Active Stand Test and Pattern Recognition Methods to Predict Vasovagal Syncope. Trinity College Dublin; Dublin, Ireland: 2013. [Google Scholar]
- 4.Sybring M., Finucane C., Nolan H., Kenny R.A. A Convenient Test for Vasovagal Syncope in Older Adults Combining Pattern Recognition and the Active Stand Test. Trinity College Dublin; Dublin, Ireland: 2014. [Google Scholar]
- 5.Carmody M., Finucane C., Nolan H., O’Dwyer C., Kwok M., Kenny R.A., Fan C.W. A Machine Learning Framework to Detect Syncope using the Active Stand. medRxiv. 2020 doi: 10.1101/2020.12.07.20245159. [DOI] [Google Scholar]
- 6.Kwok M., Nolan H., Fan C.W., O’Dwyer C., Kenny R.A., Finucane C. Machine learning for analysis of active stand responses in older adults with vasovagal syncope. medRxiv. 2020 doi: 10.1101/2020.12.07.20241109. [DOI] [Google Scholar]
- 7.Novak P. Orthostatic Cerebral Hypoperfusion Syndrome. Front. Aging Neurosci. 2016;8:22. doi: 10.3389/fnagi.2016.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Claffey P., Pérez-Denia L., Rivasi G., Finucane C., Kenny R.A. Near-infrared spectroscopy in evaluating psychogenic pseudosyncope—A novel diagnostic approach. QJM Int. J. Med. 2019;113:239–244. doi: 10.1093/qjmed/hcz257. [DOI] [PubMed] [Google Scholar]
- 9.Szufladowicz E., Maniewski R., Kozluk E., Zbiec A., Nosek A., Walczak F. Near-infrared spectroscopy in evaluation of cerebral oxygenation during vasovagal syncope. Physiol. Meas. 2004;25:823–836. doi: 10.1088/0967-3334/25/4/004. [DOI] [PubMed] [Google Scholar]
- 10.Lieshout J.J.V., Wieling W., Karemaker J.M., Secher N.H. Syncope, cerebral perfusion, and oxygenation. J. Appl. Physiol. 2003;94:833–848. doi: 10.1152/japplphysiol.00260.2002. [DOI] [PubMed] [Google Scholar]
- 11.Carey B.J., Manktelow B.N., Panerai R.B., Potter J.F. Cerebral autoregulatory responses to head-up tilt in normal subjects and patients with recurrent vasovagal syncope. Circulation. 2001;104:898–902. doi: 10.1161/hc3301.094908. [DOI] [PubMed] [Google Scholar]
- 12.Mol A., Woltering J.H.H., Colier W., Maier A.B., Meskers C.G.M., van Wezel R.J.A. Sensitivity and reliability of cerebral oxygenation responses to postural changes measured with near-infrared spectroscopy. Eur. J. Appl. Physiol. 2019;119:1117–1125. doi: 10.1007/s00421-019-04101-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim Y.S., Bogert L.W., Immink R.V., Harms M.P., Colier W.N., van Lieshout J.J. Effects of aging on the cerebrovascular orthostatic response. Neurobiol. Aging. 2011;32:344–353. doi: 10.1016/j.neurobiolaging.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 14.Immink R.V., Secher N.H., Roos C.M., Pott F., Madsen P.L., Lieshout J.J. The postural reduction in middle cerebral artery blood velocity is not explained by PaCO2. Eur. J. Appl. Physiol. 2006;96:609–614. doi: 10.1007/s00421-006-0136-6. [DOI] [PubMed] [Google Scholar]
- 15.Harms M., Colier W., Wieling W., Lenders J., Secher N., van Lieshout J. Orthostatic Tolerance, Cerebral Oxygenation, and Blood Velocity in Humans with Sympathetic Failure. Stroke. 2000;31:1608–1614. doi: 10.1161/01.STR.31.7.1608. [DOI] [PubMed] [Google Scholar]
- 16.Kim J.-M., Choi J.-K., Choi M., Ji M., Hwang G., Ko S.-B., Bae H.-M. Assessment of cerebral autoregulation using continuous-wave near-infrared spectroscopy during squat-stand maneuvers in subjects with symptoms of orthostatic intolerance. Sci. Rep. 2018;8:13257. doi: 10.1038/s41598-018-31685-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mc Nicholas T., Briggs R., Claffey P., Newman L., Tobin K., Kenny R. Symptoms of orthostatic intolerance and cerebral perfusion-Data from The Irish Longitudinal Study on Ageing (TILDA) J. Hum. Hypertens. 2018;32:693–721. [Google Scholar]
- 18.Endo A., Fujita Y., Fuchigami T., Takahashi S., Mugishima H., Skatani K. Changes in cerebral blood oxygenation induced by active standing test in children with POTS and NMS. Adv. Exp. Med. Biol. 2014;812:253–261. doi: 10.1007/978-1-4939-0620-8_34. [DOI] [PubMed] [Google Scholar]
- 19.Kim Y.T., Tanaka H., Takaya R., Kajiura M., Tamai H., Arita M. Quantitative study on cerebral blood volume determined by a near-infrared spectroscopy during postural change in children. Acta Paediatr. 2009;98:466–471. doi: 10.1111/j.1651-2227.2008.01113.x. [DOI] [PubMed] [Google Scholar]
- 20.Kawaguchi T., Fujita Y., Ishii W., Kimura K., Fukuda A., Fuchigami T., Morioka I. Cerebral Blood Oxygenation Changes in Juvenile Patients with Delayed Orthostatic Hypotension During an Active Standing Test. Adv. Exp. Med. Biol. 2020;1232:85–90. doi: 10.1007/978-3-030-34461-0_12. [DOI] [PubMed] [Google Scholar]
- 21.Finucane C., van Wijnen V.K., Fan C.W., Soraghan C., Byrne L., Westerhof B.E., Freeman R., Fedorowski A., Harms M.P.M., Wieling W., et al. A practical guide to active stand testing and analysis using continuous beat-to-beat non-invasive blood pressure monitoring. Clin. Auton. Res. 2019;29:427–441. doi: 10.1007/s10286-019-00606-y. [DOI] [PubMed] [Google Scholar]
- 22.Klem G.H., Lüders H.O., Jasper H.H., Elger C. The ten-twenty electrode system of the International Federation. The International Federation of Clinical Neurophysiology. Electroencephalogr. Clin. Neurophysiol. Suppl. 1999;52:3–6. [PubMed] [Google Scholar]
- 23.O’Connor J.D., O’Connell M.D.L., Nolan H., Newman L., Knight S.P., Kenny R.A. Impact of Standing Speed on the Peripheral and Central Hemodynamic Response to Orthostasis. Hypertension. 2020;75:524–531. doi: 10.1161/HYPERTENSIONAHA.119.14040. [DOI] [PubMed] [Google Scholar]
- 24.Soraghan C.J., Fan C.W., Hayakawa T., Cronin H., Foran T., Boyle G., Kenny R.-A., Finucane C. TILDA Signal Processing Framework (SPF) for the analysis of BP responses to standing in epidemiological and clinical studies; Proceedings of the IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI); Valencia, Spain. 1–4 June 2014; pp. 793–796. [Google Scholar]
- 25.Pérez-Denia L., Claffey P., Byrne L., Rice C., Kenny R.A., Finucane C. Increased multimorbidity is associated with impaired cerebral and peripheral hemodynamic stabilization during active standing. J. Am. Geriatr. Soc. 2022;70:1973–1986. doi: 10.1111/jgs.17810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Field A., Miles J., Field Z. Discovering Statistics Using R. Sage; Los Angeles, CA, USA: 2013. [Google Scholar]
- 27.Benjamini Y., Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Society. Ser. B (Methodol.) 1995;57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 28.Medow M.S., Kothari M.L., Goetz A.M., O’Donnell-Smith M.B., Terilli C., Stewart J.M. Decreasing cerebral oxygen consumption during upright tilt in vasovagal syncope. Physiol. Rep. 2017;5:e13286. doi: 10.14814/phy2.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aaslid R., Markwalder T.M., Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J. Neurosurg. 1982;57:769–774. doi: 10.3171/jns.1982.57.6.0769. [DOI] [PubMed] [Google Scholar]
- 30.Sung R.Y., Du Z.D., Yu C.W., Yam M.C., Fok T.F. Cerebral blood flow during vasovagal syncope induced by active standing or head up tilt. Arch. Dis. Child. 2000;82:154–158. doi: 10.1136/adc.82.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mankovsky B.N., Piolot R., Mankovsky O.L., Ziegler D. Impairment of cerebral autoregulation in diabetic patients with cardiovascular autonomic neuropathy and orthostatic hypotension. Diabet. Med. 2003;20:119–126. doi: 10.1046/j.1464-5491.2003.00885.x. [DOI] [PubMed] [Google Scholar]
- 32.Harms M.P., van Lieshout J.J. Cerebrovascular and cardiovascular responses associated with orthostatic intolerance and tachycardia. Clin. Auton. Res. 2001;11:35–38. doi: 10.1007/BF02317800. [DOI] [PubMed] [Google Scholar]
- 33.Nakamura K., Shiroto Y., Tamura Y., Koyama K., Takeuchi K., Amanuma M., Nagasawa T., Ozawa S. An increase in the deoxygenated hemoglobin concentration induced by a working memory task during the refractory period in the hemodynamic response in the human cerebral cortex. Neurosci. Lett. 2020;714:134531. doi: 10.1016/j.neulet.2019.134531. [DOI] [PubMed] [Google Scholar]
- 34.Brignole M., Rivasi G., Sutton R., Kenny R.A., Morillo C.A., Sheldon R., Raj S.R., Ungar A., Furlan R., van Dijk G., et al. Low-blood pressure phenotype underpins the tendency to reflex syncope. J. Hypertens. 2021;39:1319–1325. doi: 10.1097/HJH.0000000000002800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen W.-L., Wagner J., Heugel N., Sugar J., Lee Y.-W., Conant L., Malloy M., Heffernan J., Quirk B., Zinos A., et al. Functional Near-Infrared Spectroscopy and Its Clinical Application in the Field of Neuroscience: Advances and Future Directions. Front. Neurosci. 2020;14:724. doi: 10.3389/fnins.2020.00724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yoshitani K., Kawaguchi M., Miura N., Okuno T., Kanoda T., Ohnishi Y., Kuro M. Effects of Hemoglobin Concentration, Skull Thickness, and the Area of the Cerebrospinal Fluid Layer on Near-infrared Spectroscopy Measurements. Anesthesiol. J. Am. Soc. Anesthesiol. 2007;106:458–462. doi: 10.1097/00000542-200703000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Davie S.N., Grocott H.P. Impact of extracranial contamination on regional cerebral oxygen saturation: A comparison of three cerebral oximetry technologies. Anesthesiology. 2012;116:834–840. doi: 10.1097/ALN.0b013e31824c00d7. [DOI] [PubMed] [Google Scholar]
- 38.Thomas K.N., Cotter J.D., Galvin S.D., Williams M.J.A., Willie C.K., Ainslie P.N. Initial orthostatic hypotension is unrelated to orthostatic tolerance in healthy young subjects. J. Appl. Physiol. 2009;107:506–517. doi: 10.1152/japplphysiol.91650.2008. [DOI] [PubMed] [Google Scholar]
- 39.Lieshout J.J.v., Pott F., Madsen P.L., Goudoever J.v., Secher N.H. Muscle Tensing During Standing. Stroke. 2001;32:1546–1551. doi: 10.1161/01.STR.32.7.1546. [DOI] [PubMed] [Google Scholar]
- 40.Immink R.V., Pott F.C., Secher N.H., van Lieshout J.J. Hyperventilation, cerebral perfusion, and syncope. J. Appl. Physiol. 2014;116:844–851. doi: 10.1152/japplphysiol.00637.2013. [DOI] [PubMed] [Google Scholar]
- 41.Sorond F.A., Serrador J.M., Jones R.N., Shaffer M.L., Lipsitz L.A. The sit-to-stand technique for the measurement of dynamic cerebral autoregulation. Ultrasound Med. Biol. 2009;35:21–29. doi: 10.1016/j.ultrasmedbio.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.