Abstract
In response to concerns about healthcare access and long wait times within the Veterans Health Administration (VA), Congress passed the Choice Act of 2014 and the Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act of 2018 to create a program for patients to receive care in non-VA sites of care, paid by VA. Questions remain about the quality of surgical care between these sites in specific and between VA and non-VA care in general. This review synthesizes recent evidence comparing surgical care between VA and non-VA delivered care across the domains of quality and safety, access, patient experience, and comparative cost/efficiency (2015 to 2021). Eighteen studies met the inclusion criteria. Of 13 studies reporting quality and safety outcomes, 11 reported that quality and safety of VA surgical care were as good as or better than non-VA sites of care. Six studies of access did not have a preponderance of evidence favoring care in either setting. One study of patient experience reported VA care as about equal to non-VA care. All 4 studies of cost/efficiency outcomes favored non-VA care. Based on limited data, these findings suggest that expanding eligibility for veterans to get care in the community may not provide benefits in terms of increasing access to surgical procedures, will not result in better quality, and may result in worse quality of care, but may reduce inpatient length of stay and perhaps cost less.
Comparisons of Veterans Health Administration (VA)–delivered care settings with non-VA care settings are key to assessing the quality of care available for veterans and informing policymakers on the impact of VA-paid community care.
The Veterans Health Administration (VA) is the nation’s largest integrated healthcare system, providing care for millions of US military veterans. Concerns about quality of care in the 1990s led to the construction of the VA NSQIP, an innovative effort to measure and share risk-adjusted surgical outcomes to spur improvement efforts.1-3 Despite success reducing perioperative morbidity and mortality, veteran perceptions of inadequate access and lower quality of care remained. Congress passed the Veteran Access, Choice, and Accountability (“Choice”) Act of 2014, allowing veterans to seek care in non-VA hospitals and clinics paid by the VA if wait time was greater than 30 days or if they lived greater than 40 miles from the closest VA. This program also required independent performance assessments of VA’s healthcare services related to access and available expertise. The Choice Act funding ended in 2017 and was followed by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act of 2018 that further expanded access to care in the community and created a long-term program for VA-reimbursed non-VA care options.4,5
The Choice and MISSION Acts greatly expanded eligibility for VA-reimbursed non-VA care, but questions remain about the quality of care provided by different sites. Although previous reviews comparing surgical outcomes between VA and non-VA care found that the VA performed similarly to or better than non-VA care in most, but not all, aspects of clinical quality, their included studies predated Choice and MISSION Act implementation.6,7 In addition, little is known about the impact of these acts on additional domains of healthcare quality including access to care, patient experience, and comparative costs.8 To address these gaps, we conducted a systematic review to compare recent studies of the clinical quality and safety, access, patient experience, and cost of surgical care between the VA and non-VA care.
METHODS
This manuscript is a condensed version of a larger report prepared for the VA.9 The aim was to perform a systematic review to compare VA and non-VA quality of care for surgical conditions. The review is reported using the Preferred Reporting Items for Systematic reviews and Meta-Analyses standards, and the larger review was registered in PROSPERO: CRD42022314154.
Data sources/study selection
The searches included PubMed from January 2015 to December 2021 using terms relating to “Veterans health” and “community health services” or “private sector” (Supplemental Digital Content 1, http://links.lww.com/JACS/A242). Additional articles were identified from reference lists in consultation with content experts. We limited the search to published and indexed articles involving human subjects available in the English language.
All steps were conducted independently in duplicate by team members (MB, GS, JK, JGU), and disagreements were reconciled through group discussions. Titles passed to abstract stage if they were deemed relevant by at least 1 person. Studies were included at either the abstract or the full-text level if they were original research of any design and compared the quality of care provided to veterans in the VA compared with non-VA care among veterans or non-VA care among the general population. All surgical specialties were included.
Team members dually abstracted the following data: study design and years, sample size, geographic representativeness, outcomes, and statistical methods. Two senior members of the team with clinical and systematic review experience guided the procedures (MM-G, PS).
Assessment of data quality
We used a quality assessment tool adapted from previous reviews comparing quality of care across 2 health systems to distinguish between studies reporting results in which we have more confidence from those with lesser confidence.10 First, we evaluated whether the time frame in the VA and non-VA samples were contemporaneous; second, we determined how the samples were selected and whether they were representative of national/large regional samples or small, limited, unequal, or nonrepresentative samples; third, we assessed whether the outcome measures were identical or sufficiently similar to permit a valid comparison; and fourth, we evaluated whether the sample sizes were sufficiently robust and used appropriate statistical methods to support a valid comparison (Supplemental Digital Content 2, http://links.lww.com/JACS/A242). Studies were included in the review if all quality criteria were met. Studies were grouped into categories based on their quality assessment: those that had no obvious flaws limiting internal or external validity (“good quality” studies), and those that had some flaws limiting internal or external validity (“fair quality” studies). In cases with 2 studies on the same procedure(s) with the same or similar outcomes, we indicated which study was relatively stronger in the results text and signified the relatively lesser strength study with a small circle on the evidence map.
Synthesis of results
Because of the heterogeneity in the comparison groups, outcome domains, and procedure types, pooling the data in a meta-analysis was not possible, so a narrative synthesis was performed. Six domains of healthcare quality from a 2001 Institute of Medicine report were collapsed across categories into 4 groups: (1) clinical quality and safety, (2) access, (3) patient experience, and (4) cost and efficiency. Outcomes were classified into 1 of these 4 domains. Equity was a sixth Institute of Medicine domain, where studies had to statistically test for differences between groups of interest; we found no studies comparing VA care with non-VA care on equity. If multiple cost outcomes were reported, total cost was used. One study may include multiple outcomes spanning different domains. Given the multitude of studies reporting quality and safety outcomes, this domain is further reported by surgical discipline.
RESULTS
Description of the evidence
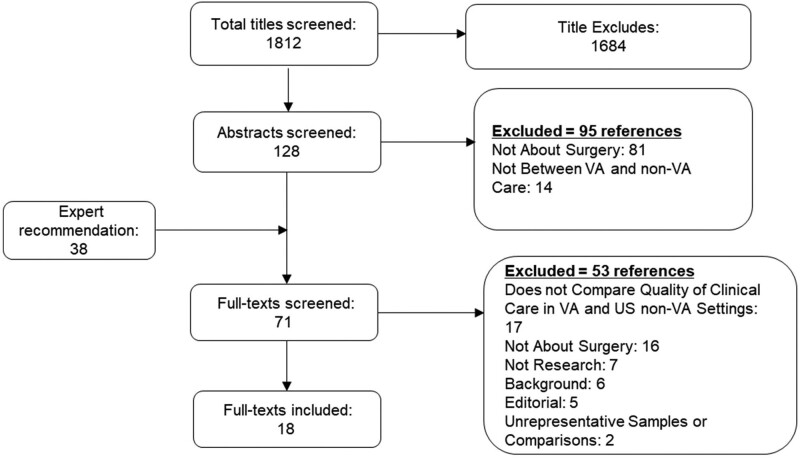
Eighteen studies were included in our review (Fig. 1). The majority of studies analyzed surgery- or patient-level outcomes on specific conditions or operations (16 of 18), and 2 studies reported hospital-level surgical outcomes. The procedures reported included orthopaedic surgery (6 studies), cataract surgery (3 studies), pulmonary resections (2 studies), kidney transplant (2 studies), and coronary artery bypass grafting (CABG; 1 study). In addition, 1 study analyzed all noncardiac surgeries, and 1 evaluated access in urologic and orthopaedic outpatient clinics.
Figure 1.
Literature flow of evidence comparing quality of surgical care in Veterans Health Administration (VA) vs non-VA settings.
Source data in all studies ranged from 1999 to 2019. There were 3 main comparisons cited in the literature: veterans receiving VA care compared with (1) veterans getting VA-paid non-VA care (including through Choice/MISSION Act community care programs; 7 studies), (2) veterans getting non-VA care not paid for by VA (1 study), and (3) a general population getting non-VA care (10 studies; eg comparison using VA NSQIP vs Medicare data). The comparison of veterans in the VA compared with VA-paid non-VA care was the strongest comparison that most directly addressed the review’s objective.
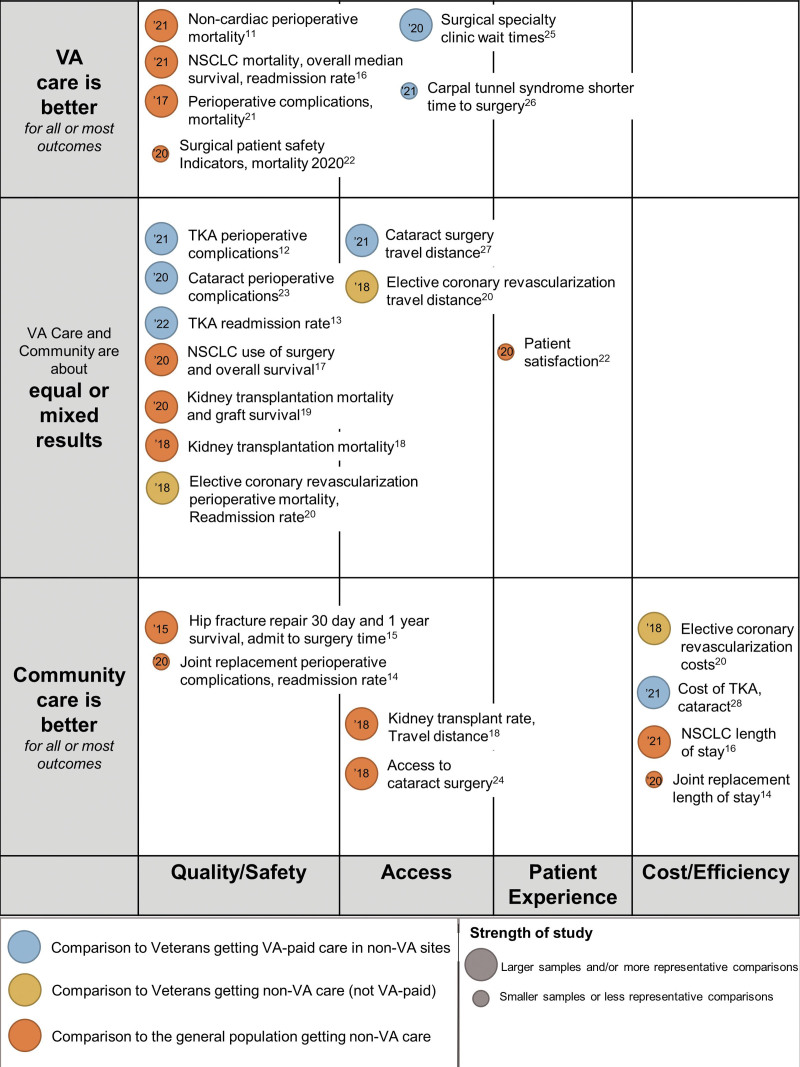
Key findings from each study were organized into 4 quality domains and are presented in the following order: (1) quality and safety; (2) access; (3) patient experience; and (4) cost and efficiency (Fig. 2; Supplemental Digital Content 4, http://links.lww.com/JACS/A242). Most studies (12 of 18) reported outcomes in only 1 quality domain, 4 studies covered 2 domains, and 1 study reported 3 domains. Five studies reported findings in multiple domains.
Figure 2.
Evidence map of published studies comparing quality of surgical care in Department of Veterans Affairs (VA) vs non-VA settings. NSCLC, non-small cell lung cancer; TKA, total knee arthroplasty; VA, Veterans Health Administration.
Risk of bias
Among the 18 included studies meeting all our risk of bias criteria, 3 were deemed fair quality studies. See Supplemental Digital Content 2 for the complete risk of bias table (http://links.lww.com/JACS/A242).
Quality and safety
Thirteen studies reported quality and safety outcomes that cover a broad range of procedures and will be discussed individually by surgical specialties including orthopaedic (4 studies), lung resection (2 studies), kidney transplant (2 studies), CABG (1 study), cataract surgery (1 study), and noncardiac surgeries (1 study); 2 additional studies reported hospital-level patient safety indicators; see Table 1.
Table 1.
Quality and Safety Outcomes in Veterans Affairs vs Non-Veterans Affairs Care
| Author, year |
Operation, national setting |
Comparison | N | Quality/safety | ||
|---|---|---|---|---|---|---|
| George and colleagues, 202111 | Noncardiac surgery | 30-d mortality, N (%) | 30-d complication, N (%) | Failure to rescue, N (%) | ||
| VA pt | 73,6477 | 8,008 (1.1) | 125,816 (17.1) | 5,918 (4.7) | ||
| Gen pop (Ref) | 3,174,274 | 2,602 (0.8) | 299,984 (9.5) | 19,936 (6.7) | ||
| RR 0.59 (0.47–0.75)* | RR 0.55 (0.44–0.68)* | |||||
| Harris and colleagues, 202112 | TKA | Any complication, N (%) | Joint/wound infection, N (%) | PE, N (%) | ||
| VA pt | 24,407 | 712 (2.9) | 236 (1.0) | 193 (0.8) | ||
| Non-VA pt (Ref) | 18,964 | 611 (3.2) | 128 (0.7) | 109 (0.6) | ||
| OR 0.45 (0.38–0.54)* | OR 0.69* | OR 0.73 (p < 0.01)* | ||||
| Rosen and colleagues, 202113 | TKA | All-cause readmission rate, % | TKA-related readmission rate, % | |||
| VA pt | 25,384 | 4.3 | 1.3 | |||
| Non-VA pt (Ref) | 19,990 | 4.6 | 1.2 | |||
| RR 0.35 (0.30–0.40)* | RR 0.30 (0.23–0.38)* | |||||
| Frisch and colleagues, 202014 | TKA | 30-d complication, N (%) | DVT, N (%) | 30-d readmit, N (%) | ||
| VA pt | 10,460 | 908 (9) | 152 (1.5) | 1,773 (17) | ||
| Gen pop (Ref) | 58,820 | 1,608 (3) | 414 (0.7)† | 1,955 (3) | ||
| OR 2.58 (2.31–2.89)† | OR 4.94 (4.51–5.41)† | |||||
| Hutt and colleagues, 201515 | Hip fracture repair | 30-d survival, % | 1-y survival, % | Admit to surgery time, d, mean (SD) | ||
| VA pt (Ref) |
947 | 89.65 | 63.04 | 5.64 (43.25) | ||
| OR 1.701 (1.184–2.445)† | OR 1.504 (1.208–1.872)† | |||||
| Medicare | 947 | 92.93 | 70.43 | 1.78 (2.35)† | ||
| Heiden and colleagues, 202116 | Lung resection | 30-d mortality, N (%) | Median overall survival, mo | 30-d readmit, N (%) | ||
| VA pt | 6,792 | 128 (1.9)‡ | 71.4‡ | 523 (7.70) | ||
| Non-VA pt | 6,792 | 188 (2.8) | 65.2 | 470 (7.02)NS | ||
| Williams and colleagues, 202017 | Lung cancer treatment | Surgical treatment only, N (%) | Chemotherapy only, N (%) | 5-y overall survival, % | ||
| VA Black race vs White race (Ref) |
7,895 | 3,648 (46.2) | 181 (2.3) | HR 1.08 (1.00–1.16) | ||
| OR 0.73 (0.62–0.86) | ||||||
| Gen pop Black race vs White race (Ref) |
8,744 | 4,454 (50.9) | 171 (2.0) | HR 1.17 (1.06–1.30) | ||
| OR 0.57 (0.47–0.70) | ||||||
| Augustine and colleagues, 201818 | Kidney transplant | Mortality | Delisting | |||
| VA pt | 2,905 | |||||
| Private (Ref) | 3,751 | HR 1.00 (0.83–1.20)NS | HR 1.23 (1.003–1.50)NS | |||
| Medicare (Ref) | 3,109 | HR 0.81 (0.68–0.96)* | HR 0.82 (0.68–0.99)* | |||
| Kesseli and colleagues, 202019 | Kidney transplant | 30-d mortality, O/E | 1-y graft survival, O/E | |||
| VA pt | 1,508 | 3/11.3 (0.26) | 78/97.8 (0.79) | |||
| O/E adj 0.27 (0.05–0.65)* | O/E adj 0.79 (0.63–0.98)NS | |||||
| Gen pop | 227,680 | 1,348/1,340 (1.01) | 14,185/14,149 (1.00) | |||
| O/E 1.00 (0.95–1.06) | O/E adj 1.00 (0.98–1.02) | |||||
| Barnett and colleagues, 201820 | CABG | 30-d mortality, N (%) | 30-d readmit, N (%) | |||
| VA pt | 4,866 | 77 (1.50) | 346 (7.12) | |||
| Non-VA pt (Ref) | 952 | 12 (1.26) | 79 (8.25) | |||
| RR 0.89 (0.45–1.77)NS | RR 1.16 (0.89–1.50)NS | |||||
| Blay and colleagues, 201721 |
Surgical PSI | Failure to rescue, N/1,000 discharges (CI) | Wound dehiscence, N/1,000 discharges (CI) | VTE/PE, N/1,000 discharges (CI) | ||
| VA hospital | 129 | 105.82 (96.7–114.92)* | 2.17 (1.64–2.71)NS | 3.94 (3.42–4.45)* | ||
| Non-VA pt | 4,010 | 136.34 (135.42–137.26) | 2.32 (2.30–2.33) | 5.08 (5.00–5.15) | ||
| Eid and colleagues, 202022 | Surgical PSI | Postop mortality, N/1,000 pts | Wound dehiscence, N/1,000 pts | VTE/PE, N/1,000 pts | ||
| VA hospital | 34 | 95* | 0.29* | 3.56NS | ||
| Non-VA pt | 319 | 167 | 0.83 | 4.05 | ||
| Rosen and colleagues, 202123 | Cataract | 30-d complication complex surgery, N (%) | 30-d complication routine surgery, N (%) | 90-d complication, N | ||
| VA pt (Ref) | 44,546 | 164 (1.61) | 313 (0.65) | 704 | ||
| RR 0.94 (0.70–1.27)NS | RR 0.91 (0.74–1.16)NS | OR 0.918 (0.765–1.097)NS | ||||
| Non-VA pt | 17,203 | 58 (1.52) | 131 (0.59) | 276 | ||
Data shown as 95% CI and mean (SD) unless otherwise specified. NS, p > 0.05.
Significantly favors VA.
Significantly favors non-VA.
Significantly favors VA in unadjusted analysis.
CABG, coronary artery bypass graft; CI, confidence interval; HR, hazard ratio; IQR, interquartile range; LOS, length of stay; N, number; O/E, observed/expected ratio; OLS coeff, ordinary least squares coefficient; OR, odds ratio; PSI, patient safety indicators; RR, relative risk; TKA, total knee arthroplasty; VA, Veterans Health Administration; VTE/PE, venous thromboembolism/pulmonary embolism.
Orthopaedic
Three studies reported outcomes for veterans undergoing elective joint replacement (hip [THA] and knee [TKA]), and 1 included outcomes for hip fracture repair. All met risk of bias criteria.
Harris and colleagues reported that 24,407 VA patients (from corporate data warehouse [CDW]) had about half the odds of developing any complication (eg joint or wound infection, myocardial infarction, pulmonary embolism; adjusted OR of any complication 0.45, 95% CI 0.38 to 0.54) compared with 18,964 veterans who underwent TKAs in VA-paid non-VA care (Medicare claims during 2017 to 2019).12 However, in their local facility-level comparison, the adjusted odds of complications were higher in 5 of 130 VA facilities compared with their non-VA counterpart sites (approximate ORs 1.8 to 2.6, 95% CI 1.1 to 4.6).
The second study of joint replacement outcomes from 2016 to 2019 by Rosen and colleagues reported considerably lower readmissions nationally among 25,384 Veterans compared with 19,990 Veterans in VA-paid non-VA care using combined VA CDW and Medicare data (adjusted OR for all-cause readmissions 0.35, 95% CI 0.30 to 0.40).13 This trend varied at 3 individual non-VA sites that had lower readmissions compared with their corresponding VA hospitals (approximate ORs 2.3 to 3.1, 95% CI 1.0 to 7.9]).
The third study of joint replacements found that VA care (n = 10,460) had substantially higher adjusted odds of complications (2.58, 95% CI 2.31 to 2.89) and readmissions (4.94, 95% CI 4.51 to 5.41) after elective primary TKA and total hip arthroplasty at 30 days compared with 58,820 NSQIP database patients in 2014.
A study of timeliness of surgery and survival found that after hip fracture in patients 65 and older, veterans (n = 947; VA-NSQIP data) waited an average of 4 more days for surgery in the VA compared with propensity-matched general population patients in non-VA care (n = 947; Medicare data) from 2003 to 2005 (mean admission date to date of surgery in VA 5.64, SD 43.25 and Medicare 1.78, SD 2.35). The Medicare cohort also had 70% higher odds of 30-day survival on average.15
Lung resection
Two studies discussed quality and safety outcomes for veterans undergoing pulmonary resection and/or non–small cell lung cancer treatment.
Heiden and colleagues16 found that veterans in the VA (CDW data) had a small but significantly lower 30-day mortality rate that persisted at 90 days compared with a matched general non-VA population in the National Cancer Database between 2006 and 2016 (VA 1.9% vs non-VA 2.8%, p < 0.001). Veterans receiving care in the VA also had longer adjusted median overall survival by about 6 months (71.4 vs 65.2 months, p < 0.001); they found no difference in unadjusted readmissions.
In a second study designed to assess racial disparities in management and outcomes of stage I non–small cell lung cancer between Black and White patients, Williams and colleagues compared 7,895 Veterans from VA CDW data with 8,744 general population patients in the Surveillance, Epidemiology, and End Results (SEER)–Medicare database from 2001 to 2009.17 They found that among patients who received treatment, Black veterans in the VA (adjusted OR 0.73, 95% CI 0.62 to 0.86) and Black general population patients in non-VA cohorts (adjusted OR 0.57, 95% CI 0.47 to 0.70) were less likely to receive surgery compared with their White peers. When these findings were adjusted for treatment received and other patient-level covariates, there was no disparity in 5-year overall survival between Black and White patients in either setting.
Kidney transplant
Two studies evaluated kidney transplant quality and safety outcomes.
Augustine and colleagues analyzed transplant rates, mortality, and delisting (ie removal from waitlist for reasons other than transplant or death) in 2,905 veterans across 4 VA transplant centers with 3,751 privately insured and 3,109 Medicare patients in non-VA transplant centers from 2004 to 2016 in the Scientific Registry of Transplant Recipients database.18 Compared with privately insured patients, veterans in VA care had a lower hazard ratio (HR) for obtaining deceased and living donor transplants combined (adjusted HR 0.72, 95% CI 0.65 to 0.79) and a slightly higher HR for delisting (adjusted HR 1.23, 95% CI 1.003 to 1.50), but they had no difference in adjusted mortality rates. Compared with Medicare patients, veterans in VA care had a lower hazard ratio for mortality (adjusted HR 0.81, 95% CI 0.68 to 0.96) and were less likely to be removed from the waitlist (adjusted HR 0.82, 95% CI 0.68 to 0.99).
In a second study using the same database, Kesseli and colleagues found significantly lower observed vs expected 30-day kidney transplant mortality rate in the 7 VA centers (n = 1,508 veterans) vs 286 non-VA centers (n = 117,680) (observed vs expected VA 0.27, 95% CI 0.05 to 0.65; observed vs expected non-VA 1.00, 95% CI 0.95 to 1.06, p = 0.03).19 In contrast, 3-year mortality and graft survival were not different between the VA and matched non-VA centers.
CABG
Barnett and colleagues studied elective coronary revascularization in veterans younger than 65 years for 4,866 patients in VA hospitals and 952 veterans in non-VA sites using VA claims data, and they found no difference in mortality and readmissions.20
Cataract surgery
One study reported similar adjusted 90-day complications for veterans undergoing complex and routine cataract surgeries in the VA (n = 44,546) compared with eterans obtaining VA-paid non-VA care (n = 17,203) (OR 0.918, 95% CI 0.765 to 1.097) from 2014 to 2015.23
Noncardiac surgery
George and colleagues compared mortality after noncardiac surgery between VA NSQIP (n = 3,174,274) and NSQIP (n = 736,477).11 The authors found that VA care was associated with lower risk of overall postoperative death (adjusted relative risk 0.59, 95% CI 0.47 to 0.75; p < 0.001) and lower risk of postoperative death after a complication (adjusted relative risk 0.55, 95% CI 0.44 to 0.68).
Patient safety indicators
Two studies used Hospital Compare data to evaluate VA hospital patient safety indicators with those reported by non-VA hospitals. Between 2012 and 2015, Blay and colleagues found lower postoperative inpatient deaths from a treatable complication in the 129 VA hospitals compared with 4,010 non-VA hospitals (VA: 105.8 deaths per 1,000 discharges, 95% CI 96.7 to 114.92; non-VA: 136.34 deaths per 1,000 discharges, 95% CI 135.42 to 137.26) and a slightly lower postoperative venous thromboembolism rate in the VA by about 1 per 1,000 discharges, but they reported no difference in wound dehiscence rates.21
Similar to Blay and colleagues, Eid and colleagues reported lower postoperative inpatients deaths from treatable complications in VA hospitals (n = 34) compared with non-VA hospitals (n = 319).22 There were no differences in venous thromboembolism rates; however, lower wound dehiscence rates were observed among VA hospitals.
Access
We identified 6 studies reporting healthcare access. Three studies described time to care (2 on time to surgery, 1 wait time to specialty appointment) and 3 studies measured geographic access in terms of distance to the provider (Supplemental Digital Content 3, http://links.lww.com/JACS/A242); all met risk of bias criteria.
Time to care
Wu and colleagues measured the proportion of 1,917,254 veterans and 1,156,211 Medicare patients with a documented cataract diagnoses who received cataract surgery within 1 and 5 years after diagnosis from 2002 to 2012.24 Compared with Medicare patients, about one-third fewer veterans underwent surgery for cataracts within 1 year (VA 6.3% vs non-VA 18.5%; adjusted OR for receiving surgery [VA ref] 3.39, 95% CI 3.36 to 3.41) and 5 years (VA 12.6%, non-VA 35.9%; adjusted OR 3.89, 95% CI, 3.87 to 3.91). This study did not assess the reasons patients did not undergo cataract surgery.
Griffith and colleagues compared wait times to specialty appointments among veterans in VA care vs Veterans in VA-paid non-VA care using VA administrative data from 2013 to 2019 (orthopaedic patients, VA 506,945 and non-VA 139,827; urology patients, VA 353,019 and non-VA 37,089).25 Mean wait times declined during the study period among both groups, but on average, they were 6 days shorter in VA sites for orthopaedics (VA 36.2 days [SD 9.3] vs non-VA 43.6 days [SD 12.9]) and 14 days shorter in VA sites for urology compared with non-VA sites (VA 36.1 days [SD 9.5] vs non-VA 50.5 days [SD 14.5]).
The third study of time to care described time from carpal tunnel referral to surgery.26 Veterans treated only within the VA had shorter median time from primary care referral to carpal tunnel release by about 200 days compared with the group with mixed VA plus VA-paid non-VA care.
Geographic access
Two national studies found travel distance to be longer for VA care and 1 with similar outcomes between VA and non-VA care; all of these studies met our risk of bias criteria.
Augustine and colleagues (discussed above in Quality and Safety) reported median distance to the 4 matched kidney transplant centers from veteran residences.18 Transplants at a VA required nearly an 8-fold greater travel distance at 347.0 miles (interquartile range 196.9 to 701.8) vs 42.5 miles (interquartile range 12.9 to 101.1) for non-VA privately insured patients and 55.6 miles (interquartile range 16.4 to 102.6) for non-VA Medicare patients. Similarly, the included study by Barnett and colleagues of CABG operations found that compared with veterans at VA hospitals, net travel distance was 73.3 miles less for veterans receiving care at non-VA hospitals.20
In a study using 2015 CDW data, Pettey and colleagues calculated median travel distances nationally for veterans undergoing cataract surgery to be 31.2 miles for VA vs 19.7 miles for VA-paid non-VA sites.27
Patient experience
As described previously, Eid and colleagues used Hospital Consumer Assessment of Healthcare Providers patient satisfaction scores in 2018 in 3 regions and found no differences in overall hospital rating. However, the VA performed slightly worse when patients were asked if they would recommend the hospital compared with general population patients at non-VA hospitals.22
Cost and efficiency
Two studies reported cost outcomes for total knee arthroplasty, cataract surgery, and elective CABG; all met the risk of bias criteria. Two studies reported efficiency measures as length of stay. All study designs were described previously.
Costs
A study by Wagner and colleagues compared VA hospital vs VA-paid non-VA total knee arthroplasties and cataract surgeries using VA Corporate Data Warehouse data from 2017 to 2018.28 The mean total unadjusted inpatient cost of total knee arthroplasty was substantially higher in VA care (6,179 VA patients: $28,969, SD $10,778; vs 6,337 veterans in VA-paid non-VA care: $13,339, SD $23,698), and the pattern persisted after controlling for location of service and patient factors. Findings were the same for outpatient cataract surgeries, with the adjusted model demonstrating that compared with VA-paid non-VA care, VA hospital cataract procedures cost $2,680 more (SE 15.8).
Barnett and colleagues (described previously) found a lower mean adjusted total cost of elective CABG in veterans receiving VA-paid non-VA care by $8,525, which included index procedure, readmission, and extra travel costs compared with VA care (VA: $65,264, SD $47,978 vs non-VA: $56,749, SD $77,283, p < 0.01).20
Length of stay
Veterans at VA hospitals experienced longer lengths of stays compared with general population patients in 2 studies. For example, mean length of stay after lung resection was 1 day longer for veterans (VA: 8.12 days, SD 6.59; non-VA: 7.08 days, SD 7.54, p > 0.001).16 After elective total hip arthroplasty, a higher proportion of patients in the VA sample had a length of stay of 4 days or greater (47% vs 17%, p < 0.001).14
DISCUSSION
Our systematic review of studies of surgical care comparing quality and safety, access, patient experience, and cost across several surgical specialties found that in all but 2 studies, VA care had comparable or better quality and safety outcomes than non-VA care. For access to care, we found that neither VA nor non-VA care was consistently better. Studies of patient experience are too limited to draw conclusions, and the few studies of cost and efficiency outcomes favored non-VA care.
This is the first such review to include data since the implementation of the Choice and MISSION Acts’ community care program. There were 3 such studies evaluating quality and safety outcomes for complications and readmissions after TKA procedures. Although the studies found that on average VA outcomes were better than non-VA care nationally, comparisons at individual sites of care identified a few individual VAs performing worse than their non-VA counterparts in the community. These well-designed studies indicate that focusing on VA’s performance in the context of their local healthcare environment may be important for providers and veterans making decisions about seeking care in the community. Notably, of the 2 studies comparing wait times, both reported that VA wait times were less than wait times for care in the community. Last, the 1 study comparing orthopaedic procedure costs found that care in the community, which was bid out by VA at Medicare rates, was less than the estimated cost to deliver the same care within the VA.
Importantly, mortality outcomes compared between sites of care mirrored the overall findings. One study of veterans in non-VA care had equivalent mortality after CABG, and 5 other studies comparing mortality with general populations of patients were distributed between lower mortality in the VA (after lung resection, noncardiac surgery, and surgical inpatient deaths) or a mixture of the VA having lower and no difference in mortality (2 studies of kidney transplant); there were no cases of lower mortality in non-VA care among the high-quality studies. These findings contrast with previous reviews that found a small minority of studies with higher mortality in the VA compared with non-VA sites.29 The updated evidence suggesting parity in mortality outcomes in these risk-adjusted studies may reflect progress in quality improvement at VA sites.
Limitations
Beyond the usual limitation of any systematic review and of the included studies, we had several additional limitations. First, there was the possibility of publication bias or subconscious investigator bias, because most of the published studies were written by VA authors. We scrutinized each study for objective evidence of bias and diminished the degree to which studies with such bias contributed to our overall conclusions. Second, there was the possibility of confounding by patient populations in VA or non-VA care. Studies attempted to control for this through multivariable methods, but VA patients generally have worse comorbidities and unmeasured social determinants of health30,31 than those in the community, so any bias introduced via insufficient case-mix adjusting is more likely to favor non-VA care. Third, we were limited by how different stakeholders may value our included outcomes. We did not attempt to rank different outcomes (eg wait times or provider ratings) by importance, because this assessment could differ by stakeholder. Finally, the outcomes and operations presented may not be generalizable to all surgical procedures. For example, common outpatient operations (eg knee replacements, cataract surgery) were more heavily investigated in the literature given how the Choice and MISSION Acts may uniquely impact them.
CONCLUSIONS
The evidence from this systematic review shows that for the surgical procedures that have been studied, veterans getting care at the VA receive on average comparable or better surgical quality and safety compared with non-VA delivered care. Evidence about comparisons between VA and non-VA care on other important domains of care is too thin to support strong conclusions.
Author Contributions
Conceptualization: Blegen, Ko, Salzman, Ulloa, Girgis, Shekelle, Maggard-Gibbons
Formal analysis: Blegen, Ko, Salzman, Ulloa, Shekelle, Maggard-Gibbons
Methodology: Blegen, Ko, Salzman, Ulloa, Girgis, Shekelle, Maggard-Gibbons
Validation: Blegen, Ko, Salzman, Begashaw, Ulloa, Girgis, Shekelle, Maggard-Gibbons
Visualization: Blegen, Ko, Salzman, Begashaw, Shekelle
Writing – original draft: Blegen, Ko, Salzman, Begashaw, Maggard-Gibbons
Writing – review & editing: Blegen, Ko, Begashaw, Ulloa, Shekelle, Maggard-Gibbons
Investigation: Ko, Salzman, Ulloa, Girgis, Shekelle, Maggard-Gibbons
Data curation: Begashaw, Shekelle
Project administration: Begashaw
Software: Begashaw
Supervision: Girgis, Shekelle, Maggard-Gibbons
Funding acquisition: Shekelle
Resources: Shekelle
Supplementary Material
Abbreviations and Acronyms
- CABG
- coronary artery bypass grafting
- CDW
- corporate data warehouse
- HR
- hazard ratio
- MISSION
- Maintaining Internal Systems and Strengthening Integrated Outside Networks
- OR
- odds ratio
- THA
- total hip arthroplasty
- TKA
- total knee arthroplasty
- VA
- Veterans Health Administration
Disclosure Information: Nothing to disclose.
Support: This project was funded by the Veterans Health Administration Quality Enhancement Research Initiative (Project #ESP 05-226). Drs Blegen and Salzman were supported by the VA Office of Academic Affiliations through the National Clinician Scholars Program.
Disclaimer: The contents of this article do not represent the views of the US Department of Veterans Affairs or the US Government.
Supplemental digital content is available for this article.
REFERENCES
- 1.Kizer KW, Dudley RA. Extreme makeover: transformation of the Veterans Health Care System. Annu Rev Public Health. 2009;30:313–339. [DOI] [PubMed] [Google Scholar]
- 2.Oliver A. The Veterans Health Administration: an American success story? Milbank Q. 2007;85:5–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348:2218–2227. [DOI] [PubMed] [Google Scholar]
- 4.Veterans Access, Choice, and Accountability Act of 2014, HR 3230, 113th Cong (2013-2014). Pub L No. 113-146.
- 5.Veterans Community Care Program. Federal Register. Published June 5, 2019. Available at: https://www.federalregister.gov/documents/2019/06/05/2019-11575/veteranscommunity-care-program. Accessed August 2, 2022.
- 6.O’Hanlon C, Huang C, Sloss E, et al. Comparing VA and Non-VA quality of care: a systematic review. J Gen Intern Med. 2017;32:105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Asch S, Glassman P, Matula S, et al. Comparison of Quality of Care in VA and Non-VA Settings: A Systematic Review. VA-ESP Project #05-226; 2010. [PubMed]
- 8.Corrigan JM, Donaldson MS, Kohn LT. eds. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001. [Google Scholar]
- 9.Shekelle P, Maggard-Gibbons M, Blegen M, et al. VA Versus Non-VA Quality of Care: A Systematic Review. Washington, DC: Evidence Synthesis Program, Health Services Research and Development Service, Office of Research and Development, Department of Veterans Affairs; 2022. [PubMed] [Google Scholar]
- 10.Trivedi AN, Matula S, Miake-Lye I, et al. Systematic review: comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Med Care. 2011;49:76–88. [DOI] [PubMed] [Google Scholar]
- 11.George EL, Massarweh NN, Youk A, et al. Comparing Veterans Affairs and private sector perioperative outcomes after noncardiac surgery. JAMA Surg. 2021;157:231–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris AHS, Beilstein-Wedel EE, Rosen AK, et al. Comparing complication rates after elective total knee arthroplasty delivered or purchased by the VA. Health Aff (Millwood). 2021;40:1312–1320. [DOI] [PubMed] [Google Scholar]
- 13.Rosen AK, Beilstein-Wedel EE, Harris AH, et al. Comparing postoperative readmission rates between veterans receiving total knee arthroplasty in the Veterans Health Administration (VA) versus community care. Med Care. 2022;60:178–186. [DOI] [PubMed] [Google Scholar]
- 14.Frisch NB, Courtney PM, Darrith B, et al. Veterans undergoing total hip and knee arthroplasty: 30-day outcomes as compared to the general population. J Am Acad Orthop Surg. 2020;28:923–929. [DOI] [PubMed] [Google Scholar]
- 15.Hutt E, Radcliff TA, Henderson W, et al. Comparing survival following hip fracture repair in VHA and non-VHA facilities. Geriatr Orthop Surg Rehabil. 2015;6:22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heiden BT, Eaton DB, Jr, Chang SH, et al. Comparison between veteran and non-veteran Populations with Clinical Stage I Non-Small Cell Lung Cancer Undergoing Surgery. Ann Surg. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams CD, Alpert N, Redding TS, et al. Racial Differences in Treatment and Survival among Veterans and Non-Veterans with Stage I NSCLC: An Evaluation of Veterans Affairs and SEER-Medicare Populations. Cancer Epidemiol Biomarkers Prev. 2020;29:112–118. [DOI] [PubMed] [Google Scholar]
- 18.Augustine JJ, Arrigain S, Balabhadrapatruni K, et al. Significantly Lower Rates of Kidney Transplantation among Candidates Listed with the Veterans Administration: A National and Local Comparison. J Am Soc Nephrol. 2018;29:2574–2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kesseli SJ, Samoylova ML, Moris D, et al. Outcomes in Kidney Transplantation Between Veterans Affairs and Civilian Hospitals: Considerations in the Context of the MISSION Act. Ann Surg. 2020;272:506–510. [DOI] [PubMed] [Google Scholar]
- 20.Barnett PG, Hong JS, Carey E, et al. Comparison of Accessibility, Cost, and Quality of Elective Coronary Revascularization Between Veterans Affairs and Community Care Hospitals. JAMA Cardiol. 2018;3:133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blay E, Jr, DeLancey JO, Hewitt DB, et al. Initial Public Reporting of Quality at Veterans Affairs vs Non-Veterans Affairs Hospitals. JAMA Intern Med. 2017;177:882–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eid MA, Barnes JA, Trooboff SW, et al. A Comparison of Surgical Quality and Patient Satisfaction Indicators Between VA Hospitals and Hospitals Near VA Hospitals. J Surg Res. 2020;255:339–345. [DOI] [PubMed] [Google Scholar]
- 23.Rosen AK, Vanneman ME, O’Brien WJ, et al. Comparing cataract surgery complication rates in veterans receiving VA and community care. Health Serv Res. 2020;55:690–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu AM, Wu CM, Tseng VL, et al. Characteristics associated with receiving cataract surgery in the US Medicare and Veterans Health Administration populations. JAMA Ophthalmol. 2018;136:738–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Griffith KN, Ndugga NJ, Pizer SD. Appointment wait times for specialty care in Veterans Health Administration Facilities vs community medical centers. JAMA Netw Open. 2020;3:e2014313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Billig JI, Evans RR, Kerr EA, et al. The impact of community care referral on time to surgery for veterans with carpal tunnel syndrome. Med Care. 2021;59(suppl 3):S279–S285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pettey WBP, Wagner TH, Rosen AK, et al. Comparing driving miles for Department of Veterans Affairs-delivered versus Department of Veterans Affairs-purchased cataract surgery. Med Care. 2021;59(suppl 3):S307–S313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wagner TH, Lo J, Beilstein-Wedel E, et al. Estimating the cost of surgical care purchased in the community by the Veterans Health Administration. MDM Policy Pract. 2021;6:23814683211057902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matula SR, Trivedi AN, Miake-Lye I, et al. Comparisons of quality of surgical care between the US Department of Veterans Affairs and the private sector. J Am Coll Surg. 2010;211:823–832. [DOI] [PubMed] [Google Scholar]
- 30.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160:3252–3257. [DOI] [PubMed] [Google Scholar]
- 31.Duan-Porter W, Martinson BC, Greer N, et al. Evidence review-social determinants of health for veterans. J Gen Intern Med. 2018;33:1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.