Where Are We Now?
Predictions seem to pervade everything we do and everything we touch. We try to predict the weather, the stock market, sports performance, test scores, and buying behavior, among many other things. Prediction is everywhere, even in the movies, where the more recognizable Moneyball, Wall Street, and Boiler Room are joined by an underrated (in my opinion) film from about 20 years back called Minority Report. In this Steven Spielberg sci-fi thriller, Tom Cruise portrays a future cop who relies on the predictions of three clairvoyant individuals (called pre-cogs) to prevent major crimes before they happen.
The desire to develop research that can serve as a pre-cog of sorts for orthopaedic and spine surgery seems to have become endemic, at least since we entered the era of “Big Data” in which large-scale, multicenter healthcare information can be accessed across the span of years and analyzed relatively quickly and inexpensively. Many prognostic papers have come out of United States data, including Medicare claims, private health insurance collectives like Marketscan or PearlDiver, and the National Inpatient Sample. In this issue of Clinical Orthopaedics and Related Research®, Heck et al. [1] present work from the German healthcare system, evaluating the trajectory of spinal fusions with a special focus on patients 75 years and older.
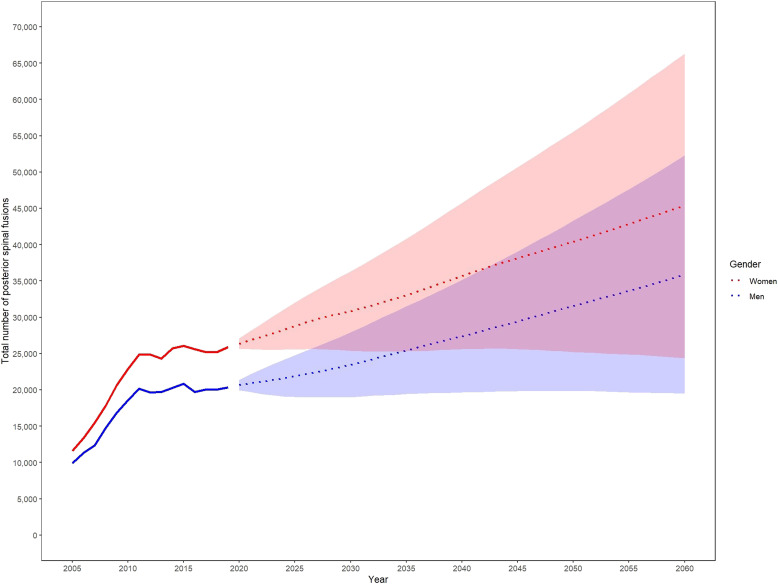
As the population in most industrialized countries continues to age, several prior investigations have highlighted the anticipated need for more extensive use of surgical interventions in orthopaedics, including joint replacement and spinal surgery. In the current work, Heck et al. [1] summarize this nicely where they state: “A higher demand for spinal fusions, including a higher number of patients experiencing age-related changes, combined with patients’ rising expectations about their quality of life, may lead to increased costs [at the societal level].” The fear, of course, is either that the use of spine surgery and other orthopaedic procedures may exceed the capacity of available providers, leading to long waiting times for treatment and thus “rationing,” or that expenditures will grow to the point of bankrupting the system and culminate in draconian austerity measures that will yield similar postdiluvian realities. To assess the outlook in a more robust manner, Heck et al. [1] used data from the German Federal Statistical Office (2005 to 2019) and determined there would be a sustained and steep rise in the demand for posterior spinal fusion, particularly in patients 75 years and older [1]. This includes the anticipated need for nearly 39,000 such procedures in 2060. These projections maintain that the number of posterior spinal fusions performed among women in 2019 will more than double by 2060, while the figure for men will nearly triple. Although the information used is specific to the German healthcare context, the suggestion is that these data would generalize to other Western nations with a similar demographic outlook, including the United States.
Where Do We Need To Go?
The predictions in the current study caused Heck et al. [1] to caution healthcare systems, federal agencies, and providers to plan now in order to manage the future need for workforce, clinical space, rehabilitation facilities, and the financial resources to pay for it all. I think the unstated expectation, however, is that these demands will quickly outpace any capacity for the health system in Germany (or elsewhere) to effectively manage them.
Readers who are interested in projections of this kind should remember that past performance is not necessarily a predictor of future behavior. Especially in healthcare, policy changes, coverage decisions, and cultural shifts in terms of what constitutes acceptable clinical practice can lead to dramatic changes in healthcare use and ultimately expenditures. Previous work using United States Medicare claims data has shown that preference-sensitive decisions by surgeons regarding the use of fusion and interbody devices are among the main differentiators in the cost of spine care delivery [2]. Additional research conducted in the federal and private sector arms of the United States military health system identified a potential financial incentive driving the use of more expensive and complex interventions, including posterior spinal fusion and interbody procedures [3].
Coming back to the movie Minority Report, the title derives from the fact that for every prognostication, there is always the possibility of a counterfactual. I would like to leverage the data provided by Heck et al. [1] in one of their figures ( Fig. 4 in their paper, but Fig. 1 here) to render a “minority report” of my own. If we consider the lower margins of the confidence intervals around their projections (the shaded area of the graph), we see that for both men and women, there is a scenario in which the current trends are projected to stabilize, or even decrease, over time. So, I would maintain that the anticipated outcome of ever-increasing surgical interventions at unsustainable costs is not inevitable.
Fig. 1.
This figure shows the projected total number of posterior spinal fusions for women and men until 2060. A color image accompanies the online version of this article.
How Do We Get There?
Clearly, the status quo of the current trajectory cannot be maintained. Previous studies [2, 3] using United States data have already called for more judicious stewardship of expensive, high-intensity surgical interventions, including posterior spinal fusions and interbody procedures. This, combined with increased use of less-invasive interventions that may decrease the use of fusion, like endoscopic decompression, and administrative advances that may provide fairer patient access for those seeking spine care and that do not rely on spine surgeons to direct patient care [4], could effectively curb some of the more-concerning trends identified by Heck et al. [1].
Perhaps more drastic postulations, such as those provided here [1], might serve as more urgent clarions. We would do well to remember, like Scrooge in Dickens’ A Christmas Carol, we are not being shown the “shadows of the things that will be, but only shades of the things that may be.” Reductions in the use of highly expensive, preference-sensitive interventions like posterior fusions and the use of interbody procedures, particularly in those 75 and older, would go a long way toward altering the trajectory anticipated by Heck et al. [1]. It is up to us to make such changes, and we have to decide for ourselves what orthopaedic, spine, and healthcare as a whole will look like globally in the decades to come. If the challenges prognosticated by Heck et al. [1], along with others, are indeed dystonic, it behooves us now to engage in near-term action that will result in meaningful change.
Footnotes
This CORR Insights® is a commentary on the article “Projections From Surgical Use Models in Germany Suggest a Rising Number of Spinal Fusions in Patients 75 Years and Older Will Challenge Healthcare Systems Worldwide” by Heck and colleagues available at: 10.1097/CORR.0000000000002576.
The author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
The opinions expressed are those of the writer, and do not reflect the opinion or policy of CORR® or The Association of Bone and Joint Surgeons®.
References
- 1.Heck VJ, Klug K, Prasse T, et al. Projections from surgical use models in Germany suggest a rising number of spinal fusions in patients 75 years and older will challenge healthcare systems worldwide. Clin Orthop Relat Res . 2023;481:1610-1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schoenfeld AJ, Harris MB, Liu H, Birkmeyer JD. Variations in Medicare payments for episodes of spine surgery. Spine J. 2014;14:2793-2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schoenfeld AJ, Makanji H, Jiang W, Koehlmoos T, Bono CM, Haider AH. Is there variation in procedural utilization for lumbar spine disorders between a fee-for-service and salaried healthcare system? Clin Orthop Relat Res . 2017;475:2838-2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simpson AK, Crawford AM, Striano BM, Kang JD, Schoenfeld AJ. The future of spine care innovation-software not hardware: how the digital transformation will change spine care delivery. Spine (Phila Pa 1976). 2023;48:73-78. [DOI] [PubMed] [Google Scholar]