Abstract
Objective
To assess the prevalence of bullying in medical residents and its associated factors.
Methods
In this systematic review and meta‐analysis, articles from MEDLINE, EMBASE, Scopus, PsycInfo, Cochrane databases, and Web of Science were searched. Published and unpublished cross‐sectional studies were included. Cochrane's Q test and I 2 statistics were used to assess the existence of heterogeneity. Subgroup analysis and sensitivity analysis were performed on evidence of heterogeneity. Egger's test and funnel plots were performed to investigate publication bias.
Results
A total of 13 cross‐sectional studies with a total of 44 566 study participants from different medical residencies were analyzed. The overall prevalence of bullying was 51% (95% CI 36–66). Furthermore, female residents and residents that belong to a minority group had higher odds of experiencing bullying compared to their peers.
Conclusion
A high prevalence of bullying in medical residents exists around the world. There is a need for education, dissemination, and more effective interventions among the residents and authorities about bullying to build and promote adequate behaviors and diminish bullying prevalence.
Keywords: bullying, interprofessional relations, medical residencies, meta‐analysis, prevalence
1. INTRODUCTION
Bullying has been a problem in the healthcare system for decades, but only recently the phenomenon has been acknowledged as a serious issue, particularly in medicine. 1 , 2 , 3 , 4 One possible reason for this delayed recognition is the lack of a universally accepted definition of bullying. 1 , 5 , 6 Several definitions have been proposed, though the definitions vary in essence, they coincide with each other at several points; bullying involves persistent negative behavior, rather than isolated incidents, and there is typically a power imbalance between the victim and the perpetrator. 5 , 6 , 7 Lastly, the condition of whether the behavior should be considered negative or not depends on the victim's perception, not on the perpetrator's intention.
Healthcare providers and medical students are a special population when it comes to bullying. Studies have found that medical students experience mistreatment during their education at twice the rate of students in other fields. 8 Prevalence of bullying in this community has been reported in primary studies before. All these studies have a wide difference in the reported prevalence, ranging from 30% to 95%. 1 , 2 , 4 , 9 , 10 , 11 , 12 , 13
Bullying can have consequences, including emotional distress, work absenteeism, and physical and psychological harm to the victims. 6 , 12 , 14 , 15 These effects not only affect the victims of bullying in the medical community but also can directly and/or indirectly affect patient care, ultimately compromising patients' health. 11 , 16 , 17 , 18 , 19
Attitudes in the healthcare workforce can make it difficult to identify and address instances of bullying and can perpetuate a culture of fear and hostility within medical education. In addition, the hierarchical nature of the healthcare system can make it challenging for victims of bullying to come forward and report their experiences without fear of reprisal or retaliation. 20 , 21 Despite these challenges, it is essential to continue working toward a culture of respect, support, and safety in medical education in order to promote the well‐being of healthcare providers and ensure the highest quality of care for patients.
Considering the reports of bullying in the healthcare workforce and the impact it has on patients' health, some research teams have made progress on raising awareness, expanding our knowledge regarding bullying, and even giving some recommended courses of action. Fnais et al. reported on the most common form of harassment, which was verbal and academic, and the most common form of discrimination, which was due to race and gender. 22 Although the definition for harassment and discrimination is essentially different from any proposed bullying definition, it highlighted the continued issue medical education is facing. Laisy and Ahmad, after qualitatively assessing literature, explored some risk factors and outcomes of bullying as well as issued some recommendations to reduce bullying in healthcare, although the impact of the proposed interventions is yet to be measured. 18 Samsudin et al. also assessed qualitatively the risk factors and outcomes of bullying, concluding that more evidence is needed to better understand this phenomenon. 23 Even still with these advances in the bullying research field, no quantitative assessment has been performed regarding bullying in medical residents.
Education, awareness, and overall eradication of bullying in medical education have been challenging. One of the main obstacles is the belief among clinical teachers and the broader healthcare system that mistreatment and intimidation are an unavoidable part of medical training. 20 , 21 , 24 , 25 , 26 , 27
The medical hierarchic environment is filled with pressure, where the difference in knowledge leads to an unbalanced power dynamic. Bullying is a very well‐known problem around the world and identifying the factors that foster its prevalence in the medical profession is essential, especially among medical residents. Medical residents are special because of the inherent nature of their work. Medical residents are not really students since their work is sometimes on par with the work of a medical attending. Yet, they are not medical specialists either, since they are still being trained in their respective specialties. As a result, medical residents occupy a somewhat ambiguous role within the healthcare system. Therefore, this systematic review and meta‐analysis aim to assess and review the different studies conducted so far on the prevalence of bullying in medical residents and its associated factors around the world.
2. MATERIALS AND METHODS
The systematic review and meta‐analysis were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) checklist and the guidelines from the Cochrane Handbook for Systematic Reviews of Interventions (Table S1). 28 , 29 The study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the registration number CRD42022333170.
2.1. Databases and search strategy
A comprehensive electronic literature search was performed by an experienced librarian from inception up to February 10, 2022. The search was conducted in multiple electronic databases including MEDLINE, Embase, Web of Sciences, Scopus, Cochrane databases, and PsycInfo. Both published and unpublished articles from the gray literature were also searched. The articles that reported the prevalence of bullying and associated factors were included in the final analysis. No language, study setting, or time frame restrictions were applied. No studies were excluded based on the risk of bias assessment.
The search terms used were [(“Bullying” AND “prevalence”) AND ((postgraduate AND “medical students”) OR residents OR postgraduate OR “medical residency” OR “post‐graduate training” OR specialty OR medical specialty OR “medical residency programs”)]. The tailored search strategy for the used databases can be found in Table S2.
2.2. Searching and eligibility of studies
Retrieved articles were exported to EndNote reference software version 9 citation manager where they were deduplicated using the native deduplication function within the software, followed by a manual review. 30 The remaining studies were then imported into a systematic review software (Distiller SR), where we screened the studies in two phases: the title and abstract phase and the full‐text phase. Articles included in both phases were evaluated independently and by two reviewers. Studies included by at least one reviewer in the abstract screening phase were considered for full‐text screening, this was done to increase sensibility in the included records for full‐text screening. During the full‐text screening, agreement of inclusion between both reviewers was required for the study to be selected. Disagreements at any phase were resolved by consensus. A pilot was made before each phase, and the chance adjusted inter‐rater agreement was estimated at the calibration and conduction of each phase by Kappa statistic. A Kappa statistic of >0.70 was set as an appropriate inter‐rater agreement.
Data extracted included the author's name, publication year, country where the study was conducted, medical specialty of the subjects, sample size, study subjects (medical residents by Post Graduate Year [PGY]), race or ethnicity of the subjects (as reported in the publication), objective of the study, reported prevalence of bullying, the instrument used to evaluate bullying, most common source of perpetrators reported, and other factor associated with the presence of bullying.
2.3. Eligibility criteria
Due to prevalence being a condition reported at a specific timeframe, only published and unpublished cross‐sectional studies were included. Articles that evaluated bullying using a validated questionnaire, or used a questionnaire with a specific question addressing bullying or provided a definition for bullying that included a persistent negative behavior rather than isolated incidents, with a power imbalance between the victim and the perpetrator, were included. Furthermore, articles without full text and not reporting the prevalence of bullying were excluded. All authors independently assessed the eligibility of the articles to be considered in the final analysis.
2.4. Outcome measurement of the study
The two main outcomes were the prevalence of bullying in medical residents and the factors associated with bullying. The prevalence of bullying was extracted as a reported proportion by the authors of the included studies, measured with either a bullying scale or a bullying questionnaire. Factors associated with bullying were extracted as reported by the authors of the included studies, including but not limiting to medical specialty, race or ethnicity of the subjects, source of bullying, acts of bullying, and psychological outcomes like burnout.
2.5. Quality assessment
Two authors independently assessed the quality of each studies using the AXIS tool to evaluate the risk of bias for cross‐sectional studies. 31 The studies were assessed for methodological quality, comparability, and the outcome of statistical analysis using established evaluation criteria. A predefined score of 17 of 20 for high‐quality studies was set by the research team. Discrepancies between evaluators during the quality appraisal process were resolved by internal discussion and, if no agreement was reached, a third author settled the discrepancies.
2.6. Data processing and analysis
The data extracted from the identified articles were recorded in a Microsoft Excel spreadsheet and cleaned for analysis. Numeric data were reported using measures of central tendency and dispersion, while categorical data were reported as frequencies and percentages. We estimated the prevalence of bullying in medical residents using a binomial–normal model for meta‐analysis of prevalence via the generalized linear mixed model. 32 Prevalence estimates were reported as binomial proportions with 95% confidence intervals (CIs). The heterogeneity of the studies was assessed using Cochrane's Q‐test and I 2 with its corresponding p‐value. A statistical test with a p value of less than .10 was considered significant for heterogeneity. 29 The values defined as the demarcation of low, moderate, and high heterogeneity were 25%, 50%, and 75% respectively. 33 A fixed‐effects model was applied when there was low heterogeneity and a random‐effects model was used when heterogeneity was moderate or high. A subgroup analysis based on PGY was planned a priori; nevertheless, the amount of included studies that reported PGY was not enough to do a proper analysis. All analysis was performed in R statistical software version 4.2.2 and p values less than 0.05 were considered statistically significant.
3. RESULTS
A total of 816 articles were retrieved on the initial search. From these, 25 articles were excluded due to duplication. After title and abstract screenings, 733 articles were excluded, leaving 58 articles to assess for eligibility. Of those articles, 13 were included in the qualitative and quantitative synthesis. Figure 1 provides a visual representation of the literature screening process.
FIGURE 1.
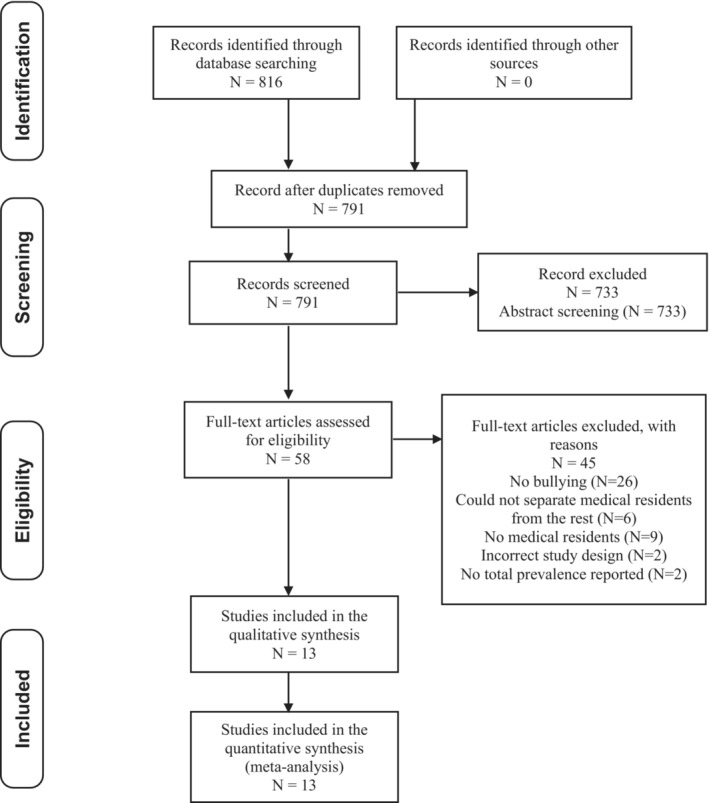
PRISMA flow diagram. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta‐Analyses.
3.1. Characteristics of the studies and study participants
We analyzed 13 cross‐sectional studies, which included a total of 44 566 participants. Of the included articles, eight were from the United States, 9 , 16 , 34 , 35 , 36 , 37 , 38 , 39 one from Australia, 40 one from Australia and New Zealand, 41 one from India, 42 one from Pakistan, 43 and a multi‐country study that included several Latin American countries. 44
The most frequently included medical residency was of surgical nature, with nine studies including them 9 , 34 , 35 , 36 , 38 , 39 , 40 , 42 , 44 and seven studies conducted only in surgical specialties without including any other specialty. 34 , 35 , 36 , 38 , 39 , 40 , 44 Interestingly, none of the studies coincided with the definition of bullying, but shared common points like the need of being a repetitive behavior that causes a negative impact. Of the included studies, six did not directly provide a definition. 35 , 36 , 37 , 39 , 41 , 44 The rest of the studies' characteristics can be seen in Table 1.
TABLE 1.
Baseline characteristics of the included studies.
| Author (year), Region | Total participants (medical specialty/residency) | Participants | Study objective | Instrument used | Bullying prevalence | AXIS score | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| According to their residency year, n (%) | Race/ethnicity % | Total, n (%) | Women, n (%) | Men, n (%) | Most common source (perpetrators) | |||||
|
Zhang et al. (2020) 34 United States |
6264 (General surgery) | NR | Non‐Hispanic White 15.9% Minorities/other 21% | Examine prevalence, types, sources, and factors associated with bullying reported by US general surgery residents | S‐NAQ | 4191 (66.9) | NR | NR |
Attendings (31.45%) Other residents (26.87%) Not identified (25.58%) |
14 |
|
Chia et al. (2022) 35 United States |
564 (Vascular surgery) |
PGY1: 65 (11.5) PGY2–3: 140 (24.8) PGY4–5: 111 (19.7) PGY6–7: 248 (44) |
White 54% Asian 24.1% Hispanic/Latino 4.7% Black 4.3% Other 7.1% Prefer not to say 5.8% |
Inform initiatives to improve wellness by assessing the prevalence of hazards in vascular training and the rates of wellness outcomes | Instrument was developed from validated instruments by a multidisciplinary committee of qualitative researchers, surgical faculty, and trainees | 307 (36.2) | 498 (49.2) | 373 (30) | NR | 14 |
|
Heiderscheit et al. (2021) 36 United States |
6381 (General surgery) |
PGY1: 1585 (24.83) PGY2–3: 2535 (39.72) PGY4–5: 2261 (35.43) |
Asian, Native Hawaiian, or Pacific Islander 18.03% Black or African American 5.08% White 67.44% Other or prefer not to say 12% |
Determine the national prevalence of mistreatment and poor well‐being for LGBTQ+ surgery residents compared with their non‐LGBTQ+ peers | S‐NAQ | 3950 (67.3) | 1777 (72.91) | 2173 (63.33) |
Attendings (76.52%) Co‐residents (30.27%) |
16 |
|
Kemper and Schwartz (2020) 37 United States |
1956 (Pediatrics) | NR |
African American 4% Asian 16% Caucasian 66% Hispanic/Latino 4% Other/mixed/prefer not to answer 10% |
(1) Describe the prevalence of bullying, discrimination, sexual harassment, and physical violence; (2) Assess the epidemiology of these experiences; and (3) analyze the relationship between them and burnout | A survey through the Association of Pediatric Program Directors' longitudinal educational assessment research network | 371 (19) | 274 (20) | 95 (16) |
Clinical staff (60%) Family members of patients (54%) Faculty (43%) Fellow resident/colleague (28%) |
13 |
|
Pei et al. (2019) 38 United States |
180 (Surgery) | NR | NR | Evaluate the incidence of bullying acts experienced by surgeons in the US | NAQ‐R | 71 (39.9) | NR | NR | NR | 7 |
|
Ayyala et al. (2019) 16 United States |
21 212 (Internal medicine) | NR | NR | Describe the prevalence of bullying among internal medicine trainees | Self‐report | 2875 (13.6) | 1347 (14) | 1528 (13) | NR | 12 |
|
De la Cerda‐Vargas et al. (2022) 44 Latin America |
111 (Neurosurgery) |
PGY1: 17 (15.3) PGY2: 19 (17.1) PGY3: 34 (30.6) PGY4: 21 (18.9) PGY5: 18 (16.2) PGY6+: 2 (1.8) |
NR | NR | Survey developed based on previous surveys focused on mistreatment, discrimination, and burnout in residents with surgical training | 84 (75) | 23 (92) | 60 (69.76) |
Other residents (42%) Patients and their relatives (28%) Managers and bosses (23%) |
14 |
|
Ling et al. (2016) 40 Australia |
370 (General surgery) | NR | NR | Determine the extent and nature of workplace bullying among general surgery trainees and consultants in Australia | NAQ‐R | 173 (47) | 67 (57) | 106 (42) |
Consultant surgeons (39%) Administration (20%) Nurses (11%) |
13 |
|
Chadaga et al. (2016) 9 United States |
1791 (16 Different residencies) |
PGY1: 389 (22) PGY2–8: 1367 (76) Prefer not to say 35 (2) |
White 63% Other ethnic groups 30% Prefer not to say 7% |
Deliver an estimated of bullying among residents and fellows in the US graduate medical education system and to explore its prevalence within unique subgroups | Self‐report | 860 (48) | 483 (52) | 364 (43) |
Attendings (29%) Nurses (27%) Patients (23%) Peers (19%) Consultants (19%) Ancillary staff (8%) |
16 |
|
Bairy et al. (2007) 42 India |
174 (Different residencies) | NR | NR | Determine the prevalence of persistent and serious bullying among junior doctors, identify its sources and determine if any personality trait pointed toward being a “bully” | Bullying survey questionnaire | 89 (51.1) | 35 (48.6) | 54 (52.9) |
Para‐clinical (35.6%) Medical personnel (15.5%) Patients or their relatives (6.3%) |
15 |
|
Hussain and Rahim (2014) 43 Pakistan |
246 (Different residencies) | NA | NA | Determine prevalence of bullying among postgraduate medical trainees in tertiary care hospitals in Peshawar | A questionnaire based on basic five types of bullying according to Rayner and Hoel 6 | 204 (89.02%) | NA | NA |
Senior registrars (20%) Junior registrars (18%) Fellow colleagues (17%) Nurses (16%) Professors (11%) |
8 |
|
Brajcich et al. (2021) 39 United States |
5574 (Surgery) |
PGY1: 1377 (24.4) PGY2–3: 2295 (40.3) PGY4–5: 2029 (35.6) |
White 66.3% Black 5% Asian 17.7% Other 10.1% Prefer not to say 4.9% |
To undertake a national evaluation of the association of resident unions with well‐being and working conditions among residents | Survey adapted from previous surveys following the American Board of Surgery | 3735 (67%) | NA | NA | NA | 18 |
|
Downey et al. (2021) 41 Australia and New Zealand |
417 (Anesthesiologist) | NA | NA | To investigate levels of stress, anxiety, and depression, and to identify factors exacerbating or relieving stress in anesthesia trainees | Survey questions based on a previous survey from the same authors | 185 (44.36%) | NA | NA | NA | 16 |
Note: Senior registrars are medical doctors that have completed their postgraduate training and are undergoing further training under supervision of a consultant or specialist. Junior registrars have the same characteristics as senior registrars, with the difference being that junior registrars have recently completed their undergraduate medical education. Adding up percentages might not result in 100% because of rounding.
Abbreviations: NR, not reported; PGY, postgraduate year; S‐NAQ: The Short‐Negative Act Questionnaire.
3.2. Prevalence of bullying
The overall pooled prevalence of bullying in medical residents was 51% (95% CI 36–66; Figure 2).
FIGURE 2.
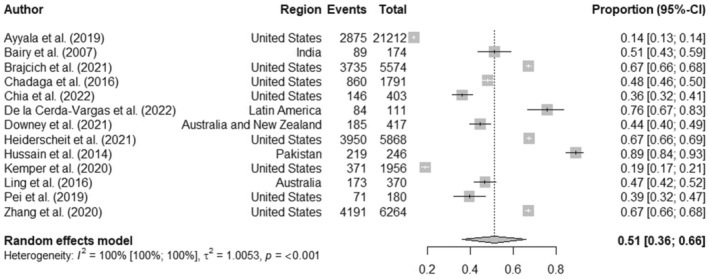
Pooled prevalence of bullying in medical residents.
3.3. Heterogeneity and publication bias
This systematic review and meta‐analysis detected high heterogeneity (I 2 = 100%; p < .001). A preplanned sensitivity analysis was performed by recalculating the pooled effects while omitting one study at a time (leave‐one‐out method). The studies by Hussain et al., 43 Kemper and Schwartz 37 and Ayyala et al. 16 showed a possible influence in the overall pooled proportion. This influence could be due to the abstract nature of bullying, along with the subjectivity and heterogeneity of its definition. The full leave‐one‐out sensitivity analysis can be seen in Figure S1. A funnel plot was performed to visually evaluate publication bias (Figure S2). Although the visual inspection of the funnel plot might show asymmetry, Egger's test did not indicate the presence of funnel plot asymmetry (p = .5820).
3.4. Factors associated with prevalence of bullying
3.4.1. Sex
Seven of the 13 reviewed articles explored the type of relationship between bullying and participant's sex. Five of them reported a higher prevalence of bullying among women, 9 , 34 , 35 , 36 , 44 and one detected a higher proportion of negative behaviors but there was not a significant difference in the mean Negative Acts Questionnaire (NAQ)‐scores between men and women. 40 One study calculated higher odds (OR 1.98, 95% CI 1.45–2.70) of experiencing bullying for females. 38
Interestingly, only one article found out that the odds of being bullied when the resident was a part of the LGBTQ+ community was 1.51 (95% CI, 1.07–2.12) for males while for females, it was 2.00 (95% CI, 1.37–2.92). 36
3.4.2. Bullying source and acts
Eight of the included studies asked participants to identify the most common perpetrators of bullying, with attending physicians being mentioned as one of the most frequent sources in all of the studies and as the main perpetrators in four studies. 9 , 34 , 36 , 40 In the work presented by Kemper and Schwartz, the most common source of bullying was clinical staff (nursing, therapy). 37 The only study that reported co‐residents as the number one perpetrator (42%) was the one by De la Cerda‐Vargas et al., 44 which focused on neurosurgery residents. The former also reported a difference between bullying perpetrators depending on the sex of the victim, bullying was more frequently inflicted on female residents by professors than on male residents (44% vs. 15%; p = .002; Yates correction p = .005).
Only three articles specified the most common bullying acts. 34 , 36 , 43 Two studies coincided in that the two most common acts were being repeatedly reminded of errors or mistakes and being shouted at the second most common. They differed in the third most reported act; Zhang et al. mentioned withholding important information while Heiderscheit et al. mentioned persistent criticism of work or effort. It is worth mentioning that Heiderscheit et al. reported that the sources of discrimination were similar for medical residents that are part of the LGBTQ+ community and non‐LGBTQ+ residents. Hussain et al. reported that their most common form of bullying was verbal, with 26% of doctors being disturbed because of repeated inappropriate jokes about them.
3.4.3. Ethnicity and bullying
Four of the studies explored the relationship between bullying and race/ethnicity. 9 , 34 , 43 , 44 Zhang et al. reported that racial/ethnic minorities experienced bullying more frequently (21.0%) than non‐Hispanic white participants (15.9%). Chadaga et al. reported that non‐White residents tend to report more bullying behaviors when compared to White residents. Hussain and Rahim identified that participants identified a prevalence of bullying based of ethnicity and gender of 16.7%.
In Latino population, a difference in the source of bullying was reported by De la Cerda‐Vargas et al. between Mexicans and non‐Mexicans; for Mexicans, the main source was other residents (42%), while non‐Mexicans were targeted more often by managers and bosses (29.6% vs. 12.5%; p = .04).
3.4.4. Bullying and burnout
Two studies associated bullying or any mistreatment as a risk factor for medical residents for burnout. 35 , 37 Chia et al. reported an OR of 3.09 (95% CI, 1.78–5.39) while Kemper and Schwartz reported an adjusted OR of 1.8 (95% CI, 1.62–2.42). 32 , 34 , 35 , 37 Additionally, Kemper also reported that in the frequency of mistreatment, each higher “dose” of mistreatment was associated with an adjusted OR of 3.01 (95% CI, 2.06–4.40).
3.5. Quality assessment
Only one 39 of the included articles met the prespecified criteria for high quality with the AXIS tool. The median of the AXIS scores was 14 (interquartile range 12.5–16). A detailed report on the quality assessment is reported in Table S3.
4. DISCUSSION
In this systematic review and meta‐analysis, the pooled prevalence of bullying in medical residents is 51%, which likely resides between 36% and 66% with 95% confidence, which indicates that there is a high prevalence of bullying among medical residents in the world. This high prevalence might be due to an absence of bullying prevention programs in teaching hospitals, limited to non‐existent media coverage of bullying in medical residents, and/or a lack of a consistent definition of bullying.
Bullying in the general workforce has been estimated at a prevalence of 38%. 45 Prevalence of bullying in the medical workforce has been reported at 25%. 19 Medical student's prevalence of bullying has been reported as well, with prevalences from 46.4% to 59.4%. 22 , 46 Although comparing numerically the prevalence of bullying sounds like a logical process, all of the reported prevalence should be considered high since bullying in any workplace should be nonexistent.
It is worth noting that the problem of bullying in the medical environment starts during undergraduate education, as medical students are more likely to experience inappropriate treatment compared to students in other degree programs. 8 While previous studies have explored the prevalence of bullying in medical students and residents, this study provides a specific focus on medical residents across various specialties. 46 , 47 , 48 , 49 , 50 , 51 , 52 However, the lack of consensus among experts regarding the definition of bullying, which is often used interchangeably with terms like discrimination or harassment, highlights the need for further research in this area. Overall, the findings of this study suggest that addressing bullying in medical residency programs should be a priority, and effective interventions and preventative measures need to be developed.
The included studies identified several associating factors of bullying. Among the associated factors, being a woman was reported as a risk factor to experience bullying, which follows the results of other studies. 53 , 54 , 55 Regarding the most common perpetrators, studies seem to differ in their reports. A study done in the general healthcare workforce of Greece reported that the most common source of bullying was colleagues of the same hierarchy (66.7%) followed by superiors (58.7%). 56 Even if they are not the most common, workers that have a superior hierarchy in the healthcare workforce, like attending physicians, are repeatedly reported as one of the most common source which goes along with the generational misunderstandings that harsh treatment is an essential part of medical education.
The two most common acts of bullying were being repeatedly reminded of errors or mistakes and being shouted at, both of which can be categorized as verbal bullying. Verbal aggression or verbal bullying has been reported as the most common acts of bullying in the medical workplace, although the specific acts vary. 11
Throughout bullying research, a wide variety of terms to describe negative interactions in the workplace have been used by researches, some of which not only describe bullying behaviors but also different constructs like discrimination. 23 Discrimination is the differential treatment or unequal access to opportunities based on certain characteristics, and, although discrimination has a different definition from bullying, it can lead to bullying behaviors. Zhang et al.'s study which is reported that minorities experience bullying more frequently is an example of this phenomenon. 34
Bullying is associated with medical burnout. Burnout has been reported as a prevalent condition in the healthcare area, especially after the COVID‐19 pandemic, with a pooled prevalence of 41% (95% CI 20.7–61.3). 57 Although there are several factors that can influence burnout in healthcare, bullying was identified as a factor on two of the included studies.
Our study falls in line with the Joint Commission's Sentinel Event Alert, which stated that intimidation and disruptive behaviors in healthcare are not rare. 58 Furthermore, this phenomenon creates an unhealthy and, sometimes, hostile environment reinforcing the need for healthcare professionals to focus on this issue.
The rapid technological and social progress that has taken place in the last century have allowed us to live with more freedom and at a higher standard than before. 26 Of course, this advancement also reflects in the medical field; healthcare professionals with more experience in their respective fields might look that the habits of new residents with contempt. This, along with the generational misunderstandings and the belief that harsh treatment is an essential part of medical education contribute to the ongoing uphill challenge of eradicating bullying in the medical community. 25 , 59 , 60
To the knowledge of the authors, this article is the first one to provide a pooled prevalence of bullying in all medical residencies in the world. There are some limitations to this review. All included studies in this systematic review and meta‐analysis were cross‐sectional studies, which may limit the generation of a causal‐effect link between independent and dependent variables. There also has been a reported difficulty to compare data across countries, especially when comparing data from countries that have a different language. 8 , 61 Another limitation is the quality of the included studies. Only one of the included studies reached the prespecified score for high quality, with domains with the lowest scores being related to addressing non‐respondents and justifying the sample size. The final results should be interpreted cautiously and only after grasping the risk of bias assessment.
The preferred instrument, identified in this review, to measure bullying in medical residents was the NAQ with its variations. This questionnaire was not specifically designed for medical residents. As mentioned before, medical residents are a special kind of population since their responsibilities land on student‐like responsibilities and teacher/attending‐like responsibilities, and evaluating them with a nonspecific questionnaire might yield unveracious results. Future research should focus in either designing a questionnaire specifically for medical residents or validating an existing one. Furthermore, future studies should focus on clearly establishing risk factors for bullying so that specific effective interventions can be designed. Although there has been heterogeneity in the reports, there is no doubt that bullying is present during medical residency worldwide.
5. CONCLUSION
This systematic review and meta‐analysis found that the prevalence of bullying among medical residents is high, with an overall prevalence of 51%. The findings suggest that bullying is a significant issue in medical residency programs and highlights the need for interventions to prevent and address bullying in this setting. Further research is needed to identify the factors contributing to bullying and to develop effective strategies to prevent and address this problem.
AUTHOR CONTRIBUTIONS
Neri Alejandro Álvarez Villalobos, Gabriela Guadalupe Elizondo Omaña, and Humberto De León Gutiérrez designed the study and run the literature search. Same authors acquired data, screened records, extracted data, and assessed the risk of bias. Neri Alejandro Álvarez Villalobos, Humberto De León Gutiérrez, Fernando Gerardo Ruiz Hernandez, Francisco Javier Carranza Guzmán, and Héctor Alejandro Vaquera Alfaro did statistical analyses and wrote the report. All authors provided critical conceptual input, analyzed, and interpreted the data, and critically revised the report. All authors read and approved the final manuscript. Neri Alejandro Álvarez Villalobos is the designated guarantor. The manuscript titled “Prevalence and associated factors of bullying in medical residents: A systematic review and Meta‐analysis,” has been read and approved by all the authors. All authors have met the authorship requirements and believe that the manuscript represents honest work.
CONFLICT OF INTEREST STATEMENT
Authors declare no conflict of interests for this article.
DISCLOSURE
Ethic Approval: Not applicable. Informed Consent: Not applicable. Registry and the Registration No. of the Study/Trial: The protocol for this systematic review and meta‐analysis has been registered in PROSPERO (International Prospective Register of Systematic Reviews) with the registration number CRD42022333170. Animal Studies: Not applicable.
Supporting information
Figure S1.
Figure S2.
Table S1.
Table S2.
Table S3.
Álvarez Villalobos NA, De León Gutiérrez H, Ruiz Hernandez FG, Elizondo Omaña GG, Vaquera Alfaro HA, Carranza Guzmán FJ. Prevalence and associated factors of bullying in medical residents: A systematic review and meta‐analysis. J Occup Health. 2023;65:e12418. doi: 10.1002/1348-9585.12418
DATA AVAILABILITY STATEMENT
All data relevant to the study are included in the article or uploaded as supplementary information.
REFERENCES
- 1. Quine L. Workplace bullying in junior doctors: questionnaire survey. BMJ. 2002;324(7342):878‐879. doi: 10.1136/bmj.324.7342.878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cheema S, Ahmad K, Giri SK, Kaliaperumal VK, Naqvi SA. Bullying of junior doctors prevails in Irish health system: a bitter reality. Ir Med J. 2005;98(9):274‐275. [PubMed] [Google Scholar]
- 3. Kelly S. Workplace bullying: the silent epidemic. N Z Med J. 2004;117(1204):U1125. [PubMed] [Google Scholar]
- 4. Silver HK. Medical students and medical school. J Am Med Assoc. 1982;247(3):309‐310. doi: 10.1001/jama.1982.03320280029024 [DOI] [PubMed] [Google Scholar]
- 5. Lyons R, Tivey H, Ball C. Bullying at work: how to tackle it; a guide for MSF representatives and members. MSF. 1995. Accessed August 29, 2022. https://scholar.google.com/scholar_lookup?title=Bullying+at+work:+how+to+tackle+it.+A+guide+for+MSF+representatives+and+members.&author=R+Lyons&author=H+Tivey&author=C+Ball&publication_year=1995&
- 6. Rayner C, Hoel H. A summary review of literature relating to workplace bullying. J Community Appl Soc Psychol. 1997;7(3):181‐191. doi: [DOI] [Google Scholar]
- 7. Olweus D. Bullying at School: What We Know and What We Can Do. 1st ed. Blackwell Publishing, Inc.; 1993. [Google Scholar]
- 8. Bormuth S, Ackermann H, Schulze J. Inadequate treatment in internships: a comparison between medical and other students. GMS J Med Educ. 2021;38(2):1‐17. doi: 10.3205/zma001441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chadaga AR, Villines D, Krikorian A. Bullying in the American Graduate Medical Education System: a national cross‐sectional survey. PLoS One. 2016;11(3):e0150246. doi: 10.1371/journal.pone.0150246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mejia R, Diego A, Aleman M, Del Rosario MM, Lasala F. Percepcion de maltrato durante la capacitacion de medicos residentes. Medicina (B Aires). 2005;65(4):295‐301. [PubMed] [Google Scholar]
- 11. Afolaranmi TO, Hassan ZI, Gokir BM, et al. Workplace bullying and its associated factors among medical doctors in residency training in a tertiary health institution in Plateau State Nigeria. Front Public Health. 2022;9:812979. doi: 10.3389/fpubh.2021.812979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ayyala MS, Chaudhry S, Windish D, Dupras D, Reddy ST, Wright SM. Awareness of bullying in residency: results of a national survey of internal medicine program directors. J Grad Med Educ. 2018;10(2):209‐213. doi: 10.4300/JGME-D-17-00386.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rutherford A, Rissel C. A survey of workplace bullying in a health sector organisation. Aust Health Rev. 2004;28(1):65‐72. doi: 10.1071/AH040065 [DOI] [PubMed] [Google Scholar]
- 14. Fajana S, Owoyemi O, Shadare S, Elegbede T, Gbajumo‐Sheriff M. Gender differences: an antecedent for workplace bullying and harassment in Nigeria workplaces. Eur J Soc Sci. 2011;21:448‐455. [Google Scholar]
- 15. Conway PM, Høgh A, Nabe‐Nielsen K, et al. Optimal cut‐off points for the short‐negative act questionnaire and their association with depressive symptoms and diagnosis of depression. Ann Work Expo Heal. 2018;62(3):281‐294. doi: 10.1093/annweh/wxx105 [DOI] [PubMed] [Google Scholar]
- 16. Ayyala MS, Rios R, Wright SM. Perceived bullying among internal medicine residents. JAMA. 2019;322(6):576‐578. doi: 10.1001/jama.2019.8616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Loerbroks A, Weigl M, Li J, Glaser J, Degen C, Angerer P. Workplace bullying and depressive symptoms: a prospective study among junior physicians in Germany. J Psychosom Res. 2015;78(2):168‐172. doi: 10.1016/j.jpsychores.2014.10.008 [DOI] [PubMed] [Google Scholar]
- 18. Leisy HB, Ahmad M. Altering workplace attitudes for resident education (A.W.A.R.E.): discovering solutions for medical resident bullying through literature review. BMC Med Educ. 2016;16(1):1‐10. doi: 10.1186/s12909-016-0639-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Askew DA, Schluter PJ, Dick ML, Ŕgo PM, Turner C, Wilkinson D. Bullying in the Australian medical workforce: cross‐sectional data from an Australian e‐cohort study. Aust Health Rev. 2012;36(2):197‐204. doi: 10.1071/AH11048 [DOI] [PubMed] [Google Scholar]
- 20. Ortiz‐León S. Experiencias de maltrato y hostigamiento en médicos residentes. Cir Cir. 2014;82(3):290‐301. www.amc.org.mx [PubMed] [Google Scholar]
- 21. Swearer SM, Hymel S. Understanding the psychology of bullying: moving toward a social‐ecological diathesis‐stress model. Am Psychol. 2015;70(4):344‐353. doi: 10.1037/a0038929 [DOI] [PubMed] [Google Scholar]
- 22. Fnais N, Soobiah C, Chen MH, et al. Harassment and discrimination in medical training: a systematic review and meta‐analysis. Acad Med. 2014;89(5):817‐827. doi: 10.1097/ACM.0000000000000200 [DOI] [PubMed] [Google Scholar]
- 23. Samsudin EZ, Isahak M, Rampal S. The prevalence, risk factors and outcomes of workplace bullying among junior doctors: a systematic review. Eur J Work Organ Psychol. 2018;27:1‐19. doi: 10.1080/1359432X.2018.1502171 [DOI] [Google Scholar]
- 24. Leah JD, Maria S, Arthur JC, Dorothy D, Frances RH. Appropriate Treatment in Medicine: A Compendium on Medical Student Mistreatment. Association of American Medical Colleges; 2000. [Google Scholar]
- 25. Brainard AH, Brislen HC. Viewpoint: learning professionalism: a view from the trenches. Acad Med. 2007;82(11):1010‐1014. doi: 10.1097/01.ACM.0000285343.95826.94 [DOI] [PubMed] [Google Scholar]
- 26. Gupta S, Mak S, Detsky AS, Young RK. The other generation. JAMA. 2015;313(13):1319‐1320. doi: 10.1001/jama.2015.1082 [DOI] [PubMed] [Google Scholar]
- 27. Lind KT, Osborne CM, Badesch B, Blood A, Lowenstein SR. Ending student mistreatment: early successes and continuing challenges. Med Educ Online. 2020;25(1):1690846. doi: 10.1080/10872981.2019.1690846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. doi: 10.1002/14651858.ED000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. The EndNote Team . EndNote. 2013. Accessed August 29, 2022. https://support.clarivate.com/Endnote/s/article/Citing‐the‐EndNote‐program‐as‐a‐reference?language=en_US
- 31. Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross‐sectional studies (AXIS). BMJ Open. 2016;6(12):e011458. doi: 10.1136/BMJOPEN-2016-011458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stijnen T, Hamza TH, Özdemir P. Random effects meta‐analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med. 2010;29(29):3046‐3067. doi: 10.1002/sim.4040 [DOI] [PubMed] [Google Scholar]
- 33. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21(11):1539‐1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 34. Zhang LM, Ellis RJ, Ma M, et al. Prevalence, types, and sources of bullying reported by US general surgery residents in 2019. JAMA. 2020;323(20):2093‐2095. doi: 10.1001/jama.2020.2901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chia MC, Hu YY, Li RD, et al. Prevalence and risk factors for burnout in U.S. vascular surgery trainees. J Vasc Surg. 2022;75(1):308‐315. doi: 10.1016/j.jvs.2021.06.476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Heiderscheit EA, Schlick CJR, Ellis RJ, et al. Experiences of LGBTQ+ residents in US general surgery training programs. JAMA Surg. 2022;157(1):23‐32. doi: 10.1001/jamasurg.2021.5246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kemper KJ, Schwartz A. Bullying, discrimination, sexual harassment, and physical violence: common and associated with burnout in pediatric residents. Acad Pediatr. 2020;20(7):991‐997. doi: 10.1016/j.acap.2020.02.023 [DOI] [PubMed] [Google Scholar]
- 38. Pei K, Klingensmith M, Alseidi A, Cochran A. National Assessment of workplace bullying among surgeons in the United States. J Am Coll Surg. 2019;229(4):e50. doi: 10.1016/j.jamcollsurg.2019.08.782 [DOI] [Google Scholar]
- 39. Brajcich BC, Chung JW, Wood DE, et al. National Evaluation of the association between resident labor union participation and surgical resident well‐being. JAMA Netw Open. 2021;4(9):1‐14. doi: 10.1001/jamanetworkopen.2021.23412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ling M, Young CJ, Shepherd HL, Mak C, Saw RPM. Workplace bullying in surgery. World J Surg. 2016;40(11):2560‐2566. doi: 10.1007/s00268-016-3642-7 [DOI] [PubMed] [Google Scholar]
- 41. Downey GB, McDonald JM, Downey RG, Garnett PBJ. Welfare of Anaesthesia trainees survey 2019. Anaesth Intensive Care. 2021;49(6):430‐439. doi: 10.1177/0310057X211017146 [DOI] [PubMed] [Google Scholar]
- 42. Bairy K, Thirumalaikolundusubramanian P, Sivagnanam G, Saraswathi S, Sachidananda A, Shalini A. Bullying among trainee doctors in southern India: a questionnaire study. J Postgrad Med. 2007;53(2):87. doi: 10.4103/0022-3859.32206 [DOI] [PubMed] [Google Scholar]
- 43. Hussain SS, Rahim R. Bullying of postgraduate medical trainees in tertiary care hospitals. J Postgrad Med Inst. 2014;28(3):251‐256. [Google Scholar]
- 44. De la Cerda‐Vargas MF, Stienen MN, Campero A, et al. Burnout, discrimination, abuse, and mistreatment in Latin America neurosurgical training during the coronavirus disease 2019 pandemic. World Neurosurg. 2022;158(2):e393‐e415. doi: 10.1016/j.wneu.2021.10.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dickson D. Bullying in the workplace. Anaesthesia. 2005;60(12):1159‐1161. doi: 10.1111/j.1365-2044.2005.04465.x [DOI] [PubMed] [Google Scholar]
- 46. Silver HK, Glicken AD. Medical student abuse: incidence, severity, and significance. JAMA. 1990;263(4):527‐532. doi: 10.1001/JAMA.1990.03440040066030 [DOI] [PubMed] [Google Scholar]
- 47. Gianakos AL, Freischlag JA, Mercurio AM, et al. Bullying, discrimination, harassment, sexual harassment, and the fear of retaliation during surgical residency training: a systematic review. World J Surg. 2022;46(7):1587‐1599. doi: 10.1007/S00268-021-06432-6 [DOI] [PubMed] [Google Scholar]
- 48. Chávez‐Rivera A, Ramos‐Lira L, Abreu‐Hernández LF. [A systematic review of mistreatment in medical students]. Gac Med Mex. 2016;152(6):796‐811. [PubMed] [Google Scholar]
- 49. Ogden PE, Wu EH, Elnicki MD, et al. Do attending physicians, nurses, residents, and medical students agree on what constitutes medical student abuse? Acad Med. 2005;80(10):S80‐S83. doi: 10.1097/00001888-200510001-00022 [DOI] [PubMed] [Google Scholar]
- 50. Richman JA, Flaherty JA, Rospenda KM, Christensen ML. Mental health consequences and correlates of reported medical student abuse. JAMA. 1992;267(5):692‐694. doi: 10.1001/JAMA.1992.03480050096032 [DOI] [PubMed] [Google Scholar]
- 51. Baldwin DC, Daugherty SR, Eckenfels EJ. Student perceptions of mistreatment and harassment during medical school. a survey of ten United States schools. West J Med. 1991;155(2):140. [PMC free article] [PubMed] [Google Scholar]
- 52. Sheehan KH, Sheehan DV, White K, Leibowitz A, Baldwin DC. A pilot study of medical student “abuse”: student perceptions of mistreatment and misconduct in medical school. JAMA. 1990;263(4):533‐537. doi: 10.1001/JAMA.1990.03440040072031 [DOI] [PubMed] [Google Scholar]
- 53. Pei KY, Hafler J, Alseidi A, Slade MD, Klingensmith M, Cochran A. National assessment of workplace bullying among academic surgeons in the US. JAMA Surg. 2020;155(6):524‐526. doi: 10.1001/jamasurg.2020.0263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. La Torre G, Firenze A, Colaprico C, et al. Prevalence and risk factors of bullying and sexual and racial harassment in healthcare workers: a cross‐sectional study in Italy. Int J Environ Res Public Health. 2022;19(11):6938. doi: 10.3390/ijerph19116938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Syed F, Sajid Mithani M, Abu Mostafa F, et al. Prevalence of aggressive behavior toward fellows, residents, and nurses at a Tertiary Care Hospital in Riyadh, Saudi Arabia. Cureus. 2022;14:e24142. doi: 10.7759/cureus.24142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Gkagkanteros A, Kontodimopoulos N, Talias MA. Does bullying in the hospital affect the health‐related quality of life of health professionals? Work. 2022;73(1):263‐272. doi: 10.3233/WOR-210306 [DOI] [PubMed] [Google Scholar]
- 57. Alkhamees AA, Aljohani MS, Kalani S, et al. Physician's burnout during the COVID‐19 pandemic: a systematic review and meta‐analysis. Int J Environ Res Public Health. 2023;20(5):4598. doi: 10.3390/ijerph20054598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. The Joint Commission . Behaviors that undermine a culture of safety. Sentinal Event Alert 40; 2008. Accessed October 28, 2022. http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_40.htm?print=yes [PubMed]
- 59. Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students' perceptions of teaching. BMJ. 2004;329(7469):770‐773. doi: 10.1136/BMJ.329.7469.770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Crowe S, Clarke N, Brugha R. ‘You do not cross them’: hierarchy and emotion in doctors' narratives of power relations in specialist training. Soc Sci Med. 2017;186:70‐77. doi: 10.1016/J.SOCSCIMED.2017.05.048 [DOI] [PubMed] [Google Scholar]
- 61. Hilbert N. Negativer Rückblick Oder Positive Aussicht? Eine Online‐Befragung Studierender Der Medizin Über Ihre Erfahrungen Während Des Studiums. Georg‐August‐Universität Zu Göttingen; 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1.
Figure S2.
Table S1.
Table S2.
Table S3.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.


