Abstract
Background
Spinal fusion is a well-established procedure in the treatment of degenerative spinal diseases. Previous research shows that the use of this operative treatment has been growing in recent decades in industrialized countries and has become one of the most cost-intensive surgical procedures. It seems that in some countries such as Germany—with its large, industrialized, European population—this increase is mainly driven by demographic changes with low fertility rates, increasing life expectancy, and an aging population. Based on current projections, however, Germany faces a population trend that many other countries are likely to follow within a few decades. An increasingly shrinking and aging working population may eventually put the healthcare system under enormous pressure, with greater demands for spinal fusions and associated higher costs. Thus, we aimed to provide reliable projections regarding the future demand for posterior spinal fusion procedures including age- and gender-related trends up to 2060, which will be necessary for future resource planning and possible improvements in actual treatment strategies.
Questions/purposes
(1) How is the use of posterior spinal fusions in Germany expected to change from 2019 through 2060, if currents trends continue? (2) How is the use of posterior spinal fusions in Germany expected to change depending on patients’ age and gender during this time period?
Methods
Comprehensive nationwide data provided by the Federal Statistical Office, the official institution for documenting all data on operations and procedures performed in Germany, were used to quantify posterior spinal fusion rates as a function of calendar year, age, and gender. Because there is a lack of evidence regarding future trends in the use of posterior spinal fusions, an autoregressive integrated moving average model on historical procedure rates from 2005 to 2019 in relation to official population projections from 2020 to 2060 was chosen to forecast future absolute numbers and incidence rates of this procedure in Germany. Long-term forecasting is more prone to unexpected disruptions than forecasting over short-term periods; however, longer spans facilitate estimates of how trends may challenge future healthcare systems if those trends continue, and thus are useful for research and planning.
Results
The incidence rate of posterior spinal fusion was projected to increase by approximately 83% (95% CI 28% to 139%) to 102% per 100,000 inhabitants (95% CI 71% to 133%) in 2060, with a 1.3-fold higher rate of women undergoing surgery in terms of absolute numbers. The highest increase identified by the model occurred in patients 75 years and older with 38,974 (95% CI 27,294 to 50,653) posterior spinal fusions in 2060, compared with 14,657 in 2019. This trend applied for both women and men, with a 246% (95% CI 138% to 355%) increase in the total number of posterior spinal fusions for women 75 years and older and a 296% (95% CI 222% to 370%) increase for men 75 years and older. At the same time, posterior spinal fusions in all age groups younger than 55 years were projected to follow a constant or even negative trend up to 2060.
Conclusion
Our findings suggest that increasing use of posterior spinal fusion, particularly in patients 75 years and older, will challenge healthcare systems worldwide if current trends persist. This study may serve as a model for many other industrialized countries facing similar demographic and procedure-specific developments in the future. This emphasizes the need to focus on frailty research as well as appropriate financial and human resource management. Effective perioperative medical management, multidisciplinary treatment, and interinstitutional protocols are warranted, especially in older patients as we attempt to manage these trends in the future.
Level of Evidence
Level III, economic and decision analysis.
Introduction
Previous research has demonstrated an increase in surgical volumes across several specialties during the past decade, particularly spine surgery [9]. In spine surgery, posterior spinal fusions are an important intervention to treat numerous spinal diseases; lumbar degenerative disc disease is the most common condition that is treated surgically [29]. After the approval of intervertebral fusion cages in 1996, lumbar interbody fusion with posterior instrumentation saw even wider use for treating degenerative spine diseases, not only in the case of degenerative disc disease in patients whose symptoms persist despite nonoperative treatment, but also to restore sagittal balance with correction of lumbar lordosis, painful segmental instability, or spinal deformities [6, 22]. According to the Federal Statistical Office of Germany, spinal fusion procedures increased by 57% from 2007 to 2015 [41]. In patients older than 70 years, increases well above average were observed in the same time period. This increasing trend in the use of these procedures is seen not only in Germany, but also in many other industrialized countries worldwide [7, 11, 25, 28, 29, 33].
However, relative and absolute numbers differ among countries as a function of differing economic and demographic characteristics and changes. Although populations continue to grow because of high immigration and fertility rates in the United States and in some European countries such as the United Kingdom, France, and the Scandinavian countries, Germany and others such as Italy, Russia, and most Eastern European countries face population declines in the near future that are driven by lower birth and immigration rates that cannot keep up with the aging population [4]. In many European countries, the proportion of people older than 75 years is projected to grow from 2.7% in 1950 to 9.1% in 2025 and to 14.6% in 2050 [38]. This is both a European and global phenomenon, because many countries are likely to follow this trend within a few decades [38, 40]. As the working population is increasingly aging, healthcare systems may face the challenge of a higher demand for spinal fusions and associated higher costs that are heavily skewed toward elderly people [1, 7, 28, 33]. In a report published in 2014, spinal fusions caused the highest total costs of any surgical procedure performed in hospitals in the United States [33, 42]. A higher demand for spinal fusions, including a higher number of patients experiencing age-related changes, combined with patients’ rising expectations about their quality of life, may lead to increased costs. Therefore, after analyzing recent trends in spinal surgery, Sheikh et al. [33] emphasized the need for projective models in order to face the challenge of rising numbers of spinal fusions in the future. Thus, we sought to provide reliable projections regarding the demand for posterior spinal fusions in upcoming decades. This will help create a basis for future resource planning, as well as for the possible need to modify actual treatment strategies and clinical standards to help meet the anticipated need.
We therefore asked: (1) How is the use of posterior spinal fusions in Germany expected to change from 2019 through 2060, if currents trends continue? (2) How is the use of posterior spinal fusions in Germany expected to change depending on patients’ age and gender during this time period?
Patients and Methods
Study Design and Setting
This was a modeling study in which we used historical data from the national inpatient statistics of Germany, which contains all annual inpatient discharge reports of procedures performed in German hospitals and medical institutions, except for military and psychiatric facilities [36]. These data were provided by the Federal Statistical Office, a German higher federal authority in the portfolio of the Federal Ministry of the Interior and the leading institution that guarantees independent quality-assured information and statistics and thus forms part of Germany's sustainable data infrastructure. Its core task is to provide politics and society with neutral, objective, and professionally independent statistics. The Federal Statistical Office is the only institution in Germany that documents, analyzes, and provides all data on operations and procedures of full inpatients in hospitals throughout Germany, which is why we used these data for our forecast models [35]. Germany not only provides complete and high-quality data on posterior spinal fusion procedures, but also offers all citizens free access to all kinds of medical care. Germany has a highly developed economy compared with other countries, based on its nominal Gross Domestic Product. Additionally, the German population will age in the near future at a rate that is similar to or even faster than the rate of other developed countries. Thus, our projections on the future use of spinal fusion procedures offer interesting information not only for Germany, but also for many other industrialized countries worldwide that show similar trends [38, 40]. The data are based on the ICD-10 and German procedure classification system (Operationen und Prozedurenschlüssel [OPS]), which is the official classification system for encoding surgical procedures in Germany.
Baseline Data
For posterior spinal fusions, the OPS codes “5-836.3” and “5-836.4” were used. A detailed breakdown of these data by age and gender was made. Age in years was categorized in 12 groups: younger than 35, 35 to 39, 40 to 44, 45 to 49, 50 to 54, 55 to 59, 60 to 64, 65 to 69, 70 to 74, 75 to 79, 80 to 84, and 85 years and older. The deadline of each year was December 31. For some analyses, we used a combination of several age groups (age < 45, age < 66, age ≥ 65, and age ≥ 75 years) to provide a general overview. All procedures reported between 2005 and 2019 were analyzed based on the corresponding OPS codes. During the study period, no coding changes were made. After thorough consideration, we decided to exclude 2020 and 2021 from our analyses because the coronavirus-19 pandemic might have distorted surgery rates at the beginning of 2020.
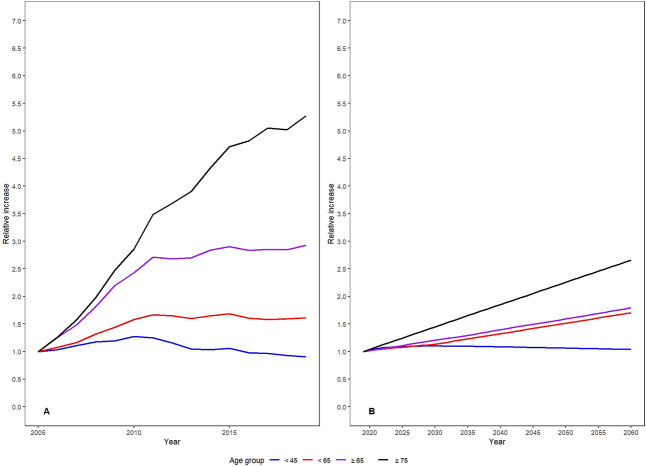
From 2005 to 2019, a total of 595,148 posterior spinal fusions were recorded in Germany. During that time, the annual number of procedures rose from 21,487 in 2005 to 46,233 in 2019, representing an increase of 115%. With respect to the population growth, the annual overall incidence changed substantially, from 26.1 per 100,000 residents to 55.6 per 100,000 residents (p < 0.001). The highest relative increase in incidence from 2005 to 2019 was in patients 75 years and older (Fig. 1A). On average, posterior spinal fusions were performed 1.2 times more often in women than in men during the study period.
Fig. 1.
(A) The historical relative increase in posterior spinal fusion procedures performed from 2005 to 2019 in relation to the numbers of 2005 (per age group) is shown here. (B) This figure shows the estimated relative increase of posterior spinal fusions performed from 2019 to 2060 in relation to the number from 2019 (per age group). A color image accompanies the online version of this article.
Population projections until 2060 were available from the official population projection statistics [26]. These population projections account for future life expectancy, birth, and immigration rates. The projection model was based on a strong increase in life expectancy (life expectancy in 2060: women: 89.6 years, men: 86.2 years) and moderate levels of birth (trend in birth: 1.55 children per woman) and immigration (immigration rate: 221,000 per year). A projection model based on actual trends in the long term provides a good baseline for future research. Because of the nature of forecasting models, it is not possible to predict future trends, medical advances, or political or socioeconomic changes; however, long-term projections including historical and current trends are helpful for long-term planning and policy making, Thus, we decided to mathematically model actual trends over the next 40 years, provided the projection can be modeled correctly in pure mathematical terms.
Projection Methodology and Statistical Analysis
The statistical analysis was performed according to the Guidelines for Accurate and Transparent Health Estimates Reporting [37]. The data from 2005 to 2019 (baseline years) and population forecasts up to 2060 were then used to project the annual incidence of posterior spinal fusions in Germany. The incidence was calculated by dividing the estimated number of spinal fusions for the national total and for each age subgroup by the corresponding official population forecast based on previous forecasting data in the medical field [18, 20, 21, 30-32]. Four alternative projection models were applied to evaluate and compare spinal fusion projections in Germany: Poisson regression, logarithmic regression, autoregressive integrated moving average modeling (ARIMA), and exponential smoothing (Supplemental Digital Content 1; http://links.lww.com/CORR/B31) [2, 8, 14, 16, 17, 23, 30]. All estimated rates and numbers of the models are presented with 95% confidence intervals (Supplemental Fig. 1; http://links.lww.com/CORR/B33).
The prediction accuracy of each model was verified by using out-of-time crossvalidation; that is, splitting the dataset into training (years 2005 to 2014) and testing subsets (years 2015 to 2019) in a ratio of approximately 75:25, as recommended by Hyndman and Athanasopoulos [13], and comparing the mean absolute percentage error, the root mean square error, and the mean absolute error of the models. Based on crossvalidation, the ARIMA model appeared to fit the historical data best and showed highly accurate forecasting (Supplemental Table 1; http://links.lww.com/CORR/B32). Therefore, we selected the ARIMA model as the most appropriate model to forecast the development of posterior spinal fusion procedures.
Ethical Approval
Ethical approval was not sought for the present study because we used anonymized data, which were provided by the German Federal Statistical Office.
Results
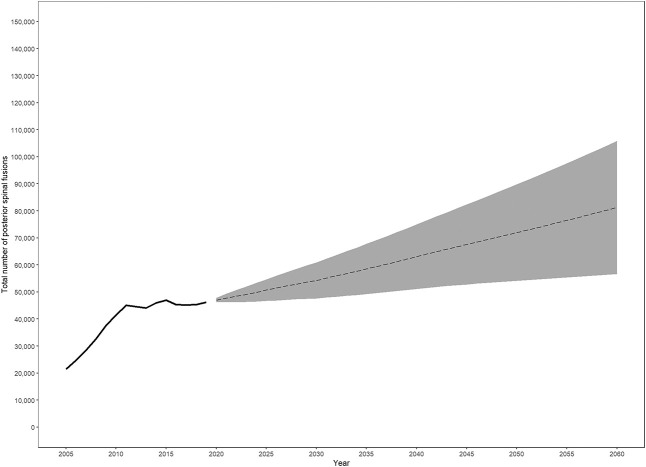
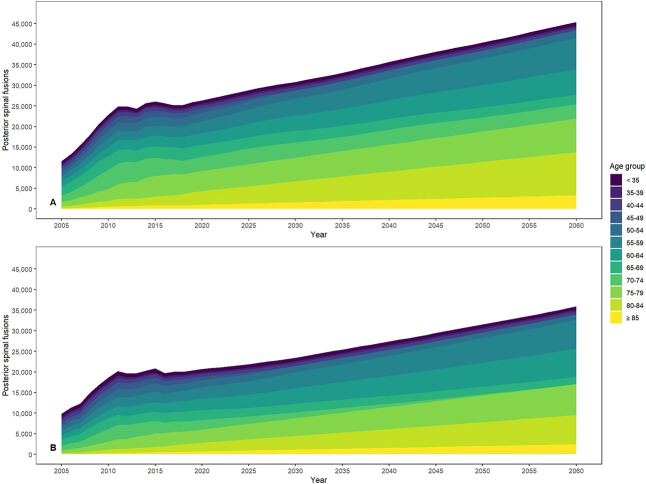
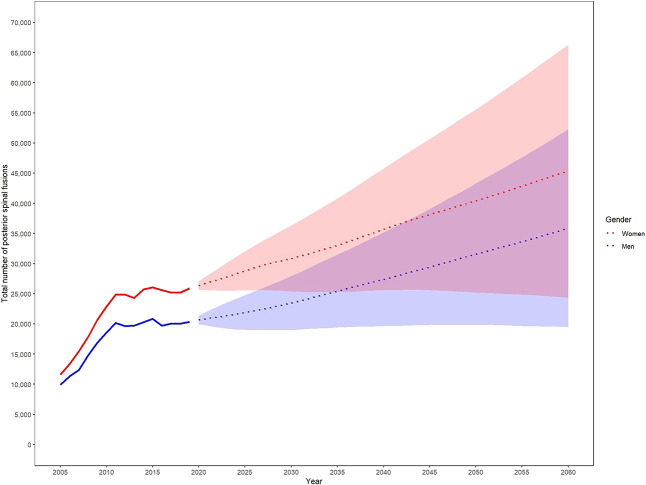
Based on our forecast, we projected that the number of posterior spinal fusions will continuously increase from 2019 to 2060 (Table 1). Specifically, we expected an 83% (95% CI 28% to 139%) rise in the incidence rate (IR) of posterior spinal fusions from 2019 to 2060 for Germany (2019: IR = 56 per 100,000 versus 2060: IR = 102 per 100,000 [95% CI 71 to 133 per 100,000]), leading to a projected total number of 81,244 (95% CI 56,663 to 105,824) posterior spinal fusions in Germany in 2060, up from 46,223 in 2019 (Fig. 2). Based on our projection, the rising incidence of posterior spinal fusions was mainly driven by a rising number of patients 75 years and older, leading to a 2.7-fold increase in performed procedures for these patients in 2060 compared with 2019. These age-related trends apply to men and women, with a 246% (95% CI 138% to 355%) increase in the total number of spinal fusions for women 75 years and older and a 296% (95% CI 222% to 370%) increase for men (Fig. 3). At the same time, posterior spinal fusions in all age groups under 55 years as well as the age group of 65 to 74 years were projected to follow a constant or even negative trend (Fig. 1). Until 2060, the annual incidence rate of women who undergo posterior spinal fusion was projected to increase by 84% (95% CI -1% to 170%), from 61 in 2019 to 113 (95% CI 61 to 166) in 2060. This corresponds to a total number of 45,343 (95% CI 24,374 to 66,312) posterior spinal fusions in 2060, up from 25,878 in 2019. For men, an increase of 83% (95% CI -1% to 166%) to an incidence rate of 91% (95% CI 49% to 132%) corresponding to a total of 35,901 (95% CI 19,495 to 52,306) posterior spinal fusions in 2060 is expected, up from 20,355 in 2019 (Fig. 4).
Table 1.
Predicted total numbers and incidence rates of dorsal spinal fusions for projection years in relation to 2019
| Year | Absolute numbers (95% CI) | Relative increase in % (95% CI) | Incidence rate per 100,000 (95% CI) | Relative increase in % (95% CI) |
| 2019 | 46,233 | 55.6 | ||
| 2020 | 47,025 (46,167 to 47,883) | 2 (0 to 4) | 57 (56 to 58) | 2 (0 to 4) |
| 2030 | 54,297 (47,651 to 60,942) | 17 (3 to 32) | 65 (57 to 73) | 17 (3 to 31) |
| 2040 | 63,067 (51,132 to 75,002) | 36 (11 to 62) | 76 (62 to 91) | 37 (11 to 63) |
| 2050 | 71,955 (54,130 to 89,780) | 56 (17 to 94) | 89 (67 to 110) | 59 (20 to 99) |
| 2060 | 81,244 (56,663 to 105,824) | 76 (23 to 129) | 102 (71 to 133) | 83 (28 to 139) |
Incidence rate is given per 100,000 individuals, relative increase in % compared to 2019 baseline data.
Fig. 2.
The projected total number of spinal fusions until 2060 according to ARIMA modeling (confidence intervals is shaded) is shown.
Fig. 3.
This figure shows the projected total number of spinal fusions for (A) women and (B) men per age group until 2060. A color image accompanies the online version of this article.
Fig. 4.
This figure shows the projected total number of posterior spinal fusions for women and men until 2060. A color image accompanies the online version of this article.
Discussion
Spinal fusion procedures are widely used globally; as a result, they are a topic of interest not only to physicians and patients, but also to researchers, policymakers, and insurance providers. In 2011, spinal fusions were responsible for higher costs than any other surgical procedure performed in hospitals in the United States, and increasing use has been reported in Germany, the United States, and many other developed countries [10, 29, 42]. This increasing use of spinal fusion procedures, combined with an estimated demographic change in many developed countries that has led to an increased number of older people (many of whom will undergo spinal fusion), is anticipated to strain the human and financial resources of healthcare systems in many countries worldwide, especially those with rapidly aging populations such as Germany. For that reason, detailed and reliable projections of the number of procedures are extremely useful. Our most robust model projected a continuous increase in the number of anticipated posterior spinal fusions in Germany over the next four decades. This projected increase in posterior spinal fusions was especially dramatic among patients aged 75 years and older, with a higher number of women anticipated to undergo surgery.
Limitations
This projection analysis carries several limitations, the most important being the use of historical rates of spinal fusions to make projections 40 years into the future. Trends determined from historical data, even if accurate, may change in the future. It is unpredictable whether or when future orthopaedic treatment technologies, new noninvasive pharmaceutical interventions, or other advances in genetics, biologics, or prevention strategies will lead to a reduced demand for posterior spinal fusions by 2060. However, those changes are unlikely to occur in the imminent future, and we believe the use projections for the early part of the 40-year time period are likely to be accurate. It would be reasonable for the reader to have less confidence in longer-term projections; that is, the first decade of our model is more likely to be accurate than the final one. Still, the longer-term time period seems important, and we believe it is useful for longer-term planning at the healthcare-system level, because having some data on this topic is superior to having none. Our model also does not account for unforeseen changes in the economic factors associated with this procedure. Thus, this may lead to an overestimation of projected numbers of spinal fusions in the long term. Furthermore, future advances in other medical specialties, such as anesthesia, cardiology, or frailty research, may enable surgery for a higher number of patients 75 and older, as well as for critically ill or high-risk patients. Moreover, any forecast—even for the near future—is subject to uncertainties that are difficult to assess. Nevertheless, we have chosen a time period of 41 years for the study, up to 2060, to not only facilitate comparisons with previous projections in the medical field [17-21, 24, 30, 31], but also give a baseline for future studies in spinal surgery.
Additionally, similar to most established forecasting models, ARIMA models use historical data to project future estimations. As such, they generally do not consider turning points, unless the turning point represents a return to a long-term equilibrium [13, 14]. The uncertainties associated with such projections can be mathematically minimized by selecting an appropriately large set of historical data. Unfortunately, because of limited official data documentation, we could only consider 15 years of historical data on posterior spinal fusions. The forecast model would clearly be more robust if it was based on a larger database. Consequently, the prognoses made in this study may become superseded in the future and should be reassessed as more years of procedural data become available. Furthermore, we noted that the trend in procedures performed during the baseline period was not strictly linear. There was a period of faster growth (2005 to 2010) and period of slower growth (2011 to 2019) (Fig. 2). We tried to consider this by comparing different forecasting models including those that emphasize more recent trends in the past for future projections, and by using a 75:25 ratio for training and test datasets for our accuracy analysis of the applied model, as recommended by Hyndman and Athanasopoulos [13]. Nevertheless, we are aware we might not have been able to capture some of the nonlinearity in the historical data. Future studies could include a spline analysis and other nonlinear models in addition to the models performed here.
Another limitation is the use of a database for our analysis; in this context, the accuracy of coding and data input is always a concern. However, because these data were provided by the Federal Statistical Office of Germany and include complete, nationwide information on all posterior spinal fusion procedures, we believe the data are reliable and suitable for the purpose we used them for. Because the study source was a national database, the projective analysis is based on data related to one country only. However, historically, German trends in the use of spinal fusion procedures have matched trends in many other industrialized nations that face similar procedure-specific developments and demographic changes. For example, in the United States, the rate of spinal fusion procedures increased approximately 88% between 1998 and 2014, and in Finland, the absolute numbers even increased by approximately 250% during the same time period [25, 33]. Thus, the predicted trends here, which are based on data from one large, industrialized, European country, are alarming for many healthcare systems worldwide.
Discussion of Key Findings
This modeling study predicted steep increases in the use of posterior spinal fusion in a large, industrialized, European country, for which actual trends toward a higher number of procedures in older patients combined with demographic changes toward an aging population seem to be the key drivers. Our findings strongly support historical trends in posterior spinal fusion in many developed countries [12, 25, 27, 33] and have important economic implications, because fusion procedures are among the costliest in all of surgery [29, 42]. However, different population structures and different nation-specific incidence rates of posterior spinal fusions as well as other nondemographic factors (such as access and reimbursement costs) can lead to differences across and between countries. In Germany, unrestricted access to medical treatment is guaranteed, which certainly is not the case for all countries. Still, a worldwide trend toward a higher future number of posterior spinal fusions seems evident and important, and our study provides a baseline model for investigating future trends in spine surgery.
Our model suggested that some of the largest increases in the use of posterior spinal fusion will occur in patients aged 75 years and older; this has important implications for healthcare systems, including a larger number of patients who will undergo spinal surgery and who have important age-related comorbid conditions such as sarcopenia, osteoporosis, and cardiovascular diagnoses. We anticipate this will contribute to an increased risk of postoperative complications and nonhome discharge, as well as longer hospital stays, ultimately resulting in higher hospital costs [3] and perhaps even postoperative deaths. Similar projections have been made for patients with osteoarthritis of the knees or hips (and the hip and knee procedures used to treat them) [18, 20, 21, 31, 33]. This emphasizes the need for an adequate number of qualified surgeons and anticipatory planning by healthcare systems, health insurance schemes, and physician practices. Further, in contrast to hip and knee procedures, the complication rate in spinal surgery remains high, occurring in up to 50% of patients undergoing surgery (depending on the diagnosis); of specific concern to patients undergoing spinal fusion (and the healthcare systems that treat them) is the so-called “failed back syndrome” [39]. Thus, to reduce the perioperative complication rate and improve clinical outcomes, the Enhanced Recovery After Surgery Society Guideline group introduced its preoperative, intraoperative, and postoperative recommendations for spinal fusion procedures in 2021, and emphasized the need for multidisciplinary perioperative care [5]. The need for such guidelines, including multidisciplinary treatment concepts, interinstitutional protocols for fast-track rehabilitation, and further frailty research, is especially urgent in light of the projected increase in the use of posterior spinal fusion we identified in patients aged 75 years and older.
Simultaneously, the use of posterior spinal fusion is projected to decrease in patients aged 65 to 74 years, especially in men, owing to a decrease in procedures in these age groups during the past 15 years. This recent decrease might be explained by a nationwide trend in increased use of spinal decompression surgeries without fusion in men, as identified by the Federal Statistical Office [34]. Some surgeons or patients prefer decompression or laminectomy without fusion as the first step; for example, to treat degenerative spondylolisthesis in younger patients with lumbar spinal stenosis. By contrast, tradeoffs—perhaps including lower risks of ongoing degeneration of the spine, painful segmental instability, and back pain occurring during the patient’s lifetime—may favor fusion in patients older than 75 years, given the lower number of anticipated years of life remaining in that age group [10, 15]. Although our study could not speak directly to this controversy, we hope it will serve as a model for future studies that may be able to do so.
Conclusion
Using data from a reliable national source, we projected a steep and sustained increase in the number and incidence of posterior spinal fusion procedures, if current trends continue. The largest increase in use was projected to occur in patients aged 75 years and older. Because many other developed countries have shown comparable procedure-specific trends in the past and will face similar demographic changes in the future, these findings are likely to challenge the German healthcare system and many other healthcare systems worldwide. Given the known risk factors associated with the surgical treatment of older patients, we think anticipatory human and financial resource planning, frailty as a focus of research, and the development of interinstitutional protocols that focus on effective perioperative medical care for these patients will be important elements of managing these trends in the future.
Acknowledgments
We thank Prof. Rob J. Hyndman of the Department of Econometrics and Business Statistics at Monash University Australia for advising and supporting the authors with the statistical analysis.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval was not sought for the present study.
This work was performed at Faculty of Medicine and University Hospital Cologne and Goethe-University Frankfurt, Germany.
Contributor Information
Kristina Klug, Email: kristina.klug@gmx.de.
Tobias Prasse, Email: tobias.prasse@uk-koeln.de.
Stavros Oikonomidis, Email: stavros.oikonomidis@uk-koeln.de.
Alexander Klug, Email: alexander.klug@bgu-frakfurt.de.
Bastian Himpe, Email: bastian.himpe@hotmail.com.
Philipp Egenolf, Email: philip.egenolf@uk-koeln.de.
Maximilian Lenz, Email: maximilian.lenz@uk-koeln.de.
Peer Eysel, Email: peer.eysel@uk-koeln.de.
Max J. Scheyerer, Email: max.scheyerer@uk-koeln.de.
References
- 1.Anderson GF, Hussey PS. Population aging: a comparison among industrialized countries. Health Aff (Millwood). 2000;19:191-203. [DOI] [PubMed] [Google Scholar]
- 2.Bozdogan H. Model selection and Akaike information criterion (AIC) - the general-theory and its analytical extensions. Psychometrika. 1987;52:345-370. [Google Scholar]
- 3.Chan V, Wilson JRF, Ravinsky R, et al. Frailty adversely affects outcomes of patients undergoing spine surgery: a systematic review. Spine J. 2021;21:988-1000. [DOI] [PubMed] [Google Scholar]
- 4.Coleman D, Rowthorn R. Who's afraid of population decline? A critical examination of its consequences. Popul Dev Rev. 2011;37:217-248. [DOI] [PubMed] [Google Scholar]
- 5.Debono B, Wainwright TW, Wang MY, et al. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) society recommendations. Spine J. 2021;21:729-752. [DOI] [PubMed] [Google Scholar]
- 6.Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005;30:1441-1445. [DOI] [PubMed] [Google Scholar]
- 7.Deyo RA, Nachemson A, Mirza SK. Spinal-fusion surgery - the case for restraint. N Engl J Med. 2004;350:722-726. [DOI] [PubMed] [Google Scholar]
- 8.Erbas B, Ullah S, Hyndman RJ, Scollo M, Abramson M. Forecasts of COPD mortality in Australia: 2006-2025. BMC Med Res Methodol. 2012;12:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garcia P, Domnick C, Lodde G, Raschke M. Operative treatment in orthopaedic surgery: are more operations carried out in Germany? [in German]. Unfallchirurg. 2018;121:20-29. [DOI] [PubMed] [Google Scholar]
- 10.Ghogawala Z, Dziura J, Butler WE, et al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med. 2016;374:1424-1434. [DOI] [PubMed] [Google Scholar]
- 11.Greenwood J, McGregor A, Jones F, Hurley M. Evaluating rehabilitation following lumbar fusion surgery (REFS): study protocol for a randomised controlled trial. Trials. 2015;16:251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grotle M, Smastuen MC, Fjeld O, et al. Lumbar spine surgery across 15 years: trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open. 2019;9:e028743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hyndman RJ, Athanasopoulos G. Forecasting: principles and practice, 2nd edition. Available at: Otexts.com/fpp2/. Accessed on August 8, 2022.
- 14.Hyndman RJ, Koehler AB, Snyder RD, Grose S. A state space framework for automatic forecasting using exponential smoothing methods. International Journal of Forecasting. 2002;18:439-454. [Google Scholar]
- 15.Ilyas H, Udo-Inyang I, Jr, Savage J. Lumbar spinal stenosis and degenerative spondylolisthesis: a review of the SPORT literature. Clin Spine Surg. 2019;32:272-278. [DOI] [PubMed] [Google Scholar]
- 16.Juang WC, Huang SJ, Huang FD, Cheng PW, Wann SR. Application of time series analysis in modelling and forecasting emergency department visits in a medical centre in southern Taiwan. BMJ Open. 2017;7:e018628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes - global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10:107-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klug A, Gramlich Y, Rudert M, et al. The projected volume of primary and revision total knee arthroplasty will place an immense burden on future health care systems over the next 30 years. Knee Surg Sports Traumatol Arthrosc. 2021;29:3287-3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klug A, Herrmann E, Fischer S, Hoffmann R, Gramlich Y. Projections of primary and revision shoulder arthroplasty until 2040: facing a massive rise in fracture-related procedures. J Clin Med. 2021;10:5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klug A, Pfluger DH, Gramlich Y, Hoffmann R, Drees P, Kutzner KP. Future burden of primary and revision hip arthroplasty in Germany: a socio-economic challenge. Arch Orthop Trauma Surg. 2021;141:2001-2010. [DOI] [PubMed] [Google Scholar]
- 21.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [DOI] [PubMed] [Google Scholar]
- 22.Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1:2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moran JL, Solomon PJ; Adult Database Management Committee (ADMC) of the Australian and New Zealand Intensive Care Society (ANZICS). Conventional and advanced time series estimation: Application to the Australian and New Zealand Intensive Care Society (ANZICS) adult patient database, 1993-2006. J Eval Clin Pract. 2011;17:45-60. [DOI] [PubMed] [Google Scholar]
- 24.Nemes S, Rolfson O, W-Dahl A, et al. Historical view and future demand for knee arthroplasty in Sweden. Acta Orthop. 2015;86:426-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ponkilainen VT, Huttunen TT, Neva MH, Pekkanen L, Repo JP, Mattila VM. National trends in lumbar spine decompression and fusion surgery in Finland, 1997-2018. Acta Orthop. 2021;92:199-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pötzsch O, Rößger F. Demographic analyses, methods and projections, births and deaths: Germany’s population by 2060—results of the 13th coordinated population projection. Available at: https://www.destatis.de/EN/Themes/Society-Environment/Population/Population-Projection/Publications/Downloads-Population-Projection/germany-population-2060-5124206159004.pdf?__blob=publicationFile. Accessed January 3, 2022.
- 27.Provaggi E, Capelli C, Leong JJH, Kalaskar DM. A UK-based pilot study of current surgical practice and implant preferences in lumbar fusion surgery. Medicine (Baltimore). 2018;97:e11169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 2012;37:67-76. [DOI] [PubMed] [Google Scholar]
- 29.Reisener MJ, Pumberger M, Shue J, Girardi FP, Hughes AP. Trends in lumbar spinal fusion-a literature review. J Spine Surg. 2020;6:752-761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Romanini E, Decarolis F, Luzi I, et al. Total knee arthroplasty in Italy: reflections from the last fifteen years and projections for the next thirty. Int Orthop. 2019;43:133-138. [DOI] [PubMed] [Google Scholar]
- 31.Rupp M, Lau E, Kurtz SM, Alt V. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin Orthop Relat Res. 2020;478:1622-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwartz AM, Farley KX, Guild GN, Bradbury TL, Jr. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35:S79-S85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sheikh SR, Thompson NR, Benzel E, et al. Can we justify it? Trends in the utilization of spinal fusions and associated reimbursement. Neurosurgery. 2020;86:E193-E202. [DOI] [PubMed] [Google Scholar]
- 34.Statistisches Bundesamt (Destatis). Datbase of the Dederal Statistical Office of Germany. Available at: https://www-genesis.destatis.de/genesis/online?operation=sprachwechsel&language=en. Accessed November 20, 2022.
- 35.Statistisches Bundesamt (Destatis). Ihr nutzen. Unser auftrag. Available at: https://www.destatis.de/DE/Ueber-uns/Ziele-Strategie/IN_UA_2020.pdf?__blob=publicationFile. Accessed November 15, 2022.
- 36.Statistisches Bundesamt (Destatis). Operationen und prozeduren der vollstationären patientinnen und patienten in krankenhäusern. Available at: https://www.statistischebibliothek.de/mir/servlets/MCRFileNodeServlet/DEHeft_derivate_00063003/5231401207014.pdf. Accessed November 15, 2022.
- 37.Stevens GA, Alkema L, Black RE, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388:e19-e23. [DOI] [PubMed] [Google Scholar]
- 38.Szpalski M, Gunzburg R, Melot C, Aebi M. The aging of the population: a growing concern for spine care in the twenty-first century. Eur Spine J. 2003;12(Suppl 2):S81-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taylor RS, Taylor RJ. The economic impact of failed back surgery syndrome. Br J Pain. 2012;6:174-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.United Nations, Department of Economic and Social Affairs, Population Division. World population ageing 2019: highlights. Available at: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf. Accessed November 20, 2022.
- 41.Volbracht E, Fürchtenicht A, Grote-Westrick M. Spotlight gesundheit: Rückenoperationen. Bertelsmann Stiftung. Available at: https://www.bertelsmann-stiftung.de/fileadmin/files/BSt/Publikationen/GrauePublikationen/VV_SpotGes_Rueckenoperation_dt_final.pdf. Accessed November 15, 2022.
- 42.Weiss AJ, Elixhausera A, Andrews RM. Characteristics of operating room procedures in U. S. hospitals, 2011. HCUP statistical brief #170. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.jsp. Accessed November 15, 2022. [PubMed] [Google Scholar]