Abstract
Introduction:
Lack of access to perinatal mental health (PMH) services is a significant public health problem in India. Barriers to accessing PMH services include the stigma, non-availability of services, poor knowledge, negative perception, attitude among perinatal women (PWs) and service providers. The present study attempted to examine the knowledge gap regarding perinatal depression (PD) among service providers [Nursing providers (NPs), Medical Practitioners (MPs)] and service utilizers (PWs).
Methods:
This cross-sectional study was conducted in two tertiary care teaching hospitals of India, one in a major metro and the other in a rural area. PWs, MPs and NPs were assessed for knowledge about PD using a semi-structured proforma and Perinatal Depression Monitor.
Results:
Among the 270 PWs, 8.51% were knowledgeable (PWA) and 91.49% were ignorant (PWB) about depression. PWB group were low educated (n = 140, 56.68%), and unemployed (n = 207, 83.80%) with lower family income [(≤₹10,356 per month), n = 170, 68.28%)]. There was knowledge discrepancy among NPs, MPs and PWA group in terms of a) PD is a normal part of pregnancy (agree- NPs = 71.52%, MPs = 10.00%, PWA- 17.39%), b)biological causes of PD (agree- NPs = 45.23%, MPs = 70.00%, PWA = 26.03%) and c)anti-depressant medications for PD (useful- NPs = 23.80%, MPs = 70.00%, PWA = 21.73%). Majority of the respondents agreed that all women should be screened for depression during pregnancy (NPs = 34.78%, MPs = 80.95%, PWA = 95.00%) and postpartum periods (NPs = 34.78%, MPs = 76.19%, PWA = 90.00%).
Conclusions:
Low PD literacy among the PWs, misconception about aetiology and management among the NPs could be major barrier for delivery and utilisation of PD services. Thus, there is an urgent need to improve PD literacy among PWs and NPs.
Keywords: Depression, Literacy, Perinatal, Postpartum, Antepartum, Knowledge, Barrier
1. Introduction
Depression accounts for the largest proportion of burden associated with mental and neurological disorders among women during perinatal period (Phoosuwan et al., 2018; Prince et al., 2007; Vos et al., 2012). Women with untreated perinatal depression are at risk of suicide (Tareen and Tandon, 2018), increased economic costs, and their infants are at risk for developmental delays, behavioural problems, mother-infant bonding disorders (Konishi et al., 2018; Miranda and Patel, 2005; Tareen and Tandon, 2018; Vengadavaradan et al., 2019; Wiguna and Ismail, 2019). Early detection and treatment of the perinatal depression improves health-related outcomes among infant and perinatal women (Williams et al., 2016).
Despite an overall increase in research with focus on integration of perinatal mental health into maternal and child health (MCH) Programmes across the world (Reilly et al., 2019), perinatal mental health remains an underemphasized part of MCH programs including the MCH programmes under National Health Mission of India (Harsha and Acharya, 2019; Rahman et al., 2008). Integrative training models based on general medical practitioners, nurses and health visitors were said to be effective in other countries but with limited success in India (Elshatarat et al., 2018; Gajaria and Ravindran, 2018; Noonan et al., 2019). A complex interaction of factors such as awareness about perinatal depression, social determinants of service utilizers, organisation-related issues, financial and administrative support hinders the success of these models in India (Gajaria and Ravindran, 2018; Patel et al., 2004; Ragesh et al., 2017; Townsend et al., 2004). In addition, poor knowledge, negative attitudes, negative perceptions, stigma, cultural issues, negative practices, misconceptions or myths about perinatal depression among higher level service providers (e.g. specialists, general practitioners),mid-level health care providers (nurses, midwives) and service utilizers (perinatal women) play a crucial role in effective implementation and integration of perinatal mental health care delivery (Gawley et al., 2011; Harsha and Acharya, 2019; Lau et al., 2015; Noonan et al., 2019; Rahman et al., 2013; Sofronas et al., 2011).
In India, these factors are highly prevalent and may limit the success of integration of perinatal mental health services into routine care, if not addressed properly. To our knowledge, no published study attempted to explore and compare the knowledge gap among service providers and service utilizers in India. The few published studies focused only on service utilizers (perinatal women) (Manjrekar and Patil, 2018), with limited utility for developing an integrative and collaborative model for perinatal mental health services.
To address this research gap, we aimed to assess the knowledge gap, perceptions, and misconceptions about perinatal depression at three different levels i.e. high-level service providers (e.g. specialists, general practitioners), mid-level health care providers (nurses, midwives) and service utilizers (perinatal women). In addition, we attempted to explore the role of their socio-demographic characteristics with perinatal depression literacy.
2. Materials and methods
2.1. Study sites
We conducted a cross-sectional study in the antenatal care (ANC)/postnatal care (PNC)/outpatient department section (OPD) run by the Department of Obstetrics and Gynecology (OBGY) at Sucheta Kriplani Hospital- Lady Hardinge Medical College(LHMC), New Delhi and at BKL Walawalkar Rural Medical College(BKLWRMC), Ratnagiri District, Maharashtra.
2.2. Study tools
Researchers and experts from Community Medicine, Psychiatry, OBGY and Paediatrics from respective sites developed a semi-structured proforma based on published studies (Highet et al., 2011a) (available with authors). The Questionnaire contained questions from the Perinatal Depression Monitor (Highet et al., 2011b; Kingston et al., 2014), an Australian population-based survey on perinatal mental health; additional questions were developed and translated in local language to reflect the socio-cultural beliefs prevalent in Indian context. The final questionnaire consisted of 26 questions designed to measure population–based awareness, attitudes, and knowledge regarding perinatal mental health. Responses were recorded on a 3 point Likert scale (Agree, Neutral and Disagree). A pilot study was conducted to ascertain the understandability and appropriateness of the questionnaire and the overall feasibility of the study, after which the questionnaires were translated into local language.
2.3. Participants
2.3.1. Perinatal women (PW)
A total of 270 participants (perinatal women) attending the antenatal clinic, were recruited by convenient sampling method. Eligibility criteria to participate in the study were as follows: (a) being 18 years or older, (b) being currently pregnant or having given birth during the previous 12 months. While 20 women participated in the pilot study at each site, 270 women participated in the main study.
2.3.2. Nursing providers (NPs) and medical practitioners (MPs)
Online survey forms were created to assess the knowledge, attitude and practices among service providers, which included any person working in perinatal clinics or indoor services of tertiary care hospital and having qualification of modern medicine (MPs) or any nursing qualification with valid licence with state nursing council (NPs). The survey form consisted of socio-demographic, educational and training details of the health care providers. The online form was circulated through email and WhatsApp groups to collect the data.
2.4. Ethical considerations
This study was approved by the both Institutional Ethics Committees as a part of BIND-P study (Ransing et al., 2018). Written informed consent was obtained from each PW, whereas online consent was obtained from MPs and NPs who answered online questions. No personally identifiable information was requested in the questionnaire.
2.5. Data collection and analysis
Data collection took place over five months (October 2018 to February 2019).Epi - Info 7 WHO software was used for data analysis. Descriptive statistics were computed (means and standard deviations, proportions and percentages) for demographic data and knowledge, attitude statements. Chi-square or Fisher’s exact tests were employed to identify associations between categorical variables and associations were considered statistically significant at the 5% level (p < 0.05).
3. Results
During the pilot study, we observed that perinatal women group could be clearly separated into two groups:
a. Group A (PWA):
Participants having some knowledge about mental illness (e.g. depression, substance use disorder) were able to respond the questions related to perinatal depression.
b. Group B (PWB):
Participants having no knowledge about mental illness (e.g. depression, substance use) failed to answer the questions related to perinatal depression.
Based on this observation, participants who were ignorant about mental illness were not asked about perinatal mental illness.
3.1. Demographic characteristics of participants
3.1.1. Perinatal women
Out of 270 perinatal women (BKLWRMC –ANC (n = 112), PNC (n = 102), LHMC, n = 51), only 23 (8.51%) responded that they had some knowledge about depression and therefore, were asked further questions pertaining to perinatal depression.
3.1.2. Group A perinatal women (PWA)
The mean age of the participants was 26.39 ± 3.72 years. Of the 23, all belonged to Hindu religion, 16 (69.56%) were unemployed, 16 (69.56%) were educated post- high school (> 10 years of schooling). Among them, 18 (78.26%) resided in urban areas and 16 (69.56%) had a family income of > Rs.10,356 per month. Of the 23 PWA, 15 (65.21%) were primigravidae.
3.1.3. Group B perinatal women (PWB)
Among PWB, mean age was 26.07 ± 4.18years. Of the 247, 216 (87.44%) were Hindus and 140 (56.68%) were educated below high school (< 10 years of schooling). Majority (n = 170, 68.82%) hailed from rural areas and had a monthly family income of ≤ Rs.10,356 per month. Of the 247 PWB, 129 (52.22%) were multigravida.
3.1.4. Nursing providers (NPs)
Mean age of NPs was 24.86 ± 3.76 years. Of the 42 NPs who answered our online survey, 33 (78%) had completed their ANM (Auxiliary Nurse Midwifery) /GNM (General Nursing and Midwifery) training while 9 (22%) had completed their nursing degree. Their average experience was 43.17 months. Of the 42, 15 (35.71%) were engaged in perinatal health care (antenatal/postnatal/neonatal care), while 22 (52.38%) were performing general duties in the hospital and 5 (11.90%) were engaged in community services.
3.1.5. Medical practitioners (MPs)
The mean age of MPs who answered the online survey was 31.8 ± 9.88 years. Of the 20 MPs, 17 (85%) were specialists while 3 (15%) were general practitioners. Of the 17 specialists, 10 (50%) were psychiatrists. The average years of practice was 9.52 years. Most worked in urban areas as compared to rural areas (n = 12, 60% vs n = 8, 40%).
3.1.6. Knowldge gap among three groups
There was significant difference among the three groups (PWA, NPs and MPs) in terms of estimates of prevalence of perinatal depression during antenatal and postnatal period (Table 1). Symptoms such as feeling low or down, unable to cope with life, relationship breakdown were well recognized as symptoms of depression among all three groups, while the PWA group did not consider change in appetite, sleep problems, feeling tired or no energy as symptoms of depression. Counseling or psychotherapy were well accepted treatment modalities among all three groups for perinatal depression. The PWAs and NPs did not consider antidepressant drugs as treatment of choice and differed in this aspect from MPs. (Appendix A. Supplementary data)
Table 1.
Awareness about the perinatal depression (Prevalance).
| PWA (n = 23) | NP (n = 42) | MP (n = 20) | Statistical significance | ||
|---|---|---|---|---|---|
|
|
|
||||
| Prevalence of depression in the antenatal period | Affects 5% | 4 (17.39%) | 12 (28.57%) | 3 (15.00%) | χ2 = 22.97, df = 8, p = 0.0034 |
| Affects 15% | 3 (13.04%) | 07 (16.66%) | 9 (45.00%) | ||
| Affects 30% | 2 (8.69%) | 13 (30.95%) | 4 (20.00%) | ||
| Affects 50% | 9 (39.13%) | 03 (7.14%) | 4 (20.00%) | ||
| Don’t Know | 5 (21.73%) | 07 (16.66%) | 00 (0.00%) | ||
| Prevalence of depression in the antenatal period | Affects 5% | 4 (17.39%) | 10 (23.80%) | 0 (0.00%) | χ2 = 16.63, df = 8, p = 0.03 |
| Affects 15% | 1 (4.34%) | 09 (21.42%) | 8 (40.00%) | ||
| Affects 30% | 5 (21.73%) | 07 (16.66%) | 7 (35.00%) | ||
| Affects 50% | 4 (17.39%) | 03 (7.14%) | 1 (5.00%) | ||
| Don’t know | 9 (39.13%) | 13 (30.95%) | 4 (20.00%) | ||
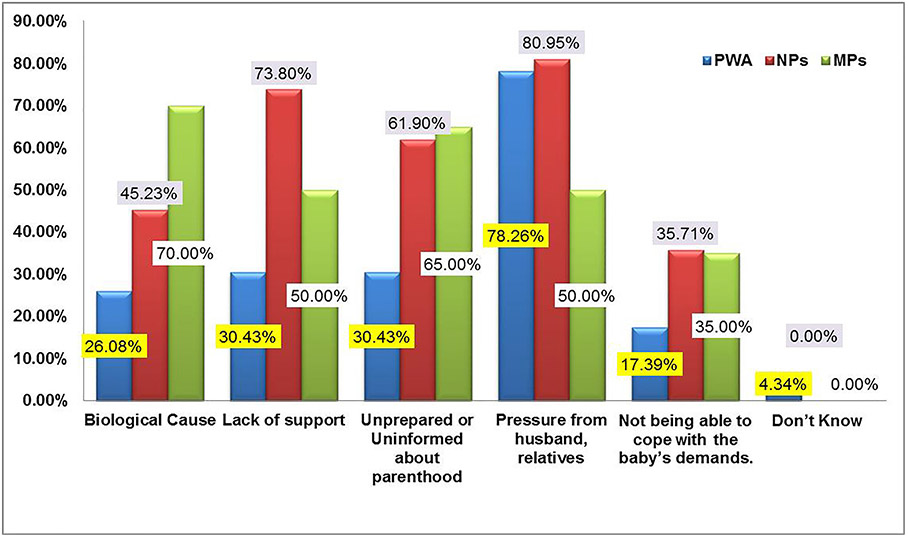
MPs agreement was highest for biological causes of depression (n = 14, 70%) as compared to the NPs (n = 19, 45.23%) and PWAs (n = 6, 26.03%) (Fig. 1). A larger proportion of NPs (n = 34, 80.95%) and PWAs (n = 18, 78.26%) stated that pressure from husband and in-laws for work and wish for male child were causes of perinatal depression than MPs (n = 10, 50%) Majority of NPs (n = 31, 73.08%) considered the lack of support from relatives as a causative factor for perinatal depression when compared to MPs (n = 6, 26.03%) and PWAs (n = 7, 30.43%). A high proportion of MPs (n = 13, 65%) and NPs (n = 26, 61.90%) considered being unprepared for parenthood as a cause for depression when compared to PWA (n = 7, 30.43%). One PWA (4.34%) reported that she was unaware about the cause of perinatal depression.
Fig. 1.
Etiology of Perinatal Depression (%).
Most PWAs and NPs opined that perinatal depression was a normal part of pregnancy and non –serious. Among the causes, PWA (n = 5, 21.73%) felt that effect of god/ devils caused postnatal depression. Most NPs mentioned unrealistic expectations from perinatal women (n = 27, 64.28%) and inability to cope with motherhood (n = 24, 57.14%) as common causes for perinatal depression when compared to the MPs. Both MPs and NPs disagreed that only working women may develop perinatal depression (n = 35, NPs = 83.33% ; n = 14,MPs = 70.00%) (Table 2).
Table 2.
Knowledge about the Perinatal Depression (Normality and Etiology).
| PWA (n = 23) | NP (n = 42) | MP (n = 20) | Statistical significance | ||
|---|---|---|---|---|---|
|
|
|
||||
| Knowledge gap related to normality | |||||
| It’s normal for women to feel depressed during pregnancy | Disagree | 9 (39.13%) | 08 (19.04%) | 12 (60.00%) | χ2 = 31.35, df = 4, p < 0.0001 |
| Neutral | 10 (43.47%) | 04 (9.52%) | 6 (30.00%) | ||
| Agree | 4(17.39%) | 30 (71.52%) | 2 (10.00%) | ||
| Postnatal depression is a normal part of having a baby | Disagree | 10 (43.47%) | 16 (38.09%) | 15 (75.00%) | χ2 = 48.33, df = 4, p < 0.0001 |
| Neutral | 12 (52.17%) | 00 (0.00%) | 5 (25.00%) | ||
| Agree | 1 (4.34%) | 26 (61.90%) | 0 (0.00%) | ||
| Knowing how to look after a baby comes naturally to women | Disagree | 3 (13.04%) | 04 (9.51%) | 13 (65.00%) | χ2 = 39.51, df = 4, p < 0.0001 |
| Neutral | 2 (8.69%) | 00 (0.00%) | 5 (25.00%) | ||
| Agree | 10 (43.47%) | 38 (90.47%) | 2 (10.00%) | ||
| Postnatal depression is not serious. | Disagree | 9 (39.13%) | 16 (38.09%) | 18 (90.00%) | χ2 = 41.63, df = 4, p < 0.0001 |
| Neutral | 10 (43.47%) | 01(2.38%) | 1 (5.00%) | ||
| Agree | 4 (17.39%) | 25 (59.52%) | 1 (5.00%) | ||
| Causes of Perinatal Depression | |||||
| Women get postnatal depression because they can’t cope with motherhood | Disagree | 5 (21.73%) | 13 (30.95%) | 10 (50.00%) | χ2 = 20.4, df = 4, p = 0.0004 |
| Neutral | 13 (56.52%) | 5 (11.90%) | 3 (15.00%) | ||
| Agree | 5 (21.97%) | 24 (57.14%) | 7 (35.00%) | ||
| Women get postnatal depression because they have unrealistic expectations | Disagree | 9 (39.13%) | 9 (21.42%) | 13 (65.00%) | χ2 = 16.37, df = 4, p = 0.0026 |
| Neutral | 7 (30.43%) | 6 (14.28%) | 2 (10.00%) | ||
| Agree | 7 (30.43%) | 27 (64.28%) | 5 (25.00%) | ||
| Bad effect of Gods/devils causes postnatal depression | Disagree | 14 (60.86%) | 42 (100.00%) | 20 (100.00%) | NA |
| Neutral | 4 (17.39%) | 0 (0.00%) | 0 (0.00%) | ||
| Agree | 5 (21.73%) | 0 (0.00%) | 0(0.00%) | ||
| Only career women get postnatal depression | Disagree | 9 (39.13%) | 35 (83.33%) | 14 (70.00%) | χ2 = 19.64, df = 4, p = 0.0006 |
| Neutral | 10 (43.47%) | 1 (2.38%) | 3 (15.00%) | ||
| Agree | 4 (17.39%) | 6 (14.28%) | 3 (15.00%) | ||
The NPs agreed that only severe symptoms such as suicide (n = 19, 45.23%) or wish to harm /kill the child (n = 14, 33.33%) were indicative of postnatal depression, while most MPs disagreed (Table 3). All PWAs neither agreed nor disagreed with beliefs such as ‘postnatal depression did not exist in previous generations’, ‘postnatal depression is a sign of weakness and ‘women choose to get postnatal depression’. In addition, NPs largely agreed that ‘postnatal depression was a sign of weakness’ (n = 18,42.85%) and ‘women choose to get postnatal depression’ (n = 20, 47.61%).
Table 3.
Knowledge about Perinatal Depression (Myths and symptoms).
| PWA (n = 23) | NP (n = 42) | MP (n = 20) | Statistical significance | ||
|---|---|---|---|---|---|
|
|
|
||||
| Myth | |||||
| Postnatal depression didn’t exist in previous generations | Disagree | 6 (26.08%) | 27 (64.28%) | 16 (80.00%) | χ2 = 21.21, df = 4, ρ = 0.0003 |
| Neutral | 9 (39.13%) | 02 (4.76%) | 3 (15.00%) | ||
| Agree | 8 (34.78%) | 13 (30.92%) | 1(5.00%) | ||
| Postnatal depression is a sign of weakness | Disagree | 8 (34.78%) | 20 (47.61%) | 15 (75.00%) | χ2 = 15.56, df = 4, ρ = 0.0037 |
| Neutral | 9 (39.13%) | 4 (9.52%) | 1 (5.00%) | ||
| Agree | 7 (30.43%) | 18 (42.85%) | 4 (20.00%) | ||
| Women choose to get postnatal depression. | Disagree | 10 (43.47%) | 17 (40.47%) | 17 (85.00%) | χ2 = 19.45, df = 4, ρ = 0.0006 |
| Neutral | 8 (34.78%) | 5(11.90%) | 1(5.00%) | ||
| Agree | 5 (21.73%) | 20 (47.61%) | 2 (10.00%) | ||
| Symptoms | |||||
| It is only postnatal depression when you want to harm or kill the child. | Disagree | 7 (30.43%) | 23 (54.76%) | 17 (85.00%) | χ2 = 14.71, df = 4, ρ = 0.0054 |
| Neutral | 7 (30.43%) | 5 (11.90%) | 2 (10.00%) | ||
| Agree | 9 (39.13%) | 14(33.33%) | 1 (5.00%) | ||
| It is only postnatal depression when you’re thinking about suicide | Disagree | 10 (43.47%) | 15 (35.71%) | 17 (85.00%) | χ2 = 27.33, df = 4, ρ < 0.0001 |
| Neutral | 11 (47.42%) | 8 (19.04%) | 3 (15.00%) | ||
| Agree | 2 (8.69%) | 19 (45.23%) | 0 (0.00%) | ||
Most NPs agreed that ‘postnatal depression will go away as the child grows older’ (n = 30, 71.42%) and ‘only weak women take drugs for postnatal depression’ (n = 24, 57.14%) (Table 4). However, most NPs and MPs disagreed that perinatal depression is untreatable (n = 34, 80.95% Vs n = 19, 95.00%) and women with postnatal depression cannot be good mothers (n = 32, 76.19% Vs n = 18, 90.00%). All NPs and MPs disagreed that perinatal depression needs to be treated by Tantriks (magico-religious practitioners) or faith healers (n = 42, 100% Vs n = 20, 100%). Further, maximum NPs and MPs agreed that all women should be checked for depression during pregnancy (n = 34, 80.95 vs. n = 19, 95.00%) and after birth of the child (n = 32, 76.19% vs. n = 18, 90.00%).
Table 4.
Knowledge about the Perinatal Depression (Treatment and Outcome).
| Treatment for Postnatal/Perinatal Depression | PWA (n = 23) | NP (n = 42) | MP (n = 20) | Statistical significance | |
|---|---|---|---|---|---|
|
|
|
||||
| Treatment for Postnatal/Perinatal Depression | |||||
| Postnatal depression requires special treatment. | Disagree | 6 (26.08%) | 11(26.19%) | 1(5.00%) | χ2 = 16.23, df = 4, p = 0.0027 |
| Neutral | 7 (30.47%) | 01(30.43) | 2 (10.00%) | ||
| Agree | 10 (43.47%) | 30 (43.47%) | 17 (85.00%) | ||
| Postnatal depression will go away on its own as the baby gets older | Disagree | 6 (26.08%) | 07 (16.66%) | 14 (70.00%) | χ2 = 40.24, df = 4, p < 0.0001 |
| Neutral | 13 (56.52%) | 05 (11.90%) | 3 (15.00%) | ||
| Agree | 4 (17.39%) | 30 (71.42%) | 3 (15.00%) | ||
| Women who take medication for postnatal depression are weak willed | Disagree | 5 (21.73%) | 12 (28.57%) | 16 (80.00%) | χ2 = 29.46, df = 4, p < 0.0001 |
| Neutral | 11 (47.82%) | 06 (14.28%) | 1(5.00%) | ||
| Agree | 7 (30.43%) | 24 (57.14%) | 3 (15.00%) | ||
| Perinatal depression is untreatable condition | Disagree | 11 (47.82%) | 34 (80.95%) | 19 (95.00%) | χ2 = 14.38, df = 4, p = 0.006 |
| Neutral | 8 (34.78%) | 5 (11.90%) | 1 (5.00%) | ||
| Agree | 4 (17.39%) | 3 (7.14%) | 0 (0.00%) | ||
| Perinatal depression can be treated by faith Healers/tantrik | Disagree | 16 (69.56%) | 42 (100%) | 20 (100%) | NA |
| Neutral | 4 (17.39%) | 0 (0.00%) | 0 (0.00%) | ||
| Agree | 3 (13.04%) | 0 (0.00%) | 0 (0.00%) | ||
| Professional help is needed for perinatal depression. | Disagree | 3 (13.04%) | 2 (4.76%) | 1 (5.00%) | χ2 = 19.08, df = 4, p = 0.0008 |
| Neutral | 12 (52.17%) | 7 (16.66%) | 1 (5.00%) | ||
| Agree | 8 (34.78%) | 33 (78.57%) | 18 (90.00%) | ||
| Prevention | |||||
| All women should be checked for depression during pregnancy | Disagree | 10 (43.47%) | 4 (9.52%) | 0 (0.00%) | χ2 = 23.99, df = 4, p < 0.0001 |
| Neutral | 5 (21.73%) | 4 (9.52%) | 1 (5.00%) | ||
| Agree | 8 (34.78%) | 34 (80.95%) | 19 (95.00%) | ||
| All women should be checked for depression after the baby is born. | Disagree | 9 (39.13%) | 5 (11.90%) | 1 (5.00%) | χ2 = 17.82, df = 4, p = 0.0013 |
| Neutral | 6 (26.08%) | 5 (11.90%) | 1 (5.00%) | ||
| Agree | 8 (34.78%) | 32 (76.19%) | 18 (90.00%) | ||
| Women with postnatal depression can’t be good mothers. | Disagree | 12 (52.17%) | 32 (76.19%) | 18 (90.00%) | χ2 =22.25, df = 4, p = 0.0002 |
| Neutral | 9 (39.13%) | 1 (2.38%) | 1 (5.00%) | ||
| Agree | 2 (8.69%) | 9 (21.42%) | 1 (5.00%) | ||
4. Discussion
We conducted this study to assess the knowledge gap about perinatal depression among different groups like PWs, NPs and MPs in tertiary care settings. We used questions from the Perinatal Depression Monitor (Highet et al., 2011b; Kingston et al., 2014). This questionnaire was used in previously conducted Australian and Canadian surveys to assess perinatal depression literacy among general population (Highet et al., 2011b; Kingston et al., 2014). Further, we formulated certain specific questions, based on socio-cultural beliefs that are prevalent in India. (e.g. perinatal depression can be treated by faith healers/Tantriks.
Responses on any Likert scale (e.g. perinatal depression monitor) are known to be influenced by response to previous questions and respondents often tend to choose the extreme options (i.e. disagree, or agree than neutral). Thus, it is said that such scales often fail to measure the true attitude of respondent. (Likert, 1932) To avoid these errors and to confirm responses from participants, we designed semi-structured questions (e.g. what are the symptoms of perinatal depression?) with the help of experts from Psychiatry, Obstetrics, Community Medicine and Pediatrics. (Appendix A. Supplementary data) These questions provided us an insight about the cultural beliefs such as not discussing about pregnancy in the first three months with anyone except family members (Ratnagiri- a rural centre). PWs in both the centers were not interested in answering these questions. The main reasons for their unwillingness were overcrowded ANC OPD, more concern about physical illness of the child, stigma and lack of awareness about perinatal depression. On the other hand, responses from NPs and MPs were collected online without collecting demographic details to ensure confidentiality and anonymity. Snowball sampling (chain referral) method was used for data collection among NPs and MPs. There is a possibility that non-interested participants might not have forwarded this questionnaire to relevant participants, thus skewing towards respondents with positive attitudes.
Our respondents had lower level of depression literacy (only 8.51% said they knew what depression was). This finding was consistent with other studies from Portugal (Fonseca et al., 2017), Australia (Highet et al., 2011b), and college students in India (29.04%) (Ogorchukwu et al., 2016). Poor knowledge about depression and treatment options creates barriers to help seeking behaviour during the perinatal period (Barney et al., 2006). On the contrary, any improvement in mental health literacy positively affects helping behaviour, reduces stigmatising attitudes and helps to overcome practical barriers to help seeking (Highet et al., 2011b).
Women with modest level of knowledge about perinatal depression were mostly educated, of higher socio-economic status, hailing from urban regions and employed, similar to previous studies (Fonseca et al., 2017; Highet et al., 2011b; Kingston et al., 2014). In our own sample of perinatal women, knowledge level among service users (PWA), mid-level service provider (NPs) and high level service provider (MPs) differed with NPs and MPs being more knowledgeable, as expected. Yet gaps were present. For instance, the disparity that we observed among the PWs and NPs when compared to MPs was that postnatal or prenatal depression is non-serious illness and normal part of pregnancy. This is could be a major deterrent to help-seeking behaviour. Though NPs generally had supportive attitude towards perinatal depression screening, but it may not be sufficient to achieve universal screening of perinatal women due to existing disparity in knowledge among the three groups; and patient barriers such as limited or no prenatal care, refusal of screening (Kim et al., 2009). In our study, 64.28% of NPs and 30.43% of PWAs agreed that women with postnatal depression have unrealistic expectations. Some NPs and PWAs agreed that inability to cope with motherhood, career and bad effects of gods/devils were important causes of perinatal depression. This limited understanding of determinants of perinatal depression among women care seekers (PWA) and health care providers (NPs) is consistent with published studies from Australia and Canada (Highet et al., 2011b; Kingston et al., 2014).
We found that a larger proportion NPs and PWAs considered pressure from husband and in-laws for work, uninformed or unplanned parenthood and wish for male child as causes of perinatal depression. Postpartum depression was predicted by the occurrence of unplanned pregnancy, preference to male child and negative relationship with husband, as reported in other studies (Mbawa et al., 2018; Phoosuwan et al., 2018)
Contrary to our finding, the key observation from an older Australian study was that most of primary causes of perinatal mental health problems are biological in nature (Highet et al., 2011b). Failure to recognize the role of biological causes of perinatal depression may be the reason for non-consideration of biological therapy (e.g. anti-depressants) by NPs and PWAs in our sample. However, NPs and PWAs considered non-biological therapies (counselling or social support) as important modalities of treatment.
These findings provide an opportunity to develop social-culturally accepted psychological interventions to implement the screening of perinatal women for depression. Further, these findings suggest that NPs might be holding a stigma or negative attitude towards antidepressants, similar to studies from Canada and Nigeria (Gawley et al., 2011; Ogunsemi et al., 2008). On other hand, this could be due to misinformation about antidepressants in India. Also, 21.73% PWAs agree that bad effect of Gods/devils caused postnatal depression, which is lower than a study conducted in Karnataka. (Manjrekar and Patil, 2018) This difference may be due to inclusion of mixed population (urban and rural), antenatal and postnatal women in our study.
All three groups agreed that PW should be screened for depression during pregnancy and after delivery. In a Canadian study, majority of men and non-pregnant women agreed that all women should be screened for depression in the prenatal (63.0%) and postpartum periods (72.7%) (Kingston et al., 2014). Further, over 80% Australian men and women believed that all new mothers should be routinely assessed for depression (Gemmill et al., 2006; Highet et al., 2011b). This finding is much higher than ours despite including only perinatal women with some knowledge about depression, whereas Canadian and Australian respondents were mostly adults of both genders. This may be attributed to stigma, gender related issues and misinformation about perinatal depression in India (Harsha and Acharya, 2019). Moreover, most NPs considered prevalence of perinatal depression to be higher during postnatal period than antenatal period and believed that screening should be done during pregnancy than after birth of the child. This could be due to perception among the NPs that postnatal depression is a normal part of pregnancy or misunderstanding about postnatal depression being only postpartum blues. However, this needs to be explored further.
NPs play a vital role in the provision of maternal health services including family planning under National Health Mission of Government of India. (Malik, 2009) Further, they are more trusted, they understand the local culture and provide service to their local communities for health promotion, prevention and early detection of diseases, and development of health literacy. For the integration of perinatal mental health care into the routine care, there is a need of a multilevel intervention. The NPs (mid-level health service provider) based integration may be more progressive, replicable and scalable than low-level service provider (e.g. grass roots worker or lay counsellor) or high–level service provider (e.g. Medical Practitioner) who are scarce on the ground in India (Chuffo Siewert et al., 2015; Cox et al., 2017; Fuhr et al., 2019; Harvey et al., 2012; Rock, 2018). Nurse-based collaborative Perinatal Depression Models were found to be effective in screening and referral of PW with depression in the mental health services. They improved accessibility, availability of mental health services and helped overcome personal barriers (negative views of mental health and treatment) (Chuffo Siewert et al., 2015; Cox et al., 2017; Harvey et al., 2012; Rock, 2018)
But, the discrepancies in knowledge, misconception, and misinformation about perinatal depression among the three groups may limit the success of NP-based collaborative model in India. Also, this could be an important underlying cause for non-consideration of routine screening of perinatal depression. For example, if NPs are misinformed that depression is normal part of pregnancy or depressed perinatal women are weak-willed, then PW might not be referred to appropriate mental health services. Therefore, training of nurses about perinatal depression should go hand in hand with creating awareness for depression among the perinatal women. In addition, there should be a uniform and unique module to educate NPs to create positive attitude and awareness about this condition. This would help to reduce wrong and stigmatising attitudes in the community.
Improved mental health literacy among NPs and PWs will promote early identification of mental disorders, improve mental health outcome, facilitate utilization of health services and empower the community to achieve better mental health under the existing National Health Mission (Srivastava et al., 2016). Thus, our findings suggest that there should be strategies such as education, screening procedures for perinatal depression and flipcharts in routine practice to increase perinatal depression literacy.
5. Strengths and limitations
This study findings highlight that treatment and management of perinatal depression is still an underemphasized field receiving little attention. Furthermore, misinformation as well as incomplete knowledge and negative attitudes among professionals (NPs) complicates this issue. Policy makers should provide basic training about perinatal depression to ensure adequate, credible information and mental health services for perinatal women. Convenience sampling, small sample size, non-validated questions in expanded revised scale and perinatal women from tertiary care settings were our main study constraints. The methodological approach (online survey) and snowball sampling may have biased the NPs and MPs sample with inclusion of particular region and English proficient participants.
6. Conclusion
This study demonstrated misconceptions, misinformation and lack of awareness about perinatal depression (such as perinatal depression is normal part of pregnancy, or requires special treatment, women are weak willed) among PWs and NPs. It is one of the primary barriers for integration of perinatal depression services in routine perinatal care. Our recommendations include strengthening public awareness of perinatal depression and developing brief, universal awareness training module especially for NPs (mid-level service providers). Further research should examine the effect of training of NPs on perinatal depression literacy, screening, referral and treatment patterns for perinatal depression.
Supplementary Material
Acknowledgements
This work is part of BIND-P project (CTRI/2018/07/014836) under the Capacity Building group of NCD- ICMR. The work was supported by the Indian Council Medical Research (ICMR) under Capacity Building Projects for National Mental Health Programme, ICMR-NMHP. We thank Dr. Soumya Swaminathan (then Secretary, Dept. of Health Research, DHR), Dr. Balram Bhargav, current Secretary DHR, Prof. V.L. Nimgaonkar, Dr. Ravinder Singh, Dr. Harpreet Singh and Dr. Krushnaji Kulkarni. We thank the faculty of ‘Cross-Fertilized Research Training for New Investigators in India and Egypt’ (D43 TW009114, HMSC File No. Indo-Foreign/35/M/2012-NCD-1, funded by Fogarty International Centre, NIH). We are also thankful to National Coordinating Unit of ICMR for NMHP Projects for their constant support and guidance. We thank Data Management Unit of ICMR for designing the database. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of NIH or ICMR. NIH and ICMR had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations:
- PW
perinatal women
- PWA
perinatal women group A
- PWB
perinatal women group B
- MPs
medical practitioners
- NPs
nursing providers
- ANC
antenatal care
- PNC
postnatal care
- ANM
auxiliary nurse midwives
- OBGY
obstetrics and gynecology
Footnotes
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ajp.2019.10.002.
Financial disclosure
None.
Declaration of Competing Interest
None
References
- Barney LJ, Griffiths KM, Jorm AF, Christensen H, 2006. Stigma about depression and its impact on help-seeking intentions. Aust. N. Z. J. Psychiatry 40, 51–54. [DOI] [PubMed] [Google Scholar]
- Chuffo Siewert R, Cline M, Segre LS, 2015. Implementation of an innovative nurse-delivered depression intervention for mothers of NICU infants. Adv. Neonatal Care 15, 104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox EQ, Raines C, Kimmel M, Richardson E, Stuebe A, Meltzer-Brody S, 2017. Comprehensive integrated care model to improve maternal mental health. J. Obstet. Gynecol. Neonatal Nurs 46, 923–930. [DOI] [PubMed] [Google Scholar]
- Elshatarat RA, Yacoub MI, Saleh ZT, Ebeid IA, Abu Raddaha AH, Al-Za’areer MS, Maabreh RS, 2018. Perinatal Nurses’ and Midwives’ Knowledge About Assessment and Management of Postpartum Depression. J Psychosoc Nurs Ment Health Serv 56, 36–46. [DOI] [PubMed] [Google Scholar]
- Fonseca A, Silva S, Canavarro MC, 2017. Depression literacy and awareness of psychopathological symptoms during the perinatal period. J. Obstet. Gynecol. Neonatal Nurs 46, 197–208. [DOI] [PubMed] [Google Scholar]
- Fuhr DC, Weobong B, Lazarus A, Vanobberghen F, Weiss HA, Singla DR, Tabana H, Afonso E, De Sa A, D’Souza E, Joshi A, Korgaonkar P, Krishna R, Price LN, Rahman A, Patel V, 2019. Delivering the thinking Healthy Programme for perinatal depression through peers: an individually randomised controlled trial in India. Lancet Psychiatry 6, 115–127. [DOI] [PubMed] [Google Scholar]
- Gajaria A, Ravindran AV, 2018. Interventions for perinatal depression in low and middle-income countries: a systematic review. Asian J. Psychiatr 37, 112–120. [DOI] [PubMed] [Google Scholar]
- Gawley L, Einarson A, Bowen A, 2011. Stigma and attitudes towards antenatal depression and antidepressant use during pregnancy in healthcare students. Adv. Health Sci. Educ. Theory Pract 16, 669–679. [DOI] [PubMed] [Google Scholar]
- Gemmill AW, Leigh B, Ericksen J, Milgrom J, 2006. A survey of the clinical acceptability of screening for postnatal depression in depressed and non-depressed women. BMC Public Health 6, 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harsha G, Acharya M, 2019. Trajectory of perinatal mental health in India. 35, 47–54. [Google Scholar]
- Harvey ST, Fisher LJ, Green VM, 2012. Evaluating the clinical efficacy of a primary care-focused, nurse-led, consultation liaison model for perinatal mental health. Int. J. Ment. Health Nurs 21, 75–81. [DOI] [PubMed] [Google Scholar]
- Highet N, Purtell CJJ, Health C, 2011a. What australians know about perinatal depression and anxiety: a043. J. Paediatr. Child Health 47, 20. [Google Scholar]
- Highet NJ, Gemmill AW, Milgrom J, 2011b. Depression in the perinatal period: awareness, attitudes and knowledge in the Australian population. Aust. N. Z. J. Psychiatry 45, 223–231. [DOI] [PubMed] [Google Scholar]
- Kim JJ, La Porte LM, Adams MG, Gordon TE, Kuendig JM, Silver RK, 2009. Obstetric care provider engagement in a perinatal depression screening program. Arch. Womens Ment. Health 12, 167–172. [DOI] [PubMed] [Google Scholar]
- Kingston D, McDonald S, Tough S, Austin MP, Hegadoren K, Lasiuk G, 2014. Public views of acceptability of perinatal mental health screening and treatment preference: a population based survey. BMC Pregnancy Childbirth 14, 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konishi A, So R, Yoshimura B, 2018. Mother-infant separation among mothers with mental illness: an exploratory observational study in Japan. Asian J. Psychiatr 32,1–4. [DOI] [PubMed] [Google Scholar]
- Lau R, McCauley K, Barnfield J, Moss C, Cross W, 2015. Attitudes of midwives and maternal child health nurses towards suicide: a cross-sectional study. Int. J. Ment. Health Nurs 24, 561–568. [DOI] [PubMed] [Google Scholar]
- Likert R, 1932. A technique for the measurement of attitudes. Arch. Psychol 22 (140) 55–55. [Google Scholar]
- Malik G, 2009. Role of auxiliary nurse midwives in national rural health mission. Nurs. J. India 100, 88–90. [PubMed] [Google Scholar]
- Manjrekar S, Patil S, 2018. Perception and attitude toward mental illness in antenatal mothers in rural population of southern india: a cross-sectional study. J. Neurosci. Rural Pract 9, 473–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbawa M, Vidmar J, Chingwaru C, Chingwaru W, 2018. Understanding postpartum depression in adolescent mothers in Mashonaland Central and Bulawayo Provinces of Zimbabwe. Asian J. Psychiatr 32, 147–150. [DOI] [PubMed] [Google Scholar]
- Miranda JJ, Patel V, 2005. Achieving the Millennium Development Goals: does mental health play a role? PLoS Med. 2 e291–e291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noonan M, Galvin R, Jomeen J, Doody O, 2019. Public health nurses’ perinatal mental health training needs: a cross sectional survey. J. Adv. Nurs 10.1111/jan.l4013. [DOI] [PubMed] [Google Scholar]
- Ogorchukwu JM, Sekaran VC, Nair S, Ashok L, 2016. Mental health literacy among late adolescents in South India: what they know and what attitudes drive them. Indian J. Psychol. Med 38, 234–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogunsemi OO, Odusan O, Olatawura MO, 2008. Stigmatising attitude of medical students towards a psychiatry label. Ann. Gen. Psychiatry 7 15–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Araya R, Bolton P, 2004. Treating depression in the developing world. Trop. Med. Int. Health 9, 539–541. [DOI] [PubMed] [Google Scholar]
- Phoosuwan N, Eriksson L, Lundberg PC, 2018. Antenatal depressive symptoms during late pregnancy among women in a north-eastern province of Thailand: prevalence and associated factors. Asian J. Psychiatr 36, 102–107. [DOI] [PubMed] [Google Scholar]
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A, 2007. No health without mental health. Lancet 370, 859–877. [DOI] [PubMed] [Google Scholar]
- Ragesh G, Sajitha K, Hamza A, 2017. Context and scope of social work interventions in perinatal mental health settings in India. Asian Soc. Work. Policy Rev 11, 102–104. [Google Scholar]
- Rahman A, Patel V, Maselko J, Kirkwood B, 2008. The neglected’ m’ in MCH programmes-why mental health of mothers is important for child nutrition. Trop. Med. Int. Health 13, 579–583. [DOI] [PubMed] [Google Scholar]
- Rahman A, Surkan PJ, Cayetano CE, Rwagatare P, Dickson KE, 2013. Grand challenges: integrating maternal mental health into maternal and child health programmes. PLoS Med. 10 e1001442–e1001442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransing R, Prerna Kukreti, Pracheth Raghuveer, Mahesh M, 2018. A Multi-Centric Randomized Controlled Trial to Assess Effectiveness of the Brief Nursing Intervention for Depression in Pregnancy. http://www.ctri.nic.in/Clinicaltrials/pdf_generate.php?trialid = 19185&EncHid = &modid=&compid = %27,%2719185det%27. [Google Scholar]
- Reilly N, Kingston D, Loxton D, Talcevska K, Austin MP, 2019. A narrative review of studies addressing the clinical effectiveness of perinatal depression screening programs. Women Birth. [DOI] [PubMed] [Google Scholar]
- Rock MM, 2018. A stepped-collaborative perinatal depression model. J. Am. Psychiatr. Nurses Assoc, 1078390318789252. [DOI] [PubMed] [Google Scholar]
- Sofronas M, Feeley N, Zelkowitz P, Sabbagh M, 2011. Obstetric and neonatology nurses’ attitudes, beliefs, and practices related to the management of symptoms of maternal depression. Issues Ment. Health Nurs 32, 735–744. [DOI] [PubMed] [Google Scholar]
- Srivastava K, Chatterjee K, Bhat PS, 2016. Mental health awareness: the Indian scenario. Ind. Psychiatry J 25, 131–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tareen RS, Tandon R, 2018. A stitch in time saves nine: untreated perinatal depression hurts future generations. Asian J. Psychiatr 38 A1–a3. [DOI] [PubMed] [Google Scholar]
- Townsend C, Whiteford H, Baingana F, Gulbinat W, Jenkins R, Baba A, Lieh Mak F, Manderscheid R, Mayeya J, Minoletti A, Mubbashar MH, Khandelwal S, Schilder K, Tomov T, Parameshvara Deva M, 2004. The mental health policy template: domains and elements for mental health policy formulation. Int. Rev. Psychiatry 16, 18–23. [DOI] [PubMed] [Google Scholar]
- Vengadavaradan A, Bharadwaj B, Sathyanarayanan G, Durairaj J, 2019. Frequency and correlates of mother-infant bonding disorders among postpartum women in India. Asian J. Psychiatr 44, 72–79. [DOI] [PubMed] [Google Scholar]
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. , 2012. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiguna T, Ismail RI, 2019. Validation study of Indonesian mother-infant bonding scale. Asian J. Psychiatr 43, 60–64. [DOI] [PubMed] [Google Scholar]
- Williams CJ, Turner KM, Burns A, Evans J, Bennert K, 2016. Midwives and women’s views on using UK recommended depression case finding questions in antenatal care. Midwifery 35, 39–46. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.