During initial surges of the severe acute respiratory syndrome coronavirus 2 (COVID-19) pandemic, case investigation processes were overwhelmed. Technology point solutions have greater potential to increase efficiency and efficacy for any communicable disease using contact tracing and case investigation as a means of control.
Background
Initial COVID-19 surges in the United States created a need for technology to supplement human resources to increase efficiency and efficacy.
Methods
Resolve to Save Lives worked with jurisdictions to co-design four technology solutions—Epi Viaduct data pipeline, Epi Contacts contact elicitation webform, Epi Locator contact information search plugin, and Epi Viewpoint case management system (CMS)—to expand the capacity of case investigation and contact tracing (CI/CT) teams. We assessed impact on reducing CI/CT time intervals for COVID-19 using product data and user feedback.
Results
Epi Viaduct accelerated the transfer of approximately 7,400,000 records from an electronic laboratory reporting system in a single jurisdiction to the respective CMS from more than 2.5 hours to less than 1 minute and reduced time to remove duplicate laboratory results from multiple days to less than 6 hours. Epi Contacts focused on increasing the efficacy of contact elicitation, and during a single period, 10% of index cases (9,440 of 96,319) completed Epi Contacts for a total of approximately 18,700 contacts elicited. User interviews indicated the tool increased speed of CI/CT workflows. In total, 134,410 searches were run in Epi Locator by 7320 distinct users—75% of which returned 1 or more person matches. A simple CMS, Epi Viewpoint, was developed and completed, but not deployed.
Conclusions
Systems to mount large-scale population-based contact tracing programs were developed and implemented during the COVID-19 pandemic and can be adapted for CI/CT programs aiming to control the spread of other communicable diseases such as sexually transmitted diseases.
In March 2020, as the COVID-19 pandemic began to take hold in the United States,1 it became evident that large-scale case investigation and contact tracing (CI/CT) systems were needed.2 Case investigation and contact tracing (CI/CT) teams working with analog or basic Excel spreadsheet tools for case management would be quickly overwhelmed by the scale and speed required to effectively trace cases.3 Effective CI/CT requires a series of actions to be completed in a timely and comprehensive fashion—from an initial case seeking testing to their close contacts being identified, notified, and quarantined, if appropriate.
Resolve to Save Lives (RTSL) initiated conversations with local and state health departments regarding their general COVID-19 response and their CI/CT capacity to surface key bottlenecks in CI/CT workflows. Complex systems for cleaning and transferring data from electronic laboratory reporting (ELR) systems to case management systems (CMS) caused significant delays, increasing the interval before case isolation or contact quarantine. A case identified by a positive laboratory result required investigation; however, an overwhelmed case investigation team could be potentially unable to investigate at least 80% of cases—the required threshold to reduce virus transmission.4 For completed case investigations, incomplete or inaccurate data may have been collected for contact tracing, with no avenue for the patient to make corrections. Mathematical models used by RTSL found that 60% of onward transmissions are prevented with a 1-day testing delay, 1-day tracing delay and tracing, and isolation of 80% of infected contacts.5 Inaccurate or missing contact information often required investigation by specialized teams, further delaying the time to start of isolation or quarantine. Finally, a range of CMS were in use or being implemented, with varying levels of sophistication. Spreadsheets soon were unable to keep up with the volume of cases recorded and were limited in the number and complexity of workflows they could support. Sophisticated platforms that could handle the volume and complexity of CI/CT workflows had a long implementation term. A basic case management workflow sometimes took months to deploy, requiring human and financial resources many jurisdictions lacked. After deployment, a complex CMS could require several days of training for a new case investigator or contact tracer.
New technologies proliferated6 to address the growing number of problems health departments were experiencing with outdated systems.7 The RTSL team convened a working group with subject matter experts in public health and technology to review CMSs commonly used inside jurisdictional departments of health, such as Commcare (Dimagi, Cambridge, MA), CMSs newly developed for COVID-19 such as SaraAlert (The MITER Corporation, Bedford, MA, and Mclean, VA), and platforms newly adapted for COVID-19 case management such as Microsoft Dynamics (Microsoft Corporation, Redmond, WA) and Work.com (Salesforce, San Francisco, CA). These technology partnerships allowed RTSL to identify whether a vendor was already considering or designing new functionality to address the bottlenecks RTSL had surfaced.
METHODS
From April 6 to 10, 2020, the RTSL digital team initiated a technology design sprint to create solutions for gaps unaddressed with future development. The team worked with jurisdictional partners to design these solutions to complement existing technology solutions for CI/CT. Key guiding principles were to deploy quickly, increase the capacity of case investigators and contact tracers, isolate cases and quarantine close contacts8 faster, and facilitate quick adoption. Following the design sprint, RTSL proceeded to develop four products: Epi Viaduct (an ELR to CMS automated data pipeline), Epi Contacts (a digital contact elicitation form), Epi Locator (a plug-in for identifying contact information), and Epi Viewpoint (a simple CMS). The digital team comprised product designers, product leaders, technology operations experts, and a solutions architect. Product data were used as descriptive measures of the impact of these tools. Long-term costs for maintenance and support were considered, because jurisdictions would eventually need to be able to sustain these expenses. Integration with open-source tools to reduce operational cost was emphasized.
Epi Viaduct
Epi Viaduct data pipeline was released in accordance with the requirements of a large state including rural, suburban, and urban county jurisdictions (state A). Deployed in July 2020 as an integration with Commcare, it aimed to reduce the time interval from when a positive COVID-19 laboratory result was available in ELR to when a new case was created in a CMS. The new data pipeline de-duplicated laboratory results and case records, implemented error logging, and simplified the existing data flow. This data pipeline could be used between any 2 health solutions with the appropriate read and upsert automated programming interface (API). A file upload to a secure server or a read-only connection to a database could be used if APIs are not available. The algorithm for de-duplication and the process for error logging could be readily reused.
Epi Contacts
Initially deployed in a large urban county (county A) in November 2020 and piloted by state A in January 2021, the Epi Contacts contact elicitation webform was designed to increase the efficiency of case investigations and elicitation of close contacts. It sends a webform with modifiable branding and content via text message, which conveys information including details of the case investigation process and references to relevant informational materials per the local health department. The creation or update of a record—as defined by the jurisdiction—triggers sending a text message to each case. The solution was not configured to send messages in bulk. The case was then guided to complete a form collecting information on household and nonhousehold close contacts and other potential points of exposure. This webform was created close contact records in the CMS upon form submission via an integration, allowing contact tracing teams to begin outreach immediately or triggering automated outreach (Fig. 1).
Figure 1.

Sample Epi Contacts mobile screens of the initial SMS message and pages from the webform.
Epi Contacts was implemented for 2 different use cases. In 1 case, the SMS trigger preceded the case investigation, giving cases an indication of what to expect and increase the accuracy of close contact data collection while decreasing the amount of time case investigators needed to conduct interviews. In a second case, Epi Contacts was used after interview to increase completeness of the number of close contacts elicited and accuracy of the contact information. The average number of close contacts elicited per case and the percentage of cases completing the webform were calculated, and user interviews to gather qualitative data were conducted.
Epi Locator
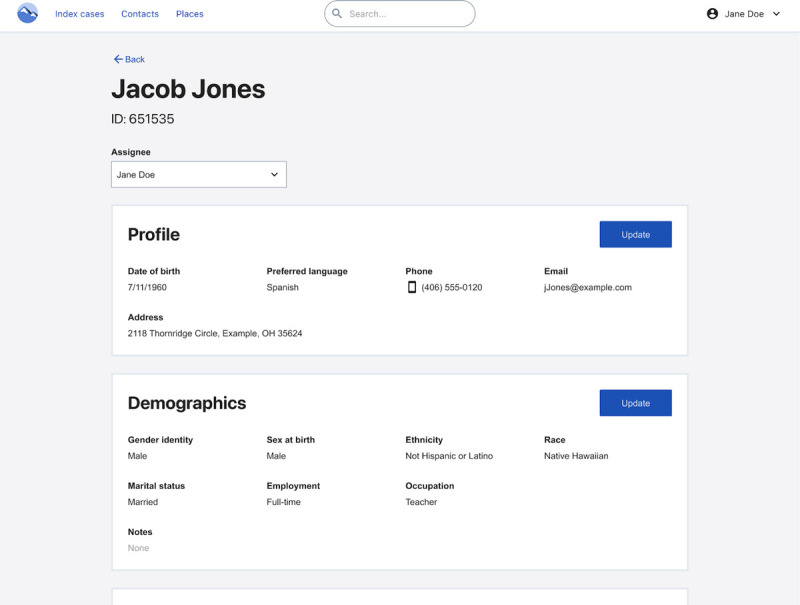
Initially launched in a large state with densely populated urban areas (state B) in August 2020 and state A in November 2020, Epi Locator contact information search (Figs. 2, 3) is a plug-in extension that connects a CMS to third-party investigative tools such as Thomson Reuters CLEAR (Thomson Reuters, Eagan, MN) or LexisNexis Public Records (LexisNexis, New York, NY). Certain search terms were auto-populated and could not be edited (to prevent unethical use), with first and last names as the minimum required search terms. Available demographic information was used, and results were sorted from the most to least likely matches. This workflow enables case investigators and contact tracers to more quickly locate critical missing information—such as a phone number—to reach index cases and close contacts. Epi Locator was developed to provide search access to broader portions of the CI/CT team, thereby decreasing the time to reach an index case or close contact and initiate isolation or quarantine. Epi Locator was available either in a pop-up window or embedded in the CMS, depending on a system's technical capabilities. Investigators could correct person records with updated address and contact information. The total number of person searches and the number of distinct users were calculated.
Figure 2.
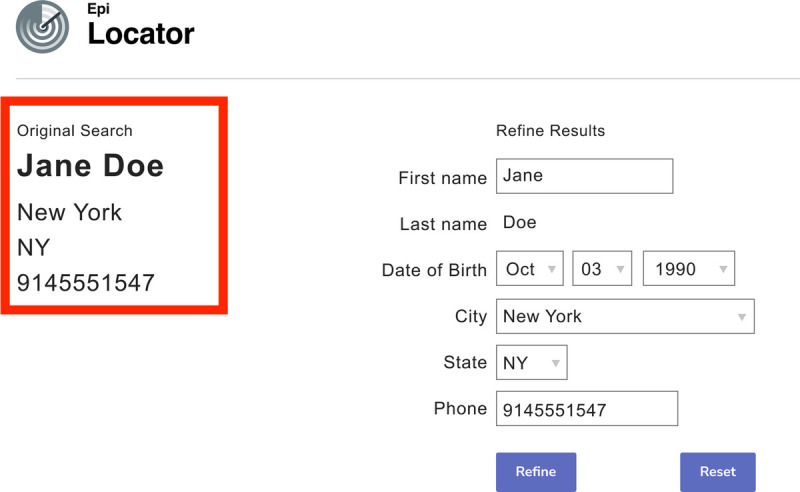
Epi Locator auto-populated search page.
Figure 3.

Epi Locator results display.
Epi Viewpoint
As the RTSL team began working with a smaller suburban county health department (county B), it learned that the county had neither a CMS to effectively manage the scale of COVID-19 cases nor the resources to implement a platform-based CMS. This led to development of Epi Viewpoint: a simple and focused CMS (Figs. 4, 5) designed to enable jurisdictions with smaller populations to quickly and cost-effectively stand up their CI/CT efforts. Design and development of Epi Viewpoint began in June 2020, with a target completed implementation in December 2020. Although it was designed to improve COVID-19 CI/CT, Epi Viewpoint is simple and flexible enough to be applied to other communicable disease CI/CT efforts. Its canonical object is a person record, and an individual can have multiple case and contact records assigned. The initial version used a csv upload to ingest laboratory results, and the ingestion de-duplicated and matched results to existing persons (when applicable).
Figure 4.
Epi Viewpoint 360° Person View.
Figure 5.
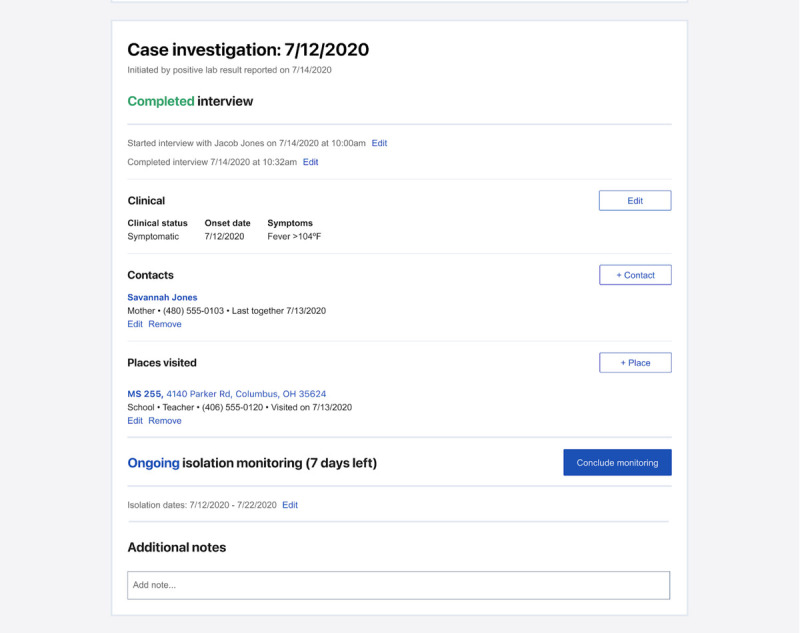
Epi Viewpoint case investigation form.
RESULTS
Epi Viaduct
Development and implementation of the Epi Viaduct data pipeline were completed in 4 months in the first pilot jurisdiction. Epi Viaduct reduced the time interval from laboratory result update in the ELR system to case creation in CMS from 2.5 hours to less than 1 minute. In addition, the time to remove duplicate cases and find missing cases for returned laboratory results was reduced from several days to less than 6 hours. From July 13, 2020, to March 9, 2022, approximately 7,400,000 test results were transmitted via Epi Viaduct in state A. Implementation was completed by 2 people in the department of health programs team and engineers from RTSL's implementation partner Ratio, PBC (Portland, OR).
The original budget allocation for development was $662,000, and the final cost was $572,812. The approximate cost of implementation per jurisdiction is $120,000, whereas the approximate cost of monthly maintenance per jurisdiction is $15,000 for a state and $5000 for a county.
Epi Contacts
Development and implementation of the Epi Contacts contact elicitation webform were completed in county A in 7 months. Epi Contacts implementation in state A was completed 9 months after the initial design sprint. For the period from March 15 to April 13, 2021, in state A, 96,319 (3211 daily average) cases triggered Epi Contacts. Of those, 22.3% of cases (21,540) accessed the application, and 44% of cases accessing the application (9,440) submitted at least 1 contact. On average, 2 contacts were submitted per index case, for a total of approximately 18,700 contacts elicited. On average, 623 contacts were elicited per day.
User interviews indicated that Epi Contacts was useful for contact elicitation. One user stated that Epi contacts would “make it easier when [we're] going through the investigation” if more cases were involved in using the solution. Another user stated that Epi Contacts “makes [case investigation] easier, as it's less steps for us to enter [close contact information].”
In jurisdictions where contact tracing and case investigation run in parallel, Epi Contacts enabled contact tracing to begin immediately after contacts were recorded in the CMS. When case investigation queues were overloaded, Epi Contacts often elicited contact information before case investigations were completed, enabling earlier outreach to identify contacts.
The original budget allocation for Epi Contacts was $250,000 with a final cost of $227,887. Cost of implementation for a jurisdiction is estimated at $90,000 with a monthly maintenance cost of $5000. Additional costs may be incurred for SMS message rates if a bundled SMS agreement or an unlimited data use agreement is not secured.
Epi Locator
Development and implementation of Epi Contacts were completed in state B in 4 months. Epi Locator implementation in state A was completed 7 months after the initial design sprint. In state A, for August 2021, a total of 134,410 searches were run, with 75% of these searches returning 1 or more person matches. Approximately 7320 distinct users completed these searches in this same period.
The original budget allocation for Epi Locator development was $390,000, and the final cost was $216,800. The approximate cost of implementation in a single jurisdiction is $90,000 with a monthly maintenance cost of $5000.
Epi Viewpoint
The Epi Viewpoint CMS development was completed in December 2020 but was not implemented in any jurisdictions. After preparing for Epi Viewpoint implementation for several months, the project experienced a critical setback when a previously unincluded section of the team became involved just before the scheduled launch and stopped the project. The estimated cost of implementation is $120,000 per jurisdiction with monthly maintenance costs between $2500 and $25,000 depending on the size of the jurisdiction.
DISCUSSION
Challenges in COVID-19 data management, integration, and completeness of information created significant time lags, making contact tracing inefficient and labor-intensive, especially during the initial wave of COVID-19. Implementing software during a crisis is challenging. Even when accelerated, implementations typically lag behind the sheer magnitude of a public health crisis such as the COVID-19 pandemic.
The Epi Viaduct data pipeline increased the efficiency of data transfer from an ELR to a CMS, thereby decreasing the interval between specimen collection from a suspected case to initiation of the case investigation (and the eventual beginning of isolation). Although the system was used to specifically transmit results for COVID-19 laboratory tests, any communicable diseases using ELR (including sexually transmitted disease [STDs]) could be automatically transmitted to a CMS if disease control included CI/CT. To add capacity, several states the team worked with had rapidly hired new CI/CT staff who needed to be trained quickly, and once trained, they often experienced an overwhelming volume of work. During the crisis, a familiar user experience requiring less training needed to be prioritized over new features or revised workflows. As a data pipeline tool, Epi Viaduct was easier to implement because it did not have a user interface and did not require extensive staff retraining or process changes.
The Epi Contacts contact elicitation webform was successfully used to automate contact elicitation from confirmed cases for contact tracing. The strongest indication came through qualitative feedback from user interviews indicating that Epi Contacts increased the efficiency of contact tracing by helping to decouple CI/CT. One user stated, “you don't need the case to be interviewed before the contact is called, which is a good thing about the application.” Another CI/CT user indicated the time interval between contact elicitation to close contact outreach: “Now it's like as soon as [close contacts] are entered [we can reach out], but we still tell people 24 hours just in case.”
There is potential to increase form submission with further iteration on verbiage, interface, or even communications campaigns to increase awareness of use of this tool by local public health departments. As engagement increases, this can reduce the burden on case investigators regarding the number of cases they need to investigate or the average time required for investigation of a single case. One case investigator interviewed suggested that Epi Contacts was more comfortable for index cases to share information on close contacts because “[index cases] don't want to tell us anything they can do in the privacy of their own home. They feel more comfortable telling it to an app who the contacts are rather than speaking to someone.”
Epi Contacts could be expanded for several other use cases that arise when CI teams are overcapacity during a surge. The tool could be used to gather more information to help prioritize case interviews or could be used as a “digital case investigation interview” for lower-risk cases (in place of a live case investigation interview), which would likely not be prioritized if capacity was overwhelmed. The tool is CMS agnostic, but the same approach could be used in jurisdictions required to use a single, already-engaged vendor. If a CMS can trigger an SMS message, any ready-built survey tool can be used, rather than using a custom webform. Existing tools created by the National Coalition of STD Directors (Washington, DC) such as tellyourcontacts.org for COVID-19 and tellyourpartner.org for STDs currently allow patients to automatically send exposure notifications to contacts. Epi Contacts builds on this type of functionality by populating the type of data collected on these sites for potential contacts into a CMS used to support case investigation for control of COVID-19 or STDs. These sites could be referenced instead of a bespoke webform; however, the information populated into these sites directly would not be integrated into a CMS.
Metrics from the Epi Locator contact information search plugin support the conclusion that CI/CT teams frequently need access to a lookup database with search functionality. A future iteration of Epi Locator could integrate multiple databases and possibly include registries, such as a state immunization information system, to find matches more quickly and easily when using CI/CT for control of STD transmission. For Epi Locator implementation, pilot jurisdictions already had licenses for a third-party search tool, and the RTSL digital team helped review these contracts to ensure API access was included and cost would not be prohibitive. Jurisdictions should consider the cost of a third-party database if they do not already have licenses for one. Automated programming interface limits should be assessed to ensure they are affordable at the anticipated scale required. Some ethical concerns have been raised because these third-party investigative tools are often used by organizations, which can be intimidating to certain communities,9 including immigrants. Guidelines for use of these technologies should be developed and communicated to the communities who these searches will benefit, to build trust and prevent misuse.
The Epi Viewpoint CMS was not implemented because of misaligned expectations and restrictions on data hosting. Jurisdictions had differing requirements for hosting—some required on-premises hosting, whereas others used various cloud providers—requiring greater investment in ensuring that the solutions could be more easily adapted to whatever environment was appropriate for a given jurisdiction. A future iteration of Epi Viewpoint could leverage a data pipeline, such as Epi Viaduct, to automate the transmission of case and laboratory records. A canonical object for places was designed but not developed once the implementation was stopped in the initial pilot jurisdiction. This would enable place-based investigations and the tracing of potential hotspots. The disease-specific case investigation forms and variables could be used for communicable diseases such as STDs, or the case investigation form could be generalized for any communicable disease case investigation or include logic to show relevant questions based on what confirmed or suspected disease is populated into the case record.
Technology vendors, implementors, and support staff should identify and align with cross-functional decision makers (including representatives of IT/security, program/end users, and procurement) to ensure that public health department requirements and protocols are met. Each project management conversation should regularly affirm that the group includes all necessary personnel and has the authority to make decisions. Unforeseen occurrences (e.g., hiring, staff turnover, promotions) can affect this group, and third parties are not always informed of these changes. Embedding technology staff in a public health department, like embedded program staff, would have enabled the RTSL digital team to identify and quickly solve problems that arose, for example, by creating a more confident map of decision makers and better understanding of the infrastructure and technology requirements the solution would be implemented within. Each project would have benefitted from deeper project planning with jurisdictions to create distinct staff responsibilities and milestones.
Technology has a clear role in improving the speed, scale, and impact of CI/CT. The RTSL digital team implemented these efficiency solutions with public health departments that were proactive and empowered to direct an effective COVID-19 response. Development of these point solutions required a large budget (2.1 million US dollars) given the diversity of technology ecosystems in which they needed to be implemented. The solutions were intended to be agnostic in terms of integrating with a CMS, third-party search database, ELR, or other infrastructure. Once implemented, these solutions could be more quickly adapted for use by CI/CT teams focused on other communicable diseases. In addition, jurisdictions with similar infrastructure could partner on implementations or share lessons to reduce time and cost. It was agreed that any tools developed would be open-sourced to minimize the cost of implementation and maintenance, and so jurisdictions could adapt implementations to their specific technology architecture and CI/CT workflows. If a jurisdiction has limited autonomy, implementation is not feasible, but it is still feasible to assist with technology assessments and recommendations. In discussions with these types of jurisdictions, we shared our design approach so they could mimic the workflows enabled by these point solutions using tooling already available in their technology ecosystem.
Interoperability has been a focus and requirement for health system software, but integration is less straightforward. When evaluating requirements for these new solutions, the RTSL digital team found that many core public health data systems are still largely closed off. Across each of the projects, the biggest technical barrier to implementing and iterating quickly was integration with source and recipient data systems. To keep up with the cloud-based infrastructure many web systems and applications are built on, health system technology stacks should be built with applications that use a modern, public, and well-documented API framework. These APIs offer a level of flexibility that gives public health leaders the ability to adapt to unforeseen needs and allows for greater resiliency of a public health system technology stack.
The team did not consider developing tools or integrations with tools that used automated (Bluetooth/GPS) or crowd-sourced surveillance apps because of the lack of evidence surrounding their efficacy.6
CONSIDERATIONS
Several elementary assumptions underlie the project, namely, that jurisdictions have a basic system for CI/CT (and capacity just needs to be increased), jurisdictions will partner with technology teams as needed to quickly build effective technology, and each jurisdiction will manage their own data, protocol decisions, permissions, and eventually the new technology.
The team maintained that jurisdictions ultimately own their technology choice and that choice should only be a complement to public health programs. In addition, in keeping with RTSL's commitment to disseminate best practices, the team decided that any solutions created would be open-sourced and tool-agnostic for integration.
RESOURCES
Each of the applications discussed is available on Github under an open-source license. For more information about these applications, contact hello@ratiopbc.com.
For more US COVID-19 resources from Resolve to Save Lives, visit https://preventepidemics.org/covid19/us-response/.
Footnotes
Resolve to Save Lives's US COVID Response program was funded by Bloomberg Philanthropies and the #startsmall foundation.
Conflict of Interest and Sources of Funding: None declared.
Contributor Information
Gloria Nuñez, Email: gnunez@resolvetosavelives.org.
Stacy La, Email: stacy.h.la@gmail.com.
Jammal H. Dorsey, Email: jdorsey@resolvetosavelives.org.
Swati Shah Patel, Email: swati.n.shah111@gmail.com.
Karen G. Luk, Email: karenluk@gmail.com.
Kristen Brillantes, Email: kristen@byknb.com.
Rebecca Birnbaum, Email: birnbaum.ra@gmail.com.
Melissa Boyette, Email: frx3@cdc.gov.
Eleanor Peters Bergquist, Email: ebergquist@resolvetosavelives.org.
Amanda McClelland, Email: amcclelland@resolvetosavelives.org.
REFERENCES
- 1.Coronavirus in the U.S.: Latest Map and Case Count (The New York Times Web site). Available at: https://www.nytimes.com/interactive/2021/us/covid-cases.html. Accessed March 11, 2022.
- 2.Reid M Enanoria W Stoltey J, et al. The SARS-CoV-2 pandemic: The race to trace: contact tracing scale-up in San Francisco—early lessons learned. J Public Health Policy 2021; 42:211–221. Available at: https://www.ncbi.nlm.nih.gov/. Accessed March 11, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Banco E. Inside America's COVID-reporting breakdown (Politico Web site). Available at: https://www.politico.com/news/2021/08/15/inside-americas-covid-data-gap-502565. Accessed March 11, 2022.
- 4.Kretzschmar ME Rozhnova G Bootsma MCJ, et al. Impact of delays on effectiveness of contact tracing strategies for COVID-19: A modelling study. Lancet Public Health 2020; 5:e452–e459. Available at: https://www.thelancet.com/. Accessed March 11, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Measures to Improve COVID-19 Response (Resolve to Save Lives Web site). Available at: https://preventepidemics.org/covid19/resources/measures-to-improve-covid-19-response-end-to-end-quality-improvement-of-covid-19-testing-case-investigation-and-contact-tracing/. Accessed February 23, 2022.
- 6.Min-Allah N Alahmed BA Albreek EM, et al. A survey of COVID-19 contact-tracing apps. Comput Biol Med 2021; 137:104787. Available at: https://www.sciencedirect.com. Accessed February 23, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gasser U Ienca M Scheibner J, et al. Lancet Digit Health 2020; 2:e425–e434. Available at: https://www.thelancet.com. Accessed March 11, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Principles of contact tracing: Appendix—Close Contact Atlanta, GA (CDC Web site). Available at: https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/appendix.html#contact. Accessed March 23, 2022.
- 9.Biddle S, Woodman S. These Are the Technology Firms Lining Up to Build Trump's “Extreme Vetting” Program (The Intercept Web site). Available at: https://theintercept.com/2017/08/07/these-are-the-technology-firms-lining-up-to-build-trumps-extreme-vetting-program/. Accessed October 15, 2020.


