Abstract
Objective
To appraise research evidence on the effects of balance training on balance and fall efficacy in patients with osteoporosis.
Methods
Six electronic databases were searched from inception of the database to 1 August 2022, with no language restrictions, and randomized controlled trials of balance training in patients with osteoporosis were included in this meta-analysis. Two authors independently screened and reviewed the articles and assessed the methodological quality using the Cochrane risk-of-bias tools. Trial sequential analysis was conducted.
Results
A total of 10 randomized controlled trials with 684 patients were included. Three of the studies that were included had low risk of bias, 5 had moderate risk of bias, and 2 had high risk of bias. A meta-analysis demonstrated that balance training improves dynamic balance measured using the Timed Up and Go Test (mean difference (MD) = –1.86, 95% CI (–2.69, –1.02), Z = 4.38, p < 0.0001) and the Berg Balance Scale (MD = 5.31, 95% CI (0.65, 9.96), Z = 2.23, p < 0.03), static balance measured using One-Leg Standing Time (MD = 4.10, 95% CI (2.19, 6.01), Z = 4.21, p < 0.0001), and fall efficacy measured using the Falls Efficacy Scale International (MD = –4.60, 95% CI (–6.33, –2.87), Z = 5.20, p < 0.00001) were also significantly improved. Trial sequential analysis showed reliable evidence of the effects of balance training on dynamic and static balance improvement. The conclusions of this review are supported by the statistical and clinical significance of all outcomes in the meta-analysis, based on the advised minimal clinically significant differences and minimum detectable changes.
Conclusion
Balance training may be effective in improving balance ability and reducing fear of falling in patients with osteoporosis.
LAY ABSTRACT
Insufficient balance will limit activities and impair physical and mental capabilities, which will increase the risk of falling and reduce quality of life. The study evidence on the effects of balance training in people with osteoporosis is summarized in this paper. The investigations identified 10 related studies that tested the effects of balance training. The data from these trials shows that balancing training can decrease patients’ fear of falling and improve their balancing abilities. For patients and therapists hoping to enhance the effectiveness of rehabilitation, these findings are crucial.
Key words: balance training, osteoporosis, fall efficacy, -systematic review, meta-analysis, trial sequential analysis
Osteoporosis (OP) is the most common bone disease, characterized by a decrease in bone mineral density and an increased risk of fracture (1, 2). OP can affect both females and males of all ages, but is more prevalent in postmenopausal women and older men (2). The World Health Organization (WHO) reports that osteoporosis has emerged as a major global health issue, second only to cardiovascular disease in terms of severity, affecting more than 200 million people globally and continuing to increase (3). Chronic pain, muscular loss, a shorter stature, postural instability, and other clinical indications of osteoporosis cause patients to lose their balance and experience a fear of falling (4, 5). Due to these factors, they avoid routine activities, their physical function deteriorates, and their risk of falling increases and highers the risk of fractures (6, 7). Estimates indicate that 50% of women and 20% of men aged over 50 years will experience an osteoporosis-related fracture.
There is a high correlation between poor balance and falls (8–12). Falls and balance are a major cause of fractures and even mortality in patients with osteoporosis (3, 13). Almost all hip and wrist fractures and approximately 30% of vertebral fractures are caused by poor balance and falls, and they come at a high cost to the healthcare system (14). To decrease these costs, strategies for poor balance and falls are essential. Balance training can increase postural stability, which lowers the risk of falls and reduces the risk of fractures (5, 15–19).
In order to improve postural control and align the body’s centre of gravity with its base of support, balance training is a rehabilitative activity that aims to improve or restore the body’s ability to maintain balance (5, 20, 21). Balance training has proven effective in the older population with positive outcomes (16, 17, 19). Studies on balance training in osteoporosis patients have resulted in a range of conclusions, but there has not been a thorough analysis of these. Therefore, the objective of this study was to review and evaluate the research evidence regarding the effects of balance training on balance and fall efficacy in patients with osteoporosis.
METHODS
The study was performed in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (22) and is reported in keeping with the updated PRISMA 2020 statement (23). This meta-analysis was prospectively registered in PROSPERO (CRD42022350756).
Literature search strategy
Six electronic databases (PubMed, EMBASE, Web of Science, EBSCO, Cochrane Central controlled trial registration, and China National Knowledge Infrastructure) were searched from inception to 1 August 2022, with no language restrictions. The literature was searched using medical subject headings (MeSH) and free terms, including (Osteoporosis OR Osteoporosis, Post-Traumatic OR Osteoporoses OR Osteoporosis, Senile OR Osteoporosis, Age-Related” and “balance training OR balance training programme OR balance exercise). Moreover, the reference lists of included studies were reviewed to identify other potential eligible articles.
Study eligibility criteria
Based on the PICOS framework, the following inclusion criteria were established: P (population): Patients are diagnosed with osteoporosis according to the WHO osteoporosis diagnostic criteria; I (intervention): receive balance training; C (comparison): receive routine medication or activities; O (outcomes): Timed Up and Go Test (TUG), Falls Efficacy Scale International (FES-I), One-Leg Standing Time (OLST), Berg Balance Scale (BBS); S (study design): randomized controlled design. Studies were excluded if the patients presented any of the following criteria: severe orthopaedic conditions other than osteoporosis, eye and internal ear pathologies that could lead to imbalance, vitamin B12 or folate deficiencies, use of any drugs that may affect balance, and uncontrolled hypertension or hypotension. In addition, reviews, meeting summaries, case reports, non--randomized controlled trials, and repetitive articles were excluded
Study selection and data extraction
To manage the data, Endnote X9 (Clarivate Analytics, Philadelphia, Pennsylvania, USA) was used to import all search results. Two researchers independently and concurrently examined the study titles and abstracts and all duplicate papers were deleted. The whole text of each paper was then examined in accordance with the requirements for eligibility, and data extraction was carried out separately. Disagreements were resolved by discussion and consultation with a third researcher.
Two researchers used a prespecified data extraction form to extract the following data from included studies: author, study year, country, sample size, participants’ characteristics (age, sex), details of the intervention and control conditions, duration of intervention, and outcomes. If possible, the authors were emailed to obtain the missing data. The mean and standard deviation (SD) of the outcome measurement and baseline measurement were extracted, and their differences were calculated, in accordance with the Cochrane manual (22).
Quality assessment
Two researchers evaluated the included randomized controlled studies’ methodological quality using the Cochrane Risk-of-Bias Tool (24). Any differences of opinion were settled by consensus, with inclusion of a third researcher. The risk tool includes 7 domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential biases. Each domain was rated as having a low, medium or high risk of bias.
Statistical analysis
RevMan (version 5.4,The Cochrane Collaboration, London, UK) was used to conduct statistical analysis. For continuous variables, the mean difference (MD) or standardized mean difference (SMD) was calculated with corresponding 95% confidence intervals (95% CI), based on whether the outcomes were measured with the same scales. A χ2 test was used for heterogeneity. When the heterogeneity test resulted in p < 0.05 and I² < 50%, the fixed effect model was used for meta-analysis; If p < 0.05 and I² < 50%, the source of heterogeneity was further analysed. After excluding the influence of obvious clinical heterogeneity, the random effect model was used for meta-analysis. RevMan 5.4.1 was used to generate forest plots. If the number of studies in the meta-analysis was 10 or more, Begg’s test, Egger’s test, and a funnel plot were constructed using STATA (version 16.0, Stata Corporation, College Station, TX, USA).
Trial sequential analysis
Meta-analysis with small sample sizes may increase the risk of false-positive (type I error) results, leading to erroneous conclusions (25, 26). To control for this potential risk, trial sequential analysis (TSA) was conducted using TSA (version 0.9.5.10 Beta, Copenhagen Trial Unit, Copenhagen, Denmark) software for outcome indicators. In this study, the probability of type I error was set at α = 0.05, statistical efficacy at 80%, and sample size at the required information size (RIS). If the cumulative Z-value reached the conventional and TSA cut-offs, it suggested that the corrected results were consistent and could be used as definitive evidence. If the Z-curve did not cross any boundary, no definitive conclusion could be drawn.
RESULTS
Study selection
The initial search yielded 864 papers. A total of 406 duplicate papers were removed, and then 434 articles excluded after reading the titles and abstracts. The full texts of the remaining 24 articles were obtained and inspected. A final total of 10 RCTs met the inclusion criteria, and 9 RCTs were selected for meta-analysis. Fig. 1 shows the study selection process.
Fig. 1.
Flow chart of literature screening.
Studies characteristics
The characteristics of the included trials are summarized in Table I. They were conducted between 2007 and 2021 with a total of 684 patients (680 women, 4 men). The main focus of the intervention was balance training, while the specifics of the intervention regimen varied between trials. Firstly, the duration of most of the interventions was 60 min; secondly, there was a variety of intervention modalities in the control group, including conventional medication, health education, aerobic exercise, maintenance of daily activities, and single-task balance training; and finally, the intervention period varied considerably, ranging from 4 weeks to 1 year.
Table I.
Characteristics of the included literature
| Reference | Year | Country | Participants, n | Sex | mean age, years (SD/range) | Intervention | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | EG | CG | EG | CG | |||||||
| Bergland et al. (27) | 2011 | Norway | 89 | 47 | 42 | F | EG, 70.8 ± 5.9 CG, 72.0 ± 5.8 | Balance training with aerobic exercise for 12 months, twice a week, 60 min/day | Warm up, walking forwards, backwards, and sideways while changing direction, avoiding and stepping over obstacles, climbing steps, getting down to and up off the floor, balance training (standing on different types of ground, standing on one leg while doing movements with the other leg, sitting, and reaching out sideways), posture promoting and trunk and chest exercises. | 3-h session of information | TUG |
| Dizdar et al. (28) | 2018 | Turkey | 50 | 25 | 25 | F | EG, 57.87 ± 4.5 CG, 60.91 ± 6.5 | Balance-coordination exercise for 24 weeks, 3 times a week, 60 min/day | Single-leg stance 30 s eyes open/eyes closed, tandem stance, toe walking, heel walking, tandem gait, reciprocal lower extremity movement, half-squatting, bridging, modified Romberg exercise eyes closed on hard/soft ground, edge walking, walking on a balance board, reciprocal leg movements, slowly sitting down-standing up on chair, going up and down stairs) | Aerobic exercise | TUG, BBS |
| FilipoviĆ et al. (29) | 2021 | Serbian | 65 | 33 | 32 | F | EG, 64.40 ± 5.45 CG, 64.20 ± 5.08 | Supervised exercise programme for 12 weeks, twice a week, 15 min/day | Warm-up, rapid walking, a strength training for both large and small muscles, tandem and semi-tandem gait, single-leg stance, toe and heel walking, with and without eyes open, on hard and soft ground. | Received medical treatment | TUG, FES-I, OLST |
| Halvarsson et al. (34) | 2015 | Sweden | 47 | 25 | 26 | F: 50, M: 1 | EG, 76 (66–87) CG, 76 (68–85) | Balance-coordination exercise for 12 weeks, 3 times a week, 45 min/day | Stability limits (changes in base of support during sitting and standing, reaching/leaning), sensory orientation (walking/standing/sitting on uneven surfaces, eyes open/closed), gait (walking at different pace), and postural responses (reactions to balance loss that will occur when the balance is highly challenged). | Live their regular lives | FES-I, OLST |
| Halvarsson et al. (35) | 2016 | Sweden | 41 | 22 | 19 | F | EG, 76 (66–87) CG, 75 (66–84) | Balance-coordination exercise for 12 weeks, 3 times a week, 45 min/day | Stability limits, anticipatory postural adjustments (APA), postural responses, sensory orientation (somatosensory, visual, and vestibular), and stability in gait (dynamic balance) | Live their regular lives | FES-I, OLST |
| Konak et al. (33) | 2016 | Turkey | 42 | 22 | 20 | F: 39, M: 3 | EG, 67.91 ± 12.45 CG, 68.80 ± 10.12 | Balance task exercises and cognitive tasks for 4 weeks, 3 times a week, 45 min/day | Gradually reduce the base of support (2-legged stand, semi-tandem stand, tandem stand, 1-legged stand), dynamic movements to disturb the centre of gravity (tandem walk, circle turns), exercises to stress the postural muscle groups (heel or toe stands) | Balance task exercises for 4-week,3 times a week, 45 min/day | |
| Madureira et al. (30) | 2007 | Philippines | 60 | 30 | 30 | F | EG, 74.57±4.82 CG, 73.40±4.61 | Balance training with aerobic exercise for 12 months, once a week, 60 min/day | Warm-up and stretching exercises, consisting of head rotation, shoulder rotation and stretching of the upper and lower limbs, walking in the tandem position (one foot in front of the other), walking on the tips of the toes and on the heel, walking sideways, walking while raising the leg and the contra-lateral arm, standing on one leg, and standing in the tandem position, while gradually increasing the period of permanence in these last 2 static positions | Received treatment for osteoporosis | TUG, BBS |
| Mikó et al. (31) | 2017 | Hungary | 97 | 49 | 48 | F | EG, 69.33 ± 4.56 CG, 69.10 ± 5.3 | Balance Training Programme (BTP) for 12 months, twice a week in the outpatient setting, exercises 60 min/day based on an exercise booklet individually at home. | BTP compiled by physiotherapists is a combination programme between conventional back, torso and lower extremity muscle strengthening exercises and the proprioceptive dynamic posture training,12 modified in its sensomotory elements in order to improve balance control and reduce falling in the study population. | Received treatment for osteoporosis | TUG, BBS |
| Otero et al. (32) | 2017 | Spain | 65 | 33 | 32 | F | EG, 57.4 ± 4.8 CG, 58.8 ± 4.5 | The physical exercise programme (balance exercises and muscle strengthening exercises) for 6 month, 3 times a week, 60 min/day | Basic warm-up and stretching exercises (10 min): joint mobility exercises, stretching, and walking. Static balance exercises (10 min): exercises varying visual support, gait support, support of upper limbs, participation of lower limbs (arms alongside the body without movement, arms asymmetrically positioned with and without movement, arms symmetrically disposed with and without movement), and exercises involving the vestibular system. Dynamic balance exercises (10 min): exercises involving changes in visual support, the distance and direction of displacement, gait support, pavement, participation of the upper limbs, exercises varying objects which had to be manipulated while walking, and exercises involving the vestibular system. Muscle strengthening exercises (20 min). | Live their regular lives | TUG |
| Stanghelle et al. (36) | 2020 | Norway | 128 | 68 | 60 | F | EG, 74.7 ± 6.1 CG, 73.7 ± 5.6 | Resistance and balance exercise programme 12 weeks, twice a week, -60 min/day | 2 rounds of eight different strength and balance exercises performed in a circuit, with a short warm-up before the circuit and closing with flexibility and stretching. | Live their regular lives | FES-I |
TUG: Timed Up and Go Test; FES-I: Falls Efficacy Scale International; OLST: One-Leg Standing Time; BBS: Berg Balance Scale; EG: experimental group; CG: control group; F: female; M: male; SD: standard deviation.
Risk of bias assessment
After the methodological quality assessment of all 10 included studies (Table II), 6 of the studies described the specific method of randomization grouping, accounting for dropouts or lost participants, while the other 4 studies did not clearly describe the randomization method. Due to the specificity of the implementation of the intervention method, blinding was difficult to implement with participants, and only 3 studies mentioned blinding of participants. For the blinding of outcome assessors, all the studies had a low risk of bias.
Table II.
Risk of bias assessment
| Study Author | Year | Was randomization adequate? (selection bias) | Was allocation concealment adequate? (selection bias) | Were care providers masked? (performance bias) | Were patients masked? (performance bias) | Were outcome assessors masked? (detection bias) | Selective reporting? (reporting bias) | Risk of bias |
|---|---|---|---|---|---|---|---|---|
| Bergland et al. (27) | 2011 | Low | Low | Low | Low | Low | Low | Low |
| Dizdar et al. (28) | 2018 | Low | High | Medium | Medium | Low | Low | Low |
| FilipoviĆ et al. (29) | 2021 | Low | Low | Low | Low | Low | Low | Low |
| Halvarsson et al. (34) | 2015 | Medium | Low | Medium | Medium | Low | Low | Low |
| Halvarsson et al. (35) | 2016 | Medium | Medium | Medium | Medium | Low | Low | Low |
| Konak et al. (33) | 2016 | Medium | Low | Medium | Medium | Low | Low | Low |
| Madureira et al. (30) | 2007 | Medium | Medium | High | Medium | Low | Low | Low |
| Mikó et al. (31) | 2017 | Low | Low | Medium | Medium | Low | Low | Low |
| Otero et al. (32) | 2017 | Low | Medium | Medium | Medium | Low | Low | Low |
| Stanghelle et al. (36) | 2020 | Low | Low | Low | Low | Low | Low | Low |
Meta-analysis results
Dynamic balance measured using Timed Up and Go Test. Six articles (27–32) reported on the effect of balance training on dynamic balance measured using the TUG in patients with osteoporosis, with 407 patients. A random effects model was adopted due to heterogeneity between studies (p < 0.0001, I2 = 82%). Pooled results showed that balance training was effective in improving patients’ dynamic balance compared with controls, with a statistically significant difference (MD = –1.86, 95% CI (–2.69, –1.02), Z = 4.38, p < 0.0001) (Fig. 2). Konak’s study (33) showed that the dual-task (cognitive and balance training) group (Change (95% CI) = –2.81 ± 1.0, p < 0.001) and the single-task (balance training) group (Change (95% CI) = –2.85 ± 0.81, p < 0.001) were both effective in improving patients’ dynamic balance measured using the TUG. Trial sequential analysis showed that (Fig. 3) the RIS was 348 cases and the cumulative Z curve crossed both the monitoring and futility boundaries, and no additional trials were needed to draw firm conclusions.
Fig. 2.
Meta-analysis of Timed Up and Go Test. 95% CI: 95% confidence interval; df: degrees of freedom; I2: measure of heterogeneity; Tau2: measure of variance; SD: standard deviation; IV: inverse variance method.
Fig. 3.
Trial sequence analysis of Timed Up and Go Test. EG: experimental group, CG: control group, RIS: the required information size.
Static balance measured using One-Leg Standing Time. Three articles (29, 34, 35) reported the effect of balance training on static balance measured using the OLST in patients with osteoporosis, with 153 patients. A fixed-effects model was adopted because there was no discernible heterogeneity among the trials (p = 0.33, I2 = 9%). Pooled results showed a statistically significant difference in change in static balance between the balance training trial and control groups (MD = 4.10, 95% CI (2.19, 6.01), Z = 4.21, p < 0.0001) (Fig. 4), significantly improving patients’ static balance. Konak’s study (33) showed that both the dual-task (cognitive and balance training) group (Change (95% CI) = 4.72 ± 0.98, p < 0.001) and the single-task (balance training) group (Change (95% CI) = 4.3 ± 1.21, p < 0.001) were effective in improving static balance measured using the OLST in patients with osteoporosis. Trial sequential analysis showed (Fig. 5) that the RIS was 105 cases, and the cumulative Z curve crossed both the monitoring and futility boundaries, meaning no more trials were needed to draw firm conclusions.
Fig. 4.
Meta-analysis of One-Leg Standing Time. 95% CI: 95% confidence interval; df: degrees of freedom; I2: measure of heterogeneity; Tau2: measure of variance; SD: standard deviation; IV: inverse variance method.
Fig. 5.
Trial sequence analysis of One-Leg Standing Time. EG: experimental group, CG: control group, RIS: the required information size.
Dynamic balance measured using Berg Balance Scale. Three articles (28, 30, 31) reported the effect of balance training on dynamic balance measured using the BBS in patients with osteoporosis, with 207 patients. A random effects model was chosen because it was determined that there was heterogeneity between studies (p < 0.00001, I2 = 94%). Pooled results showed that balance training was effective in improving patients’ dynamic balance measured using the BBS compared with the control group, with a statistically significant difference (MD = 5.31, 95% CI (0.65, 9.96), Z = 2.23, p < 0.03) (Fig. 6). Konak’s study (33) showed that both the dual-task (cognitive and balance training) group (Change (95% CI) = 4.40 ± 0.95, p < 0.001) and the single-task (balance training) group (Change (95% CI) = 3.3 ± 0.47, p < 0.001) were effective in improving dynamic balance measured using the BBS in patients with osteoporosis. The dual-task (cognitive and balance training) group showed better improvement than the single-task (balance training) group (p = 0.007). After inclusion of the second study, the traditional and TSA cut-off values were crossed (Fig. 7), but the Z value was lower than the TSA cut-off value following inclusion of the third study. This indicates that the cumulative process (with positive or negative results) is cumulative across experiments; hence, the Z-values change, and additional trials are required to draw firm conclusions.
Fig. 6.
Meta-analysis of Berg Balance Scale. 95% CI: 95% confidence interval; df: degrees of freedom; I2: measure of heterogeneity; Tau2: measure of variance; SD: standard deviation; IV: inverse variance method.
Fig. 7.
Trial sequence analysis of Berg Balance Scale. EG: experimental group, CG: control group, RIS: the required information size.
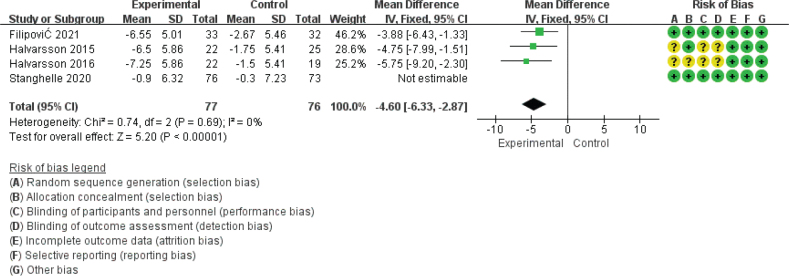
Fall efficacy measured using Falls Efficacy Scale International. Four articles (29, 34–36) reported the effect of balance training on fall efficacy measured using the FES-I in patients with osteoporosis, with 302 patients. A random effects model was adopted due to heterogeneity among the studies (p < 0.03, I2 = 65%). In a statistically significant difference from the control group, the combined data demonstrated that balance training was beneficial in reducing patients’ fear of falling (MD = –3.52, 95% CI (–5.89, –1.14), Z = 2.90, p < 0.004). Because Stanghelle’s study participants had fracture experience, sensitivity analysis was conducted. When Stanghelle’s study (36) was deleted, I2 decreased from 65% to 0%. When comparing the 2 groups, the difference remained statistically significant (MD = –4.60, 95% CI (–6.33, –2.87), Z = 5.20, p < 0.00001) (Fig. 8). Trial sequential analysis showed (Fig. 9) that the RIS was 377 cases and the cumulative Z curve crossed the monitoring and futility boundaries, but did not reach the required sample size.
Fig. 8.
Meta-analysis of Falls Efficacy Scale International. 95% CI: 95% confidence interval; df: degrees of freedom; I2: measure of heterogeneity; Tau2: measure of variance; SD: standard deviation; IV: inverse variance method.
Fig. 9.
Trial sequence analysis of Falls Efficacy Scale International. EG: experimental group, CG: control group, RIS: the required information size.
Subgroup analysis and publication bias
To explore potential sources of heterogeneity, subgroup analyses were performed according to intervention duration. Included studies evaluated the effects of short-term (3 months, n = 4), medium-term (6 months, n = 2), and long-term (12 months, n = 3) balance training on dynamic balance measured using the TUG in patients with osteoporosis. Subgroup analysis showed that both the short-term group (MD = –1.31, 95% CI (–2.03, –0.58), Z = 3.52, p = 0.0004, I2 = 55%) and the long-term group (MD = –2.80, 95% CI (–5.07, –0.53), Z = 2.42, p = 0.02, I2 = 89%) showed that balance -training intervention was effective in improving dynamic balance measured using the TUG in patients with osteoporosis. The results of the intermediate group (MD = –1.28, 95% CI (–2.66, 0.11), Z = 1.81, p = 0.07, I2 = 90%) showed similar improvement in dynamic balance measured using the TUG between the test and control patients. The difference between the 3 subgroups was not statistically significant (p = 0.52).
Subgroup analysis was performed on the studies reporting the effect of balance training on dynamic balance measured using the BBS in patients with osteoporosis. The results of the subgroup analysis showed that the short-term group (3 months, n = 2) (MD = 2.37, 95% CI (0.24, 4.51), Z = 2.18, p = 0.03, I2 = 43%) and the long-term group (12 months, n = 2) (MD = 7.55, 95% CI (5.16, 9.94), Z = 6.19, p = 0.00001, I2 = 60%) indicated that the balance training intervention was effective in improving dynamic balance measured using the BBS in patients with osteoporosis. The difference between the 2 subgroups was statistically significant (p = 0.006).
The inverted funnel plot analysis test and Egger’s test’s minimum literature size requirements were not met by the amount of literature included in the meta-analysis of this study; hence it was not possible to determine whether there was publication bias.
DISCUSSION
Main finding
The aim of this study was to investigate the effects of balance training on static and dynamic balance and fall efficacy in patients with osteoporosis. The study’s findings showed that both dynamic and static balance abilities (TUG, OLST, and BBS) improved significantly after balance training. In addition, patients with osteoporosis who received balance training indicated significantly less fear of falling.
To compensate for the concern that this analysis only evaluates statistical, and not clinical, significance, the literature was evaluated regarding the statistical and clinical significance of all outcomes in a meta-analysis based on the recommended minimum clinically significant differences and minimum detectable changes. For TUG (37), a minimally clinically important difference (in s), ranging from 0.9 to 3.0 s, has been reported in patients with lumbar degenerative disc disease (DDD). Our calculated point estimate for this measure (MD = –1.86, 95% CI (–2.69, –1.02)) falls within this range. For the BBS (38), a minimally clinically important difference in score, ranging from 2 to 3 points, has been reported in patients with multiple sclerosis. Our calculated point estimate for this measure (MD = 5.31, 95% CI (0.65, 9.96)) is higher than this range. For the OLST (39), 1 s longer OLST between 0 and 30 s resulted in a 5% lower age-adjusted risk of a hip fracture. In this review, after balance training, participants increased their OLST time by 4.1 s. For FES-I (21, 40), our calculated point estimate (MD = –4.60, 95% CI (–6.33, –2.87)) was below the reported minimally clinically important difference values (3.5 s). The information listed above serves to support the findings of this review. However, osteoporosis patients are not included in the study population linked to the minimal clinically meaningful difference and the minimum detectable change in TUG and BBS; therefore, caution should be used when interpreting the relevant results.
Comparison with previous studies
According to a previous meta-analysis (41), balancing training may play a significant part in lowering the likelihood of falls in individuals with osteoporosis. While there are certain findings that are consistent with the prior meta-analysis, it is important to highlight that the current investigation focused on examining changes in balance and fall efficacy. First, compared with the last meta-analysis, a number of new studies were included in the current meta-analysis. The current meta-analysis generally further reinforced or validated the earlier findings of the prior meta-analysis as a result of the larger combined sample size. Secondly, we conducted a subgroup analysis of intervention duration. Subgroup analysis shows that balance training may be effective in improving dynamic balance in the short term and long term. However, the results of subgroup analysis should be interpreted cautiously due to the limited amount of research included in the analysis. Finally, trial sequential analysis, a novel statistical technique, was used to assess whether the cumulative data were sufficiently informative. Trial sequence analysis indicates that additional trials are necessary before conclusive statements on body balance function and fall efficacy can be made.
An individual’s balance is a complex multidimensional concept related to postural control, which essentially refers to the ability to maintain posture (e.g. sitting or standing), to move between postures, and to not fall when responding to external disturbances (5, 17). In recent decades, studies have shown that 20% of fracture patients have osteoporosis, while 98% of low-energy fractures are caused by falls (42, 43). In addition, balance and strength training can help prevent two-thirds of falls and even fatalities (44). According to a systematic review (45), balance training is the most beneficial exercise for enhancing balance, and the secondary exercise was power. For the target population, balance training focuses on both dynamic and static balance. By enhancing dynamic and static balance, people can gain control over their posture, enhance coordinated movement of their upper and lower limbs, improve mobility, walking ability and stability, and prevent falls (46). The current study found that the experimental group with balance training had better posture control, which is consistent with the results of Eftekharsadat (47). Falls have just as serious psychological effects as they do physical ones (48). Fall efficacy is a crucial sign of a subject’s self-assurance in fall prevention, which is mostly manifested as a fear of falling (49, 50). Some osteoporosis patients experience chronic pain and fear of falling, and they are psychologically resistant to activity and exercise for fear of physical harm (51–54). As a result, balance, physical function, and even daily activity decrease, which further accelerates calcium loss and causes adverse effects. This study demonstrates how balance training can successfully reduce patients’ fear of falling and encourage active participation in activities and exercises, thereby easing daily activities and enhancing quality of life.
Implications for clinical practice
The current study demonstrates that balance training can help osteoporosis patients with their balance and fear of falling. However, some issues remain. First, only a small percentage of the study participants were men; most were osteoporotic women. Postmenopausal women are undoubtedly more at risk of osteoporosis, but there is a dearth of data from male patients. Further research is necessary to determine whether the results of this study are directly applicable to patients who are men. Furthermore, trial sequential analysis (TSA) confirms the efficacy of balance training, but further research is needed to draw definitive conclusions about fall prevention and body balance. Finally, there is insufficient evidence on the optimal duration and frequency of intervention cycles and the effect on the number of falls occurring. Only 2 studies (30, 31) included data on falls (Madureira (–0.77 ± 1.76 vs + 0.03 ± 0.98, p = 0.018); Mikó, p < 0.05). The large Cochrane Review conducted by Sherington indicates that balance and functional exercises are effective in preventing falls in older people (16). In addition, it is advised that orthopaedic outpatient healthcare providers encourage balance training in osteoporosis patients who have just received a diagnosis and who receive regular checkups in order to enhance their balance, reduce their fear of falling, increase their body control, and decrease the likelihood of falling. If conditions permit, patients who are about to be discharged from the hospital are assessed for balance and fall efficacy, and health education as well as different levels of balance training are implemented based on the assessment results. When performing community nursing duties, community nursing staff can create specialized balance training programmes to meet the needs of various groups, regularly exchange experience and feedback, increase patient training compliance, and enhance the balance and walking ability of elderly residents as well as patients with osteoporosis through long-term balance training. While the trial follow-up included in the study ranged from 4 to 48 weeks, a balance training programme to avoid falls may also have long-term advantages. It is important to note that the majority of training programmes span 12 weeks or more.
Strengths and limitations
The strength of this meta-analysis lies in its compliance with the PRISMA statement and registration on PROSPERO with protocol. This study has some limitations. First, there volume of literature is limited. Secondly, although exact exercise protocols were available for each study, confounding factors were inevitable. Furthermore, there is a lot of heterogeneity in the research; thus it is important to evaluate the results carefully. Finally, the methodological flaws in the test itself and the bias of the outcome report cannot be overcome by trial sequential analysis (TSA).
CONCLUSION
This study indicates that balance training can help individuals with osteoporosis reduce their fear of falling and enhance their dynamic and static balance. According to the trial sequential analysis findings, additional research is required to confirm dynamic balance, as measured using the BBS, and fear of falling, as measured using the FES-I.
ACKNOWLEDGEMENTS
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Svedbom A, Hernlund E, Ivergard M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 2013; 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy . Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001 Feb 14; 285(6): 785–95. doi: 10.1001/jama.285.6.785. PMID: . [DOI] [PubMed] [Google Scholar]
- 3.Cauley JA. Public health impact of osteoporosis. J Gerontol Biol Sci Med Sci 2013; 68: 1243–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Järvinen TL, Sievänen H, Khan KM, Heinonen A, Kannus P. Shifting the focus in fracture prevention from osteoporosis to falls. BMJ 2008; 336: 124–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsu W-L, Chen C-Y, Tsauo J-Y, Yang R-S. Balance control in elderly people with osteoporosis. J Formos Med Assoc 2014; 113: 334–339. [DOI] [PubMed] [Google Scholar]
- 6.Reelick MF, van Iersel MB, Kessels RP, Rikkert MGO. The influence of fear of falling on gait and balance in older people. Age Ageing 2009; 38: 435–440. [DOI] [PubMed] [Google Scholar]
- 7.Gomes GA, Cintra FA, Batista FS, Neri AL, Guariento ME, Sousa Mda L, et al. Elderly outpatient profile and predictors of falls. Sao Paulo Med J 2013; 131: 13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silsupadol P, Siu KC, Shumway-Cook A, Woollacott MH. Training of balance under single- and dual-task conditions in older adults with balance impairment. Phys Ther 2006; 86: 269–281. [PubMed] [Google Scholar]
- 9.Overstall PW, Exton-Smith AN, Imms FJ, Johnson AL. Falls in the elderly related to postural imbalance. BMJ 1977; 1: 261–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nelson RC, Amin MA. Falls in the elderly. Emerg Med Clin North Am 1990; 8: 309–324. [PubMed] [Google Scholar]
- 11.Johansson J, Nordström A, Gustafson Y, Westling G, Nordström P. Increased postural sway during quiet stance as a risk factor for prospective falls in community-dwelling elderly individuals. Age Ageing 2017; 46: 964–970. [DOI] [PubMed] [Google Scholar]
- 12.Landers MR, Oscar S, Sasaoka J, Vaughn K. Balance confidence and fear of falling avoidance behavior are most predictive of falling in older adults: prospective analysis. Phys Ther 2016; 96: 433–442. [DOI] [PubMed] [Google Scholar]
- 13.Da Silva RB, Costa-Paiva L, Morais SS, Mezzalira R, Ferreira NDO, Pinto-Neto AM. Predictors of falls in women with and without osteoporosis. J Orthopaed Sports Phys Ther 2010; 40: 582–588. [DOI] [PubMed] [Google Scholar]
- 14.Parkkari J, Kannus P, Palvanen M, Natri A, Vainio J, Aho H, et al. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int 1999; 65: 183–187. [DOI] [PubMed] [Google Scholar]
- 15.Close JC, Glucksman E. Falls in the elderly: what can be done? Med J Austral 2000; 173: 176–177. [DOI] [PubMed] [Google Scholar]
- 16.Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Systemat Rev 2019; 1: Cd012424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sörlén N, Hult A, Nordström P, Nordström A, Johansson J. Short-term balance training and acute effects on postural sway in balance-deficient older adults: a randomized controlled trial. BMC Sports Sci Med Rehabil 2021; 13: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gibbs JC, MacIntyre NJ, Ponzano M, Templeton JA, Thabane L, Papaioannou A, et al. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Systemat Rev 2019; 7: Cd008618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steadman J, Donaldson N, Kalra L. A randomized controlled trial of an enhanced balance training program to improve mobility and reduce falls in elderly patients. J Amer Geriatr Soc 2003; 51: 847–852. [DOI] [PubMed] [Google Scholar]
- 20.Chodzko-Zajko WJ, Proctor DN, Singh MAF, Minson CT, Nigg CR, Salem GJ, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc 2009; 41: 1510–1530. [DOI] [PubMed] [Google Scholar]
- 21.Gusi N, Carmelo Adsuar J, Corzo H, del Pozo-Cruz B, Olivares PR, Parraca JA. Balance training reduces fear of falling and improves dynamic balance and isometric strength in institutionalised older people: a randomised trial. J Physiother 2012; 58: 97–104. [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons, 2019. [Google Scholar]
- 23.Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021; 372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brok J, Thorlund K, Gluud C, Wetterslev J. Trial sequential analysis reveals insufficient information size and potentially false positive results in many meta-analyses. J Clin Epidemiol 2008; 61: 763–769. [DOI] [PubMed] [Google Scholar]
- 26.Thorlund K, Devereaux PJ, Wetterslev J, Guyatt G, Ioannidis JP, Thabane L, et al. Can trial sequential monitoring boundaries reduce spurious inferences from meta-analyses? Int J Epidemiol 2009; 38: 276–286. [DOI] [PubMed] [Google Scholar]
- 27.Bergland A, Thorsen H, Kåresen R. Effect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomized, controlled trial. Osteoporos Int 2011; 22: 1863–1871. [DOI] [PubMed] [Google Scholar]
- 28.Dizdar M, Irdesel JF, Dizdar OS, Topsac M. Effects of balance-coordination, strengthening, and aerobic exercises to prevent falls in postmenopausal patients with osteoporosis: a 6-month randomized parallel prospective study. J Aging Phys Activ 2018; 26: 41–51. [DOI] [PubMed] [Google Scholar]
- 29.FilipoviĆ TN, LazoviĆ MP, BackoviĆ AN, FilipoviĆ AN, IgnjatoviĆ AM, DimitrijeviĆ SS, et al. A 12-week exercise program improves functional status in postmenopausal osteoporotic women: randomized controlled study. Eur J Phys Rehabil Med 2021; 57: 120–130. [DOI] [PubMed] [Google Scholar]
- 30.Madureira MM, Takayama L, Gallinaro AL, Caparbo VF, Costa RA, Pereira RMR. Balance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: a randomized controlled trial. Osteoporos Int 2007; 18: 419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mikó I, Szerb I, Szerb A, Poor G. Effectiveness of balance training programme in reducing the frequency of falling in established osteoporotic women: a randomized controlled trial. Clin Rehabil 2017; 31: 217–224. [DOI] [PubMed] [Google Scholar]
- 32.Otero M, Esain I, González-Suarez Á M, Gil SM. The effectiveness of a basic exercise intervention to improve strength and balance in women with osteoporosis. Clin Intervent Aging 2017; 12: 505–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Konak HE, Kibar S, Ergin ES. The effect of single-task and dual-task balance exercise programs on balance performance in adults with osteoporosis: a randomized controlled preliminary trial. Osteoporos Int 2016; 27: 3271–3278. [DOI] [PubMed] [Google Scholar]
- 34.Halvarsson A, Franzén E, Ståhle A. Balance training with multi-task exercises improves fall-related self-efficacy, gait, balance performance and physical function in older adults with osteoporosis: a randomized controlled trial. Clin Rehabil 2015; 29: 365–375. [DOI] [PubMed] [Google Scholar]
- 35.Halvarsson A, Oddsson L, Franzén E, Ståhle A. Long-term effects of a progressive and specific balance-training programme with multi-task exercises for older adults with osteoporosis: a randomized controlled study. Clin Rehabil 2016; 30: 1049–1059. [DOI] [PubMed] [Google Scholar]
- 36.Stanghelle B, Bentzen H, Giangregorio L, Pripp AH, Skelton DA, Bergland A. Physical fitness in older women with osteoporosis and vertebral fracture after a resistance and balance exercise programme: 3-month post-intervention follow-up of a randomised controlled trial. BMC Musculoskel Dis 2020; 21: 471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maldaner N, Sosnova M, Ziga M, Zeitlberger AM, Bozinov O, Gautschi OP, et al. External validation of the minimum clinically important difference in the timed-up-and-go test after surgery for lumbar degenerative disc disease. Spine 2022; 47: 337–342. [DOI] [PubMed] [Google Scholar]
- 38.Gervasoni E, Jonsdottir J, Montesano A, cattaneo d. minimal clinically important difference of berg balance scale in people with multiple sclerosis. Arch Phys Med Rehabil 2017; 98: 337–340.e332. [DOI] [PubMed] [Google Scholar]
- 39.Lundin H, Sääf M, Strender LE, Nyren S, Johansson SE, Salminen H. One-leg standing time and hip-fracture prediction. Osteoporos Int 2014; 25: 1305–1311. [DOI] [PubMed] [Google Scholar]
- 40.Monjezi S, Negahban H, Tajali S, Mofateh R, Molhemi F, Mostafaee N. Psychometric properties of the Persian-version of the Activities-specific Balance Confidence scale and Fall Efficacy Scale-International in Iranian patients with multiple sclerosis. Physiother Theory Pract 2021; 37: 935–944. [DOI] [PubMed] [Google Scholar]
- 41.Zhou X, Deng H, Shen X, Lei Q. Effect of balance training on falls in patients with osteoporosis: a systematic review and meta-analysis. J Rehabil Med 2018; 50: 577–581. [DOI] [PubMed] [Google Scholar]
- 42.Parkkari J, Heikkilä J, Kannus IP. Acceptability and compliance with wearing energy-shunting hip protectors: a 6-month prospective follow-up in a Finnish nursing home. Age Ageing 1998; 27: 225–229. [DOI] [PubMed] [Google Scholar]
- 43.Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone 2004; 35: 375–382. [DOI] [PubMed] [Google Scholar]
- 44.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006; 35 Suppl 2: ii37–ii41. [DOI] [PubMed] [Google Scholar]
- 45.Kim Y, Vakula MN, Bolton DAE, Dakin CJ, Thompson BJ, Slocum TA, et al. Which exercise interventions can most effectively improve reactive balance in older adults? a systematic review and network meta-analysis. Frontiers Aging Neurosci 2021; 13: 764826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jehu DA, Paquet N, Lajoie Y. Balance and mobility training with or without concurrent cognitive training improves the Timed Up and Go (TUG), TUG cognitive, and TUG manual in healthy older adults: an exploratory study. Aging Clin Exper Res 2017; 29: 711–720. [DOI] [PubMed] [Google Scholar]
- 47.Eftekharsadat B, Babaei-Ghazani A, Mohammadzadeh M, Talebi M, Eslamian F, Azari E. Effect of virtual reality-based balance training in multiple sclerosis. Neurolog Res 2015; 37: 539–544. [DOI] [PubMed] [Google Scholar]
- 48.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol 1990; 45: P239–243. [DOI] [PubMed] [Google Scholar]
- 49.Wang C, Goel R, Rahemi H, Zhang Q, Lepow B, Najafi B. Effectiveness of daily use of bilateral custom-made ankle-foot orthoses on balance, fear of falling, and physical activity in older adults: a randomized controlled trial. Gerontol 2019; 65: 299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang R, Pepper GA. Is fall self-efficacy an independent predictor of recurrent fall events in older adults? Evidence from a 1-year prospective study. J Res Nurs Health 2020; 43: 602–609. [DOI] [PubMed] [Google Scholar]
- 51.Halvarsson A, Franzén E, Ståhle A. Assessing the relative and absolute reliability of the Falls Efficacy Scale-International questionnaire in elderly individuals with increased fall risk and the questionnaire’s convergent validity in elderly women with osteoporosis. Osteoporos intl 2013; 24: 1853–1858. [DOI] [PubMed] [Google Scholar]
- 52.Hübscher M, Vogt L, Schmidt K, Fink M, Banzer W. Perceived pain, fear of falling and physical function in women with osteoporosis. Gait Posture 2010; 32: 383–385. [DOI] [PubMed] [Google Scholar]
- 53.Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008; 37: 19–24. [DOI] [PubMed] [Google Scholar]
- 54.Halvarsson A, Ståhle A, Halén C, Roaldsen KS. “Better safe than sorry”: a qualitative content analysis of participant’s perspectives of fall-related concerns and balance in older women with osteoporosis after balance training. Disabil Rehabil 2016; 38: 796–802. [DOI] [PubMed] [Google Scholar]