Abstract
Most post-operative stroke cases occur within 24 hours. This retrospective case-control study aimed to investigate the incidence, risk factors, and outcomes of early post-operative stroke that occurred within 24 hours after surgery in a university-based tertiary care hospital. Medical records were collected and reviewed between 2015 and 2021. Early post-operative stroke cases were compared with age-matched controls in a 1:3 ratio, and data regarding patient characteristics, intra-operative events, and post-operative outcomes were analyzed. Multiple logistic regression was performed to identify the risk factors for post-operative stroke. The incidence of early (≤24 hours) post-operative stroke was 0.015% (43 out of 284,105 cases). The multivariable analysis revealed that American Society of Anesthesiologists (ASA) physical status ≥3 (adjusted odds ratio [OR]: 3.12; 95% confidence interval [CI]: 1.22–7.99, P = .017), operation time >120 minutes (adjusted OR: 10.69; 95% CI: 3.95–28.94, P < .001), and intra-operative hypotension and inotrope/vasopressor use (adjusted OR: 2.80; 95% CI: 1.08–7.24, P = .034) were risk factors for early post-operative stroke. Compared to the controls, stroke patients had higher rates of planned and unplanned intensive care unit (ICU) admission, length of stay, ventilator use, and death. Despite its low incidence (0.015%), stroke is associated with poor clinical outcomes and increased mortality. Stratification of potential risks and establishment of risk optimization may help reduce stroke incidence.
Keywords: cerebrovascular disease, complications, post-operative, risk factors, stroke
1. Introduction
Post-operative adverse events involving major organ dysfunction or even death occasionally occur. Stroke is a complication that results in high morbidity and mortality. The incidence of peri-operative stroke observed until 30 days after surgery in patients undergoing non-cardiac and non-neurological surgery ranges from 0.1% to 1.0% worldwide.[1] However, in Thailand, research regarding stroke remains limited. The incidence of stroke for all types of surgery within 24 to 72 hours post-operation in Thailand was 0.036% to 0.067%[2,3] and 0.075% for non-cardiac surgery within 30 days post-operation.[4] Age, sex, renal disease, prior transient ischemic attack (TIA) or stroke, myocardial infarction within 6 months, atrial fibrillation, hypertension, chronic obstructive pulmonary disease, current smoking, and migraine history have been reported as risk factors.[1,5] The incidence of stroke varies among different types of surgery and is considerably higher in cardiac, neurological, vascular, and emergency surgeries.[1,3–8] Other intra-operative risk factors include intra-operative hypotension in patients with large vessel stenosis[9] and hypoxemia.[10]
The majority of post-operative strokes were reported within 24 hours post-operation and are thus regarded as early post-operative strokes[11,12] with increased post-operative death.[13] As a result, it may be worthwhile to investigate early post-operative stroke events and their relationship to potential causal factors, including surgery and anesthesia. In our institutional practice, post-anesthesia care service members visit patients the day after the operation and report and record anesthesia-related complications. Anesthetic agents can remain in the body for up to 24 hours after administration.[14–16] However, difficulty in awakening or fully recovering from anesthesia may be the first indication of post-operative stroke.[5]
The present study objectives were to explore the incidence and risk factors of early (24 hours) post-operative stroke and to determine the patients’ outcomes. Considering that anesthetic agents persist in the body for <24 hours, it could be compelling to investigate relevant stroke risk factors, which might include anesthesia. With the information obtained from this study, the quality of patient preparation and optimization can be improved to achieve better clinical outcomes after surgery.
2. Methods
2.1. Study design
This retrospective case-control study was initiated in a university-based tertiary care hospital after approval by the Siriraj Institutional Review Board (SI 214/2565). This study was registered in the Thai Clinical Trials Registry (https://www.thaiclinicaltrials.org/show/TCTR20220317006).
2.2. Participants
Patients with complete medical records who were 18 years or older and scheduled for surgery at a university-based tertiary care hospital between January 2015 and December 2021 were recruited for the study. Patients who did not undergo surgery for any reason (e.g., a change in the treatment plan, cancelation of surgery, or incomplete medical records) were excluded. Cases with evidence of in-hospital post-operative stroke within 24 hours after anesthesia were included for further analysis. All records of in-hospital post-operative stroke cases at any time point in the hospital database also conformed to the guidelines outline by the International Classification of Diseases, Tenth Revision.
Stroke was defined as the sudden onset of a neurological deficit in the cerebral hemispheres, brainstem, or cerebellum, which is related to the vascular territory. Stroke can be further classified as hemorrhagic stroke, ischemic stroke, and TIA.[17,18] Patients having stroke onset within 24 hours after operation and then lasting >24 hours without spontaneous recovery were selected for further study; hence, TIA was not included. Strokes with causes other than vascular origin were also not considered. Stroke diagnosis must be confirmed by neuroimaging studies and a certified neurologist. Patients who underwent surgery and did not develop post-operative stroke within 24 hours were matched for exact age (±1–2 years) and surgery day. Non-stroke controls were matched to stroke cases at a 3:1 ratio.
2.3. Data collection
Patients’ pre-operative demographic characteristics, including age, sex, body weight, height, comorbidities, American Society of Anesthesiologists (ASA) classification of physical status, abnormal pre-operative testing, surgery type, and surgery timing, were collected. A history of cerebrovascular disease included stroke and TIA. Hypertension (any patient with blood pressure [BP] ≥ 140/90 mm Hg), well-controlled hypertension (treated hypertensive patients with BP < 140/90 mm Hg), and uncontrolled hypertension (treated patients with BP ≥ 140/90 mm Hg) were described according to the American College of Cardiology/American Heart Association (ACC/AHA) and the International Society of Hypertension (ISH) clinical practice guidelines.[19,20] To define chronic kidney disease stages and estimated glomerular filtration rate, the Kidney Disease Improving Global Outcomes practice guidelines[21] were used. Metabolic acidosis was defined as a decrease in serum bicarbonate below 22 mmol/L.[22]
The following intra-operative data were collected: anesthesia type, operation duration, blood component transfusion, intra-operative hypotension and inotrope/vasopressor use, and intra-operative hypoxemia. Intra-operative hypotension was defined as an absolute mean arterial pressure <65 mm Hg or a relative, a reduction of mean arterial pressure or systolic blood pressure of ≥20% from baseline.[23,24] Intra-operative desaturation was defined as an oxygen saturation of <90%, as reported previously.[1,25]
Post-operative data relating to the incidence of planned and unplanned intensive care unit (ICU) admissions, length of ICU stay, total hospital stay, ventilator use, duration of ventilator use, and discharge status were collected.
2.4. Sample size calculation
Similar to previous literature,[26] our work reported the actual number of stroke cases observed between January 2015 and December 2021. We did not perform a priori sample size calculation because this was an observational study. Cases were matched with controls at a ratio of 1:3, which was proven to be sufficient for analysis.[27]
2.5. Statistical analysis
According to the normality of the distribution, continuous data were reported as mean, standard deviation, or median and interquartile range and analyzed using an independent Student t test or Mann–Whitney U test. Categorical variables were reported as frequency and percentage and compared using the Chi-square test or Fisher exact test. Variables with a P value < .10 from the univariate analysis were included for multivariable logistic regression using the forward-stepwise analysis. The associated factors were presented as crude odds ratio (OR), adjusted OR, and 95% confidence intervals (CI). As reported previously, most medical studies frequently adopt small sample sizes for regression analyses, which might cause a problem in result reproducibility. We circumvented this issue by selecting the variables of interest with the optimal number of events required for multivariable regression analysis (n ≥ 25).[28] The cutoff value for the operation time was calculated from the area under the receiver operator characteristic curve. Statistical analysis was performed using SPSS version 28.0 (IBM Corp, Armonk, NY). Statistical significance was determined by a P < .05.
3. Results
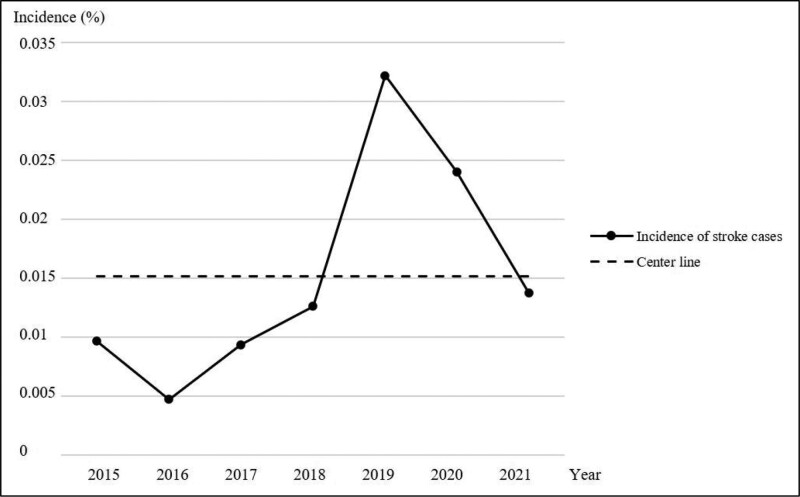
During the period 2015 to 2021, a total of 284,105 patients aged ≥18 years were scheduled for surgery. Of this population, 43 post-operative stroke cases were reported, resulting in an incidence of 0.015% or 1.5/10,000. Figure 1 displays the annual distribution of incidences. A total of 129 age- and day-matched non-stroke controls were also recruited for the study. The majority of stroke cases (88.4%) were ischemic, and the middle cerebral arteries were the most affected area (32.6%) (Supplementary Table 1, http://links.lww.com/MD/J299).
Figure 1.
Early postoperative stroke incidence from 2015 to 2021.
Patients’ pre-operative demographics were comparable between the non-stroke and stroke groups. Univariate analysis revealed significant variables (P < .10) that were associated with early post-operative stroke (≤24 hours after surgery), including cerebrovascular diseases with neurological deficit, chronic kidney disease ≥ Stage 4, ASA physical status ≥ 3, pre-operative metabolic acidosis, abnormal chest radiography, cardiothoracic and intra-cranial surgery, emergency surgery, administration of isoflurane and midazolam, operation time >120 minutes, and intra-operative events such as blood component transfusion, intra-operative hypotension and inotrope/vasopressor use, and intra-operative desaturation. The median operation time in the non-stroke group was significantly lower than that in the stroke group (98 vs 280 minutes, P < .001). The operation cutoff time of 120 minutes was considered the best sensitivity/specificity ratio determined by area under a receiver operator characteristic curve (0.756). The proportion of patients whose operation time exceeded 120 minutes was significantly higher in the stroke group (86%) than in the non-stroke group (34.9%) (Tables 1 and 2).
Table 1.
Preoperative characteristics of the non-stroke and stroke groups.
| Variables | Non-stroke (n = 129) |
Stroke (n = 43) |
P value |
|---|---|---|---|
| Age (yr) | 65.2 ± 13.9 | 66.0 ± 14.5 | .764 |
| Sex | |||
| Male (%) | 45 (34.9%) | 21 (48.8%) | |
| Female (%) | 84 (65.1%) | 22 (51.2%) | .105 |
| Body mass index (kg/m2) | 24.1 ± 5.2 | 23.6 ± 4.4 | .587 |
| Comorbidities (%) | |||
| History of cerebrovascular disease (CVD) | |||
| CVD without neurological deficit | 9 (7.0%) | 4 (9.3%) | .739 |
| CVD with neurological deficit | 2 (1.6%) | 4 (9.3%) | .035* |
| Type 2 diabetes mellitus | 32 (24.8%) | 11 (25.6%) | .919 |
| Hypertension | |||
| Well controlled hypertension | 30 (23.3%) | 12 (27.9%) | .544 |
| Uncontrolled hypertension | 53 (41.1%) | 23 (53.5%) | .162 |
| Dyslipidemia | 71 (55.0%) | 25 (58.1%) | .723 |
| Chronic kidney disease | |||
| Stage 2–3 (eGFR 30–89.9 mL/min/1.73 m2) | 81 (62.8%) | 27 (62.8%) | 1.000 |
| Stage ≥ 4 (eGFR ≤ 29.9 mL/min/1.73 m2) | 8 (6.2%) | 8 (18.6%) | .028* |
| Liver cirrhosis | 3 (2.3%) | 1 (2.3%) | 1.000 |
| Atrial fibrillation | 8 (6.2%) | 6 (14.0%) | .117 |
| Coronary artery disease | 19 (14.7%) | 9 (20.9%) | .342 |
| Structural heart disease | 7 (5.4%) | 4 (9.3%) | .374 |
| Respiratory disease | 9 (7.0%) | 2 (4.7%) | .592 |
| ASA physical status classification (%) | |||
| 1–2 | 75 (58.1%) | 11 (25.6%) | |
| ≥3 | 54 (41.9%) | 32 (74.4%) | <.001* |
| Preoperative testing abnormalities (%) | |||
| Metabolic acidosis | 5 (3.9%) | 17 (39.5%) | <.001* |
| Abnormal electrocardiogram | 43 (33.3%) | 20 (46.5%) | .122 |
| Abnormal chest radiography | 44 (34.1%) | 25 (58.1%) | .006* |
Data presented as mean ± standard deviation (SD) or number (%).
ASA = American Society of Anesthesiologists, CVD = Cerebrovascular disease, eGFR = estimated glomerular filtration rate.
P value < .05 considered statistically significant.
Table 2.
Intraoperative characteristics of the non-stroke and stroke groups.
| Variables | Non-stroke (n = 129) |
Stroke (n = 43) |
P value |
|---|---|---|---|
| Type of surgery (%) | |||
| Non-cardiothoracic, non-intracranial | 115 (89.1%) | 20 (46.5%) | |
| Cardiothoracic and Intracranial | 14 (10.9%) | 23 (53.5%) | <.001* |
| Timing of surgery (%) | |||
| Elective | 114 (88.4%) | 29 (67.4%) | |
| Emergency | 15 (11.6%) | 14 (32.6%) | <.001* |
| Type of anesthesia (%) | |||
| General | 89 (69.0%) | 33 (76.7%) | .438 |
| Regional | 19 (14.7%) | 2 (4.7%) | .102 |
| Combined general + regional | 9 (7.0%) | 7 (16.3%) | .173 |
| Others† | 12 (9.3%) | 1 (2.3%) | .159 |
| Anesthetic agents | |||
| Nitrous oxide | 12 (9.3%) | 2 (4.7%) | .344 |
| Desflurane | 48 (37.2%) | 11 (25.6%) | .167 |
| Sevoflurane | 39 (30.2%) | 15 (34.9%) | .570 |
| Isoflurane | 8 (6.2%) | 11 (25.6%) | .001* |
| Midazolam | 27 (20.9%) | 18 (41.9%) | .008* |
| Operation time (%) | |||
| ≤120 minutes | 84 (65.1%) | 6 (14.0%) | |
| >120 minutes | 45 (34.9% | 37 (86.0%) | <.001* |
| Blood component transfusion (%) | 15 (11.6%) | 25 (58.1%) | <.001* |
| Intraoperative hypotension and | |||
| inotrope/vasopressor use (%) | 59 (45.7%) | 35 (81.4%) | <.001* |
| Intraoperative desaturation (%) | 1 (0.8%) | 6 (14.0%) | .006* |
Data presented as number (%) or median (Interquartile range, IQR).
P value < .05 considered statistically significant.
Intravenous sedation or monitored anesthesia care.
The 4 variables with P values < .10 and sample sizes (n) ≥ 25, such as ASA ≥ 3, abnormal pre-operative chest radiography, operation time >120 minutes, and intra-operative hypotension and inotrope/vasopressor use, were included in the multivariable logistic regression. Only 3 variables were independent risk factors for early post-operative stroke: ASA ≥ 3 (adjusted OR: 3.12; 95% CI: 1.22–7.99, P = .017), operation time > 120 minutes (adjusted OR: 10.69; 95% CI: 3.95–28.94, P < .001), and intra-operative hypotension and inotrope/vasopressor use (adjusted OR: 2.80; 95% CI: 1.08–7.24, P = .034) (Table 3).
Table 3.
Risk factors associated with early postoperative stroke.
| Variables | Crude OR (95% CI) |
Adjusted OR (95% CI) |
P value |
|---|---|---|---|
| ASA physical status classification ≥ 3 | 4.04 (1.87–8.72) | 3.12 (1.22–7.99) | .017* |
| Abnormal preoperative chest radiography | 2.68 (1.32–5.44) | 1.72 (0.70–4.24) | .238 |
| Operation time ≤ 120 minutes >120 minutes |
1 11.51 (4.52–29.34) |
1 10.69 (3.95–28.94) |
<.001* |
| Intraoperative hypotension and inotrope/vasopressor use | 5.19 (2.24–12.05) | 2.80 (1.08–7.24) | .034* |
Data presented as crude and adjusted odds ratio (OR) (95% confidence interval [CI]).
ASA = American Society of Anesthesiologists.
P value < .05 considered statistical significant.
The post-operative outcomes of the stroke group differed significantly from those of the non-stroke group. Post-operative stroke patients had a higher rate of planned and unplanned ICU admission following surgery, longer length of ICU stay, greater need for mechanical ventilation, longer duration of ventilator use, longer hospital stay, and a higher death rate (Table 4). The causes of death in the non-stroke group were respiratory complications and underlying medical conditions, whereas all deaths in the stroke group were complications from ischemic stroke.
Table 4.
Postoperative outcomes of the non-stroke and stroke groups.
| Variables | Non-stroke (n = 129) |
Stroke (n = 43) |
P value |
|---|---|---|---|
| ICU admission (%) | 16 (12.4%) | 35 (81.4%) | <.001* |
| Planned ICU admission | 15 (11.6%) | 27 (62.8%) | <.001* |
| Unplanned ICU admission | 1 (0.8%) | 8 (18.6%) | <.001* |
| Length of ICU stay (d, IQR)† | 1 [1–4] | 10 [5–19] | <.001* |
| Ventilator use (%) | 13 (10.1%) | 27 (62.8%) | <.001* |
| Duration of ventilator (d, IQR)# | 1 [1–2] | 14 [4–20] | <.001* |
| Length of hospital stay (d, IQR) | 5 [3–8] | 19 [11–39] | <.001† |
| Discharge status (%) | <.001* | ||
| Improved | 126 (97.7%) | 34 (79.1%) | |
| Death | 3 (2.3%) | 9 (20.9%) |
Data presented as number (%) or median (Interquartile range, IQR).
ICU = intensive care unit.
P value < .05 considered statistical significant.
Analyzed from patients who were admitted in the ICU (Total n = 51, non-stroke = 16, stroke = 35).
Analyzed from patients who were on postoperative ventilators (Total n = 40, non-stroke = 13, stroke = 27).
4. Discussion
The incidence of post-operative stroke within 24 hours post- surgery in this study was 2.4 times lower than what was reported previously in a study of 24-hours post-operative stroke conducted among the major hospitals across Thailand (0.015% vs 0.036%).[2] We hypothesized that this might be due to medical advancements over the years, higher medical personnel experience, and better knowledge and enhanced vigilance in preventing post-operative complications. In addition, other international studies considered post-operative stroke as an event occurring from the immediate post-operative period until 30 days after the operation. Therefore, the overall incidence could be higher: 0.52% to 1.1% in non-cardiac and non-neurological surgery or up to 10% in cardiac and neurological surgery.[1,29]
The mean age of the patients predisposed to post-operative stroke was 66.0 ± 14.5 years, which is similar to previous reports.[3,30] In contrast to previous reviews,[1,3–5] we did not find a significant association between stroke and sex, or comorbidities such as diabetes mellitus, valvular heart disease, and atrial fibrillation. This could be due to the limited sample size of this study.
Our study proposed that the risk factors for stroke that occurred within 24 hours after surgery based on multivariable logistic regression were ASA physical status ≥ 3, operation time > 120 minutes, and intra-operative hypotension and inotrope/vasopressor use. Considering that higher ASA contributed to post-operative mortality and complications,[31,32] we speculated that patients with high ASA might have a high tendency for adverse events, including stroke. However, we presumed that a longer operation time might increase the chance of exposure to hemodynamic derangement during the operation. We reported that intra-operative hypotension and administration of inotrope/vasopressor could pose a risk for stroke. This could be because inotrope/vasopressor administration reflected severe hypotensive events that required medical treatment.
The rates of post-operative ICU admission, ventilator need, and days of hospital care were clearly higher in stroke cases than in the non-stroke controls. From our findings, most post-operative strokes were ischemic, with unfavorable outcomes. Previous studies have confirmed a higher mortality rate of ischemic stroke than of its hemorrhagic counterpart.[33,34]
This study has several limitations. First, our work was performed in a single center; thus, there could be a lower incidence of post-operative stroke or under-reported cases that presented with TIA, which was not within the scope of our study, or minor stroke with rapid self-recovery. Second, we collected only in-hospital stroke cases. Therefore, any stroke events outside the hospital that occurred within 24 hours post-operatively could have been overlooked.
Despite these limitations, our study has some strengths. This study is the first to determine intra-operative risk factors for surgery and anesthesia for early post-operative stroke, as well as post-operative outcomes. Despite the small sample size, which might result in a wide CI in the multivariable regression, our study performed a methodical analysis and displayed comparable statistical parameters to previous publications.[3,4] We overcame the small sample size issue by adopting the previously proposed solution to the minimal sample size for regression analysis.[28] As recommended, we selected only the variables with n ≥ 25 for multivariable analysis to avoid false negative and false positive results. Importantly, too small a sample size could cause a wide 95% CI. Our strategy of variable selection for multivariable analysis could narrow the variables’ CIs, thus resulting in a better representation of the population mean.
The study results could be implemented into a guide for peri-operative patient preparation and optimization, as well as prerequisite monitoring in cases with risks for post-operative stroke. Future studies should explore other variables potentially related to post-operative stroke by recruiting a larger study population or performing a multi-institutional study.
5. Conclusion
Our study explored pre- and intra-operative factors contributing to post-operative stroke and demonstrated post-operative outcomes. Pre-operative ASA physical status ≥ 3, operation time > 120 minutes, and intra-operative hypotension and inotrope/vasopressor use were potential risk factors among patients scheduled for surgery. Patients at risk can be prepared and closely monitored to mitigate stroke risk. Despite the low incidence, stroke patients experienced a higher rate of ICU admission, ventilator use, length of stay, and mortality than non-stroke patients.
Acknowledgments
The authors would like to thank Ms. Chayanan Thanakiattiwibun for the general assistance, Ms. Sudta Parakkamodom for providing the patients’ data from the anesthetic database, and Dr Chulaluk Komoltri for advice on data analysis. The authors are also indebted to Editage [http://www.editage.com] for editing and reviewing this manuscript for English language.
Author contributions
Conceptualization: Pawit Somnuke, Manee Raksakietisak.
Data curation: Pawit Somnuke, Kanya Kattiyawittayakul.
Formal analysis: Pawit Somnuke, Manee Raksakietisak.
Methodology: Pawit Somnuke, Manee Raksakietisak.
Supervision: Mingkwan Wongyingsinn, Manee Raksakietisak.
Writing – original draft: Pawit Somnuke, Manee Raksakietisak.
Supplementary Material
Abbreviations:
- ASA
- American Society of Anesthesiologists
- BP
- blood pressure
- CI
- confidence interval
- ICU
- intensive care unit
- OR
- odds ratio
- TIA
- transient ischemic attack
Supplemental Digital Content is available for this article.
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Somnuke P, Kattiyawittayakul K, Wongyingsinn M, Raksakietisak M. Incidence, risk factors and outcomes of early post-operative stroke in a university-based, tertiary care hospital: A 7-year retrospective case-control study. Medicine 2023;102:28(e34363).
Contributor Information
Pawit Somnuke, Email: pawit-pup@hotmail.com.
Kanya Kattiyawittayakul, Email: pk.kanya2336@gmail.com.
Mingkwan Wongyingsinn, Email: mingkwan.won@mahidol.ac.th.
References
- [1].Benesch C, Glance LG, Derdeyn CP, et al. Perioperative neurological evaluation and management to lower the risk of acute stroke in patients undergoing noncardiac, nonneurological surgery: a scientific statement from the American Heart Association/American Stroke Association. Circulation. 2021;143:e923–46. [DOI] [PubMed] [Google Scholar]
- [2].Charuluxananan S, Sriraj W, Punjasawadwong Y, et al. Perioperative and anesthetic adverse events in Thailand (PAAd Thai) incident reporting study: anesthetic profiles and outcomes. Asian Biomed. 2017;11:21–32. [Google Scholar]
- [3].Leemingsawat P, Kongsayreepong S, Komoltri C, et al. Incidence and risk factors of perioperative stroke in Siriraj Hospital. J Med Assoc Thai. 2012;95:1167–72. [PubMed] [Google Scholar]
- [4].Vasivej T, Sathirapanya P, Kongkamol C. Incidence and risk factors of perioperative stroke in noncardiac, and nonaortic and its major branches surgery. J Stroke Cerebrovasc Dis. 2016;25:1172–6. [DOI] [PubMed] [Google Scholar]
- [5].Ko SB. Perioperative stroke: pathophysiology and management. Korean J Anesthesiol. 2018;71:3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Larsen AM, Cote DJ, Karhade AV, et al. Predictors of stroke and coma after neurosurgery: an ACS-NSQIP Analysis. World Neurosurg. 2016;93:299–305. [DOI] [PubMed] [Google Scholar]
- [7].Al-Hader R, Al-Robaidi K, Jovin T, et al. The incidence of perioperative stroke: estimate using state and national databases and systematic review. J Stroke. 2019;21:290–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mehta A, Gleason T, Wechsler L, et al. Perioperative stroke as a predictor of mortality and morbidity in patients undergoing CABG. J Clin Neurosci. 2017;44:175–9. [DOI] [PubMed] [Google Scholar]
- [9].Bijker JB, Gelb AW. Review article: the role of hypotension in perioperative stroke. Can J Anaesth. 2013;60:159–67. [DOI] [PubMed] [Google Scholar]
- [10].Dunham AM, Grega MA, Brown CH, 4th, et al. Perioperative low arterial oxygenation is associated with increased stroke risk in cardiac surgery. Anesth Analg. 2017;125:38–43. [DOI] [PubMed] [Google Scholar]
- [11].Ng JL, Chan MT, Gelb AW. Perioperative stroke in noncardiac, non-neurosurgical surgery. Anesthesiology. 2011;115:879–90. [DOI] [PubMed] [Google Scholar]
- [12].Selim M. Perioperative stroke. N Engl J Med. 2007;356:706–13. [DOI] [PubMed] [Google Scholar]
- [13].Lisle TC, Barrett KM, Gazoni LM, et al. Timing of stroke after cardiopulmonary bypass determines mortality. Ann Thorac Surg. 2008;85:1556–62; discussion 1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].After anesthesia: the patient’s active role assists in recovery. American Association of Nurse Anesthetists. 2020. [cite 2022 May 27]. Available at: https://www.mcgill.ca/infoneuro/files/infoneuro/link_30.pdf
- [15].Khan KS, Hayes I, Buggy DJ. Pharmacology of anaesthetic agents I: intravenous anaesthetic agents. Contin Educ Anaesth Criti Care Pain. 2014;14:100–5. [Google Scholar]
- [16].Lockwood G. Theoretical context-sensitive elimination times for inhalation anaesthetics. BJA. 2010;104:648–55. [DOI] [PubMed] [Google Scholar]
- [17].Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36:1776–81. [DOI] [PubMed] [Google Scholar]
- [19].Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:1269–324. [DOI] [PubMed] [Google Scholar]
- [20].Unger T, Borghi C, Charchar F, et al. 2020 International Society of hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982–1004. [DOI] [PubMed] [Google Scholar]
- [21].Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021;99:S1–S87. [DOI] [PubMed] [Google Scholar]
- [22].Phisitkul S, Khanna A, Simoni J, et al. Amelioration of metabolic acidosis in patients with low GFR reduced kidney endothelin production and kidney injury, and better preserved GFR. Kidney Int. 2010;77:617–23. [DOI] [PubMed] [Google Scholar]
- [23].Meng L, Yu W, Wang T, et al. Blood pressure targets in perioperative care provisional considerations based on a comprehensive literature review. Hypertension. 2018;72:806–17. [DOI] [PubMed] [Google Scholar]
- [24].Bijker JB, van Klei WA, Kappen TH, et al. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology. 2007;107:213–20. [DOI] [PubMed] [Google Scholar]
- [25].Tamdee D, Punjasawadwong Y, Charuluxananan S, et al. Factors related to intraoperative oxygen desaturation in geriatric patients in a Thai university hospital. J Med Assoc Thai. 2009;92:208–16. [PubMed] [Google Scholar]
- [26].Bijker JB, Persoon S, Peelen LM, et al. Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case-control study. Anesthesiology. 2012;116:658–64. [DOI] [PubMed] [Google Scholar]
- [27].Selvin S. Statistical Analysis of Epidemiologic Data. New York: Oxford University Press; 2004. [Google Scholar]
- [28].Jenkins DG, Quintana-Ascencio PF. A solution to minimum sample size for regressions. PLoS One. 2020;15:e0229345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Levin SR, Farber A, Cheng TW, et al. Most patients experiencing 30-day postoperative stroke after carotid endarterectomy will initially experience disability. J Vasc Surg. 2019;70:1499–1505.e1. [DOI] [PubMed] [Google Scholar]
- [30].Mashour GA, Shanks AM, Kheterpal S. Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology. 2011;114:1289–96. [DOI] [PubMed] [Google Scholar]
- [31].Hackett NJ, De Oliveira GS, Jain UK, et al. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015;18:184–90. [DOI] [PubMed] [Google Scholar]
- [32].Daabiss M. American Society of anaesthesiologists physical status classification. Indian J Anaesth. 2011;55:111–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Dabilgou AA, Dravé A, Kyelem JMA, et al. Frequency and mortality risk factors of acute ischemic stroke in emergency department in burkina faso. Stroke Res Treat. 2020;2020:9745206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Abdu H, Tadese F, Seyoum G. Comparison of ischemic and hemorrhagic stroke in the medical ward of dessie referral hospital, Northeast Ethiopia: a retrospective study. Neurol Res Int. 2021;2021:9996958. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.