Clinical vignette
A 40-year-old non-smoker male was brought to the hospital due to onset of chest pain at rest 4 h before an electrocardiogram (ECG) was obtained, showing ST-segment elevation in V1–V3 leads and ST-segment depression in the inferior leads (Figure 1). The patient was transferred to the catheterization laboratory where he arrived pain free. A bedside echocardiogram was performed upon arrival, with normal left ventricular ejection fraction and no contractility abnormalities in the left ventricle (LV).
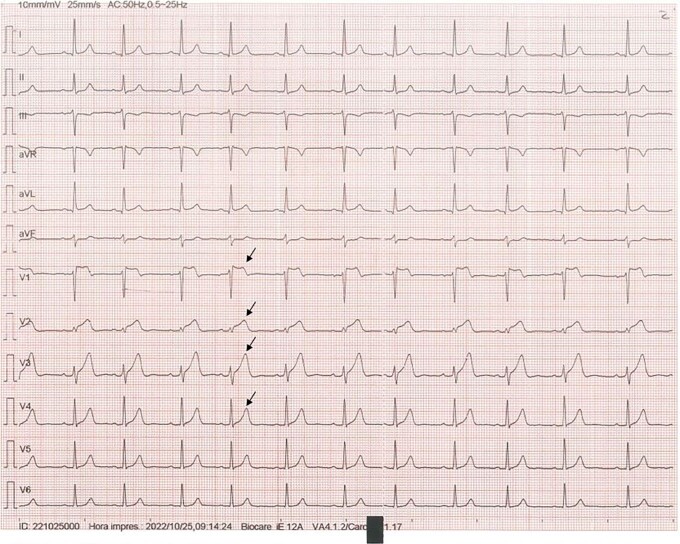
Figure 1.
Admission electrocardiogram. The 12-lead electrocardiogram upon arrival shows normal sinus rhythm at a rate of 72 b.p.m. with anterior ST-segment elevation from V1 to V3 and hyperacute T-waves in V2 and V3 (arrows), associated with a 1 mm ST-segment elevation in leads I and aVL and ST-segment depression in lead III.
The ST-segment elevation from V1 to V3 and hyperacute T-waves in V2 and V3 may suggest a left anterior descending artery occlusion. Nevertheless, the pain ceased soon after nitroglycerin and there were no LV wall motion abnormalities, making the diagnosis unlikely.
The patient underwent an emergent angiogram of the coronary arteries, which at the first glance appeared unobstructed with minor irregularities (see Supplementary material online, Figure S2A and B and Video S1), but a subtle occlusion of the conal artery was depicted (see Supplementary material online, Figure S2C). The high-sensitivity troponin peaked at 10 973 ng/L with an ischaemic curve.
Given the uncertainty of the aetiology, the small size of the occluded vessel, and the absence of pain, a conservative treatment was adopted. A cardiac magnetic resonance (CMR) was performed confirming the presence of oedema and gadolinium enhancement in the upper right ventricular free wall and outflow tract (see Supplementary material online, Figures S3 and S5).
Question 1
Given the electrocardiographic and clinical findings depicted, what is the most likely culprit artery?
Proximal left anterior descending artery
Distal left anterior descending artery
Septal branch of the left anterior descending artery
Conal artery branch of the right coronary artery
Distal portion of the left circumflex artery
Acute occlusion of a conal branch may cause ST-segment elevation in the V1–V3 leads.1
The ST-segment elevation from V1 to V3 and hyperacute T-waves in V2 and V3 may suggest a left anterior descending artery occlusion. Nevertheless, the pain ceased soon after nitroglycerine and there were no left ventricle wall motion abnormalities, making the diagnosis unlikely.
An occlusion of the distal circumflex artery may present with subtle ECG changes, such as ST-segment elevation in leads V5 and V6, I, and/or aVL or ST-segment depression in V1–V3, but it is unlikely to cause anterior ST-segment elevation. A septal branch occlusion usually has ST-segment elevation in V1 and V2 with associated Q-wave and rS in V3, while our case had R-waves in V1–V3 and no septal Q-waves.2
Question 2
What would be the appropriate management strategy for the obstructed vessel in this patient, which had been pain free for more than 4 h before the angiogram was performed?
Provisional stenting technique
Medical treatment
Kissing balloon technique
Double kissing crush technique
Proximal optimization technique
Given the uncertainty of the aetiology, the presumed small size of the occluded vessel as well as being the patient free of pain at that time, a conservative treatment was adopted. A CMR was performed confirming the presence of gadolinium enhancement in the upper right ventricular free wall and outflow tract (see Supplementary material online, Figures S3 and S5).
Question 3
Which one of the following mechanisms was presumably the cause of the conus branch occlusion?
Atherothrombotic
Embolic
Vasospasm
Takotsubo syndrome
Congenital anomaly
A repeated coronary angiogram was scheduled 7 days later (see Supplementary material online, Figure S2D and Video S2) showing a small patent conal branch with no residual obstruction remaining and partial resolution of the ECG changes (see Supplementary material online, Figure S4). This early spontaneous reperfusion of the occluded culprit vessel suggested thromboembolism as the underlying aetiology, but neither atrial fibrillation nor intra-cardiac thrombi were documented during hospital stay. Cardiac magnetic resonance and transoesophageal echocardiogram did not identify a patent foramen ovale. Even though Prinzmetal angina (vasospasm) was included in the differential diagnosis, this was the only episode he has had in his life and has not recurred since the discharge (he was not on nitrates or calcium channel antagonists), making the diagnosis unlikely.
Supplementary Material
Contributor Information
Ravi Vazirani Ballesteros, Cardiovascular Institute-Hospital Clínico San Carlos, Calle Professor Martín Lagos, S/N, 28013 Madrid, Spain.
María Anguita Gámez, Cardiovascular Institute-Hospital Clínico San Carlos, Calle Professor Martín Lagos, S/N, 28013 Madrid, Spain.
Fernando Macaya-Ten, Cardiovascular Institute-Hospital Clínico San Carlos, Calle Professor Martín Lagos, S/N, 28013 Madrid, Spain.
María Vidal Martínez, Cardiovascular Institute-Hospital Clínico San Carlos, Calle Professor Martín Lagos, S/N, 28013 Madrid, Spain.
Ana Viana Tejedor, Cardiovascular Institute-Hospital Clínico San Carlos, Calle Professor Martín Lagos, S/N, 28013 Madrid, Spain.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The patient expressed written consent for the ECG and anonymized clinical case in accordance with COPE guidelines.
Funding: None declared.
Data availability
Data is available on reasonable request.
References
- 1. Lyle M, Van Woerkom RC, Tweet M, Young PM, Best PJM. Conus artery occlusion causing isolated right ventricular outflow tract infarction: novel application of cardiac magnetic resonance in ANTERIOR STEMI. Cardiovasc Diagnosis Ther 2016;6:262–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhong WW, Blue M, Michaels AD. Acute isolated right ventricular infarction: unusual presentation of anterior ST-segment-elevation myocardial infarction. Tex Heart Institute J 2019;46:151–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is available on reasonable request.