Abstract
The relationship between trauma and psychosis is complex and multifaceted, with evidence suggesting that trauma can be both a risk factor for the development of psychosis and a consequence of psychotic experiences. The present review aimed to provide an overview of the current state of knowledge on the relationship between trauma and psychosis, including historical and conceptual considerations, as well as epidemiological evidence. The potential explanation of the link between trauma and psychosis is provided through available models and similarities in their neurobiological associations. Overall, the research confirms the relationship between trauma and psychosis, and suggests that individuals with a co-occurring history of trauma and psychosis may have increased symptom severity and worse functional outcomes compared with individuals with psychosis alone. Future research should focus on elucidating the underlying causal pathways between trauma exposure and psychosis in order to inform effective treatment approaches aiming to prevent the intensification of psychotic symptoms and processes.
Keywords: childhood trauma, schizophrenia spectrum disorders, adverse experiences, psychotic-like experiences, neurobiological associations
1. Introduction
Historically, the relationship between trauma and psychosis has been poorly understood, with traditional conceptualizations of psychosis focusing solely on biological explanations such as genetics and brain abnormalities (1). However, in the past 20 years there has been a shift towards a holistic understanding of psychosis that considers the potential influence of environmental and social factors, including trauma (2). This shift has been supported by a growing body of research that has demonstrated high rates of trauma exposure among individuals with schizophrenia spectrum disorders, with estimates ranging from 38-87% (2). Metanalytic studies indicate that the odds for developing a psychotic disorder in adults who experienced trauma in childhood is three times higher than those who did not, whereas their overall risk for the development of psychosis is 33% (3-8).
The aim of the present review was to summarize the current state of knowledge of the link between trauma and psychosis. For this purpose, a short historical overview and clarification of the trauma construct is provided first, followed by a review of the epidemiological evidence of the relationship between trauma and psychosis, and its specificity. Finally, models that explain the link between trauma and psychosis, as well as the similarities in neurobiological associations of childhood trauma (CT) and schizophrenia, are presented.
2. Trauma and mental health: A historical and conceptual overview
The relationship between trauma and psychosis has a complex and multifaceted history, with various conceptualizations and theories being proposed to explain the link between the two. From a historical perspective, ancient Greek and Roman philosophers, such as Aristotle and Cicero, were amongst the first to recognize the psychological effects of intense stress and adversity (9,10). However, it was not until the late 19th and early 20th centuries that trauma began to be systematically studied and recognized as a distinct concept in psychology and psychiatry. The term ‘trauma’ was first coined in the medical literature in the 1870s by the German neurologist Hermann Oppenheim (11) to describe the physical effects of injuries on the nervous system (12). In the late 19th and early 20th century, the psychoanalyst Sigmund Freud proposed the concept of ‘trauma neurosis’ (13), which was considered to be the result of an individual being overwhelmed by an emotionally charged event that was too difficult to process or integrate (14). The conceptualization of trauma by Freud focused on the role of repression in the development of psychological symptoms. He considered that the key to resolving trauma was to help individuals access and process the repressed memories and emotions associated with the traumatic event (12,14).
In the research literature the terms trauma, adverse childhood experiences (ACEs) and stressful life events (SLEs) are used interchangeably. However, these are measured by different assessment instruments, posing challenges in the interpretation and integration of the relevant research findings.
Trauma, as it relates to post-traumatic stress disorder (PTSD), is classified as the Criterion A (stressor) and includes direct exposure to trauma (actual or threatened mortality, serious injury or sexual violence), witnessing the trauma and learning that a relative or close friend was exposed to a trauma (15).
CT refers to the experience of a highly distressing event or situation during early childhood (0-5 years) that is beyond the coping capacity and/or control of the individual. Within this framework it may include a range of experiences such as neglect, abandonment, sexual abuse, physical abuse, witnessing abuse of a sibling or parent, or having a mentally ill parent (16). Additionally, CT is often referred to as a serious ACE that occurs in childhood (0-17 years) and includes various types of abuse and neglect, household dysfunction (for example, divorce, parental mental illness and substance use, and witnessing violence), experiencing racism/discrimination, bullying and community violence (16). Research has indicated that exposure to multiple ACEs can have a cumulative effect to the risk of an individual developing a range of physical and mental health problems, including mental illness such as schizophrenia spectrum disorders (17-20).
SLEs refer to discrete experiences that disrupt the usual activities of an individual, causing an extensive change and readjustment, such as illness or injury, divorce and changing or losing a job (21); experiencing ongoing stressful circumstances such as living with a disability or living in poverty are occasionally also included, and overlap with chronic psychosocial adversity.
3. Relationship between trauma and psychosis: Epidemiological evidence
In the epidemiological literature, there is evidence for an association between childhood psychosocial adversity and trauma (4), and an increased risk of developing psychosis or psychotic-like experiences (PLEs), which are defined as non-clinical schizophrenia spectrum symptoms (for example, unusual beliefs or perceptual abnormalities) (22).
A quantitative review and meta-analysis of 10 prospective cohort studies, 8 large population-based cross-sectional studies and 18 case-control studies confirmed, with an overall effect of odds ratio (OR) of 2.78 (95% CI, 2.34-3.31), the associations between ACEs and psychosis across all of the research designs. The case-control studies indicated that patients with psychosis had a 2.72 times increased probability of ACE exposure compared with controls (95% CI, 1.90-3.88). Furthermore, the association between childhood adversity and psychosis was significant in population-based cross-sectional studies (OR, 2.99; 95% CI, 2.12-4.20). The estimated population attributable risk (PAR) using the mean values of the calculated weighted proportion and the OR was 33% (range, 16-47%) (4).
Higher rates of CT have been revealed in individuals with an ultra-high risk (UHR) and clinical high risk (CHR) of developing psychosis. A previous review and meta-analysis of 6 studies with UHR populations indicated an increased prevalence rate of CT (86.8%), as compared with healthy controls (42-60%) (23). Additionally, a history of CT in individuals with UHR was equally common in patients with first-episode schizophrenia and was associated with the severity of psychotic symptoms (23). Similar findings were reported within CHR populations (24). In a large clinical sample of 2,608 patients with psychotic disorders, the PTSD rate was estimated to be 16% (25), whereas in a sample of 103 adolescents and young adults (12-30 years old) with CHR for developing psychosis the PTSD rate was 14% (19).
A dose-dependent response between CT and psychosis has been revealed in several studies (5,19). Exposure to multiple types of trauma has been associated with a greater risk of developing psychosis (26) and with transitioning of individuals with CHR to full psychosis (27) when compared with individuals exposed to a single type of trauma. A previous qualitative study, using semi-structured interviews with 11 participants, purposively recruited from larger quantitative research on post-traumatic reactions in individuals with psychosis, revealed high rates of interpersonal trauma. Participants recognized the link between past traumas and the characteristics of their psychotic experiences (PEs), and that these were aggravated by the lack of opportunities to discuss the trauma (23).
4. Relationship between the type of CT/ACE and psychotic symptoms
Several studies indicate that specific types of traumatic experiences with intention to harm (28), such as the experience of bullying (29,30), sexual abuse (29) or domestic violence (31), may be associated with PLEs. Similarly, neglect and interpersonal violence, as compared with parental loss, unintentional injury or economic adversity, were indicated to be strongly associated with the risk for developing psychotic symptoms (7,29,32). Exposure to any ACEs was associated with an increased probability of a later onset of PLEs (OR, 2.3; 95% CI, 1.9-2.6). Sexual abuse exhibited a strong association with the onset of PLEs during childhood (4-12 years; OR, 8.5; 95% CI, 3.6-20.2), whereas other types of ACE were associated with the onset of PLEs during adolescence. (13-19 years). The PARP for PLEs associated with all ACEs was 31% (and 24% for maladaptive family functioning) (29).
In terms of whether specific types of experienced trauma can evoke specific psychotic symptoms, the research findings vary across studies. Several studies have specifically linked exposure to CT to hallucinations (33-35), and to both hallucinations and delusions (36-38). In a large epidemiological study (39), the entire range of psychotic symptoms were strongly associated with CT, with no evidence of specific relationships between particular types of trauma and particular PEs. However, another study in a non-clinical young adult sample (aged 18-22 years; mean age, 19.7 years) indicated the differential impacts of the type of CT on specific positive psychotic symptom domains. An association was found between sexual abuse and difficulties in communication, while emotional neglect was linked with an increase in suspiciousness/persecutory ideas, which were above and beyond the effect of other co-occurring traumas. These results indicate that these experiences are mediated by trauma even in individuals that do not meet the criteria for psychotic disorders (40).
A study with young individuals (14-26 years old) at UHR indicated that physical abuse was associated with higher levels of suspiciousness, visual disturbances, low mood and grandiose beliefs compared with levels in individuals without such a history. However, sexual trauma was associated to perceptual disturbances with abusive content and PTSD symptoms (41). Another study in individuals with CHR demonstrated that trauma exposure before age 12 occurs prior to the onset of the CHR syndrome, and is associated with severe perceptual disturbances, general/affective symptoms and social functioning impairment; the number of interpersonal traumas was correlated (Spearman's correlation) with ratings of suspiciousness, perceptual disturbances, affective symptoms and global functioning impairment (19).
5. Models explaining the link between trauma and psychosis
Various models have been proposed to explain the link between trauma and psychosis (Table I). The most influential model(s) is the diathesis-stressor model/stress-vulnerability model, which suggests that following trauma exposure, individuals with a genetic risk for developing psychosis are at an increased risk of developing the disorder (42). The stress sensitization hypothesis suggests that early-life (0-5 years) psychosocial adversity may affect neurobiological pathways involved in stress regulation, by affecting the function of the hypothalamus-pituitary-adrenal (HPA) axis, leading to an altered stress response (43) and heightened stress sensitivity to future stressors in adolescence and adulthood (44-46). This, in turn, may contribute to the development of psychotic symptoms through increased activity of dopaminergic pathways (47).
Table I.
A summary of the evidence supporting the four pathway models linking childhood trauma with psychosis.
| A, Diathesis-stressor model/stress-vulnerability model | |||
|---|---|---|---|
| First author/s, year | Sample size, n | Type of study | (Refs.) |
| Read et al, 2001 | 33,648 | Systematic review (1961-2000) | (42) |
| Walker et al, 2008 | - | Narrative review | (47) |
| Myin-Germeys and van Os, 2007 | 138 | Case-control study using an experience sampling method | (46) |
| Lardinois et al, 2011 | 50 | Clinical study, using an experience sampling method | (44) |
| B, Dual-hit/two-hit hypothesis model | |||
| First author/s, year | Sample size, n | Type of study | (Refs.) |
| Bayer et al, 1999 | - | Conceptual paper based on available research findings | (52) |
| Maynard et al, 2001 | - | Conceptual paper based on available research findings | (53) |
| C, Socio-developmental hypothesis model | |||
| First author/s, year | Sample size, n | Type of study | (Refs.) |
| Morgan et al, 2010 | 780 | Systematic review of 32 studies on risk factors for psychosis in migrants and ethnic minority groups | (48) |
| Croft et al, 2019 | 4,433 | Population-based birth cohort study | (18) |
| Davis et al, 2017 | 46 | Clinical longitudinal study | (49) |
| Morgan et al, 2020 | 675 | Population-based case-control study of first-episode psychosis, conducted over a 4-year period (2010-2014) | (54) |
| D, Theory of social defeat model | |||
| First author/s, year | Sample size, n | Type of study | (Ref.) |
| Selten and Cantor-Graae, 2005 | - | Narrative review | (55) |
| Morgan et al, 2010 | 780 | Systematic review of 32 studies on risk factors for psychosis in migrants and ethnic minority groups | (48) |
| van Dam et al, 2012 | 23,721 | Metanalysis of 14 population-based studies (cross-sectional and follow-up studies) | (56) |
| Varese et al, 2012 | 78,207 | Metanalysis of 41 studies (prospective cohort, large-scale cross-sectional and case-control studies) | (4) |
| Alameda et al, 2020 | 75,086 | Systematic review (1979-2019) | (51) |
The socio-developmental hypothesis suggests that multiple stressors interact at various stages of development to cumulatively increase the risk of developing psychosis through gene-environment interactions (48) and via epigenetic mechanisms, including DNA methylation changes, histone modifications and non-coding RNAs (49,50). These epigenetic changes may affect the expression of genes involved in neurodevelopment, stress response and synaptic function, which potentially contribute to the development of psychosis following trauma (48) by impacting the dopaminergic, serotonergic, glutamatergic and GABAergic neurotransmitter systems, the immune system and oxidative stress (51). Additionally, the dual hit/two-hit hypothesis model, suggests that genetic vulnerability and pre-/perinatal risk factors (such as hypoxia, maternal stress, viral infection and malnutrition) lead to an altered neuronal network (the first hit) that may prime the individual to become more responsive to environmental stressors (such as childhood trauma, urbanicity, migration and substance abuse) early or later in life (the second hit) (52,53). According to this model, trauma activates the stress response system, leading to the release of stress hormones such as cortisol, which in turn may have a negative impact on brain function and lead to the development or worsening of psychotic symptoms. The Childhood Adversity and Psychosis (CAPsy) study in the UK using a sample of 374 cases with first-episode psychosis and 301 population-based controls (54) found that all forms of ACEs were associated with an approximately two- to four-fold increased probability of individuals developing a psychotic disorder. Furthermore, exposure to multiple adversities was associated with a linear increase in this probability. A birth cohort study of children and adolescents provided additional evidence of a cumulative effect, with an increased risk associated with an increased level/dose of exposure to trauma that persisted even after adjusting for genetic risk (18).
The theory of social defeat is another mechanism that has been proposed to explain the link between CT and psychosis, whereby prolonged or chronic exposure to victimization may lead to negative evaluations of the self and other individuals, leading to hostile interpretations of ambiguous social situations and the intention of other individuals (55). Previous meta-analyses indicated a two to four times increased risk for developing psychosis following exposure to any CT, whether from caregivers (such as abuse) or peers (such as bullying) (4,56). Proposed psychological pathways have included dissociation and post-traumatic stress, feelings of loneliness, negative self-schemas and affective pathways, such as depression, anxiety and emotional dysregulation (48,51).
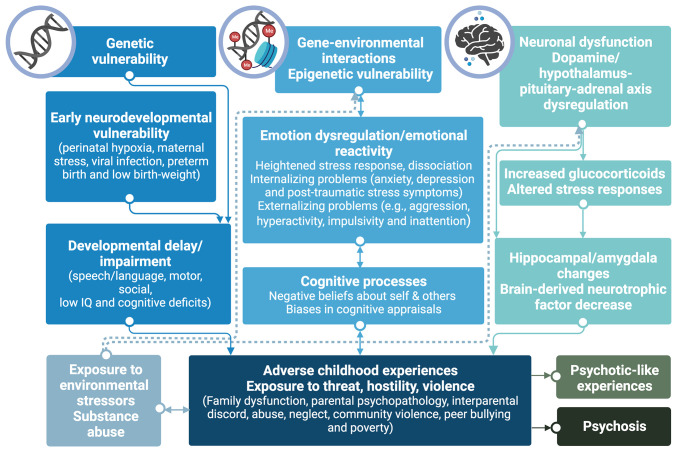
These findings suggest that the extreme experiences of threat, hostility and violence in childhood and adolescence may mediate the development of psychotic symptoms in individuals with underlying genetic susceptibility and neurodevelopmental adversity through cognitive processes (such as negative beliefs about the self, world and others, leading to distressing interpretations of everyday events or cognitive appraisal biases that could eventually result in paranoid delusion), affective pathways (such as anxiety, depression and emotional dysregulation, leading to dissociation that could eventually evoke hallucinations) and neurobiological systems implicated in psychotic disorders such as those of the amygdala, HPA axis and dopaminergic system (48,51) (Fig. 1). Additionally, data from a large population UK birth cohort study (n=3,514), the Avon Longitudinal Study of Parents and Children (57), indicated that being exposed to a traumatic experience in childhood (5-11 years) and adolescence (11-17 years) was associated with PE development by the age of 24. Neurodevelopmental adversity (for example, due to a low birth weight or being born preterm) and exposure to trauma were independently associated with PEs, even after adjusting for socio-demographic and genetic risks. The indirect relationship between neurodevelopmental adversity and PEs via an increased exposure to CT, in particular peer bullying, highlighted that early developmental risk and impairment may lead to further ACEs along the developmental pathway, cumulating in negative mental health outcomes, including psychosis (26).
Figure 1.
Overview of models explaining the link between trauma and psychosis. Evidence presented in the current review is summarized, highlighting the implication of diverse yet interrelated neurobiological and psychosocial pathways in the propagation of psychotic-like symptoms and psychosis in patients with a history of trauma or serious adverse childhood experiences. The figure was created with BioRender (https://biorender.com). IQ, intelligence quotient.
6. Similarities in neurobiological associations of CT and schizophrenia
Consistently, the data from both human and animal studies indicate that dopaminergic and glutaminergic dysfunction is implicated in psychosis and trauma-associated disorders (55,58,59,60,61). The commonly suggested mechanism linking CT to psychosis is the ‘sensitization’ of the mesolimbic dopamine system (60) that results in dopamine dysregulation and abnormal perceptual and cognitive experiences, which may increase the risk of developing schizophrenia (55,62). Exposure to ACEs is associated with mesolimbic dopamine release (62) and elevated striatal dopamine function in adulthood (58). Glucocorticoids (cortisol), which are involved in the stress response, also modify the dopamine neurotransmission (62). HPA axis dysregulation is observed in individuals exposed to trauma (63) and in individuals with schizophrenia (62). HPA axis hyperactivity in adolescents meeting clinical high risk (CHR) criteria for psychosis, as indicated by increased cortisol levels, is predictive of psychosis (64,65), and is associated with increased psychotic symptom severity and symptom progression (66).
Prolonged stress or prolonged exposure to glucocorticoids has toxic effects for the development of the brain, and in particular the hippocampus (67). Hippocampal changes such as volume reduction (68) and decreased brain-derived neurotrophic factor levels are observed in patients with schizophrenia (69-73) and in individuals with early-life adversity (74-76). Enduring childhood traumatic experiences and early-course schizophrenia seems to be associated with a reduced amygdala volume (77-79), deficits in amygdala reactivity (80,81) and altered functional connectivity with the prefrontal cortex (64,82). These disturbances in the amygdala and other emotional and related brain systems (such as ventromedial, orbitofrontal and anterior singulate cortex, mesolimbic and mesocortical dopamine pathways, hippocampus and nucleus accumbens) contribute to the schizophrenia symptoms (83).
Inflammation has also been identified as a potential contributor to the development of both psychosis and PTSD. Specifically, increased levels of inflammatory markers, such as interleukin-6, were revealed in individuals with psychosis (84), as well as in individuals with PTSD (85).
7. Conclusion
Overall, the present review of the research evidence confirms the relationship between exposure to traumatic experiences in childhood and psychosis. However, this relationship lacks specificity, is complex and is not fully understood. Future prospective studies of children with genetic and/or developmental vulnerabilities, exposed to severe and enduring traumatic events, which focus on the interplay between mediating and moderating factors (such as biological, neurocognitive, emotional and environmental factors), may elucidate the different pathways linking trauma and psychosis. In turn, this would inform interventions aimed at mitigating and managing the risk of developing psychosis or other negative mental health outcomes. The clinical implication of the present review indicates the importance of comprehensive screening for trauma in all patients presenting with psychotic-like symptoms or a psychotic disorder. Furthermore, trauma-informed interventions should be implemented with the aim of preventing the intensification of psychotic symptoms and processes.
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
IG and SG wrote the original draft, and edited and critically revised the manuscript. DAS, MIS and ER critically revised and edited the manuscript. All authors substantially contributed to the conception and revision of the work. All authors read and approved the final manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
IG, SG, MS and ER declare that they have no competing interests. DAS is the Editor-in-Chief for the journal, but had no personal involvement in the reviewing process, or any influence in terms of adjudicating on the final decision, for this article.
References
- 1.Jablensky A. The diagnostic concept of schizophrenia: Its history, evolution, and future prospects. Dialogues Clin Neurosci. 2010;12:271–287. doi: 10.31887/DCNS.2010.12.3/ajablensky. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grubaugh AL, Zinzow HM, Paul L, Egede LE, Frueh BC. Trauma exposure and posttraumatic stress disorder in adults with severe mental illness: A critical review. Clin Psychol Rev. 2011;31:883–899. doi: 10.1016/j.cpr.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bloomfield MAP, Chang T, Woodl MJ, Lyons LM, Cheng Z, Bauer-Staeb C, Hobbs C, Bracke S, Kennerley H, Isham L, et al. Psychological processes mediating the association between developmental trauma and specific psychotic symptoms in adults: A systematic review and meta-analysis. World Psychiatry. 2021;20:107–123. doi: 10.1002/wps.20841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, van Os J, Bentall RP. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heins M, Simons C, Lataster T, Pfeifer S, Versmissen D, Lardinois M, Marcelis M, Delespaul P, Krabbendam L, van Os J, Myin-Germeys I. Childhood trauma and psychosis: A case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry. 2011;168:1286–1294. doi: 10.1176/appi.ajp.2011.10101531. [DOI] [PubMed] [Google Scholar]
- 6.Morrison AP, Frame L, Larkin W. Relationships between trauma and psychosis: A review and integration. Br J Clin Psychol. 2003;42(Pt 4):331–353. doi: 10.1348/014466503322528892. [DOI] [PubMed] [Google Scholar]
- 7.Spauwen J, Krabbendam L, Lieb R, Wittchen HU, van Os J. Impact of psychological trauma on the development of psychotic symptoms: Relationship with psychosis proneness. Br J Psychiatry. 2006;188:527–533. doi: 10.1192/bjp.bp.105.011346. [DOI] [PubMed] [Google Scholar]
- 8.Meade CS, Kershaw TS, Hansen NB, Sikkema KJ. Long-term correlates of childhood abuse among adults with severe mental illness: Adult victimization, substance abuse, and HIV sexual risk behavior. AIDS Behav. 2009;13:207–216. doi: 10.1007/s10461-007-9326-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ierodiakonou C. The Psychology of Aristotle, The Philosopher: A Psychoanalytic Therapist's Perspective. Routledge, London, 2019. [Google Scholar]
- 10. Cicero: The Nature of the Gods. 1st edition. Oxford University Press, Oxford, 2008. [Google Scholar]
- 11.Oppenheim H. Wie sind diejenigen Fälle von Neurasthenie aufzufassen, welche sich nach Erschütterung des Rückenmarks insbesondere nach Eisenbahnunfällen entwickeln. Deutsche Medizinische Wochenschrift. 1888;14:194–196. [Google Scholar]
- 12.Van Der Kolk PA, Van Der Hart . The intrusisve PastQ The Flexibility of Memory and Engraving of Trauma. American Imago. 1991;48:425–454. [Google Scholar]
- 13.Strachey J. Standard Edition of the Complete Psychological Works of Sigmund Freud Volume II (1893-1895): Studies on Hysteria. Hogarth Press and the Institute of Psycho-Analysis, London, 1955. [Google Scholar]
- 14.Sletvold J. Freud's three theories of neurosis: Towards a contemporary theory of trauma and defense. Psychoanalytic Dialogues. 2016;26:460–475. [Google Scholar]
- 15. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR). 5th edition. American Psychiatric Publishing Inc., Washinghton, 2013. [Google Scholar]
- 16. Centers of Disease Control and Prevention (CDC): Violence Prevention: Injury Center: About the CDC-Kaiser ACE Study. United States Department of Health and Human Services, Atlanta, 2022. [Google Scholar]
- 17.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 18.Croft J, Heron J, Teufel C, Cannon M, Wolke D, Thompson A, Houtepen L, Zammit S. Association of trauma type, age of exposure, and frequency in childhood and adolescence with psychotic experiences in early adulthood. JAMA Psychiatry. 2019;76:79–86. doi: 10.1001/jamapsychiatry.2018.3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loewy RL, Corey S, Amirfathi F, Dabit S, Fulford D, Pearson R, Hua JPY, Schlosser D, Stuart BK, Mathalon DH, Vinogradov S. Childhood trauma and clinical high risk for psychosis. Schizophr Res. 2019;205:10–14. doi: 10.1016/j.schres.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children's self-reported psychotic symptoms and adult schizophreniform disorder: A 15-year longitudinal study. Arch Gen Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- 21.Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychol Bull. 2006;132:477–495. doi: 10.1037/0033-2909.132.3.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rössler W, Ajdacic-Gross V, Rodgers S, Haker H, Müller M. Childhood trauma as a risk factor for the onset of subclinical psychotic experiences: Exploring the mediating effect of stress sensitivity in a cross-sectional epidemiological community study. Schizophr Res. 2016;172:46–53. doi: 10.1016/j.schres.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Kraan T, Velthorst E, Smit F, de Haan L, van der Gaag M. Trauma and recent life events in individuals at ultra high risk for psychosis: Review and meta-analysis. Schizophr Res. 2015;161:143–149. doi: 10.1016/j.schres.2014.11.026. [DOI] [PubMed] [Google Scholar]
- 24.Kline E, Millman ZB, Denenny D, Wilson C, Thompson E, Demro C, Connors K, Bussell K, Reeves G, Schiffman J. Trauma and psychosis symptoms in a sample of help-seeking youth. Schizophr Res. 2016;175:174–179. doi: 10.1016/j.schres.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 25.de Bont PA, van den Berg DP, van der Vleugel BM, de Roos C, de Jongh A, van der Gaag M, van Minnen A. Predictive validity of the Trauma Screening Questionnaire in detecting post-traumatic stress disorder in patients with psychotic disorders. Br J Psychiatry. 2015;206:408–416. doi: 10.1192/bjp.bp.114.148486. [DOI] [PubMed] [Google Scholar]
- 26.Liu Y, Mendonça M, Cannon M, Jones PB, Lewis G, Thompson A, Zammit S, Wolke D. Testing the independent and joint contribution of exposure to neurodevelopmental adversity and childhood trauma to risk of psychotic experiences in adulthood. Schizophr Bull. 2021;47:776–784. doi: 10.1093/schbul/sbaa174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stowkowy J, Liu L, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, et al. Early traumatic experiences, perceived discrimination and conversion to psychosis in those at clinical high risk for psychosis. Soc Psychiatry Psychiatr Epidemiol. 2016;51:497–503. doi: 10.1007/s00127-016-1182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moriyama TS, Drukker M, Gadelha A, Pan PM, Salum GA, Manfro GG, Mari JJ, Miguel EC, Rohde LA, Polanczyk GV, et al. The association between psychotic experiences and traumatic life events: The role of the intention to harm. Psychol Med. 2018;48:2235–2246. doi: 10.1017/S0033291717003762. [DOI] [PubMed] [Google Scholar]
- 29.McGrath JJ, McLaughlin KA, Saha S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Bruffaerts R, de Girolamo G, de Jonge P, Esan O, et al. The association between childhood adversities and subsequent first onset of psychotic experiences: A cross-national analysis of 23 998 respondents from 17 countries. Psychol Med. 2017;47:1230–1245. doi: 10.1017/S0033291716003263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strauss GP, Raugh IM, Mittal VA, Gibb BE, Coles ME. Bullying victimization and perpetration in a community sample of youth with psychotic like experiences. Schizophr Res. 2018;195:534–536. doi: 10.1016/j.schres.2017.08.056. [DOI] [PubMed] [Google Scholar]
- 31.Kelleher I, Harley M, Lynch F, Arseneault L, Fitzpatrick C, Cannon M. Associations between childhood trauma, bullying and psychotic symptoms among a school-based adolescent sample. Br J Psychiatry. 2008;193:378–382. doi: 10.1192/bjp.bp.108.049536. [DOI] [PubMed] [Google Scholar]
- 32.Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children's emerging psychotic symptoms: A genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168:65–72. doi: 10.1176/appi.ajp.2010.10040567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whitfield CL, Dube SR, Felitti VJ, Anda RF. Adverse childhood experiences and hallucinations. Child Abuse Negl. 2005;29:797–810. doi: 10.1016/j.chiabu.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112:330–350. doi: 10.1111/j.1600-0447.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- 35.Hardy A, Fowler D, Freeman D, Smith B, Steel C, Evans J, Garety P, Kuipers E, Bebbington P, Dunn G. Trauma and hallucinatory experience in psychosis. J Nerv Ment Dis. 2005;193:501–507. doi: 10.1097/01.nmd.0000172480.56308.21. [DOI] [PubMed] [Google Scholar]
- 36.Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, de Graaf R, van Os J. Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatr Scand. 2004;109:38–45. doi: 10.1046/j.0001-690x.2003.00217.x. [DOI] [PubMed] [Google Scholar]
- 37.Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the adult psychiatric morbidity survey. Schizophr Bull. 2012;38:734–740. doi: 10.1093/schbul/sbs049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Read J, Argyle N. Hallucinations, delusions, and thought disorder among adult psychiatric inpatients with a history of child abuse. Psychiatr Serv. 1999;50:1467–1472. doi: 10.1176/ps.50.11.1467. [DOI] [PubMed] [Google Scholar]
- 39.van Nierop M, Lataster T, Smeets F, Gunther N, van Zelst C, de Graaf R, ten Have M, van Dorsselaer S, Bak M, Myin-Germeys I, et al. Psychopathological mechanisms linking childhood traumatic experiences to risk of psychotic symptoms: Analysis of a large, representative population-based sample. Schizophr Bull. 2014;40 (Suppl 2):S123–S130. doi: 10.1093/schbul/sbt150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ered A, Ellman LM. Specificity of childhood trauma type and attenuated positive symptoms in a non-clinical sample. J Clin Med. 2019;8(1537) doi: 10.3390/jcm8101537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Velthorst E, Nelson B, O'Connor K, Mossaheb N, de Haan L, Bruxner A, Simmons MB, Yung AR, Thompson A. History of trauma and the association with baseline symptoms in an ultra-high risk for psychosis cohort. Psychiatry Res. 2013;210:75–81. doi: 10.1016/j.psychres.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 42.Read J, Perry B, Moskowitz A, Connolly J. The contribution of early traumatic events to schizophrenia in some patients: A traumagenic neurodevelopmental model. Psychiatry. 2001;64:319–345. doi: 10.1521/psyc.64.4.319.18602. [DOI] [PubMed] [Google Scholar]
- 43.Charmandari E, Kino T, Souvatzoglou E, Chrousos GP. Pediatric stress: Hormonal mediators and human development. Horm Res. 2003;59:161–179. doi: 10.1159/000069325. [DOI] [PubMed] [Google Scholar]
- 44.Lardinois M, Lataster T, Mengelers R, Van Os J, Myin-Germeys I. Childhood trauma and increased stress sensitivity in psychosis. Acta Psychiatr Scand. 2011;123:28–35. doi: 10.1111/j.1600-0447.2010.01594.x. [DOI] [PubMed] [Google Scholar]
- 45.Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- 46.Myin-Germeys I, van Os J. Stress-reactivity in psychosis: Evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27:409–424. doi: 10.1016/j.cpr.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 47.Walker E, Mittal V, Tessner K. Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu Rev Clin Psychol. 2008;4:189–216. doi: 10.1146/annurev.clinpsy.4.022007.141248. [DOI] [PubMed] [Google Scholar]
- 48.Morgan C, Charalambides M, Hutchinson G, Murray RM. Migration, ethnicity, and psychosis: Toward a sociodevelopmental model. Schizophr Bull. 2010;36:655–664. doi: 10.1093/schbul/sbq051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Davis EG, Humphreys KL, McEwen LM, Sacchet MD, Camacho MC, MacIsaac JL, Lin DTS, Kobor MS, Gotlib IH. Accelerated DNA methylation age in adolescent girls: Associations with elevated diurnal cortisol and reduced hippocampal volume. Transl Psychiatry. 2017;7(e1223) doi: 10.1038/tp.2017.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen Q, Li D, Jin W, Shi Y, Li Z, Ma P, Sun J, Chen S, Li P, Lin P. Research progress on the correlation between epigenetics and schizophrenia. Front Neurosci. 2021;15(688727) doi: 10.3389/fnins.2021.688727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alameda L, Rodriguez V, Carr E, Aas M, Trotta G, Marino P, Vorontsova N, Herane-Vives A, Gadelrab R, Spinazzola E, et al. A systematic review on mediators between adversity and psychosis: Potential targets for treatment. Psychol Med. 2020;50:1966–1976. doi: 10.1017/S0033291720002421. [DOI] [PubMed] [Google Scholar]
- 52.Bayer TA, Falkai P, Maier W. Genetic and non-genetic vulnerability factors in schizophrenia: The basis of the ‘two hit hypothesis.’. J Psychiatr Res. 1999;33:543–548. doi: 10.1016/s0022-3956(99)00039-4. [DOI] [PubMed] [Google Scholar]
- 53.Maynard TM, Sikich L, Lieberman JA, LaMantia AS. Neural development, cell-cell signaling, and the ‘two-hit’ hypothesis of schizophrenia. Schizophr Bull. 2001;27:457–476. doi: 10.1093/oxfordjournals.schbul.a006887. [DOI] [PubMed] [Google Scholar]
- 54.Morgan C, Gayer-Anderson C, Beards S, Hubbard K, Mondelli V, Di Forti M, Murray RM, Pariante C, Dazzan P, Craig TJ, et al. Threat, hostility and violence in childhood and later psychotic disorder: population-based case-control study. Br J Psychiatry. 2020;217:575–582. doi: 10.1192/bjp.2020.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Selten JP, Cantor-Graae E. Social defeat: Risk factor for schizophrenia? Br J Psychiatry. 2005;187:101–102. doi: 10.1192/bjp.187.2.101. [DOI] [PubMed] [Google Scholar]
- 56.van Dam DS, van der Ven E, Velthorst E, Selten JP, Morgan C, de Haan L. Childhood bullying and the association with psychosis in non-clinical and clinical samples: A review and meta-analysis. Psychol Med. 2012;42:2463–2474. doi: 10.1017/S0033291712000360. [DOI] [PubMed] [Google Scholar]
- 57.Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, Molloy L, Ness A, Ring S, Davey Smith G. Cohort Profile: The ’children of the 90s’-the index offspring of the Avon longitudinal study of parents and children. Int J Epidemiol. 2013;42:111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Egerton A, Valmaggia LR, Howes OD, Day F, Chaddock CA, Allen P, Winton-Brown TT, Bloomfield MAP, Bhattacharyya S, Chilcott J, et al. Adversity in childhood linked to elevated striatal dopamine function in adulthood. Schizophr Res. 2016;176:171–176. doi: 10.1016/j.schres.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Averill LA, Purohit P, Averill CL, Boesl MA, Krystal JH, Abdallah CG. Glutamate dysregulation and glutamatergic therapeutics for PTSD: Evidence from human studies. Neurosci Lett. 2017;649:147–155. doi: 10.1016/j.neulet.2016.11.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Collip D, Myin-Germeys I, Van Os J. Does the concept of ‘sensitization’ provide a plausible mechanism for the putative link between the environment and schizophrenia? Schizophr Bull. 2008;34:220–225. doi: 10.1093/schbul/sbm163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McCutcheon RA, Krystal JH, Howes OD. Dopamine and glutamate in schizophrenia: Biology, symptoms and treatment. World Psychiatry. 2020;19:15–33. doi: 10.1002/wps.20693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pruessner JC, Champagne F, Meaney MJ, Dagher A. Dopamine release in response to a psychological stress in humans and its relationship to early life maternal care: A positron emission tomography study using [11C]Raclopride. J Neurosci. 2004;24:2825–2831. doi: 10.1523/JNEUROSCI.3422-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol Bull. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- 64.Cisler JM. Childhood trauma and functional connectivity between amygdala and medial prefrontal cortex: A dynamic functional connectivity and large-scale network perspective. Front Syst Neurosci. 2017;11(29) doi: 10.3389/fnsys.2017.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Walker EF, Brennan PA, Esterberg M, Brasfield J, Pearce B, Compton MT. Longitudinal changes in cortisol secretion and conversion to psychosis in at-risk youth. J Abnorm Psychol. 2010;119:401–408. doi: 10.1037/a0018399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Walker EF, Trotman HD, Pearce BD, Addington J, Cadenhead KS, Cornblatt BA, Heinssen R, Mathalon DH, Perkins DO, Seidman LJ, et al. Cortisol levels and risk for psychosis: Initial findings from the North American prodrome longitudinal study. Biol Psychiatry. 2013;74:410–417. doi: 10.1016/j.biopsych.2013.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry. 2000;57:925–935. doi: 10.1001/archpsyc.57.10.925. [DOI] [PubMed] [Google Scholar]
- 68.Vita A, De Peri L, Silenzi C, Dieci M. Brain morphology in first-episode schizophrenia: A meta-analysis of quantitative magnetic resonance imaging studies. Schizophr Res. 2006;82:75–88. doi: 10.1016/j.schres.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 69.Ray MT, Weickert CS, Wyatt E, Webster MJ. Decreased BDNF, trkB-TK+ and GAD67 mRNA expression in the hippocampus of individuals with schizophrenia and mood disorders. J Psychiatry Neurosci. 2011;36:195–203. doi: 10.1503/jpn.100048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Daskalakis NP, De Kloet ER, Yehuda R, Malaspina D, Kranz TM. Early life stress effects on Glucocorticoid-BDNF interplay in the hippocampus. Front Mol Neurosci. 2015;8(68) doi: 10.3389/fnmol.2015.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rizos EN, Rontos I, Laskos E, Arsenis G, Michalopoulou PG, Vasilopoulos D, Gournellis R, Lykouras L. Investigation of serum BDNF levels in drug-naive patients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:1308–1311. doi: 10.1016/j.pnpbp.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 72.Rizos EN, Papathanasiou M, Michalopoulou PG, Mazioti A, Douzenis A, Kastania A, Nikolaidou P, Laskos E, Vasilopoulou K, Lykouras L. Association of serum BDNF levels with hippocampal volumes in first psychotic episode drug-naive schizophrenic patients. Schizophr Res. 2011;129:201–204. doi: 10.1016/j.schres.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 73.Rizos EN, Michalopoulou PG, Siafakas N, Stefanis N, Douzenis A, Rontos I, Laskos E, Kastania A, Zoumpourlis V, Lykouras L. Association of serum brain-derived neurotrophic factor and duration of untreated psychosis in first-episode patients with schizophrenia. Neuropsychobiology. 2010;62:87–90. doi: 10.1159/000315438. [DOI] [PubMed] [Google Scholar]
- 74.Roth TL, Lubin FD, Funk AJ, Sweatt JD. Lasting epigenetic influence of early-life adversity on the BDNF Gene. Biol Psychiatry. 2009;65:760–769. doi: 10.1016/j.biopsych.2008.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Campbell TS, Donoghue KM, Ghosh U, Nelson CM, Roth TL. Early life stress affects Bdnf regulation: A role for exercise interventions. Int J Mol Sci. 2022;23(11729) doi: 10.3390/ijms231911729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Giannopoulou I, Pagida MA, Briana DD, Panayotacopoulou MT. Perinatal hypoxia as a risk factor for psychopathology later in life: The role of dopamine and neurotrophins. Hormones (Athens) 2018;17:25–32. doi: 10.1007/s42000-018-0007-7. [DOI] [PubMed] [Google Scholar]
- 77.Weissman DG, Lambert HK, Rodman AM, Peverill M, Sheridan MA, McLaughlin KA. Reduced hippocampal and amygdala volume as a mechanism underlying stress sensitization to depression following childhood trauma. Depress Anxiety. 2020;37:916–925. doi: 10.1002/da.23062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rich AM, Cho YT, Tang Y, Savic A, Krystal JH, Wang F, Xu K, Anticevic A. Amygdala volume is reduced in early course schizophrenia. Psychiatry Res Neuroimaging. 2016;250:50–60. doi: 10.1016/j.pscychresns.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Aas M, Navari S, Gibbs A, Mondelli V, Fisher HL, Morgan C, Morgan K, MacCabe J, Reichenberg A, Zanelli J, et al. Is there a link between childhood trauma, cognition, and amygdala and hippocampus volume in first-episode psychosis? Schizophr Res. 2012;137:73–79. doi: 10.1016/j.schres.2012.01.035. [DOI] [PubMed] [Google Scholar]
- 80.Rasetti R, Mattay VS, Wiedholz LM, Kolachana BS, Hariri AR, Callicott JH, Meyer-Lindenberg A, Weinberger DR. Evidence that altered amygdala activity in schizophrenia is related to clinical state and not genetic risk. Am J Psychiatry. 2009;166:216–225. doi: 10.1176/appi.ajp.2008.08020261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marusak HA, Martin KR, Etkin A, Thomason ME. Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology. 2015;40:1250–1258. doi: 10.1038/npp.2014.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bjorkquist OA, Olsen EK, Nelson BD, Herbener ES. Altered amygdala-prefrontal connectivity during emotion perception in schizophrenia. Schizophr Res. 2016;175:35–41. doi: 10.1016/j.schres.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 83.Aleman A, Kahn RS. Strange feelings: Do amygdala abnormalities dysregulate the emotional brain in schizophrenia? Prog Neurobiol. 2005;77:283–298. doi: 10.1016/j.pneurobio.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 84.Stojanovic A, Martorell L, Montalvo I, Ortega L, Monseny R, Vilella E, Labad J. Increased serum interleukin-6 levels in early stages of psychosis: Associations with at-risk mental states and the severity of psychotic symptoms. Psychoneuroendocrinology. 2014;41:23–32. doi: 10.1016/j.psyneuen.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 85.Passos IC, Vasconcelos-Moreno MP, Costa LG, Kunz M, Brietzke E, Quevedo J, Salum G, Magalhães PV, Kapczinski F, Kauer-Sant'Anna M. Inflammatory markers in post-traumatic stress disorder: A systematic review, meta-analysis, and meta-regression. Lancet Psychiatry. 2015;2:1002–1012. doi: 10.1016/S2215-0366(15)00309-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.