Abstract
Background
Cervical annular fissures (AFs) have not been studied specifically as to their prevalence, imaging features, and persistence over time. We sought to determine the prevalence and natural history of cervical AFs. We hypothesized that these are static lesions that are not prevalent in the population.
Methods
This was a cross-sectional retrospective study of cervical MRI examinations performed between 2011-2021. We retrospectively reviewed the studies of 115 consecutive patients (63 female, 52 male) who had 2 or more MRI studies of the cervical spine to identify (1) imaging features of cervical AFs on various pulse sequences, (2) the concurrence of disc bulges/herniations, (3) changes in those imaging findings over time (mean follow-up 39.3 months) and (4) rate at which cervical AFs were mentioned in radiology reports. 620 initial and follow-up studies were reviewed.
Results
50/115 (43.5%) patients had cervical AFs; 21 patients had a single AF and 29 patients had multi-level AFs (total 109 AFs). The most common levels affected were C4-C5 (28%, n = 31) and C5-C6 (27%, n = 30). All cervical AFs were hyperintense on T2WI and, over time, 95% (n = 104/109) of the AFs remained hyperintense; 22% (n = 25) showed less hyperintensity, 10% (n = 11) more hyperintensity, and 60% (n = 66) the same hyperintensity. 5 AFs (4%) resolved completely. Only 2 (8%) of 25 cervical AFs enhanced with gadolinium. The rate of concomitant disc bulges and herniations was 71% (n = 78) and 22% (n = 24) respectively. The presence of cervical AFs did not increase the risk of progression to bulges or herniations. None of the cervical AFs were mentioned in the radiology reports.
Conclusions
Cervical AFs occurred in 43.5% of patients but were rarely reported. They usually remained bright on T2W but their brightness could vary over time. Cervical AFs were often associated with disc bulges/herniations and enhanced less frequently (8%) than lumbar disk AFs.
Keywords: Cervical spine, Magnetic resonance imaging (MRI), Annular fissure, Intervertebral disc, Degenerative disc disease, Herniation, Bulge
Introduction
Degenerative disc disease is a common health condition, which affects individuals at a greater rate with increasing age. The intervertebral disc, effectively a fibrocartilage cushion between the vertebral bodies of the spine, is divided into a central nucleus pulposus and peripheral annulus fibrosus [1]. Annular fissures (AFs), previously termed annular tears, represent a structural failure of the annulus fibrosus at an early stage of intervertebral disc degeneration. AFs have been extensively studied in the lumbar spine [2,3] but have not been specifically addressed in the cervical spine by MRI.
One of the degenerative changes of the intervertebral disc is manifested on MRI by alteration of the signal intensity characteristics and morphologic features of both the nucleus pulposus and annular fibrosis of the intervertebral disc. While the nucleus loses T2 signal with degeneration as a result of dehydration or conversion of proteoglycans to more fibrous connective tissue, the annulus often shows high signal intensity zones (HIZ) in areas where a defect/fissuring has developed in these peripheral fibers.
Similar to back pain, the prevalence of neck pain has become more common in the cell phone and computer-based era where people are often looking down (or up) at their handheld or desktop screens [4]. The prevalence of cervical disc degeneration increases with age, and it affects more than 80% of people older than 60 years. These degenerative changes seen by MRI may be asymptomatic and/or may be difficult to correlate directly with neck pain. It is unclear whether the cervical AFs seen on MRI are related to acute events, gradual disc degeneration, or a physiological process caused by normal aging [5,6].
This study explores cervical spine AFs using a retrospective but longitudinal analysis of MR images. We hypothesized that cervical annular fissures are an uncommon finding and are static lesions, ie, have imaging findings that do not change over time.
Methods
Data selection
We evaluated the archives of our picture archiving and communication system (PACS) in the time interval between 2011 to 2021, to identify all patients who underwent multiple MRI scans of the cervical spine (with or without contrast). Patients with prior spinal surgery, spinal tumors, infection, fractures, or any other inflammatory diseases that may affect the disks were excluded. This retrospective study was approved by the institutional review board at our university. The study maintained patient privacy and was deemed HIPAA compliant. The electronic medical record was accessed as part of the IRB approval; patient data was acquired only from MRI reports and demographic data from headers.
MR imaging analysis
Three neuroradiologists assessed the MRI exams of the cervical spine and reached consensus about the imaging results of the cervical AFs. The cervical intervertebral disks were examined for the following characteristics: the existence of annular fissures, signal-intensity change over time, and the presence and variations of disk herniation. Additionally, at each level, the period between exams and the persistence or resolution of AFs were recorded. The intervertebral disks were evaluated using sagittal T1W, Short Tau Inversion Recovery (STIR), and T2W images. Fast spin echo T2W sequences were also performed in an axial plane. If contrast enhanced studies were included, the sagittal and axial postgadolinium (0.1 mmol/kg) T1W studies were reviewed for enhancement of the annulus (n = 29 studies). All MRI scans were conducted using Siemens 3T scanners. Sagittal spin-echo T2W MR imaging (repetition time [TR]/shortest of echo time [TE] = 3500/103 ms, T1W MR imaging (TR/TE = 2000/9 ms), and sagittal STIR imaging (TR/TE = 2800/45 ms) were used in all studies. All of these imaging techniques had the same parameters (277 mm × 250 mm of field of view [FOV], 320 × 320 of matrix, 4 mm of slice thickness, 0.4 mm of gap). Contrast-enhanced T1W MR images were acquired using the same settings as noncontrast T1W MR images after intravenous gadolinium (0.1 mmol/kg, Gadavist) administration.
Any T2 hyperintense signal intensity of the posterior peripheral annulus or contrast enhancement in the posterior annulus of a disk was characterized as an AF. As specified by lumbar disk nomenclature: version 2, a disk protrusion was characterized as a focal expansion of the disk material whereas bulges were more diffuse and/or affected greater than 90 degrees of the circumference of the disk [7].
Statistical analysis
The independent sample t-test and the paired t-test were used to assess continuous data across time. Continuous data were reported as mean and standard deviation (SD). If the variances were not normally distributed, the Mann-Whitney U test was applied. A chi-squared test was run on the categorized variables. SPSS for Windows version 28.0 was used to analyze all of the data (SPSS Inc, Chicago, IL). A 2-tailed p value of 0.05 was judged statistically significant.
Results
One hundred and fifteen (115) consecutive patients (63 female, 52 male) were identified with multiple cervical spine MR studies during the 2011 to 2021 period of inquiry and comprise the study population: 620 current and follow-up studies were reviewed on these 115 patients. The mean follow-up period was 39.3 months (39.4 SD). For the 115 patients, neck pain was the most common indication for performing the cervical MRI, accounting for 44 of 115 (38.3%) of the cases. Radiculopathy was identified as the reason for the study in 25/115 (21.7%) of the cases. Symptoms associated with cervical stenosis, such as pain, weakness, and numbness, ranked next in frequency, accounting for 14 of 115 (12.2%) of the cases. Less than 10% of the patients (n = 11) complained of shoulder pain, deltoid muscle weakness, myelopathy, leg paresthesias, abnormal posture and incoordination. There were single cases of trauma, meningioma, vascular malformation, Sprengel deformity, and myelitis.
Fifty (50/115 = 43.5%) patients had cervical AFs; 21/50 (42%) had a single cervical AF and 29/50 (58%) patients had multi-level AFs (total 109 cervical AFs) as seen in Table 1.
Table 1.
Number of cervical levels affected with annular fissures.
| Number of AF levels | Patient number [total: 50 patients, (109 AFs)] |
|---|---|
| 1 level | 21 patients, 21 AFs |
| 2 levels | 10 patients, 20 AFS |
| 3 levels | 11 patients, 33 AFs |
| 4 levels | 5 patients, 20 AFs |
| 5 levels | 3 patients, 15 AFs |
| TOTAL | 50 patients, 109 AFs |
Abbreviation: AF = annular fissure.
The imaging features of the 109 cervical AFs are seen in Table 2.
Table 2.
Imaging characteristics of cervical annular fissures.
| Imaging feature of AF | Frequency | Total | Rate % |
|---|---|---|---|
| T2 Bright | 109 | 109 | 100 |
| T2 Signal remain Bright over time | 104 | 109 | 95.4 |
| T2 Signal Increase over time (Brighter) | 11 | 109 | 10.1 |
| T2 Signal Decrease over time (less Bright) | 25 | 109 | 22.9 |
| T2 no change over time | 66 | 109 | 60.6 |
| T2 Signal Normalized over time | 5 | 109 | 4.6 |
| Gadolinium Enhancement | 2 | 25 | 8.0 |
| Gadolinium Enhancement no change over time | 23 | 25 | 92.0 |
| Concomitant Disc Bulge | 78 | 109 | 71.6 |
| Concomitant Disc Herniation | 24 | 109 | 22.0 |
| Concomitant Disc Bulge or Herniation: increased in size over time | 13 | 102 | 12.7 |
| Concomitant Disc Bulge or Herniation: decrease in size over time | 10 | 102 | 9.8 |
| Concomitant Disc Bulge or Herniation: No change over time | 83 | 102 | 81.4 |
| Develop New herniation over time | 2 | 50 | 4.0 |
| Develop New bulge over time | 1 | 50 | 2.0 |
| Decrease in AF size over time | 15 | 109 | 13.8 |
| Increase in AF size over time | 11 | 109 | 10.1 |
| Normalized AF over time (went away) | 7 | 109 | 6.4 |
The level of the cervical AFs is depicted in Table 3: the most common levels affected were C4 to C5 (28%, n = 31) and C5 to C6 (27%, n = 30).
Table 3.
Number of annular fissures at each level of the cervical spine.
| Annular fissure level | Frequency | Rate % |
|---|---|---|
| C2-C3 Level | 2 | 1.8% |
| C3-C4 Level | 12 | 11.0% |
| C4-C5 Level | 31 | 28.4% |
| C5-C6 Level | 30 | 27.5% |
| C6-C7 Level | 27 | 24.8% |
| C7-T1 Level | 7 | 6.4% |
| TOTAL | 109 | 100% |
Over time, 95% (n = 104/109) of the AFs remained bright on T2WI, but showed less hyperintensity in 22% (n = 25) (Fig. 1), more hyperintensity in 10% (n = 11) or the same hyperintensity 60% (n = 66) on follow-up (Fig. 2). The remaining 5 AFs (4%) resolved completely (Fig. 3). Twenty-five cervical AFs had gadolinium enhanced evaluations, 84 were only evaluated with un enhanced studies. Only 2 (8%) of these 25 cervical AFs enhanced with gadolinium (Fig. 4). There were no instances where an annular fissure enhanced but was not bright on T2W. One of the 2 cases of enhancing cervical AF had a follow-up study with enhanced sequences. This 1 cervical AF continued to enhance.
Figure 1.
Hyperintensity on T2W of annular fissures at initial and follow-up imaging. Initial (A) Sagittal T2W TSE and Sagittal STIR images (left to right) showing central disc protrusion at levels C4-C5, C5-C6, and C6-C7 (long and short arrows) associated with posterior annular fissures at the levels C4-C5, C5-C6 (long arrow) and C6-C7 (short arrow) that appears hyperintense on T2W and STIR; (B) Follow-up of the same patient 1984 days later shown in (A) reveals unchanged multilevel central disc protrusion, reduced AF's signal intensity on T2W images with no discernible annular fissures at C4-C5 and C5-C6 (long arrow), and unchanged C6-C7 T2W hyperintense annular fissure (short arrow).
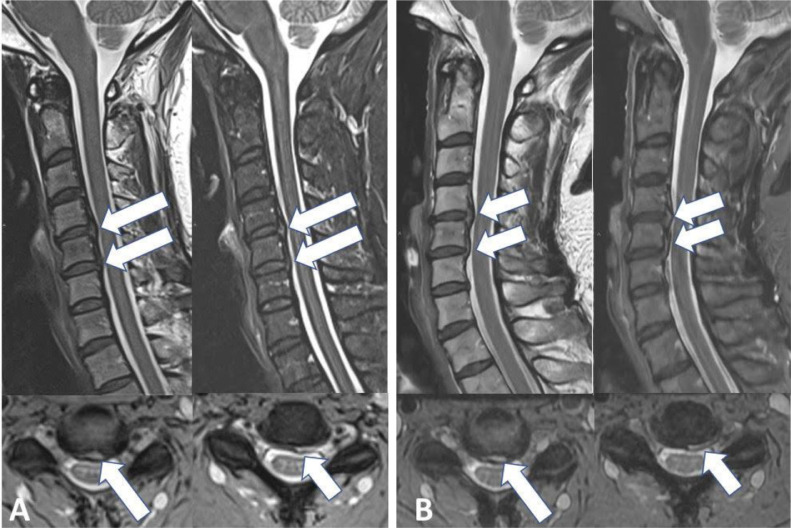
Figure 2.
Unchanged annular fissures and disc protrusions over 252 days. Initial (A) Sagittal T2W TSE (left), Sagittal STIR (right) and Axial spoiled T2* (multiple-echo recombined gradient echo-MERGE) images (bottom) show disc protrusions associated with abnormal focal hyperintensity on T2W, STIR and MERGE images in the posterior margin of the C4-C5 and C5-C6 discs, consistent with annular fissures. (B) Follow-up imaging, Sagittal T2W TSE (left), Sagittal STIR (right) and MERGE (bottom) images reveal unchanged discs protrusions and abnormal focal hyperintensity on T2 related to annular fissures.
Figure 3.
Interval decreased size and hyperintensity on T2W related to annular fissure on follow-up imaging. Initial (A) Sagittal T2W TSE and Sagittal STIR images reveal central disc protrusion associated with posterior T2W hyperintense annular fissure at the level C4-C5 (long arrow). (B) Follow-up imaging performed 235 days later, Sagittal T2W TSE and Sagittal STIR images show slight reduced disc protrusion, as well as decreased signal intensity on T2W of previously seen hyperintense annular fissure at C4-C5, although the fissure remains bright. Additional small disc protrusion at the level C5-C6 (short arrow) on initial images (A) and interval appearance of subtle T2W hyperintense annular fissure on the follow-up imaging (B), better characterized on Sagittal STIR sequence (short arrow).
Figure 4.
Interval decreased size and hyperintensity on T2W with preserved contrast enhancement related to annular fissure on follow-up imaging. Initial (A) Sagittal T2W and Axial T2W GRE and Sagittal and axial T1W with Gad images reveal paracentral disc herniation associated with posterior T2W hyperintense annular fissure with contrast enhancement at the level C4-C5 (arrow). (B) Follow-up imaging performed 655 days later, Sagittal, and axial T2W and Sagittal and axial T1W post contrast images show slight reduced disc herniation, as well as decreased signal intensity on T2W of previously seen hyperintense annular fissure at C4-C5, post gadolinium images show same contrast enhancement.
The rate of concomitant disc bulges and herniations was 71% (n = 78) and 22% (n = 24), respectively. The concomitant disc bulge or herniation increased in size over time in 13 of 102 cases (12.7%) and in 10 of 102 cases (9.8%) decreased in size over time. On follow-up studies of the cervical AFs, 1 new disc bulge and 2 herniations developed over time. The presence of cervical AFs did not increase progression to disc bulges or herniations. None of the cervical AFs were mentioned in the radiology reports.
Discussion
Neck pain is a common complaint and often requires the expense of imaging and treatment. Fajer et al. performed a systematic review of the prevalence of neck pain and showed the 1 year and lifetime mean prevalence of neck pain among the adult population as 37.2%, and 48.5%, respectively [7]. However, cervical intervertebral disc degeneration is commonly seen on cervical MRI even in the absence of neck pain [6,8].
Loss of integrity of annular fibers or detachment of annular fibers from their attachment to the vertebral endplate defines the annular fissure. These are then classified into various forms such as radial, transverse and concentric fissures based on their orientation [9]. According to histopathological examinations, 2 factors contribute to discogenic pain; annular fissures and nerve ingrowth [10]. The pathogenesis begins with an increase in pro-inflammatory cytokine within the annular fissure. As nerve fibers grow into the granulation tissue, they become sensitized, which culminates in discogenic pain [11,12].
In the Lumbar disc nomenclature version 2.0, recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology, and the American Society of Neuroradiology the term “annular tear” is replaced by the term “annular fissure” because the term “tear” can be misunderstood to imply a traumatic injury [9].
In 2009 Sharma et al. performed a longitudinal study of lumbar annular fissures and disc degeneration and demonstrated that annular fissures occur in the early stage of disc degeneration and the presence of these annular fissures accelerate disc degeneration [13]. This study was performed on symptomatic patients with back pain and did not compare findings with asymptomatic healthy control subjects. Years later Nadja et al. [14] in a control study demonstrated a similar rate of lumbar disc degeneration progression between those with annular fissures and those without annular fissures concluding that annular fissures do not predict the rate of disc degeneration.
Slipman et al.[15] showed no correlation between the annular fissure location and location of concordant pain elicited on provocative lumbar discography. In 2000, Carragee et al., [16] in a prospective observational study demonstrated the presence of lumbar annular fissure in 59% of the symptomatic population and 24% in the asymptomatic group. Others however, reported that the rate of AF was higher in asymptomatic patients [17], [18], [19], [20].
Although many studies have reported on the prevalence and clinical significance of lumbar annular fissures, few studies have been performed on the cervical spine. [21]. Ernst et al. performed a prospective study of cervical annular fissures in 30 asymptomatic patients and revealed the prevalence was 37%, and 94% of those AFs showed enhancement. The most common site for cervical AFs (50%) was the C5-6 level. The prevalence of cervical AFs increased by age (2) up to age 61 years and older in whom the prevalence was 33%. Our data differed from Ernst in that we saw a much lower rate of enhancement (8%) and slightly higher overall prevalence (43.5%). The most common level that we found was C4-C5 (n = 31) but the C5-C6 (n = 30) and C6-7 levels (n = 27) were close behind.
Siivola et al. conducted a longitudinal study of neck and shoulder pain with cervical MRI findings. They found that the prevalence of AF in the asymptomatic group was higher (66%) than the recurrent or persistent symptomatic group (50%) [20]. This parallels the aforementioned study by Wang et al demonstrating that there was no correlation between lumbar AF and pain response in lumbar discography [22] suggesting that the mere presence of an AF was not a reliable marker of discogenic pain [16]. Kong et al looked at 381 patients with cervical degenerative disease and noted that the odds ratio of having severe neck pain when one had a cervical annular fissure was 1.58 [23]. When all degenerative factors were analyzed in multivariate analysis annular fissures had an even higher odds ratio of 1.75, but below that of spondylolisthesis (2.89) and kyphotic curvature (2.62). The correlation of annular fissures and persistent neck pain in multivariate analysis was not significant [23].
We found that cervical spine annular fissures were always bright on T2W sequences and remained bright in all but 4% of cases. This finding is in keeping with the previous literature describing lumbar disk annular fissures where they have been reported to be T2 hyperintense in 96% of cases and persistently bright on T2W in 88% of cases [24]. As opposed to lumbar AFs where the rate of enhancement has been reported to be 100% [24], only 8% of our cervical AFs showed enhancement. All enhancing cervical AFs were bright on T2W. Lumbar spine AFs are said to resolve their enhancement in less than 30% of cases. We only had follow-up on one of the 2 cervical AFs that enhanced and it continued to enhance.
We used the T2W sequence to detect cervical AFs, but Stadnik et al noted that lumbar AFs enhanced in 27 of 28 (96%) AFs on contrast enhanced T1 images whereas they were seen in only 21 of 28 (75%) on T2 sequence images [3]. Similarly, Ross et al, in the study of 18 AFs (12 lumbar and 6 cervical) found only 4 of 12 enhancing lumbar AFs (33%) and 1 of 6 enhancing cervical AFs showed hyperintensity signals on T2 images [25]. We found the opposite. All cervical AFs were bright on T2W whether they enhanced or not.
What is the clinical significance of cervical annular fissures? We know from the CT discography literature that patients who have AFs have a higher rate of neck pain, but whether that is due to the AF or not is hard to prove even with provocative maneuvers on discography. Similarly, the literature is inconclusive as to whether the rate of cervical AFs is higher in patients with neck pain than those without [2,21,22,26]. A cause and effect relationship has not been established. Besides analgesics and nonsteroidal anti-inflammatory drugs, more aggressive interventions in patients with AFs alone have not been contemplated. For that reason, we sought to determine whether cervical AFs were a harbinger of disk bulges and/or herniations. The coincidence of such disk disease with AFs was found to be 71% for disk bulges and 22% for disk herniations. We found that 6% (3 patients) with a cervical AF developed a new disk bulge or herniation after the AF was discovered on follow up exams. Again, no cause and effect relationship are so implied.
This study has several limitations. This was a blinded study and we did not review the EMR for patients’ change in symptoms. The purpose of this manuscript, as stated in our introduction was to assess cervical spine annular fissures using a retrospective but longitudinal analysis of MR images. Note that we did not wish to access the clinical symptoms associated with annular fissures and our hypotheses were that cervical annular fissures are an uncommon finding and are static lesions. With regard to these hypotheses, we have demonstrated that cervical AFs occur in 43.5% of the population and that they remained at the same level of hyperintensity on T2W in 60% with only 4% resolving. We would like to address this issue regarding why correlating cervical AFs with clinical symptomatology is highly problematic:
-
1.
Based on the purpose of the study, looking at the evolution of AFs, our institutional IRB gave approval to review images and reports in the PACS, not to serially access the electronic medical record to explore patient symptomatology over time.
-
2.
The study was a retrospective study so we could not inquire about the patient's complaints at the time of the examination and some studies were several years old.
-
3.
Assigning symptoms to AFs when the literature is not definitive as to the significance of AFs as a source of pain (see discussion above) would be misleading.
-
4.
A total of 29 of 50 (58%) of patients had multiple AFs. Ascribing any increase, decrease or elimination of “neck pain” to a specific level of annular fissure whether one is enhancing or not, or enlarging or not, or bright or not would be illogical in this setting, i.e. we did not do discography to identify which was the symptomatic disk.
-
5.
To determine whether one's neck pain was due to a cervical annular fissures without reviewing any accompanying upper thoracic spine AFs would be suspect.
-
6.
Given the pain generators in the cervical spine of uncovertebral joint degeneration, facet degeneration, ligamentous strains, disk herniations, osteophytes and muscular sources, it would be ludicrous to ascribe someone's neck pain to the annular fissure with so many potential confounders. As Kong et al state, “…the cause of (neck) pain cannot be definitely attributed to a specific pathology… (but is a) multifactorial condition..” [23]
Although this is the largest specific cohort of cervical AFs reported in the literature, more cases would increase the statistical power of our findings, particularly for those with gadolinium enhancement. We also did not look at the use of medications that may have affected the inflammation or enhancement of the disks (eg, steroids). This study is the largest yet reported on cervical AFs with long-term follow-up (mean 39.3 months) and was designed to provide the natural evolutional history of cervical disk AFs. The clinical implications remain to be discovered.
Conclusions
Cervical AFs are common, occurring in 43.5% of the subjects studied, but are rarely described in radiology reports. They usually remain bright on T2W but their brightness may vary with time. AFs in the cervical spine are often linked with disc bulges and/or herniations, and enhance much less frequently (8%) than lumbar disk AFs.
Statement of data access and integrity
The authors declare that they had full access to all of the data in this study and the authors take complete responsibility for the integrity of the data and the accuracy of the data analysis.
Author contributions
M.H., F.R., D.Y. : conception or design of the work; S.A., R.L., M.H., F.R., D.Y., G.G. : acquisition, analysis, or interpretation of data for the work; S.A., R.L., M.H., F.R., David Yousem, Gary Gong: drafting the work or revising it critically for important intellectual content; Shadi Asadollahi, Rodrigo Luna, Meisam Hoseinyazdi, Faranak Rafiee, David Yousem, Gary Gong: final approval of the version to be publisher; Shadi Asadollahi, Rodrigo Luna, Meisam Hoseinyazdi, Faranak Rafiee, David Yousem, Gary Gong: agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declarations of Competing Interests
The authors declare no conflict of interest. Unrelated, Dr. Yousem reports royalties from Elsevier, personal fees from Medicolegal consultant, speaking and consulting fees from MRIOnline.com, outside the submitted work.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: MH: Nothing to disclose. SA: Nothing to disclose. RL: Nothing to disclose. FR: Nothing to disclose. GG: Nothing to disclose. DMY: Nothing to disclose.
Funding: None.
References
- 1.Adams MA, Dolan P. Intervertebral disc degeneration: evidence for two distinct phenotypes. J Anat. 2012;221(6):497–506. doi: 10.1111/j.1469-7580.2012.01551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ernst CW, Stadnik TW, Peeters E, et al. Prevalence of annular tears and disc herniations on MR images of the cervical spine in symptom free volunteers. Eur J Radiol. 2005;55(3):409–414. doi: 10.1016/j.ejrad.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Stadnik TW, Lee RR, Coen HL, et al. Annular tears and disk herniation: prevalence and contrast enhancement on MR images in the absence of low back pain or sciatica. Radiology. 1998;206(1):49–55. doi: 10.1148/radiology.206.1.9423651. [DOI] [PubMed] [Google Scholar]
- 4.Blumenberg C, Wehrmeister FC, Barros FC, et al. Association of the length of time using computers and mobile devices with low back, neck and mid-back pains: findings from a birth cohort. Public Health. 2021;195:1–6. doi: 10.1016/j.puhe.2021.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Son S, Lee SG, Park CW, et al. Combined open door laminoplasty with unilateral screw fixation for unstable multi-level cervical stenosis: a preliminary report. J Korean Neurosurg Soc. 2013;53(2):83–88. doi: 10.3340/jkns.2013.53.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee TH, Kim SJ, Lim SM. Prevalence of disc degeneration in asymptomatic korean subjects. Part 2: cervical spine. J Korean Neurosurg Soc. 2013;53(2):89–95. doi: 10.3340/jkns.2013.53.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15(6):834–848. doi: 10.1007/s00586-004-0864-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang ZX, Hu YG. Factors associated with lumbar disc high-intensity zone (HIZ) on T2-weighted magnetic resonance image: a retrospective study of 3185 discs in 637 patients. J Orthop Surg Res. 2018;13(1):307. doi: 10.1186/s13018-018-1010-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fardon DF, Williams AL, Dohring EJ, et al. Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014;14(11):2525–2545. doi: 10.1016/j.spinee.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 10.Stefanakis M, Al-Abbasi M, Harding I, et al. Annulus fissures are mechanically and chemically conducive to the ingrowth of nerves and blood vessels. Spine. 2012;37(22):1883–1891. doi: 10.1097/BRS.0b013e318263ba59. [DOI] [PubMed] [Google Scholar]
- 11.Lagerstrand K, Hebelka H, Brisby H. Identification of potentially painful disc fissures in magnetic resonance images using machine-learning modelling. Eur Spine J. 2022;31(8):1992–1999. doi: 10.1007/s00586-021-07066-x. [DOI] [PubMed] [Google Scholar]
- 12.Eldaya RW, Parsons MS, Orlowski HLP, et al. Evaluating the effect of a post-processing algorithm in detection of annular fissure on MR imaging. Eur Spine J. 2021;30(8):2150–2156. doi: 10.1007/s00586-021-06793-5. [DOI] [PubMed] [Google Scholar]
- 13.Sharma A, Pilgram T, Wippold FJ., 2nd. Association between annular tears and disk degeneration: a longitudinal study. AJNR Am J Neuroradiol. 2009;30(3):500–506. doi: 10.3174/ajnr.A1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farshad-Amacker NA, Hughes AP, Aichmair A, et al. Is an annular tear a predictor for accelerated disc degeneration? Eur Spine J. 2014;23(9):1825–1829. doi: 10.1007/s00586-014-3260-8. [DOI] [PubMed] [Google Scholar]
- 15.Slipman CW, Patel RK, Zhang L, et al. Side of symptomatic annular tear and site of low back pain: is there a correlation? Spine. 2001;26(8):E165–E169. doi: 10.1097/00007632-200104150-00026. [DOI] [PubMed] [Google Scholar]
- 16.Carragee EJ, Paragioudakis SJ, Khurana S. 2000 Volvo Award winner in clinical studies: Lumbar high-intensity zone and discography in subjects without low back problems. Spine. 2000;25(23):2987–2992. doi: 10.1097/00007632-200012010-00005. [DOI] [PubMed] [Google Scholar]
- 17.Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331(2):69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- 18.Weishaupt D, Zanetti M, Hodler J, et al. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209(3):661–666. doi: 10.1148/radiology.209.3.9844656. [DOI] [PubMed] [Google Scholar]
- 19.Modic MT, Ross JS, Obuchowski NA, et al. Contrast-enhanced MR imaging in acute lumbar radiculopathy: a pilot study of the natural history. Radiology. 1995;195(2):429–435. doi: 10.1148/radiology.195.2.7724762. [DOI] [PubMed] [Google Scholar]
- 20.Siivola SM, Levoska S, Tervonen O, et al. MRI changes of cervical spine in asymptomatic and symptomatic young adults. Eur Spine J. 2002;11(4):358–363. doi: 10.1007/s00586-001-0370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boden SD, McCowin PR, Davis DO, et al. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am Vol. 1990;72(8):1178–1184. [PubMed] [Google Scholar]
- 22.Wang HD, Hou SX, Wang XN, et al. [Correlation between high intensity zone on MRI and positive pain response on lumbar discography in the diagnosis of discogenic low back pain] Zhonghua Wai Ke Za Zhi. 2008;46(13):973–976. [PubMed] [Google Scholar]
- 23.Kong L, Tian W, Cao P, Wang H, Zhang B, Shen Y. Predictive factors associated with neck pain in patients with cervical disc degeneration: a cross-sectional study focusing on Modic changes. Medicine. 2017;96(43):e8447. doi: 10.1097/MD.0000000000008447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Munter FM, Wasserman BA, Wu HM, et al. Serial MR imaging of annular tears in lumbar intervertebral disks. AJNR Am J Neuroradiol. 2002;23(7):1105–1109. [PMC free article] [PubMed] [Google Scholar]
- 25.Ross JS, Modic MT, Masaryk TJ. Tears of the anulus fibrosus: assessment with Gd-DTPA-enhanced MR imaging. AJNR Am J Neuroradiol. 1989;10(6):1251–1254. [PMC free article] [PubMed] [Google Scholar]
- 26.Schellhas KP, Smith MD, Gundry CR, et al. Cervical discogenic pain. Prospective correlation of magnetic resonance imaging and discography in asymptomatic subjects and pain sufferers. Spine. 1996;21(3):300–311. doi: 10.1097/00007632-199602010-00009. discussion 11-2. [DOI] [PubMed] [Google Scholar]