Abstract
BACKGROUND
Worldwide, people with hypertensive urgency experience high rates of hospitalization and death due to medication non-adherence. Interventions to improve medication adherence and health outcomes after hypertensive urgency are urgently needed.
METHODS
This prospective cohort assessed the effect of a peer counselor intervention—named Rafiki mwenye msaada—on the 1-year incidence of hospitalization and/or death among adults with hypertensive urgency in Mwanza, Tanzania. We enrolled 50 patients who presented with hypertensive urgency to 2 hospitals in Mwanza, Tanzania. All 50 patients received a Rafiki mwenye msaada an individual-level, time-limited case management intervention. Rafiki mwenye msaada aims to empower adult patients with hypertensive urgency to manage their high blood pressure. It consists of 5 sessions delivered over 3 months by a peer counselor. Outcomes were compared to historical controls.
RESULTS
Of the 50 patients (median age, 61 years), 34 (68%) were female, and 19 (38%) were overweight. In comparison to the historical controls, the intervention cohort had a significantly lower proportion of patients with a secondary level of education (22% vs. 35%) and health insurance (40% vs. 87%). Nonetheless, the 1-year cumulative incidence of hospitalization and/or death was 18% in the intervention cohort vs. 35% in the control cohort (adjusted Hazard Ratio, 0.48, 95% CI 0.24–0.97; P = 0.041). Compared to historical controls, intervention participants maintained higher rates of medication use and clinic attendance at both 3- and 6-months but not at 12 months. Of intervention participants who survived and remained in follow-up, >90% reported good medication adherence at all follow-up time points.
CONCLUSION
Our findings support the hypothesis that a peer counselor intervention may improve health outcomes among adults living with hypertensive urgency. A randomized clinical trial is needed to evaluate the intervention’s effectiveness.
Keywords: adherence, blood pressure, hospitalization, hypertension, hypertensive urgency, mortality, peer counselor intervention, Tanzania
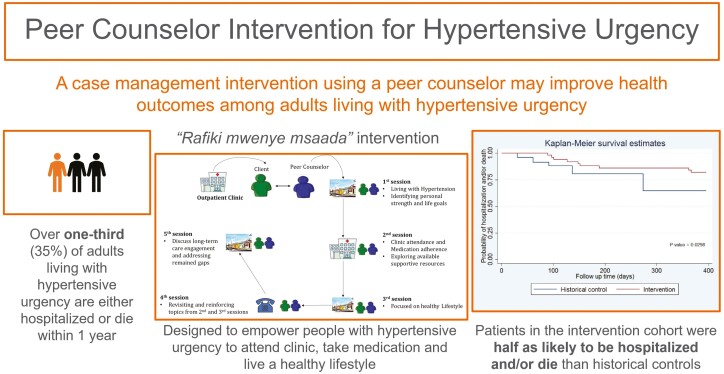
Graphical Abstract
Graphical Abstract.
Globally, hypertension is the greatest risk factor for morbidity and mortality.1 It is estimated that nearly 1 billion people have hypertension,2 about half of them reside in sub-Saharan Africa (SSA).3 Among individuals with hypertension, 1%–2% develop hypertensive crisis—defined as blood pressure (BP) above 180/120 mm Hg—in their lifetime.4 Hypertensive crisis is often fatal if left untreated.5
We and others have documented that hypertensive crisis was common in a typical outpatient clinic or emergency department in Tanzania.6,7 Also, in our previous report, the 1-year cumulative rate of hospitalization and/or death among adult patients with hypertensive urgency—defined as a hypertensive crisis without end-organ damage8—was 35% compared to 1%–18% reported in the United States and Italy.7,9,10 Patients who reported poor adherence to anti-hypertensive medications at the time of enrollment were at the highest risk of re-hospitalization and/or death.8 Qualitative research exploring factors that drive and inhibit engagement with clinical care among Tanzanian adults with hypertensive urgency11 found many similarities to what we have previously observed in people with advanced HIV disease.12 Similar factors included traditional health beliefs, low self-efficacy, lack of transportation, lack of social support, stigma, and low perceived need for medical care. These findings highlighted the need to incorporate social medicine interventions in our therapeutic approach to hypertensive urgency to address social barriers to care engagement.
We therefore adapted a social worker intervention that we have used to increase antiretroviral therapy in Tanzanians with HIV,13,14 for use by peer counselors to improving health outcomes in people with hypertensive urgency. The rationale for adopting this social worker intervention was the observed similarity of challenges to care engagement between adult patients with hypertensive urgency and those living with HIV in our setting together with the impact of this intervention on both increasing linkage to outpatient care and 1-year survival.12 Moreover, literature has shown that peer support interventions have the potential to improve self-efficacy among patients with heart diseases.15 However, no such studies have yet been published to evaluate social interventions for hypertensive urgency.
This prospective cohort study with historical controls aimed to assess the association between a peer counselor intervention and the 1-year cumulative incidence of hospitalization and/or death among adult patients with hypertensive urgency in Mwanza, Tanzania.
METHODS
Overview
This was a prospective cohort study with historical controls aimed at assessing the association between a peer counselor intervention and the 1-year cumulative incidence of hospitalization and/or death among adults with hypertensive urgency. The study involved 50 patients who were receiving hypertensive care from outpatient clinics in 2 hospitals in Mwanza, Tanzania. The study received ethical approval from the Weill Cornell Medicine [Ref: 19-11021145] and the Tanzanian National Institute for Medical Research [Ref: NIMR/HQ/R.8a/Vol. IX/3349].
Setting
The study was conducted in the medical outpatient clinics of 2 government hospitals in Mwanza City, Tanzania. The 2 study sites together serve approximately 2,500 adults living with hypertension annually. All clinics were following the national guidelines for treating hypertension, which recommends thiazide diuretics as a first-line treatment. Combination therapy including a calcium channel blocker is considered if the first line does not achieve BP control.16 Although anti-hypertensive medications are widely available and relatively inexpensive by high-income country’s standards, they can still be cost-prohibitive for most Tanzanians who live at <$100/month. For most patients on 2 or more medications, the average monthly cost of medications starts from $17 US dollars (USD) per month. Patients pay for services through a combination of insurance, government subsidy, and out-of-pocket contributions.
Participants
The intervention cohort.
Patients with hypertensive urgency, defined as BP above 180/120 mm Hg without end-organ damage,8 were eligible to participate if they met the following criteria:
Minimum 18 years of age
Lives in the city of Mwanza
Has mobile phone or access to mobile phone
Planning to stay in the city of Mwanza for the next 12 months
Willing to have a home visit by a peer counselor and/or a study team member
Patients with hypertensive urgency were excluded from study enrollment if they had a history of cardiovascular or end-stage renal disease, or a known diagnosis with prognosis of less than 1 year of survival. Study enrollment for the intervention cohort occurred between August and December 2020, with follow-up occurring through December 2021.
The historical cohort.
Patients with hypertensive urgency who attended medical outpatient clinic at one of the same hospitals served as a historical control cohort. The inclusion criteria and survey methodology were the same as for the intervention cohort.
The historical control cohort involved 150 adult patients with hypertensive urgency who were enrolled in a registry of hypertensive urgency at Bugando Medical Centre between October 2018 and February 2019, with follow-up occurring through March 2020. The previously published manuscript provides additional details about the baseline characteristics and 1-year follow-up outcomes.6
Both historical control and intervention cohorts received similar standardized treatment at the standard of care, guided by the Tanzania Ministry of Health guidelines for the treatment of hypertension. The medical staff and the standard of care for hypertension remained comparable during the implementation of both cohorts.
Procedures
After the routine hypertension screening, the clinic nurse introduced the study to the hypertensive urgency patients at the outpatient clinic. If a patient expressed interest in participating in the study, the nurse referred the patient to the study team to receive additional information, confirm eligibility, and complete written informed consent procedures in a private room. We limited the number of enrollments per week to 3 participants per site, to ensure reasonable workload for peer counselors.
Upon enrollment, all participants provided contact information, including an alternative contact, and their preferences of how they could be reached for future follow-up and completed a structured baseline survey enumerated by the trained research assistant. The follow-up surveys were conducted monthly in the first 3 months, at 6- and 12-month follow-up, and implemented via phone calls.
Intervention
Following completion of enrollment procedures, each study participant was assigned to a peer counselor, who was responsible to deliver the intervention called Rafiki mwenye msaada (“A helpful friend”). The peer counselors were patients with hypertension, with well-controlled BP, and attending hypertension care at the respective outpatient clinic. All peer counselors received an intensive 2-week training on how to deliver the intervention. The training was conducted by a team of experienced medical doctors and social scientists.
Rafiki mwenye msaada.
Rafiki mwenye msaada is an individual-level, time-limited, 5-session case management intervention with the goal of empowering adult patients with hypertensive urgency to manage their high BP. The intervention was based on the Antiretroviral Treatment and Access to Services (ARTAS) intervention13,14 which we had previously adapted for use in people with advanced HIV in Tanzania.12 The Rafiki mwenye msaada’s intervention involved 5 sessions with patients over 3 months (see Table 1). The first session occurred at the participant’s home within 2 days after being enrolled into the study and aimed to briefly introduce the intervention and build the social relationship between the peer counselor and patient. The second session occurred 1 week after the first session at the participant’s outpatient clinic and focused on the importance of medication adherence and personal treatment goals and targets. Also, in this session, use of traditional herbal medicines and access to resources to support treatment costs, such as health insurance and medical exemptions, were discussed. The third session occurred at approximately 4 weeks at the participant’s home and focused on a healthy lifestyle including diet and exercise. The fourth session was done over the phone at ~6 weeks and the goal of this session was to follow-up on the participant’s progress in taking medications, attending the clinic, and following lifestyle recommendations. The fifth and final session occurred at 10–12 weeks at the participant’s house and aimed on reviewing treatment goals and targets and developing a sustainability plan. Although first, third, and fifth sessions were usually held at the participants home, participants could choose a different location if it was more convenient. Except for session 4 which lasted for about 5–10 minutes, all other sessions lasted for approximately 1 hour.
Table 1.
Core activities of Rafiki mwenye msaada across 5 sessions
| Session | Theme | Content and activities |
|---|---|---|
| 1 | Getting to know | (a) Introduction to the Rafiki mwenye msaada (b) Information regarding living with hypertension (c) Knowing about blood pressure (causes and effects) (d) Identifying personal strengths and weaknesses (e) Identifying social support including a “treatment supporter” |
| 2 | Understanding treatment and setting attainable goals | (a) Information about blood pressure medication (b) Developing strategies for optimizing clinic visits Setting short-, medium-, and long-term goals |
| 3 | Healthy habits | (a) Discussing healthy diet and identifying available food options (b) Practical information on physical activity (c) Identifying symptoms of stress and coping mechanisms |
| 4 | Recap | (a) Peer counselor call participant to revisit the importance of attending a clinic, taking medications, and healthy lifestyles (b) Scheduling the last session |
| 5 | Long-term care engagement | (a) Reviewing personal goals (b) Addressing remained gaps (c) Setting a sustainability plan to remain in hypertension care |
Study outcomes
The primary study outcome was 1-year cumulative rate of hospitalization and/or death. Follow-up phone calls were made to assess vitality status and hospitalizations among participants. If the participant was not available by phone, the alternative contact was called to determine the participant’s health status. If a hospitalization or death had occurred, exact dates were determined whenever possible. If the exact date could not be determined, the date of the event was assumed to be halfway between the current date and the last phone call. We have used this same methodology in many other studies in Tanzania.17–19
Secondary outcomes were use of anti-hypertensive medicine (defined as taking pills in the past 2 weeks) and clinic attendance (defined as at least 1 visit in the prior 3 months). In the intervention cohort we also assessed adherence of hypertensive medication by using 3 questions that we have previously adapted, translated, and validated from the Hill Bone questionnaire.6,20 Participants were given 1 point for each answer, for a possible total adherence score of 3. Good adherence was defined as a score of 3/3.
Analysis
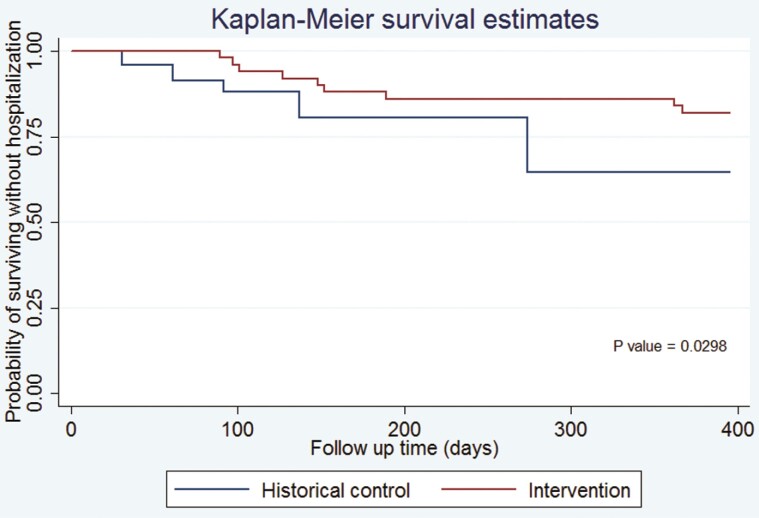
Data were double entered and managed on REDCap database hosted at Weill Cornell Medicine.21,22 Analysis was conducted in Stata (14.2, StataCorp LLC, College Station, TX). Baseline demographic and clinical characteristics were summarized by median and interquartile range for continuous variables and frequency and percentage for categorical variables. Data were compared using the chi-square/fisher’s test or Student t test, as appropriate. Cox regression analysis was used to calculate hazard ratios between the 2 cohorts. We used a time-dependent covariate to test the assumption of proportional hazards. For the comparison of hospital admissions between the 2 cohorts, we used the Fine-Grey approach to adjust for the competing risk of death. A 2-sided P value of less than 0.05 was regarded as statistically significant. Kaplan-Meier curves were used to display outcomes stratified by the study cohort (Figure 1). Additional analyses were conducted to compare patients’ outcomes between the 2 intervention sites.
Figure 1.
Kaplan-Meier estimates for survival without hospitalization and/or death in patients with hypertensive urgency in the intervention versus historical control cohorts.
RESULTS
Study enrollment and baseline characteristics
Intervention cohort.
We screened 103 patients with hypertensive urgency between August and December 2020, 50 were enrolled in the intervention cohort. Among 53 patients who were not enrolled, 41 lived outside Mwanza city, 11 did not consent, and 1 did not have a mobile phone.
In comparison to the historical control cohort, the intervention cohort had a significantly lower educational attainment and less health insurance. Baseline characteristics of both the historical control and intervention cohort are described in Table 2.
Table 2.
Background characteristics of the participants in the intervention and historical control cohorts
| Intervention cohort (N = 50) | Historical control cohort (N = 150) | P-valuea | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Demographics | |||||
| Age (median, IQR) | 61 (50–70) | 62 (54–68) | 0.475 | ||
| Gender | |||||
| Female | 34 | 68 | 101 | 67 | 0.931 |
| Education | |||||
| None/some primary school | 15 | 30 | 30 | 20 | 0.040 |
| Primary school | 24 | 48 | 67 | 45 | |
| Secondary school | 10 | 20 | 30 | 20 | |
| University | 1 | 2 | 23 | 15 | |
| Health insurance status | |||||
| Have insurance | 20 | 40 | 130 | 87 | <0.001 |
| Clinical | |||||
| Systolic blood pressure (mm Hg) | 189 (183–203) | 196 (185–210) | 0.313 | ||
| eGFRb | |||||
| ≤60 (mL/min/1.73 m2) | 7 | 14 | 39 | 26 | 0.081 |
| BMIc (Kg/m2) | |||||
| Normal weight (18.5–24.9) | 15 | 30 | 31 | 21 | 0.184 |
| Overweight (25–30) | 19 | 38 | 50 | 33 | |
| Obese (≥30) | 16 | 32 | 69 | 46 | |
aChi-square test (or Fisher’s exact test for cells with <5 observations).
beGFR—estimated glomerular filtration rate.
cBMI—body mass index.
Intervention, follow-up, and outcomes.
Of the 50 patients enrolled in the intervention cohort, 45 (90%) completed all 5 sessions. Four participants did not complete sessions due to travel outside the study area during the intervention period. Only 1 participant died before completing the 5 sessions.
The 1-year cumulative incidence of death and hospital admission were 8% (4/50) and 16% (8/50), respectively, compared to 9% (13/150) and 34% (51/150), respectively in the historical controls. Combined rates of hospitalization and/or death were 18% (9/50) in the intervention cohort vs. 35% (53/150) in the historical controls (Hazard Ratio [HR], 0.48, 95% CI 0.24–0.97; P = 0.041). Adjusting for differences in attained education level and health insurance status, the hazards of hospitalization and/or death was 61% lower in the intervention cohort compared to the historical cohort (adjusted HR, 0.39, 95% CI 0.18–0.85; P = 0.018) (Table 3). The assumption of proportional hazards was met in all models as the effect of the covariate*time interaction was not statistically significant.
Table 3.
Comparison of outcomes between historical cohort and intervention
| Primary outcomes | ||||||
|---|---|---|---|---|---|---|
| Intervention group (N = 50) | Historical group (N = 150) | Crude analysis | Adjusted analysis | |||
| HR (95% CI) | P value | aHRa(95% CI) | P value | |||
| Cumulative rate of hospitalization and/or dead | 9 (18%) | 53 (35%) | 0.48 (0.24–0.97) | 0.041 | 0.39 (0.18–0.85) | 0.018 |
| Cumulative rate of hospitalization | 8 (16%) | 51 (34%) | 0.35 (0.14–0.87) | 0.024 b | 0.33 (0.13–0.83) | 0.018 b |
| Cumulative death | 4 (8%) | 13 (9%) | 0.95 (0.1–2.92) | 0.930 | 0.54 (0.16–1.81) | 0.316 |
| Secondary outcomes | ||||||
| Intervention group (N = 50) | Historical group (N = 150) | P-valuec | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| 3 months (intervention period) | ||||||
| Used blood pressure medicinee | 46 | 92 | 108 | 72 | 0.003 | |
| Clinic attendanced | 46 | 92 | 73 | 49 | <0.001 | |
| 6 months | ||||||
| Used blood pressure medicinee | 46 | 92 | 118 | 79 | 0.035 | |
| Clinic attendanced | 46 | 92 | 104 | 69 | 0.001 | |
| 12 months | ||||||
| Used blood pressure medicinee | 40 | 80 | 115 | 77 | 0.625 | |
| Clinic attendanced | 39 | 78 | 114 | 76 | 0.773 | |
aAdjusted for insurance status and education level.
bHazard ratios and P-values adjusted for death as a competing risk using the Fine-Grey approach.
cChi-square test (or Fisher’s exact test for cells with <5 observations).
dAt least once within the past 3 months.
eIn the past 2 weeks.
Compared with the historical control group, the intervention group was more likely to use medicine in the past 2 weeks and attend the outpatient clinic at least once within the past 3 months at 3- and 6-months of follow-up (Table 3). Good adherence to medication was observed in more than 90% of the intervention cohort at all follow-up time points (Table 4).
Table 4.
Medication adherence in the intervention cohort at 3, 6, and 12 months of follow-up among participants who remained alive and in follow-up
| Intervention cohort (N = 50) | ||
|---|---|---|
| n | % | |
| 3 months (intervention period) (n = 49, 1 dead) | ||
| Medication adherence score | ||
| Adherence score = 3 | 46 | 94 |
| Adherence score <3 | 3 | 6 |
| 6 months (n = 48, 2 dead) | ||
| Medication adherence score | ||
| Adherence score = 3 | 46 | 96 |
| Adherence score <3 | 2 | 4 |
| 12 months (n = 44, 4 dead)a | ||
| Medication adherence score | ||
| Adherence score = 3 | 40 | 91 |
| Adherence score <3 | 4 | 9 |
aTwo living participants missed adherence score.
The 1-year cumulative incidence of hospitalization and/or death at the 2 sites was not statistically different. Likewise, anti-hypertensive medicine use, clinic attendance, and adherence score were not significantly different, except at 12 months. However, we noted fewer hospitalization and/or death events among patients from site A, where the historical control cohort was conducted (Table 5).
Table 5.
Comparison of outcomes between study sites of the intervention cohort
| Site A (N = 24) | Site B (N = 26) | P-valuea | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| 1-year incident of hospitalization and/or death | 3 | 12 | 6 | 23 | 0.467 |
| 3 months (intervention period) | |||||
| Used medicineb | 22 | 92 | 24 | 92 | 1.000 |
| Clinic attendancec | 24 | 100 | 22 | 85 | 0.111 |
| Good adherenced | 23 | 96 | 23 | 88 | 0.611 |
| 6 months | |||||
| Used medicineb | 23 | 96 | 23 | 88 | 0.611 |
| Clinic attendancec | 23 | 96 | 23 | 96 | 0.611 |
| Good adherenced | 24 | 100 | 22 | 85 | 0.111 |
| 12 months | |||||
| Used medicineb | 23 | 96 | 17 | 65 | 0.007 |
| Clinic attendancec | 24 | 79 | 15 | 58 | <0.001 |
| Good adherenced | 24 | 100 | 16 | 62 | 0.001 |
aChi-square test (or Fisher’s exact test for cells with <5 observations).
bIn the past 2 weeks.
cAt least once within the past 3 months.
dAdherence score = 3.
DISCUSSION
This study sought to assess the association between a peer counselor intervention and the 1-year cumulative incidence of hospitalization and/or death among adult patients with hypertensive urgency in the Mwanza region in Tanzania. We found that patients in the intervention cohort at any time point during the study period were half as likely to be hospitalized and/or die than historical control cohort patients. The peer counselor intervention was also associated with greater use of anti-hypertensive medicine and outpatient clinic attendance at 3- and 6-months of follow-up and high rates of medication adherence up to 1 year. These findings suggest that a peer counselor intervention may improve health outcomes in people with hypertensive urgency.
This study preliminarily demonstrated the efficacy of peer counselors’ intervention in improving outcomes among patients with hypertensive urgency in a resource-limited setting. Case management interventions support the transformation of patients’ mentality from a passive recipient of health care towards an active role.23 Specifically, the use of peer counselors—patients with hypertension who have achieved pressure control—create a unique environment where patients with hypertensive urgency could learn through a lived experience of the peer on how to navigate barriers to good health outcomes. Furthermore, through the interactions with peer counselors, patients with hypertensive urgency are likely to be empowered. Previous studies23–25 have shown that empowered patients (i.e., when patients understand their condition and their role in the healthcare process and take self-initiated actions to benefit their health) are likely to have good adherence and better outcomes. As such, the use of peer counselors in the current study is novel in our setting, where the health care system has limited human resources.
In this study, we found that clinic attendance and medication use did not significantly differ between the 2 cohorts at the 12-month follow-up. Given that intervention sessions took place in the first 3 months, this observation suggests that the intervention effect might have worn off at 12 months and that additional follow-up intervention sessions might be needed. Literature26–30 has shown that booster sessions often help to maintain the gains of the intervention.
The present study raises the possibility that lessons learned from managing advanced HIV disease could be applied to developing and implementing interventions to improve outcomes for other chronic disease emergencies—such as hypertensive crises—in SSA.31 For adults living with HIV, clinical trials have demonstrated that case management interventions can increase clinic attendance and medication adherence.32 The ARTAS intervention is one such case management intervention with strong support from clinical trials in the United States.13,14 It is encouraging to observe that the present study, which adapted the ARTAS intervention, positively impacted outcomes in patients with hypertensive urgency.
In this study, near half (40%) of screened patients with hypertensive urgency were from out of the study region. This is an important issue for future intervention design. Individuals in low- and middle-income countries (LMICs) seem to frequently travel as they seek to obtain employment and receive high-quality medical care.12 Thus, prospective interventions should be designed to address challenges related to patients’ mobility. Given the grown access to mobile phones in LMICs,33–35 mHealth could be used to deliver interventions.
The results of this prospective cohort study must be interpreted in the context of its limitations. Although the intervention cohort was a pilot study, using the historical control group rather than a parallel control is a weak study design for determining intervention effects. Therefore, further study is necessary to define the efficacy of the peer counselor intervention. Additionally, we could not objectively establish the cause of hospitalization and/or death because most of these events occurred outside the study sites. We are aware that this information would strengthen the evidence of peer counselors’ intervention effectiveness. However, for all documented deaths in this study, the informant reported that the death was related to the diagnosis of hypertension.
In conclusion, the study provided preliminary data that case management intervention using peer counselors for adult patients with hypertensive urgency may be effective in reducing the 1-year cumulative rate of hospitalization and/or death and may improve medication use and clinic attendance. Further research should be conducted to assess the impact of the peer counselor intervention on a broader scale among adult patients with hypertensive urgency.
ACKNOWLEDGMENTS
We thank all of the participants for their willingness to participate in this study. We thank the peer counselors for their help in delivering the Rafiki mwenye msaada intervention. Also, we are grateful for the input of Saidi Kapiga, a scientific director at the Mwanza Intervention Trials Unit, throughout the process of writing this manuscript. Finally, the authors acknowledge Mayombo Daud for his contributions to data management and participant follow-up.
Contributor Information
Godfrey A Kisigo, Center for Global Health, Weill Cornell Medicine, New York, New York, USA; Department of Internal Medicine, Weill Bugando School of Medicine, Mwanza, Tanzania; Mwanza Intervention Trials Unit, National Institute for Medical Research, Mwanza, Tanzania.
Frank Mgeta, Department of Internal Medicine, Weill Bugando School of Medicine, Mwanza, Tanzania.
Onike Mcharo, Mwanza Intervention Trials Unit, National Institute for Medical Research, Mwanza, Tanzania.
Elialilia Okello, Mwanza Intervention Trials Unit, National Institute for Medical Research, Mwanza, Tanzania.
Bahati Wajanga, Department of Internal Medicine, Weill Bugando School of Medicine, Mwanza, Tanzania.
Fredrick Kalokola, Department of Internal Medicine, Weill Bugando School of Medicine, Mwanza, Tanzania.
Graham Mtui, Department of Internal Medicine, Sekou Touré Referral Regional Hospital, Mwanza, Tanzania.
Radhika Sundararajan, Center for Global Health, Weill Cornell Medicine, New York, New York, USA; Department of Emergency Medicine, Weill Cornell Medicine, New York, New York, USA.
Robert N Peck, Center for Global Health, Weill Cornell Medicine, New York, New York, USA; Department of Internal Medicine, Weill Bugando School of Medicine, Mwanza, Tanzania; Mwanza Intervention Trials Unit, National Institute for Medical Research, Mwanza, Tanzania.
DISCLOSURE
The authors declare that they have no conflict of interest.
FUNDING
This study was funded through the Weill Cornell Medicine Diversity and Healthcare Disparity Grant. G.A.K. was supported by the Fogarty International Center and the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (D43 TW009337). R.N.P. was supported by the grant from the National Institutes of Health (R01 HL160332). R.S. was supported by a grant from the National Institutes of Health (K23 MH111409). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Furthermore, the funding bodies had no role in the collection, analysis, and interpretation of data and in writing the manuscript.
AUTHORS’ CONTRIBUTIONS
G.A.K.: study design, investigation, formal analysis, and original draft preparation, F.M., O.M.: investigation and review & editing, BW: review & editing, E.O., G.M., F.K., R.S., and R.N.P.: study design, supervision, and review & editing. All authors read and approved the final manuscript.
CONSENT TO PARTICIPATE
All study participants provided written informed consent.
CONSENT FOR PUBLICATION
Not applicable.
DATA AVAILABILITY
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- 1. Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A, Delwiche K, Estep K, Frostad JJ, Kc A, Kyu HH, Moradi-Lakeh M, Ng M, Slepak EL, Thomas BA, Wagner J, Aasvang GM, Abbafati C, Ozgoren AA, Abd-Allah F, Abera SF, Aboyans V, Abraham B, Abraham JP, Abubakar I, Abu-Rmeileh NME, Aburto TC, Achoki T, Adelekan A, Adofo K, Adou AK, Adsuar JC, Afshin A, Agardh EE, Al Khabouri MJ, Al Lami FH, Alam SS, Alasfoor D, Albittar MI, Alegretti MA, Aleman AV, Alemu, Alfonso-CristanchoZA, AlhabibR, AliS, AliR, AllaMK, AllebeckF, AllenP, AlsharifPJ, AlvarezU, Alvis-GuzmanE, AmankwaaN, AmareAA, AmehAT, AmeliEA, AminiO, AmmarH, AndersonW, AntonioBO, AnwariCAT, CunninghamP, ArnlövSA, ArsenijevicJ, ArtamanVSA, AsgharA, AssadiRJ, AtkinsR, AtkinsonLS, AvilaC, AwuahMA, BadawiB, BahitA, BakfalouniMC, BalakrishnanT, BalallaK, BaluS, BanerjeeRK, BarberA, Barker-ColloRM, BarqueraSL, BarregardS, BarreroL, Barrientos-GutierrezLH, Basto-AbreuT, BasuAC, BasuA, BasulaimanS, RuvalcabaMO, BeardsleyCB, BediJ, BekeleN, BellT, BenjetML, BennettC, BenzianDA, BernabéH, BeyeneE, BhalaTJ, BhallaN, BhuttaA, BikbovZA, AbdulhakB, BloreAAB, BlythJD, BohenskyFM, BaşaraMA, BorgesBB, BornsteinG, BoseNM, BoufousD, BourneS, BraininRR, BrazinovaM, BreitbordeA, BrennerNJ, BriggsH, BrodayADM, BrooksDM, BrucePM, BrughaNG, BrunekreefTS, BuchbinderB, BuiR, BukhmanLN, BullochG, BurchAG, BurneyM, Campos-NonatoPGJ, CampuzanoIR, CantoralJC, CaravanosAJ, CárdenasJ, CardisR, CarpenterE, CasoDO, Castañeda-OrjuelaV, CastroCA, Catalá-LópezRE, CavalleriF, ÇavlinF, ChadhaA, ChangVK, CharlsonJ, ChenFJ, ChenH, ChenW, ChiangZ, Chimed-OchirPP, ChowdhuryO, ChristophiR, ChuangCA, ChughT-W, CirilloSS, ClaßenM, ColistroTK, ColomarV, ColquhounM, ContrerasSM, CooperAG, CooperriderC, CooperK, CoreshLT, CourvilleJ, CriquiKJ, Cuevas-NasuMH, Damsere-DerryL, DanawiJ, DandonaH, DandonaL, DarganR, DavisPI, DavitoiuA, DayamaDV, de CastroA, De la Cruz-GóngoraEF, De LeoV, de LimaD, DegenhardtG, del Pozo-CruzL, DellavalleB, DeribeRP, DerrettK, JarlaisS, DessalegnDCD, DeVeberM, DevriesGA, DharmaratneKM, DheraniSD, DickerMK, DingD, DokovaEL, DorseyK, DriscollER, DuanTR, DurraniL, EbelAM, EllenbogenBE, ElshrekRG, EndresYM, ErmakovM, ErskineSP, EshratiHE, EsteghamatiB, FahimiA, FaraonS, FarzadfarEJA, FayF, FeiginDFJ, FeiglVL, FereshtehnejadAB, FerrariS-M, FerriAJ, FlaxmanCP, FlemingAD, FoigtTD, ForemanN, PaleoKJ, FranklinUF, GabbeRC, GaffikinB, GakidouL, GamkrelidzeE, GankpéA, GansevoortFG, García-GuerraRT, GasanaFA, GeleijnseE, GessnerJM, GethingBD, GibneyP, GillumKB, GinawiRF, GiroudIAM, GiussaniM, GoenkaG, GoginashviliS, DantesK, GonaHG, de CosioP, González-CastellTG, GotayD, GotoCC, GoudaA, GuerrantHN, GugnaniRL, GuilleminHC, GunnellF, GuptaD, GuptaR, GutiérrezR, Hafezi-NejadRA, HaganN, HagstromerH, HalasaM, HamadehYA, HammamiRR, HankeyM, HaoGJ, HarbY, HareguHL, HaroTN, HavmoellerJM, HayR, HedayatiSI, Heredia-PiMT, HernandezIB, HeutonL, HeydarpourKR, HijarP, HoekM, HoffmanHW, HornbergerHJ, HosgoodJC, HoyHD, HsairiDG, HuM, HuG, HuangH, HuangC, HubbellJJ, HuiartBJ, HusseiniL, IannaroneA, IburgML, IdrisovKM, IkedaBT, InnosN, InoueK, IslamiM, IsmayilovaF, JacobsenS, JansenKH, JarvisHA, JassalDL, JaureguiSK, JayaramanA, JeemonS, JensenP, JhaPN, JiangV, JiangF, JiangG, JonasY, JuelJB, KanK, RoselineH, KaramSSK, KarchNE, KaremaA, KarthikeyanCK, KaulG, KawakamiA, KaziN, KempDS, KengneAH, KerenAP, KhaderA, KhalifaYS, KhanSEAH, KhangEA, KhatibzadehY-H, KhonelidzeS, KielingI, KimC, KimD, KimS, KimokotiY, KinfuRW, KingeY, KisselaJM, KivipeltoBM, KnibbsM, KnudsenLD, KokuboAK, KoseY, KosenMR, KraemerS, KravchenkoA, KrishnaswamiM, KromhoutS, KuH, DefoT, BicerBK, KuipersBK, KulkarniEJ, KulkarniC, KumarVS, KwanGA, LaiGF, BalajiT, LallooAL, LallukkaR, LamT, LanH, LansinghQ, LarsonVC, LarssonHJ, LaryeaA, LavadosDO, LawrynowiczPM, LeasherAE, LeeJL, LeighJ-T, LeungJ, LeviR, LiM, LiY, LiangY, LiangJ, LimX, LindsaySS, LipshultzMP, LiuSE, LiuS, LloydY, LogroscinoBK, LondonG, LopezSJ, Lortet-TieulentN, LotufoJ, LozanoPA, LuneviciusR, MaR, MaJ, MachadoS, MacIntyreVMP, Magis-RodriguezMF, MahdiC, MajdanAA, MalekzadehM, MangalamR, MapomaS, MarapeCC, MarcenesM, MargolisW, MargonoDJ, MarksC, MartinGB, MarzanRV, MashalMB, MasiyeMT, Mason-JonesF, MatsushitaAJ, MatzopoulosK, MayosiR, MazorodzeBM, McKayTT, McKeeAC, McLainM, MeaneyA, MedinaPA, MehndirattaC, Mejia-RodriguezMM, MekonnenF, MelakuW, MeltzerYA, MemishM, MendozaZA, MensahW, MeretojaGA, MhimbiraA, MichaFA, MillerR, MillsTR, MisganawEJ, MishraA, IbrahimS, MohammadNM, MokdadKA, MolaAH, MonastaGL, HernandezL, MonticoJCM, MooreM, MorawskaAR, MoriL, MoschandreasR, MoturiJ, MozaffarianWN, MuellerD, MukaigawaraUO, MullanyM, MurthyEC, NaghaviKS, NahasM, NaheedZ, NaidooA, NaldiKS, NandL, NangiaD, NarayanV, NashKV, NealD, NejjariB, NeupaneC, NewtonSP, NgalesoniCR, de Dieu NgirabegaFN, NguyenJ, NguyenG, NieuwenhuijsenNT, NisarMJ, NogueiraMI, NollaJR, NolteJM, NorheimS, NormanOF, NorrvingRE, NyakarahukaB, OhL, OhkuboI-H, OlusanyaT, OmerBO, OpioSB, OrozcoJN, PagcatipunanR, PainRS, PandianAW, PaneloJD, PapachristouCIA, ParkC, ParryE-K, CaicedoCD, PattenAJP, PaulSB, PavlinVK, PearceBI, PedrazaN, PedrozaLS, StokicA, PekericliLP, PereiraA, Perez-PadillaDM, Perez-RuizR, PericoF, PerryN, PervaizSAL, PesudovsA, PetersonK, PetzoldCB, PhillipsM, PhuaMR, PlassHP, PoenaruD, PolanczykD, PolinderGV, PondS, PopeCD, PopeCA, PopovaD, PourmalekS, PowlesF, PrabhakaranJ, PrasadD, QatoNM, QuezadaDM, QuistbergAD, RacapéDAA, RafayL, RahimiA, Rahimi-MovagharK, RahmanV, RajuSU, RakovacM, RanaI, RaoSM, RazaviM, ReddyH, RefaatKS, RehmAH, RemuzziJ, RibeiroG, RiccioAL, RichardsonPM, RiedererL, RobinsonA, RocaM, RodriguezA, Rojas-RuedaA, RomieuD, RonfaniI, RoomL, RoyR, RuhagoN, RushtonGM, SabinL, SaccoN, SahaRL, SahathevanS, SahraianR, SalomonMA, SalvoJA, SampsonD, SanabriaUK, SanchezJR, Sánchez-PimientaLM, Sanchez-RieraTG, SandarL, SantosL, SapkotaIS, SatpathyA, SaundersM, SawhneyJE, SaylanM, ScarboroughMI, SchmidtP, SchneiderJC, SchöttkerIJC, SchwebelB, ScottDC, SeedatJG, SepanlouS, SerdarSG, Servan-MoriB, ShaddickEE, ShahrazG, LevyS, ShangguanTS, SheS, SheikhbahaeiJ, ShibuyaS, ShinK, ShinoharaHH, ShiriY, ShishaniR, ShiueK, SigfusdottirI, SilberbergID, SimardDH, SindiEP, SinghS, SinghA, SinghGM, SkirbekkJA, SliwaV, SoljakK, SonejiM, SøreideS, SoshnikovK, SposatoS, SreeramareddyLA, StapelbergCT, StathopoulouNJC, StecklingV, SteinN, SteinDJ, StephensMB, StöcklN, StraifH, StroumpoulisK, SturuaK, SunguyaL, SwaminathanBF, SwaroopS, SykesM, TabbBL, TakahashiKM, TalongwaK, TandonRT, TanneN, TannerD, TavakkoliM, Te AoM, TeixeiraBJ, Téllez RojoCM, TerkawiMM, Texcalac-SangradorAS, ThackwayJL, ThomsonSV, Thorne-LymanB, ThriftAL, ThurstonAG, TillmannGD, TobollikT, TonelliM, TopouzisM, TowbinF, ToyoshimaJA, TraebertH, TranJ, TrasandeBX, TrilliniL, TrujilloM, DimbueneU, TsilimbarisZT, TuzcuM, UchenduEM, UkwajaUS, UzunKN, van de VijverSB, Van DingenenS, van GoolR, van OsCH, VarakinJ, VasankariYY, VasconcelosTJ, VavilalaAMN, VeermanMS, Velasquez-MelendezLJ, VenketasubramanianG, VijayakumarN, VillalpandoL, ViolanteS, VlassovFS, VollsetVV, WagnerSE, WallerGR, WallinSG, WanMT, WangX, WangH, WangJ, WangL, WangW, WarouwY, WattsTS, WeichenthalCH, WeiderpassS, WeintraubE, WerdeckerRG, WessellsA, WestermanKR, WhitefordR, WilkinsonHA, WilliamsJD, WilliamsHC, WoldeyohannesTN, WolfeSM, WongCDA, WoolfJQ, WrightAD, WurtzJL, XuB, YanG, YangLL, YanoG, YeY, YenesewP, YentürM, YipGK, YonemotoP, YoonN, YounisS-J, YounoussiMZ, YuZ, ZakiC, ZhaoME, ZhengY, ZhouY, ZhuM, ZhuJ, ZouS, ZuntX, LopezJR, VosAD, MurrayT, CJ.. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, Alexander L, Estep K, Hassen Abate K, Akinyemiju TF, Ali R, Alvis-Guzman N, Azzopardi P, Banerjee A, Bärnighausen T, Basu A, Bekele T, Bennett DA, Biadgilign S, Catalá-López F, Feigin VL, Fernandes JC, Fischer F, Gebru AA, Gona P, Gupta R, Hankey GJ, Jonas JB, Judd SE, Khang Y-H, Khosravi A, Kim YJ, Kimokoti RW, Kokubo Y, Kolte D, Lopez A, Lotufo PA, Malekzadeh R, Melaku YA, Mensah GA, Misganaw A, Mokdad AH, Moran AE, Nawaz H, Neal B, Ngalesoni FN, Ohkubo T, Pourmalek F, Rafay A, Rai RK, Rojas-Rueda D, Sampson UK, Santos IS, Sawhney M, Schutte AE, Sepanlou SG, Shifa GT, Shiue I, Tedla BA, Thrift AG, Tonelli M, Truelsen T, Tsilimparis N, Ukwaja KN, Uthman OA, Vasankari T, Venketasubramanian N, Vlassov VV, Vos T, Westerman R, Yan LL, Yano Y, Yonemoto N, Zaki MES, Murray CJL.. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA 2017; 317:165–182. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 3. WHO. WHO Health Statistik: Monitoring health for the SDGs, Sustainable Development Goal s. World Health Organization, Geneva, 2019. [Google Scholar]
- 4. Papadopoulos DP, Sanidas EA, Viniou NA, Gennimata V, Chantziara V, Barbetseas I, Makris TK.. Cardiovascular hypertensive emergencies. Curr Hypertens Rep 2015; 17:5. doi: 10.1007/s11906-014-0515-z. [DOI] [PubMed] [Google Scholar]
- 5. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT.. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Pr. J Am Coll Cardiol 2018; 71:e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 6. Reis KG, Wilson R, Kalokola F, Wajanga B, Lee MH, Safford M, Peck RN.. Hypertensive urgency in Tanzanian adults: a 1-year prospective study. Am J Hypertens 2020; 33:1087–1091. doi: 10.1093/ajh/hpaa129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paini A, Tarozzi L, Bertacchini F, Aggiusti C, Rosei CA, De Ciuceis C, Malerba P, Broggi A, Perani C, Salvetti M, Muiesan ML.. Cardiovascular prognosis in patients admitted to an emergency department with hypertensive emergencies and urgencies. J Hypertens 2021; 39:2514–2520. doi: 10.1097/HJH.0000000000002961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, Mac Laughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT.. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Pr. Hypertension 2018; 71:e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 9. Patel KK, Young L, Howell EH, Hu B, Rutecki G, Thomas G, Rothberg MB.. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting. JAMA Intern Med 2016; 176:981–988. doi: 10.1001/jamainternmed.2016.1509. [DOI] [PubMed] [Google Scholar]
- 10. Kumar N, Simek S, Garg N, Vaduganathan M, Kaiksow F, Stein JH, Fonarow GC, Pandey A, Bhatt DL.. Thirty-day readmissions after hospitalization for hypertensive emergency. Hypertension 2019; 73:60–67. doi: 10.1161/HYPERTENSIONAHA.118.11691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Paini A, Tarozzi L, Bertacchini F, Aggiusti C, Rosei CA, De Ciuceis C, Malerba P, Broggi A, Perani C, Salvetti M, Muiesan ML.. Cardiovascular prognosis in patients admitted to an emergency department with hypertensive emergencies and urgencies. J Hypertens 2021; 39:2514–2520. doi: 10.1097/HJH.0000000000002961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kisigo GA, Mcharo OC, Robert JL, Peck RN, Sundararajan R, Okello ES.. Understanding barriers and facilitators to clinic attendance and medication adherence among adults with hypertensive urgency in Tanzania. PLOS Glob Public Heal. 2022; 2(8):e0000919. doi: 10.1371/journal.pgph.0000919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kisigo GA, Issarow B, Abel K, Hashim R, Okello ES, Ayieko P, Lee MH, Grosskurth H, Fitzgerald D, Peck RN, Kapiga S.. A social worker intervention to reduce post-hospital mortality in HIV-infected adults in Tanzania (Daraja): study protocol for a randomized controlled trial. Contemp Clin Trials 2022; 113:106680. doi: 10.1016/j.cct.2022.106680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Craw J, Gardner L, Marks G, Rapp R, Bosshart J, Duffus W, Rossman A, Coughlin S, Gruber D, Safford L, Overton J, Schmitt K.. Brief strengths-based case management promotes entry into HIV medical care: results of the antiretroviral treatment access study-II. J Acquir Immune Defic Syndr 2008; 47:597–606. doi: 10.1097/QAI.0b013e3181684c51. [DOI] [PubMed] [Google Scholar]
- 15. Gardner LI, Metsch LR, Anderson-Mahoney P, Loughlin AM, del Rio C, Strathdee S, Sansom SL, Siegal HA, Greenberg AE, Holmberg SD.. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS 2005; 19:423–431. doi: 10.1097/01.aids.0000161772.51900.eb. [DOI] [PubMed] [Google Scholar]
- 16. Parry M, Watt-Watson J.. Peer support intervention trials for individuals with heart disease: a systematic review. Eur J Cardiovasc Nurs 2010; 9:57–67. doi: 10.1016/j.ejcnurse.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 17. Peck RN, Wang RJ, Mtui G, Smart L, Yango M, Elchaki R, Wajanga B, Downs JA, Mteta K, Fitzgerald DW.. Linkage to primary care and survival after hospital discharge for HIV-infected adults in Tanzania: a prospective cohort study. J Acquir Immune Defic Syndr 2016; 73:522–530. doi: 10.1097/QAI.000000000001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chen Y, Alphonce E, Mujuni E, Kisigo GA, Kingery JR, Makubi A, Peck R, Kalokola F.. Atrial fibrillation and mortality in outpatients with heart failure in Tanzania: a prospective cohort study. BMJ Open 2022; 12:e058200. doi: 10.1136/bmjopen-2021-058200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hau DK, Ambrose EE, Smart LR, Kayange NM, Peck RN.. Linkage to care intervention to improve post-hospital outcomes among children with sickle cell disease in Tanzania: a pilot study. J Pediatr. 2021; 232:290–293.e1. doi: 10.1016/j.jpeds.2021.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Maginga J, Guerrero M, Koh E, Holm Hansen C, Shedafa R, Kalokola F, Smart LR, Peck RN.. Hypertension control and its correlates among adults attending a hypertension clinic in Tanzania. J Clin Hypertens. 2016; 18:207–216. doi: 10.1111/jch.12646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN; REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019; 95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG.. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kuo CC, Lin CC, Tsai FM.. Effectiveness of empowerment-based self-management interventions on patients with chronic metabolic diseases: a systematic review and meta-analysis. Worldviews Evid Based Nurs 2014; 11:301–315. doi: 10.1111/wvn.12066. [DOI] [PubMed] [Google Scholar]
- 24. Simmons LA, Wolever RQ, Bechard EM, Snyderman R.. Patient engagement as a risk factor in personalized health care: a systematic review of the literature on chronic disease. Genome Med 2014; 6:16. doi: 10.1186/gm533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, Rhodes S, Shekelle P.. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med 2005; 143:427–438. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 26. Whisman MA. The efficacy of booster maintenance sessions in behavior therapy: review and methodological critique. Clin Psychol Rev 1990; 10:155–170. doi: 10.1016/0272-7358(90)90055-F. [DOI] [Google Scholar]
- 27. Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR.. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry 1999; 38:272–279. doi: 10.1097/00004583-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 28. Baggs K, Spence SH.. Effectiveness of booster sessions in the maintenance and enhancement of treatment gains following assertion training. J Consult Clin Psychol 1990; 58:845–854. doi: 10.1037/0022-006X.58.6.845. [DOI] [PubMed] [Google Scholar]
- 29. Metcalf CA, Malotte CK, Douglas JM, Paul SM, Dillon BA, Cross H, Brookes LC, DeAugustine N, Lindsey CA, Byers RH, Peterman TA, Efficacy of a booster counseling session 6 months after HIV testing and counseling: a randomized, controlled trial (RESPECT-2). Sex Transm Dis 2005; 32:123–129. doi: 10.1097/01.olq.0000151420.92624.c0. [DOI] [PubMed] [Google Scholar]
- 30. Vaterlaus JM, Allgood SM, Higginbotham BJ.. Stepfamily education booster sessions. Soc Work Groups 2012; 35:150–163. doi: 10.1080/01609513.2011.599017. [DOI] [Google Scholar]
- 31. Palma AM, Rabkin M, Nuwagaba-Biribonwoha H, Bongomin P, Lukhele N, Dlamini X, Kidane A, El-Sadr WM.. Can the success of HIV scale-up advance the global chronic NCD agenda? Glob Heart 2016; 11:403–408. doi: 10.1016/j.gheart.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Govindasamy D, Meghij J, Negussi EK, Baggaley RC, Ford N, Kranzer K.. Interventions to improve or facilitate linkage to or retention in pre-ART (HIV) care and initiation of ART in low- and middle-income settings - a systematic review. J Int AIDS Soc 2014; 17:19032. doi: 10.7448/IAS.17.1.19032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Aker JC, Mbiti IM.. Mobile phones and economic development in Africa. J Econ Perspect 2010; 24:207–232. doi: 10.1257/jep.24.3.207. [DOI] [Google Scholar]
- 34. Vasudevan L, Ostermann J, Moses SM, Ngadaya E, Mfinanga SG.. Patterns of mobile phone ownership and use among pregnant women in southern Tanzania: cross-sectional survey. JMIR mHealth uHealth 2020; 8:e17122. doi: 10.2196/17122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Doyle AM, Bandason T, Dauya E, McHugh G, Grundy C, Dringus S, Dziva Chikwari C, Ferrand RA.. Mobile phone access and implications for digital health interventions among adolescents and young adults in Zimbabwe: cross-sectional survey. JMIR mHealth uHealth 2021; 9:e21244. doi: 10.2196/21244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.