Abstract
Background
The objective to assess the outcomes from different palliative radiotherapy (RT) schedules in incurable head and neck cancer (HNC), to evaluate if there is a relationship between RT dose, technique, and fractionation with tumor response in contrast to the occurrence of adverse effects.
Materials and methods
Eligible studies were identified on Medline, Embase, the Cochrane Library, and annual meetings proceedings through June 2020. Following PRISMA and MOOSE guidelines, a cumulative meta-analysis of studies for overall response rate (ORR), overall survival (OS), progression-free survival (PFS), pain/dysphagia relief, and toxicity was performed. A meta-regression analysis was done to assess if there is a connection between RT dose, schedule, and technique with ORR.
Results
Twenty-eight studies with 1,986 patients treated with palliative RT due to incurable HNC were included. The median OS was 6.5 months [95% confidence interval (CI): 5.6–7.4], and PFS was 3.6 months (95% CI: 2.7–4.3). The ORR, pain and dysphagia relief rates were 72% (95% CI: 0.6–0.8), 83% (95% CI: 52–100%), and 75% (95% CI: 52–100%), respectively. Conventional radiotherapy (2D-RT) or conformational radiotherapy (3D-RT) use were significantly associated with a higher acute toxicity rate (grade ≥ 3) than intensity-modulated radiation therapy (IMRT) or stereotactic body radiation therapy (SBRT). On meta-regression analyses, the total biological effective doses (BED) of RT (p = 0.001), BED > 60 Gy10 (p = 0.001), short course (p = 0.01) and SBRT (p = 0.02) were associated with a superior ORR.
Conclusions
Palliative RT achieves tumor response and symptom relief in incurable HNC patients. Short course RT of BED > 60 Gy using IMRT could improve its therapeutic ratio. SBRT should be considered when available.
Keywords: head and neck cancer, radiotherapy, palliative treatment, palliative radiotherapy, meta-analysis
Introduction
Globally, head and neck squamous cell carcinoma (HNSCC) is the seventh most common cancer, resulting in about 300,000 deaths per year [1]. At diagnosis, many patients are unsuitable for curative treatment due to advanced loco-regional disease, the presence of significant comorbidities, and poor performance status [2, 3]. Patients with advanced HNSCC without curative treatment have a shortened survival rate [4–6]. Nevertheless, even without radical therapy and with a reduced survival rate, these patients still require some type of therapy to control their loco-regional disease, to mitigate pain, bleeding, dysphagia, and other local symptoms [7, 8].
Palliative radiotherapy (RT) is a frequently used modality to relieve local symptoms from locally advanced head and neck cancer (HNC) [7, 9]. However, there is a scarcity of randomized controlled trials to guide the choice of the optimal fractionation and the optimal radiation dose for these patients [9]. An ideal palliative RT course should be capable of producing significant tumor regression, symptom control within a short treatment time, and with minimal side effects and preservation of quality of life [10, 11].
Recently, Grewal et al. published a critical review demonstrating a lack of standardization in terms of dose per fraction, treatment technique, overall treatment time, and biologically effective dose (BED) for choosing a palliative RT schedule [9]. In this systematic review, no significant advantage among conventional, short, or cycled fractionated RT was observed, and doubts remain whether there is a relationship between radiation dose and tumor or symptom control [9]. Moreover, another previous review article also reported a wide variety in the dose in palliative RT courses [10]. In general, palliative RT was effective with low toxicity rates; in contrast, there was an increase in side effects in studies with higher RT doses [12]. These conflicting results from numerous RT fractionations employed in clinical practice highlight the need to investigate if there is an optimal RT scheme.
This meta-analysis is intended to assess the outcomes from different palliative RT schedules for incurable HNC evaluating if there is a relationship among BED, RT technique, and RT schedule with tumor or symptom control.
Material and methods
We conducted this systematic review and meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement and the Meta-analyses of Observational Studies in Epidemiology (MOOSE) guideline [13, 14]. Two reviewers (GAV, MLKC) performed the research, selected the articles initially by title and abstract, and then read the full article. The two investigators conducted a systematic search in MEDLINE, (via PubMed), the CENTRAL (Cochrane Library Central Register of Controlled Trials, via Wiley), and EMBASE (via Elsevier) for studies assessing the treatment outcomes with palliative RT for incurable locally advanced HNC patients. Disagreements were resolved by consulting a third reviewer (AGG).
We have used the following search terms: (“head and neck neoplasms”[MeSH Terms] OR (“head”[All Fields] AND “neck”[All Fields] AND “neoplasms”[All Fields]) OR “head and neck neoplasms”[All Fields] OR (“head”[All Fields] AND “neck”[All Fields] AND “cancer”[All Fields]) OR “head and neck cancer”[All Fields]) AND (“palliative”[All Fields] OR “palliatively”[All Fields] OR “palliatives”[All Fields]) AND (“radiotherapy”[MeSH Terms] OR “radiotherapy”[All Fields] OR “radiotherapies”[All Fields] OR “radiotherapy”[MeSH Subheading] OR “radiotherapy [All Fields]). The list containing the articles and reviews was inspected, and the related studies were analyzed to complement the electronic query. Searches were performed from January 1966 up to July 2020, and the exploration was not limited by the publication’s language.
Study selection
We included only published studies evaluating the treatment outcomes of palliative RT for incurable HNC. Retrospective, prospective, or randomized clinical trials with at least 6 months of follow-up were included. Case reports or publications without information on survival, symptom control, toxicity, or RT were excluded.
Patients
We included only studies with patients over 18 years old with locally advanced HNC treated with palliative RT without curative intention. Publications that included patients treated with surgery followed by adjuvant RT or patients undergoing RT with curative intent were not considered.
Intervention
We assessed the efficacy of palliative RT in HNC patients. We classified the palliative schedule as short-course RT if the treatment was delivered in less than ten fractions. Long-course RT was classified as schedules delivering ≥10 fractions without treatment breaks to evaluation. Cycled RT was defined as an RT schedule delivering short RT B.I.D (i.e., twice a day) or not with treatment breaks for evaluation of at least 1 week between the RT periods. Studies using conventional RT (2D-RT), conformational RT (3D-RT), intensity-modulated RT (IMRT), or stereotactic body RT (SBRT) were allowed.
Outcomes
The primary objectives were to evaluate the overall objective response rate (ORR), overall survival (OS), and progression-free survival (PFS). The secondary endpoints were symptom relief (pain and dysphagia) and treatment-related toxicities. The toxicity analysis was estimated based on grade ≥3 acute side effects as a severe complication from palliative RT. ORR was categorized as complete response (CR), partial response (PR), stable disease (SD) or progressive disease (PD) based on the data reported in the publications. Furthermore, patients were recognized as objective responders with a complete (CR) or partial response (PR). We also estimated median OS and PFS. The PFS was estimated considering the criteria employed in the studies, i.e., the period without disease progression.
Clinical data
We obtained data of patients, treatment characteristics, and outcomes. Two reviewers (GAV, MLKC) independently selected data using a standardized method. The following information was collected: authors, year of publication, study design, number of patients, RT dose and fractionation, RT technique, ORR, symptom relief, median OS, median PFS, and grade ≥ 3 acute toxicities. The two reviewers were in charge of gathering all data for all studies using a standardized data extraction form. A third reviewer (AGG) was used to solve different issues by consensus
Data synthesis and analysis
The cumulative meta-analysis gives cumulative pooled estimates and 95% confidence intervals (CIs). The studies were successively combined by year of publication and evaluated using the random-effects model. The OS outcomes and 95% CIs were estimated, giving a general view of the evolution of intervention effects over time. The rates for each outcome were defined using the proportion rate (i.e., % of event and toxicity grade ≥ 3). We used the random-effects model due to a relevant variation in trial characteristics. A p-value lower than 0.05 was considered significant in all analyses. The meta-analysis was performed using the Open Meta-Analyst free open software. The following variables were evaluated in the meta-regression analysis; RT technique (2D-RT, 3D-RT, MIXED, IMRT, and SBRT), study design, type of fractionation (short, long, or cycled), and cumulative BED (as continuous and categorized by BED < 40 Gy10, BED40–60 Gy10, and BED > 60 Gy10). To calculate the BED, we used the formula:
where d = dose per fraction, n = number of fractions, and α/β= 10 Gy for HNC [15].
Results
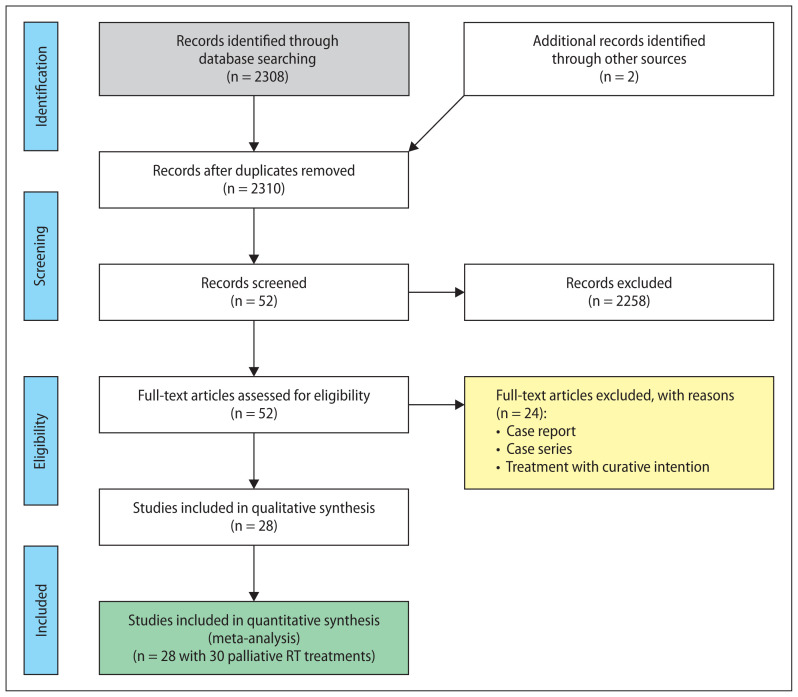
The search found 2,310 studies reporting the treatment outcomes employing palliative RT for HNC. After applying the inclusion criteria, 2,258 studies were excluded. The published studies were excluded due to several reasons, as described in the flowchart in Figure 1. Therefore, finally, we selected 28 studies [16–43], including 1,986 patients (Supplementary File — Tab. S1). Two studies were counted twice because they had more than one group using different schedules of palliative RT [40, 41]. In the statistical analysis, we considered each group as a single trial, resulting in thirty studies. The study design was retrospective, prospective, and randomized in sixteen, ten, and two studies, respectively. In general, the studies included elderly patients, with a median of 66 (range: 65–78) years, with 93% of squamous cell carcinoma (Tab. 1). Ten studies used short-, ten used long-, and eight trials used cycled-course RT. The median BED Gy10 was 56 Gy10 ranging from 30 to 72Gy10, with 12, 3, 5, 5, and 3 studies using 2D-RT, 33D-RT, 3D/IMRT (mixed), IMRT, and SBRT, respectively. Table 1 summarized the characteristics of studies included in the meta-analysis.
Figure 1.
Flow chart with article selection and inclusion methods according to PRISMA guidelines
Table 1.
Characteristics of studies included in the meta-analysis and meta-regression analysis of categorical and continuous moderator variables related to overall response rate
| Variables | Study level n, median % (range) | Patients | Age | Gender | KPS |
|---|---|---|---|---|---|
| Number of studies Median/% (range) |
28 studies (2 studies with two arms counted as a study) | 28 studies 1986 (15–505) |
28 studies 66 years (65–78 y) |
26 studies Female: 24% patients (18–73%) Male: 76% patients (27–82%) |
24 studies 70 (60–80) |
| Metaregression analysis | |||||
|
Histology Squamous cell carcinoma |
26 studies, 93% patients (60–100%) | Coefficients | Lower bound | Upper bound | p-value |
| Total BED Gy10 | 22 studies, median 56 Gy10 (30–72 Gy10) BED > 60 Gy10 BED 40–60 Gy10 BED < 40 Gy10 |
Ref −0.4 −0.7 |
−0.6 −1.1 |
−0.2 −0.3 |
0.001 0.001 |
|
RT course Cycled Long Short |
8 studies — 315 (21–75) patients 10 studies — 660 (25–158) patients 10 studies — 1011 (17–505) patients |
Ref −0.012 0.23 |
−0.13 0.10 |
0.10 0.44 |
0.88 0.01 |
|
RT technique 2D-RT 3D-RT Mixed IMRT SBRT |
12 studies — 1289 (23–550) patients 3 studies — 98 (30–35) patients 5 studies — 393 (21–148) patients 5 studies — 127 (17–34) patients 3 studies — 79 (15–44) patients |
Ref 0.08 −0.06 −0.13 0.47 |
−0.08 −0.24 −0.32 0.06 |
0.25 0.10 0.05 0.88 |
0.31 0.44 0.16 0.02 |
|
Study design Prospective Randomized Retrospective |
10 studies — 592 (25–158) patients 2 studies — 80 (17–23) patients 16 studies — 1314 (15–505) patients |
Ref 0.23 0.24 |
0.04 0.10 |
0.4 0.38 |
0.015 0.001 |
|
Intercept Total BED |
22 studies, median 56 Gy10 (30–72 Gy10) | 2.4 0.03 |
1.4 0.01 |
3.4 0.4 |
0.001 0.001 |
BED— biological effective dose; 2D-RT — conventional radiotherapy; 3D-RT — conformational radiation therapy; IMRT — intensity-modulated radiation therapy; SBRT — stereotactic body radiation therapy
Clinical outcomes
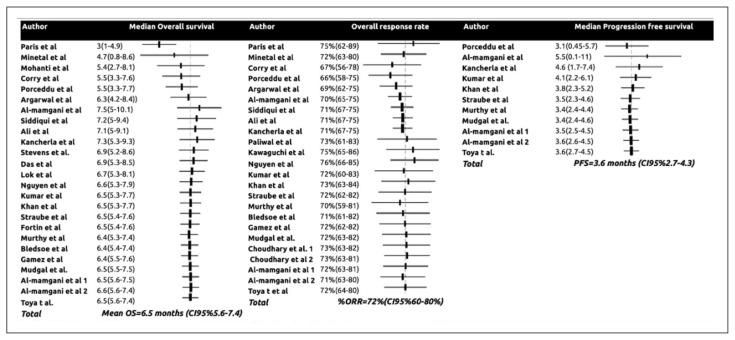
Twenty-five studies including 1,851 patients reported the median OS. The cumulative effect size of palliative RT was estimated at a median OS of 6.5 (95% CI: 5.6–7.4) months, and the PFS was 3.6 (95% CI: 2.7–4.3) months (Fig. 2AC). Pooling the data from 24 studies with 1,168 patients, the cumulative effect for ORR was 72% (95% CI: 60–80%) (Fig. 2B). Evaluating the cumulative effect over time, the OS changed significantly after the publication of Agarwal et al., and achieved stability from 2010 onwards after the publication of Nguyen et al. (Fig. 2A) [22, 32]. The PFS remained inside of 95% CI; after the publication of Kumar et al. in 2015, the PFS achieved stability, (Fig. 2C) [33].
Figure 2.
The cumulative effect of palliative radiation therapy (RT) on median overall survival (OS), overall response rate (ORR) and median progression-free survival (PFS)
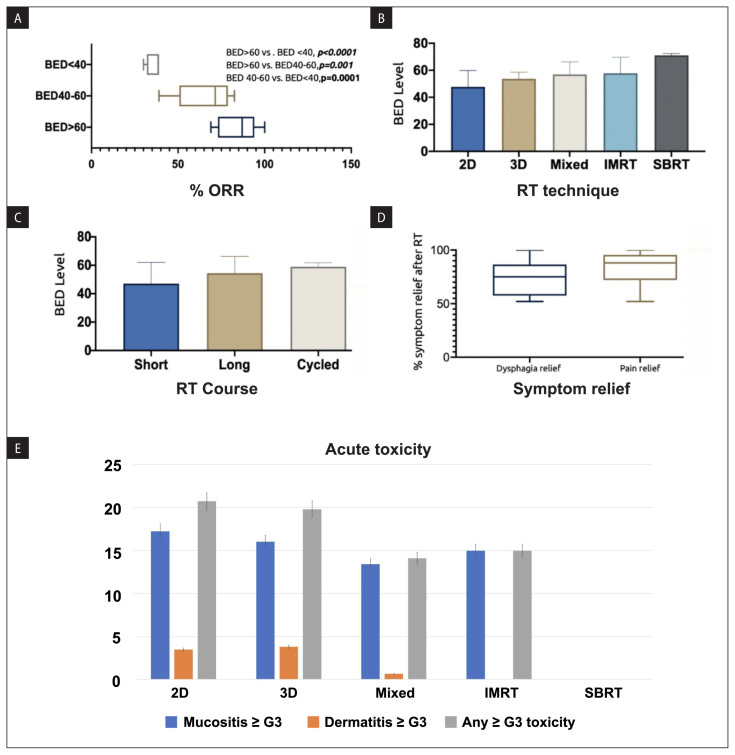
Meta-regression for ORR
In the meta-regression analysis, three variables were significantly associated with ORR (Tab. 1). BED was considered both a continuous and categorical variable. The BEDs ranged from 30 to 72 Gy10, and they were stratified into three levels — BED < 40 Gy10, BED 40–60 Gy10, and BED > 60 Gy10 so as to obtain a comparable number of studies in each bin. In the meta-regression analysis, the ORR for BED < 40 Gy10 and BED 40–60 Gy10 were significantly different from BED > 60 Gy10 (p = 0.001) (Fig. 3A, Tab. 1). The BED levels regarding the RT technique and type of RT course are illustrated in Figure 3BC. Additionally, short-course RT (p = 0.01), SBRT (p = 0.02), and study design (retrospective and RCT) were also associated with a better ORR, as shown in Table 1.
Figure 3.
A. Variables significantly associated with overall response rate (ORR); B. Radiation therapy (RT) technique and biological effective doses (BED) level; C. Type of RT course and BED level; D. Pain and dysphagia relief after palliative RT; E. Cumulative rates of grade ≥ 3 acute mucositis, dermatitis, and any grade ≥ 3 toxicity by RT technique
Pain and dysphagia relief
Fourteen and eleven studies, with 1,181 and 861 patients treated with palliative RT reported pain and dysphagia relief as an outcome, respectively. Combining the studies, the cumulative rate of pain and dysphagia relief after palliative RT were 83% (95% CI: 52–100), and 75% (95% CI: 52–100%), respectively (Fig. 3D).
Grade ≥ 3 acute toxicity
Twenty-three studies with 1578 patients reported toxicity as an outcome. The cumulative rates of grade ≥ 3 acute mucositis and dermatitis were 16.8% (95% CI: 9–24.4%) and 3.4% (95% CI: 1.8–5%), respectively (Fig. 3E). Evaluating the cumulative rates of grade ≥ 3 acute mucositis and dermatitis by RT technique, rates were higher for 2D-RT (17.1% and 3.5%) and 33D-RT (16% and 3.8%) techniques than for studies employing mixed (2D-RT, 33D-RT and IMRT) techniques (13% and 0.7%), IMRT (14% and 0) and SBRT (0 and 0) (Fig. 3E).
Discussion
This meta-analysis evaluated the impact of RT technical aspects on palliative HNC patients’ treatment outcomes. The results showed that palliative RT, independent of the scheme, achieves a high ORR and relief of symptoms. The most common symptoms were pain and dysphagia, and for both, palliative RT provided a remission rate of 83% and 75%, respectively. The estimated median OS of these patients was 6.5 months, with a median PFS of 3.2 months. Putting these outcomes together, an obvious query would be the optimal choice of RT schedule and dose. Herein, we attempted to address this question by using ORR as an independent variable in a meta-regression analysis and total BED, BED levels (< 40 Gy10, 40–60 Gy10, and > 60 Gy10), RT schedule (short, long, and cycled), study design, and RT technique were recognized as the dependent variables. The ORR was chosen as an independent variable because a higher ORR can be associated with a high rate of symptom relief, longer duration of response, and local control. Moreover, we observed a stable trend for the clinical endpoints of OS and PFS, which reduces the likelihood of detecting an association between the variables and these outcomes. We found that significant factors for ORR included cumulative BED and RT schedule.
These outcomes of the meta-regression analysis are hypothesis-generating and, at the same time, significant for the clinical practice. The magnitude of the difference in ORR between the trials using a BED > 60 Gy10 compared to a BED < 40 Gy10 was significant (84.7% vs. 36.5%, p < 0.0001) (Fig. 3A). These findings raise the question if the combination of SBRT with an ultra-hypofractionated schedule achieving a high BED in well-selected patients could confer a survival advantage. The outcomes recently presented by Al-Assaf et al. support this hypothesis [44]. In their retrospective study, SBRT with ultra-hypofractionation was used in elderly patients unfit for radical treatment [44]. Patients were treated with SBRT delivering a total dose ranging from 35 to 50 Gy in 4 to 6 fractions. Patient characteristics were, however, heterogeneous and included those previously untreated (n = 48), recurrent never irradiated (n = 19), oligometastatic (n = 17) and previously irradiated (n = 33) [44]. Local control (LC) at 12 months and median PFS for the respective subgroups were 85.8%, 78.2%, 85%, 78.9% (p = 0.86) and 23.7, 14.8, 10.5 and 7.8 months (p = 0.04), respectively [44]. Although Al-Assaf et al. included a mixed HNC population, their good results using SBRT point in the same direction as our findings using the same technique in a palliative setting.
Moreover, Malik et al, in a systematic review and meta-analysis, also analyzed the role of SBRT for de novo HNC [45]. In this review, with 157 patients from nine studies, SBRT was safe and provided good locoregional control rates with a low rate of side effects [45]. The OS rates at 1, 2, and 3 years were 75.9%, 61.1%, and 50.0%, respectively [45]. LC rates at 1, 2, and 3 years were 90.7%, 81.8%, and 73.4% each [45]. The late G5 toxicity rate was 0.1%, and the G3–4 rate was 3.3% [45].
Regarding the relevance to clinical practice, the fact that HNC patients undergoing palliative RT harbored a shortened survival makes a short-course treatment appealing [7]. Next, short-course RT could increase patient convenience and reduce non-compliance and interruptions [9]. However, it is critical to stress that the short course studies used a similar BED level than cycled- and long-course RT. The similar BED between the different radiation schedules (short, long, and cycled) raises the question if the better ORR observed with the short course is possibly related to better patient adherence, fewer treatment interruptions, treatment gap, reducing the tumor repopulation, or smaller treatment volumes. Nonetheless, we lack information on these variables to resolve any potential confounders of our findings. On the other hand, the contribution of the SBRT for a better ORR than other techniques can be explained by the use of better images to define the gross tumor volume combining MRI with PET-CT, by the use of image-guided radiation therapy (IGRT) to deliver the treatment which allows employing a short course with a high BED closing the intricate net to explain the better result found [45].
Toxicity is another crucial element to acknowledge in the decision about RT schedule, dose, and technique to palliate HNC patients [7]. The evaluation considered early toxicity as a parameter due to the reduced median OS and its connection with treatment interruption and adherence. The rate of acute ≥G3 mucositis and dermatitis was higher with conventional techniques than with IMRT and SBRT. There was a difference of approximately 5% and 20% for any G3 toxicity comparing IMRT, and SBRT vs. 2D and 3D techniques (Fig. 3E). Nonetheless, we acknowledge that these differences may be attributed to using older RT techniques to deliver comparable BEDs and smaller treatment target volumes with SBRT. Regarding some planning aspects of 2D/33D-RT and IMRT/SBRT studies, in general, the margins were ≥ 1.0 cm with parallel opposite fields in 2D/33D-RT trials compared with margins ≤ 1.0 cm in IMRT/SBRT publications (Supplementary File — Tab. S1).
Based on the meta-analysis, trials employing a high BED, ideally higher than 60 Gy10, with a short RT schedule, delivered with IMRT or SBRT, obtained a better ORR with a lower incidence of severe acute toxicity.
However, even with these positive findings, it is important to highlight some limitations of the present study. Foremost, a meta-analysis of observational studies can carry the same bias from the source data. Next, we were unable to resolve several potential confounders for analyses of the symptom relief and toxicity endpoints. Moreover, another limitation is the lack of detailed data and outcomes concerning disease subsites, clinical stage, and clinical (ECOG) and tumor parameters. With most studies including a population with mixed disease sites, a more detailed analysis was not possible. Nonetheless, the present study is hypothesis-generating for the design of future studies, and these findings represent the best evidence available to guide the radiation oncologist to maximize the treatment outcomes in the HNC palliative setting.
Conclusion
Palliative RT is effective in providing tumor response and symptom relief in patients with incurable HNC. Considering the differences detected by the meta-analysis, short RT courses with a high BED using IMRT or SBRT can improve the therapeutic index of RT. Acknowledging the studies heterogeneity, the limited number of patients, and the absence of long-term data, further research is demanded in this area. The findings reported here are hypothesis-generating and can guide the development of future clinical trials investigating palliative RT in HNC.
Supplementary Information
Acknowledgements
None declared.
Footnotes
Conflict of interests
M.L.K.C. declare the following financial interests/personal relationships: funds by the National Medical Research Council Clinician-scientist award (NMRC/CSA/0027/2018) and the Duke-NUS Oncology Academic Clinical Programme — Proton Therapy Research Philanthropic Funds, both outside the current work. F.Y.M. reports previous consulting fees from Elekta and honoraria from Astra-Zeneca, both outside the current work. All other authors have no competing interests.
Funding
None declared.
Ethical permission
Ethical approval was not necessary for the preparation of this article.
Data availability statement
Research data are stored and will be shared upon request to the corresponding author.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Vokes EE, Weichselbaum RR, Lippman SM, et al. Head and neck cancer. N Engl J Med. 1993;328(3):184–194. doi: 10.1056/NEJM199301213280306. [DOI] [PubMed] [Google Scholar]
- 3.Porceddu SV, Scotté F, Aapro M, et al. Treating Patients With Locally Advanced Squamous Cell Carcinoma of the Head and Neck Unsuitable to Receive Cisplatin-Based Therapy. Front Oncol. 2019;9:1522. doi: 10.3389/fonc.2019.01522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kowalski LP, Carvalho AL. Natural history of untreated head and neck cancer. Eur J Cancer. 2000;36(8):1032–1037. doi: 10.1016/s0959-8049(00)00054-x. [DOI] [PubMed] [Google Scholar]
- 5.Pignon JP, le Maître A, Maillard E, et al. MACH-NC Collaborative Group. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiother Oncol. 2009;92(1):4–14. doi: 10.1016/j.radonc.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Stell PM. Survival times in end-stage head and neck cancer. Eur J Surg Oncol. 1989;15:407–10. [PubMed] [Google Scholar]
- 7.Shahid Iqbal M, Kelly C, Kovarik J, et al. Palliative radiotherapy for locally advanced non-metastatic head and neck cancer: A systematic review. Radiother Oncol. 2018;126(3):558–567. doi: 10.1016/j.radonc.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 8.Thompson AR, Krouse RS. Terminal care in head and neck cancer patients: a framework for medical decision making. J Am Coll Surg. 2004;198(5):837–841. doi: 10.1016/j.jamcollsurg.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 9.Grewal AS, Jones J, Lin A. Palliative Radiation Therapy for Head and Neck Cancers. Int J Radiat Oncol Biol Phys. 2019;105(2):254–266. doi: 10.1016/j.ijrobp.2019.05.024. [DOI] [PubMed] [Google Scholar]
- 10.Talapatra K, Gupta T, Agarwal JP. Palliative radiotherapy in head and neck cancers: Evidence based review. Indian Journal of Palliative Care. 2006;12(2):44. doi: 10.4103/0973-1075.30244. [DOI] [Google Scholar]
- 11.Hodson DI, Bruera E, Eapen L, et al. The role of palliative radiotherapy in advanced head and neck cancer. Can J Oncol. 1996;6(Suppl 1):54–60. [PubMed] [Google Scholar]
- 12.Shahid Iqbal M, Kelly C, Kovarik J, et al. Palliative radiotherapy for locally advanced non-metastatic head and neck cancer: A systematic review. Radiother Oncol. 2018;126(3):558–567. doi: 10.1016/j.radonc.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group, PRISMA Group, PRISMA Group, PRISMA Group, PRISMA Group, PRISMA Group, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3(3):e123–e130. [PMC free article] [PubMed] [Google Scholar]
- 14.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 15.Fowler JF, Rezvani M, Fowler JF, et al. The first James Kirk memorial lecture. What next in fractionated radiotherapy? Br J Cancer Suppl. 1984;6(2):285–300. [PMC free article] [PubMed] [Google Scholar]
- 16.Paris KJ, Spanos WJ, Lindberg RD, et al. Phase I–II study of multiple daily fractions for palliation of advanced head and neck malignancies. Int J Radiat Oncol Biol Phys. 1993;25(4):657–660. doi: 10.1016/0360-3016(93)90012-k. [DOI] [PubMed] [Google Scholar]
- 17.Minatel E, Gigante M, Franchin G, et al. Combined radiotherapy and bleomycin in patients with inoperable head and neck cancer with unfavourable prognostic factors and severe symptoms. Oral Oncol. 1998;34(2):119–122. doi: 10.1016/s1368-8375(97)00073-0. [DOI] [PubMed] [Google Scholar]
- 18.Mohanti BK, Umapathy H, Bahadur S, et al. Short course palliative radiotherapy of 20 Gy in 5 fractions for advanced and incurable head and neck cancer: AIIMS study. Radiother Oncol. 2004;71(3):275–280. doi: 10.1016/j.radonc.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Ghoshal S, Patel F, Mudgil N, et al. Palliative radiotherapy in locally advanced head and neck cancer-A prospective trial. Indian J Palliat Care. 2004;10:19–23. [Google Scholar]
- 20.Corry J, Peters LJ, Costa ID’, et al. The ‘QUAD SHOT’--a phase II study of palliative radiotherapy for incurable head and neck cancer. Radiother Oncol. 2005;77(2):137–142. doi: 10.1016/j.radonc.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Porceddu SV, Rosser B, Burmeister BH, et al. Hypofractionated radiotherapy for the palliation of advanced head and neck cancer in patients unsuitable for curative treatment--”Hypo Trial”. Radiother Oncol. 2007;85(3):456–462. doi: 10.1016/j.radonc.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 22.Agarwal JP, Nemade B, Murthy V, et al. Hypofractionated, palliative radiotherapy for advanced head and neck cancer. Radiother Oncol. 2008;89(1):51–56. doi: 10.1016/j.radonc.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Al-mamgani A, Tans L, Van rooij PHE, et al. Hypofractionated radiotherapy denoted as the “Christie scheme”: an effective means of palliating patients with head and neck cancers not suitable for curative treatment. Acta Oncol. 2009;48(4):562–570. doi: 10.1080/02841860902740899. [DOI] [PubMed] [Google Scholar]
- 24.Siddiqui F, Patel M, Khan M, et al. Stereotactic body radiation therapy for primary, recurrent, and metastatic tumors in the head-and-neck region. Int J Radiat Oncol Biol Phys. 2009;74(4):1047–1053. doi: 10.1016/j.ijrobp.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 25.Ali MY, Alam M, Mannan MA, et al. Short Course Palliative Radiotherapy in Locally Advanced Squamous Cell Carcinoma of Head and Neck. J Armed Forces Med Coll. 1970;6(1):16–20. doi: 10.3329/jafmc.v6i1.5986. [DOI] [Google Scholar]
- 26.Kancherla KN, Oksuz DC, Prestwich RJD, et al. The role of split-course hypofractionated palliative radiotherapy in head and neck cancer. Clin Oncol (R Coll Radiol) 2011;23(2):141–148. doi: 10.1016/j.clon.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Stevens CM, Huang SH, Fung S, et al. Retrospective study of palliative radiotherapy in newly diagnosed head and neck carcinoma. Int J Radiat Oncol Biol Phys. 2011;81(4):958–963. doi: 10.1016/j.ijrobp.2010.06.055. [DOI] [PubMed] [Google Scholar]
- 28.Paliwal R, Kumar-Patidar A, Walke R, et al. Palliative Hypo-fractionated Radiotherapy in Locally Advanced Head and Neck Cancer with Fixed Neck Nodes. Iran J Cancer Prev. 2012;5(4):178–182. [PMC free article] [PubMed] [Google Scholar]
- 29.Kawaguchi K, Sato K, Yamada H, et al. Stereotactic radiosurgery in combination with chemotherapy as primary treatment for head and neck cancer. J Oral Maxillofac Surg. 2012;70(2):461–472. doi: 10.1016/j.joms.2011.02.063. [DOI] [PubMed] [Google Scholar]
- 30.Das S, Thomas S, Pal SK, et al. Hypofractionated Palliative Radiotherapy in Locally Advanced Inoperable Head and Neck Cancer: CMC Vellore Experience. Indian J Palliat Care. 2013;19(2):93–98. doi: 10.4103/0973-1075.116709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lok BH, Jiang G, Gutiontov S, et al. Palliative head and neck radiotherapy with the RTOG 8502 regimen for incurable primary or metastatic cancers. Oral Oncol. 2015;51(10):957–962. doi: 10.1016/j.oraloncology.2015.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nguyen NTA, Doerwald-Munoz L, Zhang H, et al. 0-7-21 hypofractionated palliative radiotherapy: an effective treatment for advanced head and neck cancers. Br J Radiol. 2015;88(1049):20140646. doi: 10.1259/bjr.20140646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kumar A, Sharma A, Mohanti BK, et al. A phase 2 randomized study to compare short course palliative radiotherapy with short course concurrent palliative chemotherapy plus radiotherapy in advanced and unresectable head and neck cancer. Radiother Oncol. 2015;117(1):145–151. doi: 10.1016/j.radonc.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 34.Khan L, Tjong M, Raziee H, et al. Role of stereotactic body radiotherapy for symptom control in head and neck cancer patients. Support Care Cancer. 2015;23(4):1099–1103. doi: 10.1007/s00520-014-2421-y. [DOI] [PubMed] [Google Scholar]
- 35.Straube C, Pigorsch SU, Scherb H, et al. Reduced volume SIB-IMRT/IGRT to head and neck cancer in elderly and frail patients: outcome and toxicity. Radiat Oncol. 2016;11(1):133. doi: 10.1186/s13014-016-0711-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fortin B, Khaouam N, Filion E, et al. Palliative Radiation Therapy for Advanced Head and Neck Carcinomas: A Phase 2 Study. Int J Radiat Oncol Biol Phys. 2016;95(2):647–653. doi: 10.1016/j.ijrobp.2016.01.039. [DOI] [PubMed] [Google Scholar]
- 37.Murthy V, Kumar DP, Budrukkar A, et al. Twice-weekly palliative radiotherapy for locally very advanced head and neck cancers. Indian J Cancer. 2016;53(1):138–141. doi: 10.4103/0019-509X.180847. [DOI] [PubMed] [Google Scholar]
- 38.Bledsoe TJ, Noble AR, Reddy CA, et al. Split-Course Accelerated Hypofractionated Radiotherapy (SCAHRT): A Safe and Effective Option for Head and Neck Cancer in the Elderly or Infirm. Anticancer Res. 2016;36(3):933–939. [PubMed] [Google Scholar]
- 39.Gamez ME, Agarwal M, Hu KS, et al. Hypofractionated Palliative Radiotherapy with Concurrent Radiosensitizing Chemotherapy for Advanced Head and Neck Cancer Using the “QUAD-SHOT Regimen”. Anticancer Res. 2017;37(2):685–691. doi: 10.21873/anticanres.11364. [DOI] [PubMed] [Google Scholar]
- 40.Mudgal A, Arya AK, Yadav I, et al. Role of hypofractionated palliative radiotherapy in patients with stage four head-and-neck squamous cell carcinoma. J Cancer Res Ther. 2019;15(3):528–532. doi: 10.4103/jcrt.JCRT_116_18. [DOI] [PubMed] [Google Scholar]
- 41.Choudhary A, Gupta A. Conventional Fractionation versus Quad Shot in Advanced Head-and-Neck Cancers: A Randomized Controlled Trial. Indian J Palliat Care. 2019;25(4):527–534. doi: 10.4103/IJPC.IJPC_209_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Al-Mamgani A, Kessels R, Verhoef CG, et al. Randomized controlled trial to identify the optimal radiotherapy scheme for palliative treatment of incurable head and neck squamous cell carcinoma. Radiother Oncol. 2020;149:181–188. doi: 10.1016/j.radonc.2020.05.020. [DOI] [PubMed] [Google Scholar]
- 43.Toya R, Saito T, Yamaguchi K, et al. Hypofractionated palliative volumetric modulated arc radiotherapy with the Radiation Oncology Study Group 8502 “QUAD shot” regimen for incurable head and neck cancer. Radiat Oncol. 2020;15(1):123. doi: 10.1186/s13014-020-01548-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al-Assaf H, Erler D, Karam I, et al. Stereotactic body radiotherapy for medically unfit patients with cancers to the head and neck. Head Neck. 2020;42(8):2050–2057. doi: 10.1002/hed.26138. [DOI] [PubMed] [Google Scholar]
- 45.Malik NH, Kim MS, Chen H, et al. Stereotactic Radiation Therapy for De Novo Head and Neck Cancers: A Systematic Review and Meta-Analysis. Adv Radiat Oncol. 2021;6(1):100628. doi: 10.1016/j.adro.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Research data are stored and will be shared upon request to the corresponding author.