Abstract
Adult cutaneous T-cell lymphoma is an uncommon malignancy with poor prognosis and is usually seen in association with human T-cell lymphotropic virus type 1. We present the case of a 25-year-old female who gave a history of extensive whole-body polypoidal cutaneous and bilateral orbital and breast swellings. Biopsy was suggestive of cutaneous T-cell lymphoma and the patient was evaluated with 18F-labeled fluoro-2-deoxyglucose positron emission tomography and computed tomography for initial staging of the disease.
Keywords: Cutaneous T-cell lymphoma, fluoro-2-deoxyglucose, immunohistochemistry, leukemia, T-cell lymphotropic virus
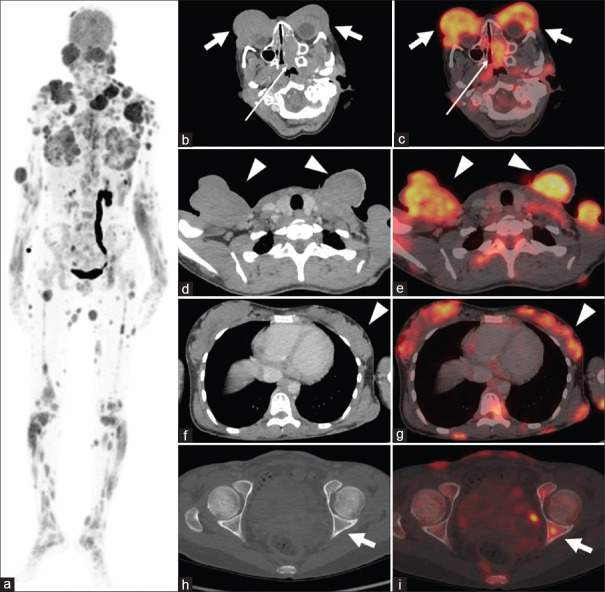
A 25-year-old female visited our hospital with complaints of multiple cutaneous polypoidal swellings all over the body for the past 7 months. On clinical examination, multiple polypoidal and noduloulcerative lesions were noted throughout the body along with bilateral orbital swellings and associated exophthalmos. Excisional biopsy was done from the right thigh lesion, which was suggestive of cutaneous T-cell lymphoma. Immunohistochemistry shows leukocyte common antigen and CD 3 positivity. The patient came to our department for initial staging with 18F-labeled fluoro-2-deoxyglucose positron emission tomography and computed tomography (18F-FDG PET/CT). The patient was given 210 mBq of 18F-FDG intravenously and scan was acquired after 45 min of injection. Maximum intensity projection image [Figure 1a] showed multiple FDG-avid lesions throughout the body. Axial CT and fused PET/CT images showed FDG-avid soft tissue density lesions involving bilateral orbits [Figure 1b and c, thick white arrows], left nasal cavity [Figure 1b and c, thin white arrows], skin and subcutaneous tissue of scalp, neck [Figure 1d and e, white arrow heads], bilateral breasts [Figure 1f and g, white arrow heads], and bilateral upper and lower limbs with skin, pleural, and marrow deposits [Figure 1h and i, thick white arrow]. The patient was started on rituximab cyclophosphamide hydroxydaunomycin oncovin prednisolone (R-CHOP) chemotherapy, but unfortunately, the patient’s condition deteriorated rapidly and was ultimately succumbed to death.
Figure 1.
(a) MIP (a) image showing multiple FDG-avid lesions throughout the whole body. Physiological FDG uptake is noted in the brain, kidneys, dilated left ureter, and bladder. (b-i) Axial CT and fused PET/CT showing intensely FDG-avid bilateral orbital swellings (b and c, thick white arrows), left nasal cavity lesion (b and c, thin white arrows), bilateral cervical and supraclavicular polypoidal lesions (d and e, white arrow heads), bilateral breast parenchymal nodular swellings (f and g, white arrow heads), and bone marrow deposits (h and i, thick white arrows). MIP: Maximum intensity projection, FDG: Fluoro-2-deoxyglucose, PET CT: Positron emission tomography and computed tomography
Adult T-cell lymphoma/leukemia (ATLL) is an aggressive malignancy with poor prognosis and has strong association with human T-cell lymphotropic virus type 1.[1] The most common extralymphatic site to be involved in a patient with T-cell lymphoma is skin.[2] Skin manifestations are primarily due to direct invasion of ATLL tumor cells and the most common skin lesions are nodulotumoural and maculopapular eruptions.[2-4] Orbital involvement in T-cell lymphoma is rare and if involved may present as exophthalmos, ulcerated conjunctival mass, lid edema, chemosis, and pain.[5,6] Early diagnosis of adult cutaneous T-cell lymphoma is difficult due to wide spectrum of clinical presentations and absence of definite diagnostic criteria. Multiple biopsies are often warrantied for definitive diagnosis due to variable morphological and phenotypical manifestations. 18F-FDG PET/CT can detect cutaneous and extracutaneous lesions and often help in assessing therapy response and evaluating disease recurrence. PET/CT helps in simultaneous assessment of thickness and metabolic activity of cutaneous lesions. Previous studies have shown that thickness of lesion correlates with the survival and thereby helps in risk stratification. Combined assessment of cutaneous lesion thickness and metabolic activity helps in better assessment of tumor burden. PET/CT also plays an important role in differentiating malignant from reactive lymphadenopathy. There is no definite cure for adult cutaneous T-cell lymphoma; therapeutic options are mainly for palliation. The goals of therapy include relieving symptoms, delaying disease progression, and inducing remission. Before considering the best option for treating this condition, accurate staging is mandatory. By providing both anatomical and physiological information, PET/CT can improve the initial staging and thereby helps in optimization of treatment regimen. 18F-FDG PET/CT in this case shows high FDG avidity in the lesions of adult cutaneous T-cell lymphoma with an extensive whole-body cutaneous, orbital, nasal cavity, breast, and skeletal involvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, et al. Arevised European-American classification of lymphoid neoplasms: A proposal from the International Lymphoma Study Group. Blood. 1994;84:1361–92. [PubMed] [Google Scholar]
- 2.Sawada Y, Hino R, Hama K, Ohmori S, Fueki H, Yamada S, et al. Type of skin eruption is an independent prognostic indicator for adult T-cell leukemia/lymphoma. Blood. 2011;117:3961–7. doi: 10.1182/blood-2010-11-316794. [DOI] [PubMed] [Google Scholar]
- 3.Pezeshkpoor F, Yazdanpanah MJ, Shirdel A. Specific cutaneous manifestations in adult T-cell leukemia/lymphoma. Int J Dermatol. 2008;47:359–62. doi: 10.1111/j.1365-4632.2008.03526.x. [DOI] [PubMed] [Google Scholar]
- 4.Tokura Y, Sawada Y, Shimauchi T. Skin manifestations of adult T-cell leukemia/lymphoma: Clinical, cytological and immunological features. J Dermatol. 2014;41:19–25. doi: 10.1111/1346-8138.12328. [DOI] [PubMed] [Google Scholar]
- 5.White WL, Ferry JA, Harris NL, Grove AS., Jr Ocular adnexal lymphoma. A clinicopathologic study with identification of lymphomas of mucosa-associated lymphoid tissue type. Ophthalmology. 1995;102:1994–2006. doi: 10.1016/s0161-6420(95)30764-6. [DOI] [PubMed] [Google Scholar]
- 6.Coupland SE, Foss HD, Assaf C, Auw-Haedrich C, Anastassiou G, Anagnostopoulos I, et al. T-cell and T/natural killer-cell lymphomas involving ocular and ocular adnexal tissues: A clinicopathologic, immunohistochemical, and molecular study of seven cases. Ophthalmology. 1999;106:2109–20. doi: 10.1016/S0161-6420(99)90492-X. [DOI] [PubMed] [Google Scholar]