Abstract
Background/Aim: Τhe aim of this study was to investigate the possible effect of the Mediterranean diet (Med Diet) on the progression of age-related macular degeneration (AMD) in patients with early or intermediate stages of dry AMD.
Patients and Methods: The present study included 164 patients with early or intermediate dry AMD. Data collected included demographics, anthropometric data, ophthalmic and medical history. AMD progression was evaluated using patients’ optical coherence tomography (OCT) and visual acuity. Using the MedDietScore, sample’s attachment to Med Diet was evaluated, and distinguished into high and low. The association of supplement intake and adherence to Med Diet with AMD progression was investigated using logistic regression.
Results: Sample’s mean age was 73±7.4 years. A positive correlation was found between dietary supplementation and slowing of AMD progression, as well as between high adherence to Med Diet and slowing of AMD progression. In contrast, smokers had 51.4% higher risk of AMD progression (p=0.043). The rate of slowing AMD progression was higher in patients who followed Med Diet and received a dietary supplement, compared to patients who followed one or none of the aforementioned recommendations (p<0.001).
Conclusion: Adherence to the Med Diet could have a positive effect on delaying AMD progression in advanced stages, both in patients receiving or not antioxidants. Therefore, our study proposes to strengthen recommendations to AMD patients to follow a Med Diet.
Keywords: Mediterranean diet, age-related macular degeneration (AMD), dry AMD, dietary supplement, lutein, zeaxanthin
Age-related macular degeneration (AMD) is the leading cause of blindness among individuals over 55 years of age in developed countries. There are two types of AMD: non exudative or dry AMD and neovascular/exudative or wet AMD. Early AMD is characterized by drusen formation and/or pigmentation changes in the retinal pigment epithelium (RPE). Advanced AMD can show as atrophic changes in the macula (geographic atrophy form) or choroidal neovascularization (neovascular AMD) (1). Several studies have shown the protective effect of antioxidant dietary supplements on delaying AMD progression. Supplementation with lutein, zeaxanthin, vitamins C and E, and zinc has been shown to significantly reduce the risk of AMD progression in a dose-response relationship (2,3). This suggests that a diet rich in carotenoids and vitamins could also help the retina from oxidative stress and delay macular degeneration.
The Mediterranean diet (Med Diet) is a plant-based dietary pattern traditionally found in countries of the Mediterranean basin such as Greece, Spain, and Italy. Med diet is considered as one of the healthiest diets, as adherence to this eating pattern reduces general mortality, mortality from cardiovascular disease and cancer, as well as the occurrence of chronic degenerative diseases (4).
Diet is an important consideration in the counseling of patients because unlike other AMD risk factors, such as genetic, age, and sex, it presents a potential opportunity for intervention. However, studies on the effects of dietary patterns on AMD progression are scarce (5). Therefore, to expand current knowledge, in the present study we investigated associations between adherence to Mediterranean dietary pattern and AMD progression.
Patients and Methods
Study population, clinical examination, and definition of progression. A total of 164 Caucasian patients with early or intermediate dry type of AMD were recruited for a period of two years. Recruitment was based on AREDS 2 AMD Classification, in which patients with early AMD have medium sized drusen (63-124 μm) and no pigment abnormalities and patients with intermediate AMD stage have large drusen (≥125 μm) and/or any AMD pigmentary abnormalities. Inclusion criteria were age over 55 years, the presence of drusen (larger than 65μm) in at least one eye without geographic atrophy or neovascularization and the absence of other retinal or macular diseases. Patients with cataract, glaucoma or diabetic retinopathy were excluded. Patients with diabetes or unregulated blood pressure as well as patients with severe systemic disease, such as cancer or autoimmune disease, were also excluded.
At enrollment, patients underwent a complete ophthalmic examination, which included visual acuity measurement using Snellen optotype and macular optical coherence tomography (OCT) using (SD)-OCT Optovue. Information collected included the OCT results and visual acuity measurements of patients one year before enrollment, demographic data, a brief medical history, smoking habits, measurement of weight and height and a complete dietary assessment. Body mass index (BMI) was measured in kg/m2 and patients were divided into three groups: normal weight (BMI=18.0-24.9), overweight (BMI=25.0-29.9), and obese (BMI >30.0) (6). Patients were divided into current smokers and non-smokers (including ex-smokers and never smokers). The brief medical history included history of hypertension, dyslipidemia, and cardiovascular diseases (CVD). All participants were asked about supplement intake and their adherence to Med Diet was assessed using a food-frequency questionnaire (FFQ) and the nutritional index MedDietScore.
AMD progression was evaluated by comparing changes in OCT and visual acuity between patients’ previous and one-year after examination. AMD progression slowed in patients with no change or improvement in visual acuity and without observed anatomical change on OCT. On the other hand, AMD progressed in patients with either deterioration in visual acuity and/ or anatomical change.
All procedures performed in these patients were in accordance with the Ethics Code of the National and Kapodistrian University of Athens (NKUA) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Dietary assessment and evaluation of adherence to Mediterranean diet. Dietary intake during the previous 12 months was assessed by using a semi-quantitative food-frequency questionnaire (FFQ). To evaluate the adherence to Mediterranean diet pattern the MedDietScore was calculated for each participant (7), by considering the consumption of food items from nine food groups, olive oil, and alcohol consumption. The components and the scoring system for calculating MedDietScore are presented in Table I. The range of the MedDietScore is 0-55, with higher values indicating greater adherence to the Med Diet. Patients’ adherence was described as high or low based on the median.
Table I. The range of the Mediterranean diet score (MedDietScore).
The range of the Mediterranean diet score (MedDietScore) is from 0 to 55, with higher values indicating greater adherence to the Mediterranean diet (7).
To evaluate the supplement intake, patients were distinguished into two groups, those who were daily taking nutritional supplement based on AREDS 2 formula (lutein 10 mg, zeaxanthin 2 mg, vitamin C 500 mg, vitamin E 400 IU, zinc oxide 80 mg or 25 mg, and cupric oxide 2 mg) (8) for more than 6 months and the non-takers.
Data analysis. According to AMD progression, patients were classified into two groups: those who maintained or improved their visual acuity and in whom no anatomical change of the retina was observed based on the OCT image, i.e., the progression of the disease was slowed, and those in whom the disease progressed, causing a decrease in visual acuity, and altering the OCT image.
According to dietary habits, patients were divided into four groups depending on receiving the supplement of antioxidants and on their adherence to Med Diet as shown in Table II.
Table II. Groups of participants according to supplement intake and adherence to Med Diet.
Suppl: Supplement; Med Diet: Mediterranean diet.
Statistical analysis. Statistical analysis of data was carried out with the SPSS program (Version 21.0 IBM SPSS STATISTICS, Chicago, IL, USA). Normality was assessed using the Kolmogorov–Smirnov test and graphically through histograms. For continuous variables, the Mann-Whitney U-test or Kruskal-Wallis test have been performed. The Pearson’s chi-squared test and logistic regression models have been used for binary variables. Logistic regression was applied to identify associations between supplement intake and adherence to Med Diet and the likelihood of AMD progression, by estimating the odds ratios (OR). In all analyses, the level of statistical significance was set at p-value<0.05.
Results
Median age of the 164 study participants was 73 and ranged from 55 to 87 years. Additionally, 112 patients (68.3%) were women and 43 (26.2%) were current smokers. The mean BMI was 28.4±3.9 kg/m2 and most of patients (44.5%) were overweight. Dietary supplement was received daily for more than 6 months by 137 patients and high adherence to Med Diet appeared in 82 patients. In Table III, demographic and clinical characteristics of participants according to supplement intake and AMD progression are presented.
Table III. Characteristics of supplement takers and patients with high adherence to Mediterranean diet (Med Diet). Values represent number of patients and the percentage of supplement takers and patients with high adherence.
CVD: Cardiovascular disease; Med Diet: Mediterranean diet.
AMD improvement or stabilization was observed in 94 patients (57.3%). Demographic and clinical characteristics according to AMD progression are shown in Table IV. A statistically significant association was indicated between smoking habits and AMD progression. Current smokers have 51.4% higher risk of AMD progression compared to non-smokers (ex-smokers and never smokers) (OR=0.49; 95%CI=0.24-0.98, p=0.043). A statistically significant positive correlation was found between dietary supplementation and slowing of AMD progression (OR=8.16; 95%CI=2.90-22.91, p<0.001), as well as between high adherence to Med Diet and a decrease in the rate of AMD progression (OR=2.25; 95%CI=1.20-4.23, p=0.012). 67.1% of patients with high adherence to Med Diet and 65.0% of patients who received supplement showed AMD improvement or stabilization.
Table IV. Characteristics of improvers and non-improvers of agerelated macular degeneration (AMD) progression. Values represent number of patients and percentage of improvers and non-improvers.
CVD: Cardiovascular disease; Med Diet: Mediterranean diet. Significant p-values are shown in bold.
Patients were divided into four groups based on supplement intake and adherence to Med Diet. 85.4% of patients with high adherence to MedDietScore (n=70) were taking supplement based on AREDS 2 formula for more than 6 months. 51.1% of patients who were taking supplement showed high adherence to MedDietScore. Table V shows the distribution of various characteristics of the participants between the four groups. Sex, BMI, smoking habits, or any medical condition did not present any significant statistical difference between the groups. On the contrary, AMD progression did present a statistically significant difference, as shown in Figure 1.
Table V. Characteristics of four Groups. Values represent number of patients and percentage of each group.
Suppl: Supplement; CVD: cardiovascular disease.
Figure 1. Percentage of improvers and non-improvers across each group. Each plot shows the percentage of improvers and non-improvers compared with the Low/No supplement (Suppl) group.
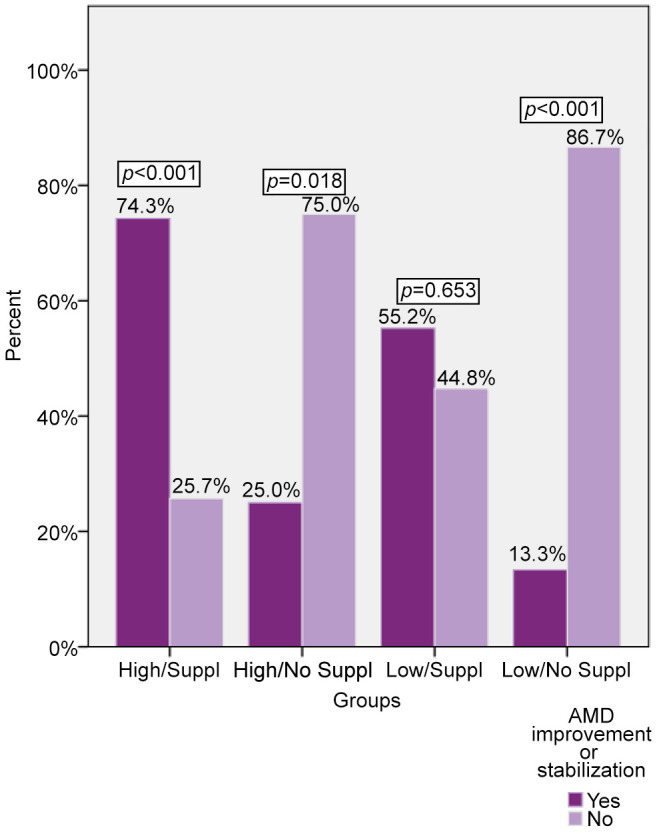
Results of logistic regression are shown in Table VI. Patients who follow a Med Diet pattern and take a daily supplement are more likely to slow AMD progression compared to patients who follow one or neither recommendation.
Table VI. Associations between groups and age-related macular degeneration (AMD) improvement or stabilization. Data represent odds ratio for each group. Reference group: Low/No supplement (Suppl).
*Adjusted for age, sex, BMI, and smoking. Significant p-values are shown in bold.
Discussion
In this cross-sectional study among Greek patients suffering from dry form of AMD in early or intermediate stages, we investigated the relationship between adherence to the Med Diet pattern and AMD progression over the course of a year. We found that greater compliance to Med Diet, as assessed through MedDietScore, was associated with AMD improvement or stabilization (no change in OCT and improvement or no change in visual acuity).
Patients with high adherence to Med Diet had 2.2 times higher likelihood of slowing AMD progression compared to patients with low adherence (p=0.012). Regarding patients who received supplement, they had 8.2 times higher likelihood of slowing AMD progression (p<0.001). It is important to highlight that after adjustment for age, sex, BMI, and smoking habits, patients who follow both recommendations had 24.5 times higher likelihood of slowing AMD progression compared to patients who do not receive any supplement and do not follow Med Diet (p<0.001).
To date, several studies have investigated the relationship between Med diet pattern and AMD progression. Merle et al., collecting data from 2,525 patients of the AREDS study, concluded that high adherence to Med Diet, evaluated with alternate Med Diet (aMeDi) score, decreases to 26% the risk of AMD progression (HR=0.74; 95%CI=0.61-0.91; p-trend=0.007). An important finding in agreement with our findings was that dietary supplements’ intake did not affect the protective effect of the Med Diet on disease progression (9). Retrospective analysis of AREDS and AREDS 2 by Keenan et al., also showed that higher adherence to Med Diet, evaluated with modified aMEDi score was associated with lower odds of AMD progression (10).
In another study by Merle et al., collecting data from the Rotterdam and Alenior studies, concluded that patients who showed greater adherence to the Med Diet pattern according to the MeDi score (Med Diet score) had a 41% lower risk of developing advanced AMD stage, compared to those with a low MeDi score. Studying the two forms of advanced disease separately, high Med Diet adherence was associated with a reduced risk of developing geographic atrophy, whereas the association with the neovascular form did not result in a statistically significant difference (11). In contrast, in the study by Hogg et al., higher adherence to Med diet according to the Med Diet Score (MDS) index decreased the odds of developing the neovascular form of AMD by 48%. The association between Med Diet and AMD progression was not modified by allelic risk for the polymorphism Y402H in the CFH gene. Also, patients with high Med Diet adherence were 20% less likely to have large drusen (≥125 μm) in the RPE compared to those with low adherence (12). More recent studies also showed an inverse association between Mediterranean-style diet and enlargement of drusen (10,13).
Our results have been adjusted for common cofounders that contribute to AMD pathogenesis: age, sex, BMI, and smoking habits (14,15). In our findings, smoking showed a statistically significant association with AMD progression (p=0.043). Smokers are 51.4% less likely to slow AMD progression compared to non-smokers or ex-smokers. According to epidemiological studies, smokers seem to show lower adherence to Med Diet compared to non-smokers and ex-smokers (16). In our study, the majority of smokers (74.4%) showed low adherence to Med Diet, although it was not statistically significant (p=0.859).
As shown in our study, Med diet has a beneficial effect for all patients regardless of supplement intake. Med diet has been characterized as a low glycemic diet with antioxidant and anti-inflammatory effects (17). Med Diet is a plant-based diet that includes daily consumption of a variety of fruits and vegetables. High adherence to Med Diet has been positively associated with dietary intake of lutein and zeaxanthin, as well as adequate serum levels of vitamin C, lutein, zeaxanthin, and β-cryptoxanthin (12). These substances have a proven antioxidant effect and contribute to the health of the retina by enhancing retinal defense to oxidative damage (18).
The dietary pattern of Med Diet also includes rare consumption of red meat, frequent consumption of fish and seafood, low-to-moderate consumption of dairy products, and daily use of olive oil as the primary source of fat (19). As a result, high dietary intake of omega-3 polyunsaturated fatty acids (PUFA) and monounsaturated fatty acids (MUFA), low intake of omega 6 fatty acids, and high ratio of monounsaturated to saturated fatty acids (SFA) have been observed in individuals with high adherence to Med Diet (12). Omega-3 PUFA have proven antithrombotic action and can inhibit neovascularization, unlike SFA that increase oxidative stress in RPE (20). Therefore, patients who follow the Med Diet may delay macular degeneration even if they take supplements of antioxidants, due to avoidance of foods rich in SFA that enhance AMD progression (21).
In our study, the MedDietScore by Panagiotakos et al., was used to evaluate the patients’ adherence to Med Diet. The MedDietScore shows high validity and comparability with other indices of adherence to Med Diet (7,22). The approach of evaluating dietary patterns instead of single food groups or nutrients when studying the effects of diet on diseases, is becoming popular in nutritional epidemiology. Foods and food patterns may act synergistically and influence the risk of several chronic diseases (1). Following a Mediterranean dietary pattern does not only supply the retina with the necessary micronutrients for protection from oxidative stress and neovascularization, but also prevents from adopting eating habits such as a Western diet, that is related with AMD pathogenesis and progression (23,24).
Supplements of antioxidants and zinc have a proven positive effect on slowing AMD progression (2,21,25,26). In our study in 65% of supplement takers AMD progression delayed, while in 85% of non-supplement takers the disease progressed (p<0.001). Patients who received a daily dietary supplement for longer than 6 months were 8.2 times more likely to slow AMD progression compared to those who did not. In many countries such as Greece, antioxidant supplements are not prescribed to patients suffering from AMD and the cost of purchasing them is borne by the patients. As a result, despite ophthalmologists’ recommendations many patients cannot afford buying them (27). Therefore, in patients who cannot afford dietary supplementation, adherence to a Mediterranean dietary pattern may have a positive effect on delaying AMD progression. Our study suggests enhancing the recommendations for adherence to Med Diet to all patients, regardless of supplement intake.
Our study has several limitations. The main limitation of the study stems from its cross-sectional nature, limiting our ability to determine causality. Other limitations are the small sample size and short time of follow-up. In addition, in our analysis, we did not consider the genetic risk of AMD progression, as the sample was not screened for risk alleles or protective polymorphisms. The efficacy of the antioxidants on slowing AMD progression appears to differ by genotype (28,29). However, there are studies that support the beneficial effect of Med Diet in all patients regardless of genetic profile (12).
In summary, adopting a Mediterranean-type diet and complementing it with antioxidant supplement may play an important role in the risk of progression to advanced stages of AMD. Currently there are no efficient treatments for curing dry AMD and preventative measures for delaying its onset. Although further studies are needed, our findings provide further evidence for the potential value of the Mediterranean diet pattern on eye health and may encourage the development and implementation of lifestyle-modifying strategies aimed at reducing the risk of AMD progression.
Conflicts of Interest
The Authors state that they have no conflicts of interest to declare in relation to this study.
Authors’ Contributions
DG and MMM were involved in study concept and design. IG, SS, and MMM contributed to the acquisition of data. DG, KG, and ET analyzed the data. DG wrote the manuscript. MS, DP, and MMM supervised the analysis. MMM critically revised the manuscript. All Authors read and approved the final manuscript.
References
- 1.Gastaldello A, Giampieri F, Quiles J, Navarro-Hortal M, Aparicio S, García Villena E, Tutusaus Pifarre K, De Giuseppe R, Grosso G, Cianciosi D, Forbes-Hernández T, Nabavi S, Battino M. Adherence to the Mediterranean-style eating pattern and macular degeneration: a systematic review of observational studies. Nutrients. 2022;14(10):2028. doi: 10.3390/nu14102028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chew E, Clemons T, Agrón E, Sperduto R, Sangiovanni J, Kurinij N, Davis M, Age-Related Eye Disease Study Research Group Long-term effects of vitamins C and E, β-carotene, and zinc on age-related macular degeneration. Ophthalmology. 2023;120(8):1604–1611.e4. doi: 10.1016/j.ophtha.2013.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu R, Wang T, Zhang B, Qin L, Wu C, Li Q, Ma L. Lutein and zeaxanthin supplementation and association with visual function in age-related macular degeneration. Investigative Ophthalmology & Visual Science. 2017;56(1):252–258. doi: 10.1167/iovs.14-15553. [DOI] [PubMed] [Google Scholar]
- 4.Sofi F, Abbate R, Gensini G, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. The American Journal of Clinical Nutrition. 2023;92(5):1189–1196. doi: 10.3945/ajcn.2010.29673. [DOI] [PubMed] [Google Scholar]
- 5.Hogg R, Woodside J. Mediterranean diet and age-related macular degeneration: is it time to attempt dietary modification. Ophthalmology. 2019;126(3):391–392. doi: 10.1016/j.ophtha.2018.09.032. [DOI] [PubMed] [Google Scholar]
- 6.Weir CB, Jan A. BMI classification percentile and cut off points. StatPearls Publishing Treasure, Treasure Island, FL, USA. 2023 [PubMed] [Google Scholar]
- 7.Panagiotakos D, Milias G, Pitsavos C, Stefanadis C. MedDietScore: A computer program that evaluates the adherence to the Mediterranean dietary pattern and its relation to cardiovascular disease risk. Computer Methods and Programs in Biomedicine. 2019;83(1):73–77. doi: 10.1016/j.cmpb.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Chew E, Clemons T, Sangiovanni J, Danis R, Domalpally A, McBee W, Sperduto R, Ferris F. The age-related eye disease study 2 (AREDS2) Ophthalmology. 2019;119(11):2282–2289. doi: 10.1016/j.ophtha.2012.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Merle B, Silver R, Rosner B, Seddon J. Adherence to a Mediterranean diet, genetic susceptibility, and progression to advanced macular degeneration: a prospective cohort study. The American Journal of Clinical Nutrition. 2023;102(5):1196–1206. doi: 10.3945/ajcn.115.111047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keenan T, Agrón E, Mares J, Clemons T, van Asten F, Swaroop A, Chew E. Adherence to the Mediterranean diet and progression to late age-related macular degeneration in the age-related eye disease studies 1 and 2. Ophthalmology. 2020;127(11):1515–1528. doi: 10.1016/j.ophtha.2020.04.030. [DOI] [PubMed] [Google Scholar]
- 11.Merle BMJ, Colijn JM, Cougnard-Gregoire A, de Koning-Backus APM, Delyfer MN, Kiefte-de Jong JC, Meester-Smoor M, Feart C, Verzijden T, Samieri C, Franco OH, Korobelnik JF, Klaver CCW, Delcourt C, Consortium E-R. Mediterranean diet and incidence of advanced age-related macular degeneration: The eye-risk consortium. Ophthalmology. 2019;126(3):381–390. doi: 10.1016/j.ophtha.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Hogg R, Woodside J, McGrath A, Young I, Vioque J, Chakravarthy U, de Jong P, Rahu M, Seland J, Soubrane G, Tomazzoli L, Topouzis F, Fletcher A. Mediterranean diet score and its association with age-related macular degeneration. Ophthalmology. 2019;124(1):82–89. doi: 10.1016/j.ophtha.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 13.Merle B, Rosner B, Seddon J. Genetic susceptibility, diet quality, and two-step progression in drusen size. Investigative Opthalmology & Visual Science. 2020;61(5):17. doi: 10.1167/iovs.61.5.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mares J. Healthy lifestyles related to subsequent prevalence of age-related macular degeneration. Archives of Ophthalmology. 2016;129(4):470. doi: 10.1001/archophthalmol.2010.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan JS, Wang JJ, Flood V, Mitchell P. Dietary fatty acids and the 10-year incidence of age-related macular degeneration: The blue mountains eye study. Arch Ophthalmol. 2009;127(5):656–665. doi: 10.1001/archophthalmol.2009.76. [DOI] [PubMed] [Google Scholar]
- 16.Eguaras S, Toledo E, Hernandez-Hernandez A, Cervantes S, Martinez-Gonzalez MA. Better adherence to the mediterranean diet could mitigate the adverse consequences of obesity on cardiovascular disease: The sun prospective cohort. Nutrients. 2015;7(11):9154–9162. doi: 10.3390/nu7115457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castro-Quezada I, Roman-Vinas B, Serra-Majem L. The Mediterranean diet and nutritional adequacy: A review. Nutrients. 2014;6(1):231–248. doi: 10.3390/nu6010231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis C, Bryan J, Hodgson J, Murphy K. Definition of the Mediterranean diet; a literature review. Nutrients. 2018;7(11):9139–9153. doi: 10.3390/nu7115459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carneiro A, Andrade JP. Nutritional and lifestyle interventions for age-related macular degeneration: A review. Oxid Med Cell Longev. 2017;2017:6469138. doi: 10.1155/2017/6469138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seddon JM, Cote J, Rosner B. Progression of age-related macular degeneration: Association with dietary fat, transunsaturated fat, nuts, and fish intake. Arch Ophthalmol. 2003;121(12):1728–1737. doi: 10.1001/archopht.121.12.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chew EY, Clemons TE, Sangiovanni JP, Danis RP, Ferris FL 3rd, Elman MJ, Antoszyk AN, Ruby AJ, Orth D, Bressler SB, Fish GE, Hubbard GB, Klein ML, Chandra SR, Blodi BA, Domalpally A, Friberg T, Wong WT, Rosenfeld PJ, Agron E, Toth CA, Bernstein PS, Sperduto RD. Secondary analyses of the effects of lutein/zeaxanthin on age-related macular degeneration progression: Areds2 report no. 3. JAMA Ophthalmol. 2014;132(2):142–149. doi: 10.1001/jamaophthalmol.2013.7376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zaragoza-Marti A, Cabanero-Martinez MJ, Hurtado-Sanchez JA, Laguna-Perez A, Ferrer-Cascales R. Evaluation of Mediterranean diet adherence scores: A systematic review. BMJ Open. 2018;8(2):e019033. doi: 10.1136/bmjopen-2017-019033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chiu CJ, Chang ML, Li T, Gensler G, Taylor A. Visualization of dietary patterns and their associations with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2017;58(3):1404–1410. doi: 10.1167/iovs.16-20454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nunes S, Alves D, Barreto P, Raimundo M, da Luz Cachulo M, Farinha C, Lains I, Rodrigues J, Almeida C, Ribeiro L, Figueira J, Santos L, Silva R. Adherence to a Mediterranean diet and its association with age-related macular degeneration. The coimbra eye study-report 4. Nutrition. 2018;51-52:6–12. doi: 10.1016/j.nut.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 25.Chew EY, Clemons TE, Agron E, Domalpally A, Keenan TDL, Vitale S, Weber C, Smith DC, Christen W. Long-term outcomes of adding lutein/zeaxanthin and omega-3 fatty acids to the areds supplements on age-related macular degeneration progression: Areds2 report 28. JAMA Ophthalmol. 2022;140(7):692–698. doi: 10.1001/jamaophthalmol.2022.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clemons TE, Milton RC, Klein R, Seddon JM, Ferris FL 3rd. Risk factors for the incidence of advanced age-related macular degeneration in the age-related eye disease study (areds) areds report no. 19. Ophthalmology. 2005;112(4):533–539. doi: 10.1016/j.ophtha.2004.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ng W, Goggin M. Awareness of and compliance with recommended dietary supplement among age-related macular degeneration patients. Clinical and Experimental Ophthalmology. 2021;34(1):9–14. doi: 10.1111/j.1442-9071.2006.01141.x. [DOI] [PubMed] [Google Scholar]
- 28.Awh C, Hawken S, Zanke B. Treatment response to antioxidants and zinc based on CFH and ARMS2 genetic risk allele number in the age-related eye disease study. Ophthalmology. 2018;122(1):162–169. doi: 10.1016/j.ophtha.2014.07.049. [DOI] [PubMed] [Google Scholar]
- 29.Gourgouli K, Gourgouli I, Tsaousis G, Spai S, Niskopoulou M, Efthimiopoulos S, Lamnissou K. Investigation of genetic base in the treatment of age-related macular degeneration. International Ophthalmology. 2021;40(4):985–997. doi: 10.1007/s10792-019-01274-7. [DOI] [PubMed] [Google Scholar]








