Abstract
Introduction
Older age is associated with multimorbidity, chronic diseases and acute deteriorations and leads to complex care needs. Nursing home residents are more often unnecessarily transferred to emergency departments or hospitals than community dwellers—largely due to a lack of qualified staff and diffusion of responsibility in the institutions. In Germany, only few academically trained nurses work in nursing homes, and their potential roles are unclear. Therefore, we aim to explore feasibility and potential effects of a newly defined role profile for nurses with bachelors’ degree or equivalent qualification in nursing homes.
Methods and analysis
A pilot study (Expand-Care) with a cluster-randomised controlled design will be conducted in 11 nursing homes (cluster) in Germany, with an allocation ratio of 5:6 to the intervention or control group, aiming to include 15 residents per cluster (165 participants in total). Nurses in the intervention group will receive training to perform role-related tasks such as case reviews and complex geriatric assessments. We will collect data at three time points (t0 baseline, t1 3 months and t2 6 months after randomisation). We will measure on residents’ level: hospital admissions, further health services use and quality of life; clinical outcomes (eg, symptom burden), physical functioning and delivery of care; mortality, adverse clinical incidents and changes in care level. On nurses’ level, we will measure perception of the new role profile, competencies and implementation of role-related tasks as part of the process evaluation (mixed methods). An economic evaluation will explore resource use on residents’ (healthcare utilisation) and on nurses’ level (costs and time expenditure).
Ethics and dissemination
The ethics committees of the University of Lübeck (Nr. 22-162) and the University Clinic Hamburg-Eppendorf (Nr. 2022-200452-BO-bet) approved the Expand-Care study. Informed consent is a prerequisite for participation. Study results will be published in open-access, peer-reviewed journals and reported at conferences and in local healthcare providers’ networks.
Trial registration number
DRKS00028708.
Keywords: Aged, Health Services for the Aged, Patient-Centered Care, Quality of Life
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The intervention was developed systematically based on a root cause analysis of unplanned hospital admissions or emergency service utilisation and participatory workshops with patient representatives and other stakeholders.
A logic model including assumed causal mechanisms, distinct distal and proximal (mediating) outcomes and potentially relevant moderators (context factors) guides the evaluation, including a comprehensive process evaluation.
Outcomes will be assessed at patient and staff levels and include patient-reported outcome and experience measures as well as objective measures such as hospital admissions.
A potential limitation is the risk of early drop out of whole clusters (nursing homes) due to nursing staff shortages in the German elderly long-term care sector.
This pilot study will be exploratory in nature as we will rely on a small sample size and a short follow-up of three months after completion of implementation.
Introduction
Background and rationale
Older age and ageing processes are associated with multimorbidity, including both acute and chronic diseases. Symptom control in long-term illnesses, cognitive impairment, an overall high degree of dependency or need for end-of-life care lead to increasingly complex care needs.1 2 Nursing professionals in nursing homes (NHs) are often the first to decide whether the use of emergency medical services is necessary when residents’ health status deteriorates. These decisions are influenced by diverse contextual factors, among them unclear expectations of responsibilities of the NH regarding primary care, limited availability of qualified staff and the fear of exceeding one’s scope of responsibilities. Inadequate access to multidisciplinary outpatient care, as well as poor communication with other decision-makers or families exerting pressure may also contribute to hospital admissions although in principle they might be avoidable.3 Consequently, NH residents are significantly more often transferred to hospitals than community dwellers. Ninety per cent of these hospital transfers are unplanned, and between 4% and 55% are considered avoidable.4 For these residents, skills of academically qualified nurses could create a meaningful benefit.5 Academic training enables nurses to combine their clinical expertise with scientific evidence to provide care according to patient’s or resident’s preferences (evidence-based nursing).6 Care that is guided by individuals’ values and preferences is referred to as person-centred care and can improve patient experiences and outcomes, and enhance the efficiency of healthcare delivery.7 8
With the introduction of the new Nursing Professions Act (PflBG) 2020, academic nursing education is now implemented as a regular primary nursing qualification in Germany. Work areas of bachelor graduates are predominantly in direct patient care, but include taking over process responsibility in complex or unclear patient situations.9 However, surveys show that bachelor graduates rarely find satisfyingly suitable job profiles.10 Especially in the long-term care setting, defined work areas and competency-oriented differentiation of tasks and responsibilities for bachelor-qualified nurses are lacking.
In the Expand-Care project, we developed a role profile for academically trained nurses in a participatory research process11: PEPA (German acronym for nurse specialists with expanded competencies for person-centred elderly care (Pflegefachperson mit erweiterten Handlungskompetenzen für personenzentrierte Pflege in der Altenpflege)). The PEPA covers competence areas with a focus on residents’ needs regarding management of chronic and geriatric diseases, and empowerment and communication. Comprehensive implementation strategies target educational, supervisory and organisational levels.
Trial objectives
The objective of this trial is to explore feasibility, safety and resident-relevant benefits of the Expand-Care intervention programme promoting person-centred care in NH residents.
To assess safety and potential patient-relevant benefits, we will examine:
-
What are potential effects of the programme on
Patient-relevant indicators of quality of care (distal outcomes) like hospital admissions, emergency service utilisation, residents’ out-of-hour physician contacts and quality of life within 6 months of follow-up?
Intermediate (proximal) outcomes regarding residents’ clinical well-being and functioning and the delivery of care?
What is the risk of adverse effects of the programme on residents’ health, for example, with regard to mortality?
To assess programme feasibility, we will conduct a process evaluation addressing (A) nurses’ ability to acquire, maintain and apply the desired competencies for expanded care tasks; (B) implementation (reach and dose); (C) nurses’ perception of feasibility and fidelity of the intervention; (D) adaptations to intervention care tasks; (E) changes to care processes induced by the intervention and (F) changes to subjective professional roles, self-concept and self-efficacy of nurses.
With an economic analysis, we will assess implementation costs of the programme and consequences for healthcare resource utilisation.
Methods and analysis
Trial design
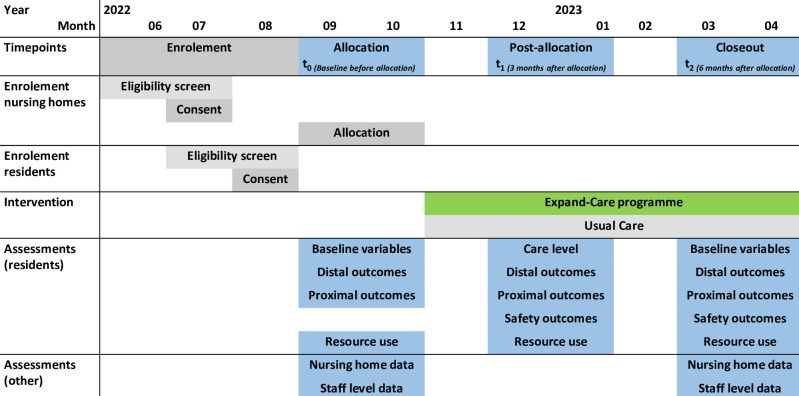
The Expand-Care trial is an exploratory bicentric cluster-randomised controlled trial (cRCT). NHs (clusters) will be randomly assigned either to the implementation of the Expand-Care intervention programme (intervention group) or to usual care (control group). Follow-up measurements take place 3 (t1) and 6 months (t2) post randomised allocation. For the process evaluation, the trial includes a parallel mixed-methods study which is described in detail in online supplemental file 1.
bmjopen-2023-072955supp001.pdf (321.5KB, pdf)
Study setting and participants
The trial will take place in 11 NH in Northern Germany. Eligible residents living in the participating NH will be invited to participate. Each NH has to nominate a qualified nurse specialist who will perform the intervention if randomised to this group (table 1, eligibility criteria).
Table 1.
Eligibility criteria for nursing homes, residents and nurse specialists
| Participants | Eligibility criteria |
| Nursing homes | All of the following conditions apply:
|
| Residents | One of the following conditions applies:
|
| Nurse specialists | One of the following conditions applies:
|
DEGAM: Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin e.V. (German association for primary care)39; German care levels (range from 0 to 5) are assessed by expert raters of the German statutory healthcare insurance and can be described as low (0/1/2), medium (3/4), high (5).
Interventions
Control group residents will receive optimised usual care: we will offer a 1.5-hour workshop on principles of person-centred care to control group NH.
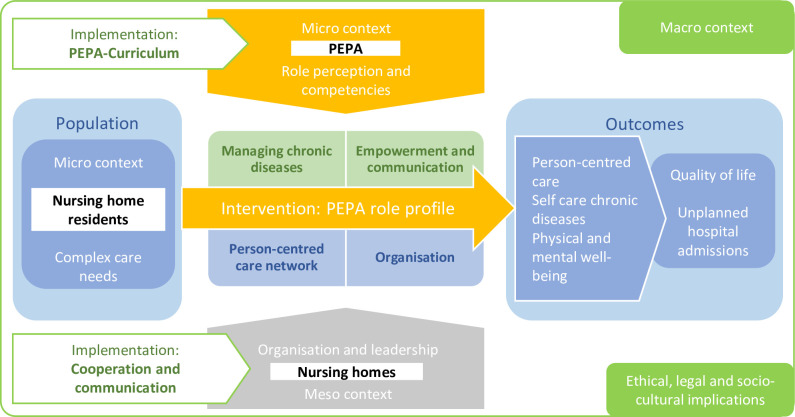
Intervention group residents will receive person-centred care through the implementation of a new role profile for nurses with expanded competencies (PEPA). The role profile addresses four competence areas: (1) managing chronic diseases; (2) empowerment and communication; (3) person-centred care network and (4) organisation (figure 1, logic model).
Figure 1.
Logic model of the expand-care intervention and implementation strategies. PEPA, German acronym for nurse specialists with expanded competencies for person-centred elderly care.
In practice, PEPAs will perform specific intervention components (PEPA activities) which are defined as core (obligatory) and optional activities on direct care (resident-related) and organisational levels (table 2).
Table 2.
Intervention components
| Core activities | Optional activities |
| Direct care level | |
|
|
| Organisational level | |
|
|
ISBAR, Structure for interprofessional communication consisting of Identification, Situation, Background, Assessment, Recommendation.
Parallel to the intervention development, we have designed implementation strategies targeting areas of education, supervision/evaluation and organisation.12 13 Detailed information on rationale, target groups, mode of delivery and materials for each intervention component and implementation strategy is described according to the TIDieR template (Template for Intervention Description and Replication) (online supplemental file 2).14
bmjopen-2023-072955supp002.pdf (177.5KB, pdf)
The main educational strategy is a 300-hour training for participating nurses (PEPA training programme) led by lecturers of the University of Lübeck. This education will be delivered based on a detailed curriculum containing two modules: (1) enhanced roles and competencies for nurses and (2) person-centred nursing and care for people with chronic diseases. Module (1) targets topics such as interprofessional communication, coaching and consulting, evidence-based practice, role development and legal aspects. Example topics of module (2) are pathology of chronic diseases, geriatric and nursing assessments, exacerbation of symptoms, pharmacological therapy, models of self-care, person-centred care and advanced care planning. Training methods comprise classroom and online teaching, training on the job and self-study time (about 100 hours each). Training will start immediately after randomisation and last for 3 months. Supervision and evaluation strategies will be performed by members of the research team via on-site or online mentoring sessions. By target agreement talks with PEPAs and nurse managers, a shared goal for the implementation will be established. Supervisors will review and give feedback on PEPAs’ performance of the implementation of intervention components in practice.
Organisational strategies aim to strengthen NHs’ commitment to the study: formal cooperation agreements between the university and participating NH comprise responsibilities regarding recruitment of residents and granted worktime for PEPAs. NHs are allowed to adapt the intervention locally to their needs to a defined degree (optional activities, table 2). A detailed description of the intervention development and the PEPA training programme will be published elsewhere.
Outcomes
Trial outcomes are based on the programme’s logic model (figure 1) and comprise distal and proximal outcomes. Distal outcomes include patient-important indicators of the quality of care that are assumed to be influenced by the Expand-Care intervention and are highly critical to residents’ well-being (eg, hospital admissions, need for emergency services and health-related quality of life). Proximal outcomes are variables targeted by the intervention and deemed to mediate its effects on distal outcomes. They include clinical outcomes (eg, falls and fall-related injuries, pressure ulcers category ≥2 and patient-reported symptom burden), outcomes on physical functioning (self-care and/or health behaviour and management), and outcomes on delivery of care in terms of patient-reported experiences and use of potentially inappropriate medication. For the assessment of safety, we consider mortality of residents, other adverse events not captured by distal or proximal outcomes, and increased care needs of residents (care level). Outcomes will be followed up until 6 months post randomisation (figure 2).
Figure 2.
Participant timeline.
Sample size
Sample size is calculated for the purpose of planning a confirmatory trial rather than any confirmatory efficacy analyses (online supplemental file 3, statistical study plan). We expect to achieve a cluster size of 15 residents per NH based on an average NH size of 50 residents, eligibility rate of 60% and participation rate of 50%.15–18 Considering an intracluster correlation coefficient of 0.02119 20 this mean cluster size results in a design factor (inflation factor) of 1.294. Based on empirical results on the annual incidence of hospital admissions among NH residents,16 it is assumed that the proportion of residents with at least one hospital admission in the control group will be 25% (ie, 0.25 rate of hospital admissions) for the 6-month observation period in this study. Furthermore, it is assumed that the Expand-Care programme to be tested in the intervention group can realistically lead to a reduction in the incidence by a maximum of 10%–15% (=0.152 rate of hospital admissions) within the 6-month observation period. The planned sample sizes allow these rates to be estimated with a CI of ±0.119 in the control group and ±0.0985 in the intervention group. This is considered to be sufficient for a precise calculation of the required sample size for subsequent RCTs.
bmjopen-2023-072955supp003.pdf (7MB, pdf)
Initially, 12 NH had consented to participate. One NH declined participation before recruitment of residents had started and we revised the sample size calculation. Now, in total, 11 NH shall be included with at least 15 participating inhabitants for a total of 75 (5×15) and 90 (6×15) individual participants per study arm (165 participants in total). We will not replace institutions or residents lost to follow-up.
Recruitment
We will apply two recruitment strategies for NH: (1) eligible facilities already collaborating with the study centres (Universities) will be invited to participate and (2) public lists of NH in the target regions will be screened and eligible facilities (table 1) invited to participate. Invitations will comprise written material (per post and email) and follow-up phone calls by the research team.
Recruitment of residents will start after NH directors’ written confirmation of participation. Ward nurses will screen residents’ eligibility following the given eligibility criteria. If residents (or their legal guardians, if applicable) have confirmed their willingness to participate, research staff will check eligibility based on information from residents’ charts.
Allocation
NH (unit of randomisation) will be randomised with an allocation ratio of 5:6 to the intervention or control group. Investigators in charge of the respective NH will initiate randomised allocation after completion of baseline assessment (t0). The random sequence will be generated by permutation with validated software.
Registration and randomisation of NH are carried out centrally at the Institut für Medizinische Biometrie und Statistik of the Universitätsklinikum Schleswig-Holstein (UKSH), Campus Lübeck, at the Universität zu Lübeck. This ensures the concealment of allocation until the intervention commences (online supplemental file 3, statistical study plan).
Blinding
Due to the intervention’s nature, blinding of residents and nursing staff against the allocated intervention will not be feasible. Information provided to participants contains no specific hypotheses about possible directions of effects in measured outcomes. Study assistants blinded to allocation will collect distal outcome data (hospitalisation). The trial statistician will be unaware of assignments until after blinded review and data base closure (online supplemental file 3, statistical study plan).
Data collection methods
Baseline assessment
At resident level, we will extract data on age, sex, date of moving into the NH (length of stay), current medical diagnoses and treatment, nomination of legal guardians and existence of agreements for advance care planning from residents’ records.
Additionally, NH directors will provide baseline information about NH characteristics (eg, sponsorship, number of care places, wards, residents, nursing staff capacity, medicotechnical infrastructure and mode of collaboration with external healthcare providers) in a written standardised questionnaire.
Potential benefits and safety outcomes
We will extract data from residents’ record using instruments which have been successfully applied in other studies.20 21 To collect self-reported data, we will conduct standardised interviews with residents and/or proxies (table 3, outcomes and data sources).
Table 3.
Outcomes, measurements and metrics for the evaluation of potential benefits and safety of the expand-care intervention
| Outcome | Specific measurement | Specific metric | Time point | ||
| t0 | t1 | t2 | |||
| Distal outcomes (extracted from residents’ record) | |||||
| Hospital admissions (primary outcome) | No of admissions | Within 3 months | X | X | X |
| No of hospital days | Within 3 months | X | X | X | |
| Reason for admission, initiator, discharge diagnosis | Within 3 months | X | X | X | |
| Out-of-hour physician contacts | No of contacts | Within 3 months | X | X | X |
| No of contacts | Within 3 months | X | X | X | |
| Kind of contacts: telephone, visit to nursing home | Within 3 months | X | X | X | |
| Reason for admission, initiator | Within 3 months | X | X | X | |
| Emergency service use | No of service utilisations | Within 3 months | X | X | X |
| Kind of services used: (emergency) ambulance, emergency control centre, emergency room | Within 3 months | X | X | X | |
| Distal outcomes (self-reported by resident or proxy assessment by nursing staff) | |||||
| Health-related quality of life | EuroQol-5 Dimension-5 Level | At the day of data collection | X | X | |
| Proximal outcomes (data extracted from residents’ records) | |||||
| Falls and fall-related injuries | No of falls and fall-related injuries | Within 3 months | X | X | X |
| Pressure ulcer category ≥2 | No of newly developed pressure ulcers per category | Within 3 months | X | X | X |
| Incontinence-associated dermatitis (IAD) | No of newly developed IAD | Within 3 months | X | X | X |
| Potentially inappropriate medication | Prescribed medication and dosage, evaluated according to PRISCUS criteria | Current medication | X | X | X |
| Contacts with GP | Kind of contact (remote via fax, phone or other electronic form, visit in nursing home or GP office) | Within 3 months | X | X | X |
| Reason for contact, initiator | Within 3 months | X | X | X | |
| Planned versus unplanned | Within 3 months | X | X | X | |
| Proximal outcomes (self-reported by resident) | |||||
| Symptom burden | Four-dimensional Symptom Questionnaire Dimensions: distress, depression, anxiety, somatisation |
Within the last 7 days | X | X | |
| Self-care/health behaviour and management | LTCQ-8, German version | Within the last 4 weeks | X | X | |
| Person-centredness of care | PCQ-P-G, Dimensions: safety climate and everyday living climate | X | X | ||
| Safety outcomes (harms) (data extracted from residents’ records) | |||||
| All-cause mortality | Death (date, reasons) | Within 3 months | X | X | |
| Level of care | Current level of care based on the Nursing Care Insurance Act (Sozialgesetzbuch XI) | Current level | X | X | X |
| Resource use (data extracted from residents’ records) | |||||
| Other healthcare utilisation | FIMA categories of resource use (eg, medical specialists, physiotherapy, occupational therapy, speech therapy, rehabilitation) | Within 3 months | X | X | X |
FIMA, (Fragebogen zur Inanspruchnahme medizinischer und nicht-medizinischer Versorgungsleistungen im Alter) Questionnaire for Health-Related Resource Use in an Elderly; GP, general practitioner; LTCQ-8, Long-Term Conditions Questionnaire Short Form; PCQ-P-G, Person-centred Climate Questionnaire-Patient version; PRISCUS, List of potentially inadequate medication for elderly people.
Distal outcomes
Hospital admissions as primary outcome is defined according to Müller et al.21 For each hospital admission, we will collect information about the kind (elective vs unplanned), initiator, reason, length of stay and discharge diagnoses, similarly for each episode of general practitioner, medical specialists, out-of-hour physician or emergency services utilisation.
Health-related quality of life will be measured using the EQ-5D-5L (EuroQol-5 Dimension-5 Level).22 The EQ-5D-5L measures health-related quality of life on five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. It uses 5-point ordinal scales ranging from 1 (no problems) to 5 (unable to/extreme problems). Dimensions are combined into a 5-digit code that represents the unique health state. This code can be transformed into an index value between 0 and 1 using standard value sets. The EQ-5D-5L contains a Visual Analogue Scale ranging from 0 to 100 (worst to best possible health status).23–25 We will apply German versions of the EQ-5D-5L for self-reported quality of life to all residents with a Dementia Screening Score <4, else, we will perform the EQ-5D-5L proxy instrument with nurses in charge of residents at data collection.20 26
Proximal outcomes
Residents’ records will provide data on falls, fall-related injuries and care activities responding to falls, pressure ulcers and incontinence-associated dermatitis (IAD). Reported fall-related injuries will be categorised as: no injuries, minor injuries, moderate injury, major injuries, death or unclear/not reported.27 For pressure ulcers, we will extract categories at first observation and at data collection as well as successive medical treatments (hospital admission, outpatient surgical treatment) from residents’ records. All record entries classifying observed skin damages as IAD or describing perianal/perigenital skin damages associated with urinary or faecal incontinence and information about progression or healing since first observed will be extracted.
We will document current medication prescriptions (permanent and on-demand) and classify them as potentially inadequate according to the PRISCUS list relevant for the German healthcare system.28
The Four-Dimensional Symptom Questionnaire is a 50-item self-report questionnaire designed to measure common expressions of psychological problems in primary care patients. Items are distributed over four scales: distress, depression, anxiety and somatisation. With a reference period of the last 7 days, it offers a 5-point Likert scale (scored 0 (no); 1 (sometimes) and 2 (regularly, often and very often or constantly)). Corresponding item scores are summed up for scale scores.29 30 Each dimension is interpreted in itself. We will use the cross-culturally validated German version of this instrument.30
We will use the Long-Term Conditions Questionnaire Short-Form (LTCQ-8) to measure self-care comprising health behaviour and management. The LTCQ-8 is an eight-item questionnaire assessing the impact of long-term health conditions on people’s lives and their support needs.31 32 A long-term condition is defined as any health issue that has lasted, or will last, for at least 12 months. It uses a 5-point Likert-scale (never—rarely—sometimes—often—always). Each question is scored with values ranging from 0 to 4 or 4 to 0 (depending on the question’s meaning) to a single composite measure. A higher score indicates a higher health-related quality of life. We will generate a German version of this instrument prior to this trial following the translation and evaluation protocol of the original scale’s authors.
With the German Person-centred Climate Questionnaire-Patient version (PCQ-P-G) we will assess residents’ perception of person-centredness of experienced care delivery.33 34 PCQ-P-G is a 14-item self-report questionnaire measuring person-centredness of care in the dimensions: a climate of safety, a climate of everydayness and a climate of community. It uses a 6-point Likert scale ranging from 1 (no, I totally disagree) to 6 (yes, I totally agree). Items are summated to an overall score and one subscore for each dimension. For this study, we will use only dimension-wise summated items on a climate on safety and a climate of everydayness, as the climate of community is not addressed by the intervention.
Safety outcomes
We will extract residents’ current need of nursing care (care level) based on external assessment of residents’ care needs according to criteria laid down in the Nursing Care Insurance Acts (Sozialgesetzbuch XI). Criteria cover functional impairments (eg, regarding mobility, communication and cognitive abilities), behavioural and psychological well-being, self-care (eg, eating and drinking, personal hygiene, elimination), coping with illnesses and treatment requirements, and social participation. Care levels range from 1 to 5, higher levels indicating larger need of (professional) care support.
NHs continuously record residents’ mortality. In case of death, we will extract information about date, place and reasons of death from residents’ records.
Resource use
We will use the FIMA questionnaire (FIMA: Questionnaire for Health-Related Resource Use in an Elderly) to measure healthcare utilisation (monetary value by standard unit costs).35 36 The FIMA is adapted to the German healthcare system and specialised for elderly populations. It measures utilisation of healthcare providers (eg, hospital stays, outpatient visits to physicians and non-physicians, use of pharmaceuticals or out-of-hour care).
Data management
All resident-related data will be documented with patient identifiers. (Sub)investigators will keep patient identification lists and NH identifiers under lock at the respective study centre, separated from resident data, and data will be archived for 10 years.
Worksheets used for data collection in NH are defined as source data. Source data will be transferred to an electronic case report form, which the (sub)investigator will check and sign digitally.
We will manage data with the study management tool secuTrial®. The database programmer will in cooperation with the responsible biometrician and the documentarists check the study database for errors before use and afterwards release it for use. Data of the worksheets are entered into the secuTrial®-database via input masks. Data will be analysed using SAS V.9.3 or higher. We will implement editing checks in the electronic data capture system and use SAS V.9.3 or higher for manual programming.
A daily complete backup of all data will take place. Correctness of data is checked by further range, validity and consistency checks. Implausible or missing data are queried at the test centre (query management) and corrected or supplemented if necessary. We will document any changes to the data, for example, due to the incorporation of answered queries, in the database via automatic change tracking system (audit trail). A hierarchical access concept based on roles makes unauthorised access to patient data impossible. Anonymity of data within the scope of evaluations is ensured.
We will use the Medical Dictionary for Regulatory Affairs to code database entries on prior diseases, comorbidities, and diagnoses and the anatomical, chemical and therapeutic classification for drugs to code medication. Minimal objective is the first level of those hierarchical classifications.
After final analyses, the data base will be closed and data handed over to the study management for archiving.
Statistical methods
To prepare a confirmatory clinical trial that will be adequately powered, this pilot study will yield two-sided 95% CIs for the 6 months incidence of hospitalisation that extend <10% in either direction. All participants will be analysed by intention to treat. Absorbing endpoints like death are considered as competing risk or worst possible assessment, so that other missing observations may be considered missing at random. The hospitalisation rates in treatment groups are estimated by mixed logistic regression from the occurrence of hospitalisation within 6 months on treatment and occurrence of hospitalisation within 3 months prior to the trial (both fixed factors with two levels) and institution (random effects). The primary treatment effect estimator is the marginal OR in that model fit. The HR from Cox regression and the marginal rate ratio from Poisson regression serve as sensitivity analyses. Proof of mechanism is tested at multiple significance level 0.05 in a Bonferroni-Holm procedure for 16 endpoints of the 9 variables of formal process evaluation (proximal endpoints describing changes in care). All other analyses are adjusted for the respective baseline measurement in mixed models without imputation. Safety, exploratory and subgroup analyses are prespecified in the statistical study plan (online supplemental file 3). The true allocation list will be used only after all analyses will have been coded and the code tested.
Process evaluation
We will conduct an embedded parallel mixed-methods study to examine processes at the cluster level (nursing facilities) and at the individual level (nursing staff, residents) in the participating NH. Data will be evaluated in terms of recruitment, implementation, intervention and maintenance, and context factors.37 Target groups are NH managers, PEPAs, other NH nursing staff, residents and relatives. Written informed consent is a prerequisite for participation in the study. Qualitative methods of data collection are guideline-based semistructured interviews, focus groups and observation or recording of practice supervision, conducted by trained members of the research team at the NH or via telephone (relatives). We will evaluate these data by qualitative content analysis.38 Quantitative methods of data collection are questionnaires, which we will analyse using descriptive statistics. We will triangulate data at the analysis stage on the level of results using joint displays. The process evaluation study design and procedures are outlined in online supplemental file 1.
Health economic analyses
The economic evaluation covers two aspects: (1) analysis of implementation costs and (2) analysis and modelling of incurred healthcare expenditures.
Analysis of implementation costs
Economic analysis will focus on the main implementation strategy, the PEPA training programme. This comprises time expenditures and costs for the programme (eg, lecturer and expert fees), employers’ expenses for time off (release of human capital) and time spent on PEPA training including self-study time. Considering potential government support and funding opportunities, we will develop a preliminary cost figure to estimate implementation costs in case of a positive evaluation of the intervention.
Analysis and modelling of incurred healthcare expenditures
Healthcare expenditure and savings comprise (1) avoidance of empty journeys during ambulance service missions and (2) billable inpatient stays.
We will analyse occurring rescue service interventions (ambulance, emergency ambulance, control centre, transport to the emergency room) regarding projected costs incurred by the service, including initiators, reason for initiation and empty runs.
Reasons for inpatient stays will be derived from patients’ diagnosis and discharge letters. We will, therefore, rate data on usage of medical services monetarily with standardised cost unit rates.
Data monitoring
A qualified Clinical Research Associate (CRA) of the ZKS (centre for clinical studies Lübeck) will conduct risk-based monitoring according to ICH GCP (International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use - Good Clinical Practice) and written SOPs (Standard Operating Procedures) to ensure patients’ rights and safety as well as reliability of trial results. Initiation visits and two regular on-site visits per study centre are planned. Recruitment of residents requires centre initiation by a CRA. Closeout visits will be conducted by telephone. Details of the monitoring, such as key data, will be defined and documented in a monitoring manual. The principal investigator will receive a monitoring report after each visit.
Harms
We will collect comprehensive data on potential harms throughout the trial to allow valid assessment of the intervention’s safety. The research team will continuously supervise and follow-up implementation of the Expand-Care programme to strengthen fidelity. We will discuss any concerns due to unintended changes to care procedures or care outcomes observed and report to the Ethics Committee with a suggestion for amendments to the trial plan, if required.
Patient and public involvement
Representatives of the senior citizens advisory council and of NH resident boards participated in the intervention development. We will capture perspectives of residents, their family/surrogates and NH staff on acceptability and feasibility of the intervention through process evaluation. Results will be presented and discussed at conferences with local healthcare providers and relevant stakeholders. The project’s advisory board comprises representatives for patient and public, nursing science and education, nursing practice and medical law.
Ethics and dissemination
Research ethics approval
This trial adheres to the Declaration of Helsinki in the current version. The ethics committees of the University of Lübeck (Nr. 22-162) and the University Clinic Hamburg-Eppendorf (Nr. 2022-200452-BO-bet) approved the study protocol.
Protocol amendments
Principal investigators and the affected collaborators will consent to any amendments to this protocol before submission to ethics review. Protocol deviations are documented in writing and filed with the coordinating investigator and the trial biostatistician together with the rationale.
Consent or assent
Eligible residents and/or their authorised surrogates will receive written information about objectives and scope of the study from ward nurses. If residents are interested in further information, researchers of the study centres will provide further oral and written information (online supplemental file 4).
bmjopen-2023-072955supp004.pdf (5.8MB, pdf)
Residents will only be enrolled in the trial if they or their authorised surrogates have provided written informed consent. Residents can end participation at any time either orally or in writing, regardless of written confirmation by the surrogate. NH directors will inform the facility’s residents’ board, NH staff and employee representation about the objectives of the trial.
Confidentiality
For this study, we developed a comprehensive data protection concept in collaboration with the data protection official of the University of Lübeck. The concept comprises study information including information on data protection, forms for written informed consent for participants, descriptions of all data processing processes, and measures to protect data and participants rights according to the General Data Protection Regulation (Datenschutzgrundverordnung).
Access to data
The Sponsor (UKSH, nursing research unit) will retain records until 10 years after the publication of the article on the primary endpoint. Anonymised individual patient data used for all analyses reported in the article on the primary endpoint will be made available on reasonable request for medical research purposes in easily machine-readable format.
Dissemination policy
We will publish study results following the CONSORT statement (Consolidated Standards of Reporting Trials) in open-access, peer-reviewed journals and at conferences. A stakeholder advisory board including patient representatives discusses study procedures regularly. Furthermore, we will present results in local networks of relevant healthcare providers.
Trial status
At submission of this manuscript (17 February 2023) the recruitment of residents had been completed, while data collection was ongoing.
First patient in: 26 July 2022.
Last patient out: 13 April 2023.
Supplementary Material
Acknowledgments
We would like to thank all members of the Expand-Care advisory board for their valuable advice and guidance in the development of the intervention and the study design, as well as nursing homes, residents, family, staff, general practitioners and other stakeholders for participation in the intervention development phase.
Footnotes
Twitter: @degampraesident
Contributors: KB, SI, RV, IK, MS and DL developed the study design; RV and IK designed the statistical analysis plan for the study. F-SF and KB designed the economic evaluation. KTS, KB, JS, NJP and DL designed the process evaluation plan. KB, KTS, TAH, NJP and DL developed the intervention. RV and MV (Maren Vens) developed the database and pilot-tested it. KTS, JS, TAH, NJP, MV and DO were responsible for data collection, data entry and controls. Analysis and interpretation of data will be performed by RV, IK, KB, KTS, NJP and DL. KTS, RV and KB drafted the manuscript, all authors contributed to the writing of the report and read, provided important revisions and approved the final version of the manuscript.
Funding: The trial is funded by the German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung) (01GY2003A and 01GY2003B).
Disclaimer: The funding institution will not interfere in any part of the study.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Chadborn NH, Goodman C, Zubair M, et al. Role of comprehensive geriatric assessment in healthcare of older people in UK care homes: realist review. BMJ Open 2019;9:e026921. 10.1136/bmjopen-2018-026921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kiljunen O, Välimäki T, Kankkunen P, et al. Competence for older people nursing in care and nursing homes: an integrative review. Int J Older People Nurs 2017;12. 10.1111/opn.12146 [DOI] [PubMed] [Google Scholar]
- 3.Laging B, Ford R, Bauer M, et al. A meta-synthesis of factors influencing nursing home staff decisions to transfer residents to hospital. J Adv Nurs 2015;71:2224–36. 10.1111/jan.12652 [DOI] [PubMed] [Google Scholar]
- 4.Lemoyne SE, Herbots HH, De Blick D, et al. Appropriateness of transferring nursing home residents to emergency departments: a systematic review. BMC Geriatr 2019;19:17. 10.1186/s12877-019-1028-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ewers M, Lehmann Y. Hochschulisch qualifizierte Pflegende in der Langzeitversorgung?! In: Jacobs K, Kuhlmey A, Greß S, et al., eds. Pflege-Report 2019. Berlin, Heidelberg: Springer, 2020. 10.1007/978-3-662-58935-9 [DOI] [Google Scholar]
- 6.Scott K, McSherry R. Evidence-based nursing: clarifying the concepts for nurses in practice. J Clin Nurs 2009;18:1085–95. 10.1111/j.1365-2702.2008.02588.x [DOI] [PubMed] [Google Scholar]
- 7.American Geriatrics Society Expert Panel on Person-Centered Care . Person-centered care: A definition and essential elements. J Am Geriatr Soc 2016;64:15–8. 10.1111/jgs.13866 [DOI] [PubMed] [Google Scholar]
- 8.Santana MJ, Manalili K, Jolley RJ, et al. How to practice person-centred care: A conceptual framework. Health Expect 2018;21:429–40. 10.1111/hex.12640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bergjan M, Tannen A, Mai T, et al. Einbindung von Pflegefachpersonen mit Hochschulabschlüssen an Deutschen Universitätskliniken: ein Follow-up-Survey. Zeitschrift Für Evidenz, Fortbildung Und Qualität Im Gesundheitswesen 2021;163:47–56. 10.1016/j.zefq.2021.04.001 [DOI] [PubMed] [Google Scholar]
- 10.Baumann A-L, Kugler C. Berufsperspektiven von Absolventinnen und Absolventen grundständig qualifizierender Pflegestudiengänge — Ergebnisse einer bundesweiten Verbleibstudie. Pflege 2019;32:7–16. 10.1024/1012-5302/a000651 [DOI] [PubMed] [Google Scholar]
- 11.Bryant-Lukosius D, Dicenso A. A framework for the introduction and evaluation of advanced practice nursing roles. J Adv Nurs 2004;48:530–40. 10.1111/j.1365-2648.2004.03235.x [DOI] [PubMed] [Google Scholar]
- 12.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Regauer V, Seckler E, Campbell C, et al. German translation and pre-testing of consolidated framework for implementation research (CFIR) and expert recommendations for implementing change (ERIC). Implement Sci Commun 2021;2:120. 10.1186/s43058-021-00222-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:bmj.g1687. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 15.Statistisches Amt für Hamburg und Schleswig-Holstein. Pflegestatistik Schleswig-Holstein 2017. Korrektur. Statistischer Bericht Kennziffer K II 8 - 2J 17 SH (2020). Available: https://www.statistik-nord.de/fileadmin/Dokumente/Statistische_Berichte/arbeit_und_soziales/K_II_8_2j_S/K_II_8_2j17_SH_korr.pdf [Accessed 31 Jul 2020].
- 16.Leutgeb R, Berger SJ, Szecsenyi J, et al. Potentially avoidable hospitalisations of German nursing home patients? A cross-sectional study on utilisation patterns and potential consequences for healthcare. BMJ Open 2019;9:e025269. 10.1136/bmjopen-2018-025269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brucksch A, Hoffmann F, Allers K. Age and sex differences in emergency department visits of nursing home residents: a systematic review. BMC Geriatr 2018;18:151. 10.1186/s12877-018-0848-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saal S, Klingshirn H, Beutner K, et al. Improved participation of older people with joint contractures living in nursing homes: feasibility of study procedures in a cluster-randomised pilot trial. Trials 2019;20:411. 10.1186/s13063-019-3522-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adams G, Gulliford MC, Ukoumunne OC, et al. Patterns of intra-cluster correlation from primary care research to inform study design and analysis. J Clin Epidemiol 2004;57:785–94. 10.1016/j.jclinepi.2003.12.013 [DOI] [PubMed] [Google Scholar]
- 20.Richter C, Berg A, Langner H, et al. Effect of person-centred care on antipsychotic drug use in nursing homes (Epcentcare): a cluster-randomised controlled trial. Age Ageing 2019;48:419–25. 10.1093/ageing/afz016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Müller C, Hesjedal-Streller B, Fleischmann N, et al. Effects of strategies to improve general practitioner-nurse collaboration and communication in regard to hospital admissions of nursing home residents (Interprof ACT): study protocol for a cluster randomised controlled trial. Trials 2020;21:913. 10.1186/s13063-020-04736-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ludwig K, Graf von der Schulenburg J-M, Greiner W. German value set for the EQ-5D-5L. Pharmacoeconomics 2018;36:663–74. 10.1007/s40273-018-0615-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Janssen MF, Pickard AS, Golicki D, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 2013;22:1717–27. 10.1007/s11136-012-0322-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhadhuri A, Kind P, Salari P, et al. Measurement properties of EQ-5D-3L and EQ-5D-5L in recording self-reported health status in older patients with substantial multimorbidity and polypharmacy. Health Qual Life Outcomes 2020;18:317. 10.1186/s12955-020-01564-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marten O, Greiner W. EQ-5D-5L reference values for the German general elderly population. Health Qual Life Outcomes 2021;19:76. 10.1186/s12955-021-01719-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Köhler L, Weyerer S, Schäufele M. Proxy screening tools improve the recognition of dementia in old-age homes: results of a validation study. Age Ageing 2007;36:549–54. 10.1093/ageing/afm108 [DOI] [PubMed] [Google Scholar]
- 27.Zimmermann J, Swora M, Pfaff H, et al. Organizational factors of fall injuries among residents within German nursing homes: secondary analyses of cross-sectional data. Eur J Ageing 2019;16:503–12. 10.1007/s10433-019-00511-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int 2010;107:543–51. 10.3238/arztebl.2010.0543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Terluin B, van Marwijk HWJ, Adèr HJ, et al. The four-dimensional symptom questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry 2006;6:34. 10.1186/1471-244X-6-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Exner A, Kleinstäuber M, Maier W, et al. Cross-cultural validation of the German version of the four-dimensional symptom questionnaire (4DSQ) in multimorbid elderly people. Qual Life Res 2018;27:2691–7. 10.1007/s11136-018-1924-2 [DOI] [PubMed] [Google Scholar]
- 31.Peters M, Potter CM, Kelly L, et al. The long-term conditions questionnaire: conceptual framework and item development. Patient Relat Outcome Meas 2016;7:109–25. 10.2147/PROM.S104552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Batchelder L, Fox D, Potter CM, et al. Rasch analysis of the long-term conditions questionnaire (LTCQ) and development of a short-form (LTCQ-8). Health Qual Life Outcomes 2020;18:375.:375. 10.1186/s12955-020-01626-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Edvardsson D, Koch S, Nay R. Psychometric evaluation of the English language person-centred climate questionnaire—staff version. J Nurs Manag 2010;18:54–60. 10.1111/j.1365-2834.2009.01038.x [DOI] [PubMed] [Google Scholar]
- 34.Dichter MN, Berg A, Hylla J, et al. Evaluation of a multi-component, non-pharmacological intervention to prevent and reduce sleep disturbances in people with dementia living in nursing homes (Monopol-sleep): study protocol for a cluster-randomized exploratory trial. BMC Geriatr 2021;21:40. 10.1186/s12877-020-01997-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bock J-O, Brettschneider C, Seidl H. Ermittlung standardisierter Bewertungssätze aus gesellschaftlicher Perspektive für die gesundheitsökonomische Evaluation [calculation of standardised unit costs from a societal perspective for health economic evaluation]. Gesundheitswesen 2015;77:53–61. 10.1055/s-0034-1374621 Available: http://www.thieme-connect.de/products/ejournals/issue/10.1055/s-005-28452 [DOI] [PubMed] [Google Scholar]
- 36.Seidl H, Bowles D, Bock JO. FIMA-Fragebogen zur Erhebung von Gesundheitsleistungen im Alter: Entwicklung und Pilotstudie [FIMA-questionnaire for health-related resource use in an elderly population: development and pilot study]. Gesundheitswesen 2015;77:46–52. 10.1055/s-0034-1372618 Available: http://www.thieme-connect.de/products/ejournals/issue/10.1055/s-005-28452 [DOI] [PubMed] [Google Scholar]
- 37.Grant A, Treweek S, Dreischulte T, et al. Process evaluations for cluster-randomised trials of complex interventions: a proposed framework for design and reporting. Trials 2013;14:15. 10.1186/1745-6215-14-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuckartz U. Qualitative content analysis. Methods, practice, computer support. Weinheim, Basel: Beltz Juventa, 2012. [Google Scholar]
- 39.Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin e.V. Multimorbidität. S3-Leitlinie. AWMF-Register-Nr. 053-047. Available: awmf.org/leitlinien/detail/ll/053-047.html [Accessed 18 Feb 2022].
- 40.Müskens W, Lübben S. Generic descriptors for informal learning [Generische Deskriptoren für informelles Lernen]. Oldenburg: Carl von Ossietzky Universität Oldenburg, 2018. Available: https://uol.de/fileadmin/user_upload/anrechnungsprojekte/Download/Artikel_Generische_Deskriptoren_GDIL.pdf [accessed Feb 2023]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-072955supp001.pdf (321.5KB, pdf)
bmjopen-2023-072955supp002.pdf (177.5KB, pdf)
bmjopen-2023-072955supp003.pdf (7MB, pdf)
bmjopen-2023-072955supp004.pdf (5.8MB, pdf)