Sir,
Reactive arthritis (ReA) is a syndrome characterized by a triad of arthritis, conjunctivitis, and urethritis with specific skin manifestations in the form of circinate balanitis and keratoderma blennorrhagicum. The entity has been linked to HLA-B27 and has either a preceding diarrheal illness or venereal urethritis caused by Chlamydiae trachomatis. We report a case of ReA with circinate balanitis and keratoderma blennorrhagicum, also associated with circinate oral mucositis.
A 42-year-old male presented with 4-weeks history of asymptomatic whitish superficial lesions over the glans penis. The patient had a history of long-standing arthritis of the right knee and ankle joints, along with low back aches accompanied by early morning stiffness lasting for an hour. The lesions were preceded by a history of dysuria 1 month prior. There was no history of cutaneous lesions, oral or genital ulcers, diarrhea, redness of eyes, prior dental procedures, or any history of high-risk sexual behavior. Examination revealed multiple superficial whitish circinate well-defined plaques over the glans penis [Figure 1] and hard palate [Figure 2]. Palms had classical lesions of keratoderma blennorrhagicum characterized by multiple, well-defined, erythematous, crusty to scaly plaques with desquamating edges and surrounding erythema [Figure 3]. Laboratory evaluation revealed pyuria on urine microscopy, but the urine culture was sterile. HLA-B27 was positive, Veneral disease research laboratory (VDRL) and HIV serologies were negative. Magnetic resonance imaging of the spine and large joints was suggestive of sacroiliitis and inflammatory arthritis. The patient was diagnosed with ReA given characteristic joint involvement and specific skin lesions of circinate mucositis (balanitis and oral mucositis) and keratoderma blennorrhagicum. He was managed symptomatically with nonsteroidal anti-inflammatory drugs (NSAIDs) for 4 weeks. However, owing to chronic arthritis, he was started on weekly methotrexate.
Figure 1.

Multiple whitish circinate well-defined plaques over the glans penis
Figure 2.
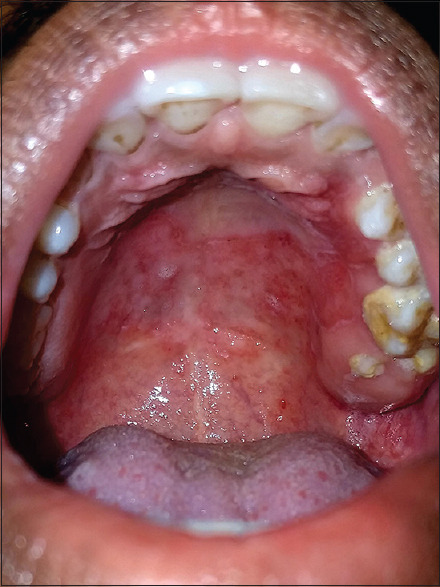
Whitish circinate well-defined plaques over hard palate reminiscent of circinate oral mucositis
Figure 3.

Palmar lesions of keratoderma blennorrhagicum
ReA is a specific form of seronegative spondylo-arthritis first described in 1916 by “Fiessinger and Leroy” and “Hans Reiter.” A triad of ocular, articular, and urethral inflammation with specific cutaneous lesions in the form of keratoderma blennorrhagicum and circinate mucositis constitute ReA.[1,2] A strong association with HLA-B27 (60%–70%) is seen beside an antecedent enteric infection or venereal urethritis 2–4 weeks before onset. Enteric pathogens include Yersinia, Shigella, and Campylobacter, the more common predisposing infection; on the other hand, Chlamydia trachomatis urethritis less commonly causes sexually acquired reactive arthritis (SARA). Pathogenesis is still elusive, yet HLA-B27-carrying antigen-presenting cells like macrophages are activated by infectious triggers to form unfolded protein response (UPR). UPRs arthritogenic proteins subsequently activate T-cell immune response, causing inflammation. Nonspecific skin lesions include the geographic tongue, skin, and nail lesions that mimic psoriasis clinically and on histopathology.[3] Diagnostic criteria for reactive arthritis proposed by the American College of Rheumatology include the following:[4]
-
Major criteria
-
Arthritis with the presence of two of the following:
- Asymmetrical
- Mono or oligoarthritis
- Predominantly lower limb involvement.
-
Preceding symptomatic infection with 1 of the following:
- Enteritis (diarrhea for at least 1 day, up to 3 days to 6 weeks before onset of arthritis)
- Urethritis (dysuria or discharge for at least 1 day, up to 3 days to 6 weeks before onset of arthritis).
-
-
Minor criteria
-
Evidence of triggering infection:
- Positive nucleic acid amplification test (NAAT) for chlamydia in the morning urine or urethral/cervical swab
- Positive stool culture for enteric pathogens associated with reactive arthritis.
- Evidence of persistent synovial infection (positive immunohistology or PCR for Chlamydia).
-
Definite ReA is diagnosed when both major criteria and one minor criterion are present. Diagnosis of ReA is probable when both major criteria but no minor criteria; or one major and one minor criterion are fulfilled. Investigations include complete blood count, urine analysis, erythrocyte sedimentation rate, c-reactive protein, NAAT for C. trachomatis, and screening for STIs. An HLA-B27 serology is usually done owing to strong affiliation besides radiological and serological tests to rule out other spondyloarthritides. ReA is mostly a self-limiting disease seldom requiring long-term treatment. NSAIDs, preferably selective COX-2 inhibitors, are used. SARA requires a month-long course of antibiotics. Chronic disease of the joints or eyes warrants disease-modifying anti-rheumatoid drugs such as methotrexate and sulfasalazine. At present, biologics like TNF-α inhibitors and Janus-kinase inhibitors have been used with promising results.[5]
We report a rare case of circinate balanitis and circinate oral mucositis occurring simultaneously in a patient of ReA. Circinate lesions in the oral cavity, vulva and cutaneous circinate lesions, though less frequent, should be thought of when encountering a case of ReA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rovira-López R, Bertolín-Colilla M, Pujol RM. Circinate oral and genital mucositis. JAAD Case Rep. 2018;4:622–4. doi: 10.1016/j.jdcr.2018.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fakih O, Biguenet A, Gallais Sérézal I, Aubin F. Cutaneous manifestation of reactive arthritis. Joint Bone Spine. 2020;87:658. doi: 10.1016/j.jbspin.2020.06.010. [DOI] [PubMed] [Google Scholar]
- 3.Jubber A, Moorthy A. Reactive arthritis: A clinical review. J R Coll Physicians Edinb. 2021;51:288–97. doi: 10.4997/JRCPE.2021.319. [DOI] [PubMed] [Google Scholar]
- 4.Selmi C, Gershwin ME. Diagnosis and classification of reactive arthritis. Autoimmun Rev. 2014;13:546–9. doi: 10.1016/j.autrev.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Carlin E, Marzo-Ortega H, Flew S. British Association of Sexual Health and HIV national guideline on the management of sexually acquired reactive arthritis 2021. Int J STD AIDS. 2021;32:986–97. doi: 10.1177/09564624211020266. [DOI] [PubMed] [Google Scholar]


