Abstract
Objective
The performance of the platelet times neutrophil-to-lymphocyte ratio, namely systemic immune inflammation (SII) index, is an inflammatory index that shows controversial results as a predicting indicator of the poor outcomes of COVID-19. In this study, this indicator was analyzed in 3280 patients admitted at a COVID-19 reference hospital in Quito (Ecuador).
Methods
The Receiver Operating Characteristic (ROC) curve analysis was conducted on SII values upon admission to identify the most appropriate cut-off values in discriminating COVID-19 severity and in-hospital mortality.
Results
SII was higher in both severe patients and in those who finally died (cut-off points of 757.3 and 808.5 respectively). However, the AUC-ROC analysis (0.60-0.67) demonstrated a modest discriminating performance of SII for COVID-19 severity (61.2% sensitivity and 61.5% specificity), which sensibly improved for COVID-19 mortality (AUC-ROC: 0.73-0.83, sensitivity: 80.6% specificity; 63.6%).
Conclusion
SII index may well be an indicator of inflammatory conditions secondary to COVID-19 leading to a higher mortality, rather than a predictor of severe forms of the disease.
Key words: biomarkers, COVID-19, mortality, ROC curve, severity of illness index
1. INTRODUCTION
During SARS-CoV-2 infection, the activation of hyper-inflammation, cytokine storm, coagulopathies, and disseminated intravascular coagulation are the most prevalent pathobiological processes leading to severe acute respiratory distress syndrome (ARDS) and multi-organ failure. This is the rationale of including platelet counts in the development of new blood-cell based composed inflammation indices for the forecasting of COVID-19 patients. The systemic immune inflammation index (SII= (platelet counts × neutrophil counts)/lymphocyte counts), a composed blood parameter originally set to assist with the diagnosis, progress, and risk stratification of inflammatory diseases [1], can also predict COVID-19 severity and mortality [2-9]. Despite the evidence, doubts exist regarding the prognostic performance of SII [10,11], which may fall short as a biomarker of poor clinical outcomes, especially in hospitalized COVID-19 patients who present comorbidities [12,13]. The use of patients at different stages of the disease, or even the disparate sizes of the samples used (from 119 to 1800 patients), would account for the controversy. In this study, it was investigated the association between SII values and COVID-19 severity and in-hospital mortality using the records of a large sample of patients from a COVID-19 reference hospital of Northern Ecuador. During the epidemic, Ecuador had the highest death toll in all South America.
2. METHODS
This observational retrospective study included 3280 consecutive patients over 18 years old, who were admitted at the IESS Hospital Quito Sur in Quito (Ecuador) from March 13 to June 17, 2020 with COVID-19 (CDC 2019-Novel Coronavirus Real-Time RT-PCR Diagnostic Panel in upper and lower respiratory specimens) and showing COVID-19-like symptoms. Blood samples for routine laboratory tests were drawn upon admission (after a 40-min interval of average) and subsequently run in a Sysmex XN-550™ Hematology Analyzer (Sysmex America Inc., Japan). In addition, an arterial blood gas exam was also conducted on room air under a controlled oxygen environment at the time of admission using a RAPIDPoint® 500 blood gas system (Siemens Healthcare GmbH; Germany). Patient categorization was conducted in agreement with the NIH guidelines (https://www.covidl9treatmentguidelines.nih.gov/overview/clinical-spectrum/) for the severity of COVID-19 pneumonia. The “Severe group” included a total of 635 patients who had blood hypoxemia (PaO2 < 60 mmHg; SpO2 < 94%). The rest (2645 cases) were classified as “Non-Severe” (PaO2 ≥ 60 mmHg and SpO2 ≥ 94%.). Discrepant cases showing values of PaO2 < 60 mmHg and SpO2 ≥ 94% were not included in the analysis.
Non normally distributed variables were determined by the Shapiro Wilk test and expressed as medians and interquartile ranges (IRs). The Mood test was chosen to compare the medians of NLR and SII (annotated as P*N/L) across COVID-19 severity and in-hospital mortality/survival groups. Odds ratios (ORs) were calculated using a simple logistic regression as well as a multiple logistic regression analysis when convenient to estimate the likelihood of severity and mortality on a multiple variable basis of confounding factors such as age, sex and the SII index. The Receiver Operating Characteristic curve (AUC-ROC) analysis was conducted to evaluate the discriminative performance of the SII and NLR indices as well as to identify the optimal cut-off points of both the maximum sensitivity and specificity (Youden index). Concerning the performance criterion, AUC values were interpreted as follows: 0.5-0.6 (failed), 0.6-0.7 (worthless), 0.7-0.8 (poor), 0.8-0.9 (good), > 0.9 (excellent) [14]. Alpha value was set at 0.05. Written informed consent was waived due to the use of secondary data obtained from anonymized patients (Public Health Ministerial order of December 31st, 2014). The STROBE (Strengthening The Reporting of OBservational Studies in Epidemiology) guidelines were followed in reporting this study.
3. RESULTS
The sample included similar numbers of men (1643) and women (1637). There were 635 Severe cases (19.4%) and 2645 non-Severe cases (80.6%). The median age was as follows (years (SD)): Non-Severe 42.1 (22.3), Severe 42.9 (21.7), Survivor 42.2 (22.2), non-Survivor 45.5 (22.3). Mortality rate (3.1%, two thirds of whom were men) in the Severe group was higher than in the non-severe group (4.9% and 2.7% respectively). The median of SII and NLR were significantly higher in both the Non-Survival and the Severe groups (Table 1).
Table 1.
Medians of the SII index and NLR ratio in COVID-19 patients grouped according to mortality and severity
| SII (P*N/L) | Median (IR) | Median (IR) | p-value* |
|---|---|---|---|
| Mortality | Yes n=103 | No n=3177 | < 0.001 |
| 1766.7 (884.3-3339.0) | 615.0 (379.7-1082.9) | ||
| Severity | Severe n=635 | Non-Severe n=2645 | |
| 684.0 (421.7-1293.7) | 609.0 (376.8-1090.4) | < 0.001 | |
| NLR | |||
| Mortality | Yes n=103 | No n=3177 | < 0.001 |
| 9.0 (4.7-15.0) | 2.4 (1.5-4.3) | ||
| Severity | Severe n=635 | Non-Severe n=2645 | |
| 2.9 (1.8-5.5) | 2.4 (1.5-4.3) | < 0.001 | |
*Mood test (median test).
In the AUC-ROC analysis (Figure 1), the optimal cut-off points for severity were 757.3 (SII) and 2.28 (NLR), while for mortality were 808.5 (SII) and 3.81 (NLR). The AUCs of the SII index were modest (0.66 for severity and 0.77 for mortality) compared to the NLR ratio (AUC values of 0.57 and 0.84 for severity and mortality respectively). The sensitivity and specificity of the SII index for severity were 61.2% and 61.5% respectively. As to mortality, the sensitivity of SII increased up to 80.6%, while its specificity barely changed (63.6%). For the association analysis, the patients were divided in two groups according to the SII cut-off points so that 58.8% of the patients (n=1929) were below the cut-off for severity and 62.2% of the patients (n=2041) for mortality. After considering potential confounders such as age, gender and SII, the logistic regression analysis revealed that those patients with levels of SII above the cut-off were more likely to either have severe COVID-19 (adjusted OR [95%CI]: 2.233(1.787-2.790)) or to die during hospitalization (adjusted OR [95%CI]: 5.690 (3.438-9.416)). The SII index was independently associated with mortality in patients hospitalized for COVID-19.
Figure 1.
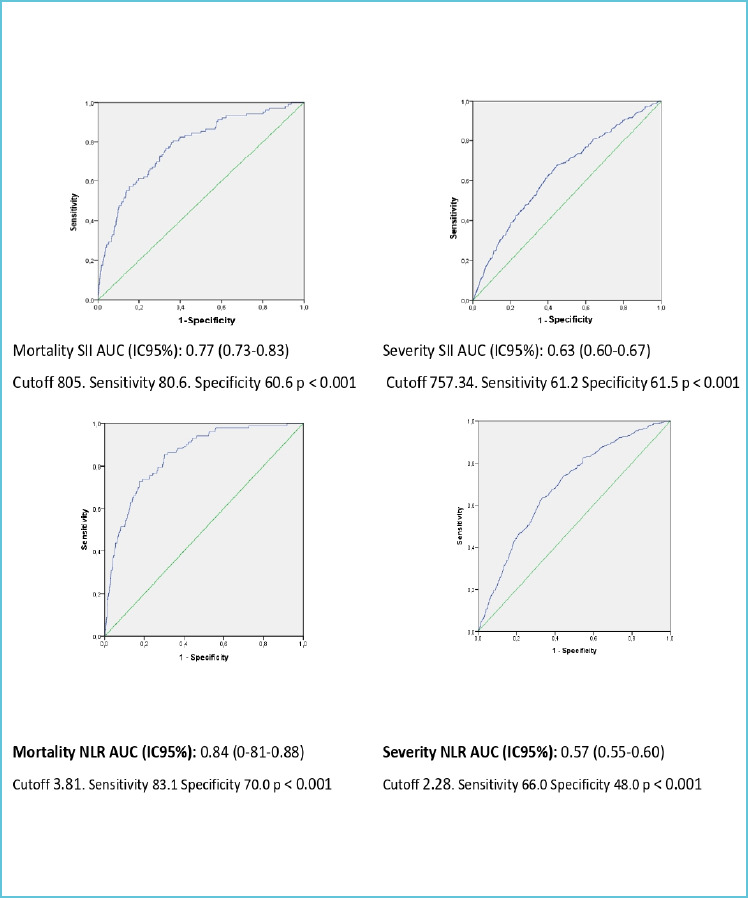
ROC curves of SII (top) and NLR (bottom) for mortality (left) and severity (right)
4. DISCUSSION
Despite the fact that COVID-19 mortality risk is undoubtedly associated with a high SII value [2], our ROC analysis demonstrated a modest discriminating power for SII in predicting COVID-19 severity upon admission compared to other studies [4-6,8,9,13], where the sensitivity and specificity as well as the AUC values were higher than in this study. Different categorization criteria for COVID-19 severity (blood hypoxemia versus ICU admission and invasive mechanical ventilation) suggests that SII cannot discriminate well disease severity at early stages of the disease as the NLR parameter does [15]. However, the discriminating power for SII notably improved when considering mortality showing AUC values (0.73-0.83), which were in line with others [5,6-8]. The SII cut-off value for mortality (835) was in line with previous reports [2,3,12]. The sensitivity of SII for mortality (80.6%) was even higher to what was reported in other studies [2,7]. This improvement of the discriminating power of SII for mortality may partially be related to the ongoing increment of platelets counts, which along with an excessively high values of NLR often shown by COVID-19 patients, might provoke coagulopathies in late stages of the illness [16]. Although the analysis of records from a single institution may be considered a limitation, this study showed that the SII index at the time of admission was only associated with COVID-19 in-hospital mortality. Whereas a complex interaction between inflammation and hemostasis may be the reason for the modest performance of SII in the prediction of severe COVID-19 [11], the index may well be an indicator of inflammatory conditions secondary to COVID-19 disease, which could ultimately precipitate death [5,12,13,16].
Acknowledgments
We thank Francisco Mora (IESS Quito Sur Hospital) who worked with us in the database management.
Abbreviations
- AUC-ROC
Area Under the Curve-Receiver Operating Characteristic
- NLR
Neutrophil-to-Lymphocyte Ratio
- SII
Platelet by Neutrophil-to-Lymphocyte Ratio
Footnotes
Compliance with ethical standards
Written informed consent for participation was not required for this study due to the use of secondary data in accordance with the national legislation and the institutional requirements. We followed the STROBE guideline to report this study. The authors declare they had no access to identifying patient information when analyzing the data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
The authors have no competing interests to declare.
Authors’ contributions statement
Both authors have contributed sufficiently and equally to this research work.
REFERENCES
- 1.Putzu C., Cortinovis D.L., Colonese F., Canova S, Carru C, Zinellu A, Paliogiannis P. (2018) Blood cell count indexes as predictors of outcomes in advanced non-small-cell lung cancer patients treated with Nivolumab. Cancer Immunol Immunother 67:1349–1353. 10.1007/S00262-018-2182-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fois AG, Paliogiannis P, Scano V, Cau S, Babudieri S, Perra R, Ruzzittu G, Zinellu E, Pirina P, Carru C, Arm LB, Fancellu A, Mondoni M, Mangoni AA, Zinellu A. (2020) The systemic inflammation index on admission predicts in-hospital mortality in COVID-19 patients. Molecules 25:5725. 10.3390/molecules25235725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rokni M, Ahmadikia K, Asghari S, Mashaei S, Hasanali F. (2020) Comparison of clinical, para-clinical and laboratory findings in survived and deceased patients with COVID-19: diagnostic role of inflammatory indications in determining the severity of illness. BMC Infect Dis; 20:869. doi: 10.1186/S12879-020-05540-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gujar RK, Meena A, Chouhan SS, Likhar KS. (2021) Hematological profiles of COVID-19 patients at the Ratlam district, Madhya Pradesh State, India. Bioinformation 17:686-690. doi: 10.6026/97320630017686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moisa E, Corneci D, Negoita S, Filimon CR, Serbu A, Negutu Ml, Grintescu IM. (2021) Dynamic changes of the Neutrophil-to-Lymphocyte Ratio, Systemic Inflammation Index, and derived Neutrophil-to-Lymphocyte Ratio independently predict invasive mechanical ventilation need and death in critically ill COVID-19 patients. Biomedicines 9:1656. doi: 10.3390/biomedicines9111656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halmaciu I, Arbănaşi EM, Kaller R, Mureşan AV, Arbănaşi EM, Bacalbasa N, Suciu BA, Cojocaru II, Runcan AI, Grosu F, Vunvulea V, Russu E. (2022) Chest CT Severity Score and Systemic Inflammatory biomarkers as predictors of the need for invasive mechanical ventilation and of COVID-19 patients’ mortality. Diagnostics (Basel) 12:2089. doi: 10.3390/diagnostics12092089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghobadi H, Mohammadshahi J, Javaheri N, Fouladi N, Mirzazadeh Y, Aslani MR. (2022) Role of leukocytes and systemic inflammation indexes (NLR, PLR, MLP, dNLR, NLPR, AISI, SIR-I, and SII) on admission predicts in-hospital mortality in non-elderly and elderly COVID-19 patients. Front Med (Lausanne) 9:916453. doi: 10.3389/fmed.2022.916453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mallappa S, Khatri A, Bn G, Kulkarni P. (2022) A retrospective analysis of the importance of biochemical and hematological parameters for mortality prediction in COVID-19 cases. Cureus 14:e30129. doi: 10.7759/cureus.30129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xia W, Tan Y, Hu S, Li C, Jiang T. (2022) Predictive value of Systemic Immune-Inflammation index and neutrophil-to-lymphocyte ratio in patients with severe COVID-19. Clin Appl Thromb Hemost 28:10760296221111391. doi: 10.1177/10760296221111391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Citu C, Gorun F, Motoc A, Sas I, Gorun OM, Burlea B, Tuta-Sas I, Tomescu L, Neamtu R, Malita D, Citu IM. (2022) The predictive role of NLR, d-NLR, MLR, and SIRI in COVID-19 mortality. Diagnostics (Basel). 12:122. doi: 10.3390/diagnosticsl2010122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nooh HA, Abdellateif MS, Refaat L, Kandeel EZ, Bayoumi A, Samra M, Khafagy M. (2021) The role of inflammatory indices in the outcome of COVID-19 cancer patients. Med Oncol 39:6. doi: 10.1007/sl2032-021-01605-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sevinc C, Demirci R, Timur O. (2021) Predicting hospital mortality in COVID-19 hemodialysis patients with developed scores. Semin Dial 34:347-359. 10.1111/sdi.l3004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamad DA, Aly MM, Abdelhameid MA, et al. (2022) Combined blood indexes of systemic inflammation as a mirror to admission to intensive care unit in COVID-19 patients: a multicentric study. J Epidemiol Glob Health 12:64–73. doi:10.1007/s44197-021-00021-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polo TCF, Miot HA. (2020) Use of ROC curves in clinical and experimental studies. J Vase Bras 19:e20200186. doi: 10.1590/1677-5449.200186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu J, Liu Y, Xiang P, Pu L, Xiong H, et al. (2020) Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Trans Med 18:206. 10.1186/sl2967-020-02374-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wool GD, Miller JL. (2021) The impact of COVID-19 disease on platelets and coagulation. Pathobiology 88:15-27. doi: 10.1159/000512007 [DOI] [PMC free article] [PubMed] [Google Scholar]


