Abstract
We assessed the risk of reinfection among all residents in South Korea who tested positive for coronavirus disease 2019 from January to August 2022. Children 5–11 years [adjusted hazard ratio (aHR) = 2.20], and 12–17 years old (aHR = 2.00), were at higher risk; whereas 3-dose vaccination (aHR = 0.20) lowered the risk of reinfection.
Keywords: COVID-19, SARS-CoV-2, coronavirus, reinfection
Following the introduction of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron subvariant, many countries have experienced large numbers of coronavirus disease 2019 (COVID-19) reinfections.1 However, few detailed cohort studies are available from countries where vaccination rates remain suboptimal in children. South Korea has a relatively lower vaccine coverage rate of 1.5% among children 5–11 years old, compared with a vaccine coverage rate of more than 80% in adolescents 12–17 years of age, as of August 2022. In this study, we aimed to assess the risk of SARS-CoV-2 reinfection using the Korean national cohort.
Details of the surveillance and vaccination system in South Korea have been previously described.2 All residents in South Korea who tested positive for COVID-19 infection via rapid antigen test or polymerase chain reaction from January 1 to August 30, 2022, were included (Figure, Supplemental Digital Content 1, http://links.lww.com/INF/F61). Reinfection is defined as occurring ≥45 days after initial positive laboratory-confirmed COVID-19. Risk of reinfection by demographic characteristics, health status (immunocompromised, or living in a long-term care facility) and vaccination status (0–3 doses) were assessed. For each individual, a Cox proportional hazards model was fitted, and adjusted for sex, age, residence, health status, and vaccination status. Adjusted hazard ratios from the age-and-sex-adjusted and fully adjusted models are reported with 95% confidence intervals. All statistical analyses were conducted using R v.4.02 (R Core Team, Vienna). This work was approved by Korea Disease Control and Prevention Agency Institutional Review Board (IRB No. 2021-12-03-PE-A).
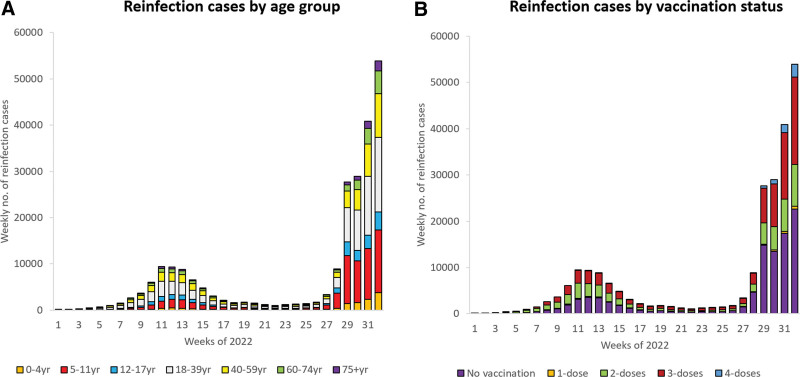
In 2022, there were 2 peaks of the COVID-19 outbreak in Korea, largely attributable to Omicron subvariant BA.1 and BA.2 in March and BA.5 in August (Figure 1, Supplemental Digital Content 1, http://links.lww.com/INF/F61). Between January and August 2022, a total of 154,924 SARS-CoV-2 reinfection cases were identified, which was 0.9% of 17,543,961 total COVID-19 cases (Table 1). Figure 1 shows the secular trend of SARS-CoV-2 reinfection by (1) age group and by (2) vaccination status. Females [adjusted hazard ratio (aHR) = 1.18; 95% CI: 1.17–1.20], children 5–11 years (aHR = 2.20; 95% CI: 2.15–2.26) and adolescents 12–17 years of age (aHR = 2.00; 95% CI: 1.95–2.05) were associated with increased risk of SARS-CoV-2 reinfection (Table 1). Residents of noncapital area (aHR = 1.13; 95% CI: 1.12–1.14) and long-term care facility (aHR = 2.34; 95% CI: 2.26–2.43) were at increased risk of reinfection. Individuals with 2-dose vaccination (aHR = 0.54; 95% CI: 0.49–0.59) and 3-dose vaccination (aHR = 0.20; 95% CI: 0.07–0.53) were at lower risk of SARS-CoV-2 reinfection.
TABLE 1.
Risk Factor for SARS-CoV-2 Reinfection Cases, Jan 2022–Aug 2022, South Korea
| Variables | Reinfection | /Total infection | (%) | Incidence* | aHR | (95% CI) |
|---|---|---|---|---|---|---|
| Total | 154,924 | 17,543,961 | (0.9) | 6.15 | ||
| Sex | ||||||
| Male | 69,444 | 8,209,962 | (0.8) | 5.88 | Ref. | |
| Female | 85,480 | 9,333,999 | (0.9) | 6.38 | 1.18 | (1.17–1.20) |
| Age group (yrs) | ||||||
| 0–4 | 10,015 | 820,843 | (1.2) | 8.46 | 1.13 | (1.10–1.16) |
| 5–11 | 49,123 | 1,944,653 | (2.5) | 17.32 | 2.20 | (2.15–2.26) |
| 12–17 | 12,457 | 1,324,395 | (0.9) | 6.49 | 2.00 | (1.95–2.05) |
| 18–39 | 43,912 | 5,560,239 | (0.8) | 5.47 | 1.70 | (1.67–1.72) |
| 40–59 | 22,907 | 4,842,637 | (0.5) | 3.30 | Ref. | |
| 60–74 | 11,021 | 2,224,252 | (0.5) | 3.51 | 1.03 | (1.01–1.06) |
| 75+ | 5,489 | 826,942 | (0.7) | 4.74 | 1.16 | (1.12–1.20) |
| Residence | ||||||
| Capital area | 79,920 | 9,172,732 | (0.9) | 5.99 | Ref. | |
| Non-capital area | 75,004 | 8,371,229 | (0.9) | 6.32 | 1.13 | (1.12–1.14) |
| Health status | ||||||
| Immunocompromised | 2,620 | 447,934 | (0.6) | 4.12 | 1.23 | (1.18–1.28) |
| LTCF residents | 4,182 | 293,178 | (1.4) | 9.84 | 2.34 | (2.26–2.43) |
| General population | 148,122 | 16,802,849 | (0.9) | 6.13 | Ref. | |
| Vaccination status† | ||||||
| Unvaccinated | 143,804 | 15,958,222 | (0.9) | 6.30 | Ref. | |
| 1-dose | 10,689 | 1,555,628 | (0.7) | 4.59 | 0.94 | (0.92–0.96) |
| 2-doses | 427 | 29,542 | (1.4) | 9.26 | 0.54 | (0.49–0.59) |
| 3-doses+ | 4 | 569 | (0.7) | 4.16 | 0.20 | (0.07–0.53) |
Incidence per 100,000 person-days.
Vaccination status, post-primary infection and before reinfection.
aHR indicates adjusted hazard ratio (adjusted for sex, age, residence, health status, vaccination status); LTCF, long-term care facility.
FIGURE 1.
Weekly number of SARS-CoV-2 reinfection cases by (A) age group and (B) by vaccination status, Jan – Aug 2022, South Korea.
We found that during the surge of Omicron BA.1, BA.2 and BA.5 outbreaks in South Korea, 2022, unvaccinated persons, notably, children, were associated with increased risk of SARS-CoV-2 reinfection. This finding is in line with a meta-analysis of 91 studies, showing that the risk of infection was substantially lower among vaccinated individuals compared with unvaccinated persons. (0.32% vs. 0.74%).3 Before the emergence of the Omicron variant, the risk of reinfection was lower in children. In England between 2020 and 2021, children had a lower risk of reinfection than did adults (21.53 vs. 72.53 per 100,000).4 However, following the introduction of the Omicron variant, the risk of reinfection has increased in all population, most notably in unvaccinated children. Vaccines have shown to provide protection against SARS-CoV-2 infection, severe infection, or death in children. In the US, the estimated effectiveness of Omicron infection alone against reinfection with Omicron in vaccinated children was 79.4–94.3%, highlighting the benefit from the vaccines.5
There are several limitations to this study. First, we used surveillance data that does not collect detailed clinical information including the timing of the vaccination. Therefore, the interpretation of the result should be made cautiously since the clinical implication of reinfection and vaccination may vary according to the significance of the clinical spectrum. Second, given the nature of the observational study, we were not able to control uniformed inclusion criteria for testing, thus poses ascertainment bias. Third, although we cannot exclude the possibility that some of the reinfections might have been due to false positive results, we anticipate that these cases represented only a small fraction of results with a negligible overall impact on study findings and conclusions.
Our study provides large-scale population-level evidence on reinfection of SARS-CoV-2, showing that the risk is elevated in unvaccinated individuals and in children. These findings suggest that although there are breakthrough infections among vaccinated persons, vaccination further decreased the risk of reinfection compared to unvaccinated persons.
ACKNOWLEDGMENTS
We thank the COVID-19 Vaccination Task Force and Division of National Immunization, Korea Disease Control and Prevention Agency; relevant ministries, including the Ministry of Interior and Safety, Si/Do and Si/Gun/Gu; medical staff in health centers; and medical facilities for their efforts in responding to the COVID-19 outbreak. This study was part of the Korea COvid-19 Vaccine Effectiveness (K-COVE) Initiative.
E.J.J. is a public health officer at the Korea Disease Control and Prevention Agency. Her main research interests are epidemiologic investigations and surveillance measures of infectious diseases. Y.J.C. is a clinical associate professor of pediatrics at the Korea University Anam Hospital. His main research addresses the mechanisms of the immunization program’s impact on public health.
Supplementary Material
Footnotes
The authors have no funding or conflicts of interest to disclose.
Eun Jung Jang and Young June Choe contributed equally to the study.
The data that support the findings of this study are available on request from the corresponding author, Y.-J.P. The data are not publicly available due to Personal Information Protection Act of the Republic of Korea.
E.J.J., Y.J.C. and Y.-J.P. conceived and designed the study. E.J.J., G.-W.Y. and R.K.K. gathered, processed, and cleaned the data. E.J.J. and G.-W.Y. analyzed the data. E.J.J. and Y.-J.P. had full access to all the data in the study. S.K.P., J.H.L., K.H.L., S.Y. and S.L. worked on project administration and methodology. E.J.J. and Y.J.C. wrote the first draft of the article followed by iterative revision with Y.J.C. and Y.-J.P. All authors substantially contributed to discussion of content and reviewed and edited the article before submission. All authors were involved in the decision to submit and agreed to publish the article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (www.pidj.com).
REFERENCES
- 1.Pulliam JRC, van Schalkwyk C, Govender N, et al. Increased risk of SARS-CoV-2 reinfection associated with emergence of Omicron in South Africa. Science (New York, NY). 2022;376:eabn4947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim YY, Choe YJ, Kim J, et al. Effectiveness of second mRNA COVID-19 booster vaccine in immunocompromised persons and long-term care facility residents. Emerg Infect Dis. 2022;28:2165–2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ren X, Zhou J, Guo J, et al. Reinfection in patients with COVID-19: a systematic review. Glob Health Res Policy. 2022;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mensah AA, Campbell H, Stowe J, et al. Risk of SARS-CoV-2 reinfections in children: a prospective national surveillance study between January, 2020, and July, 2021, in England. Lancet Child Adolesc Health. 2022;6:384–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin DY, Gu Y, Xu Y, et al. Effects of vaccination and previous infection on omicron infections in children. N Engl J Med. 2022;387:1141–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.