Abstract
This cohort study examines the association between COVID-19 pandemic restrictions and obesity prevalence among youths aged 2 to 19 years in Monroe County, Indiana.
Introduction
Childhood obesity is linked to adulthood obesity and to childhood and adulthood noncommunicable diseases.1,2 Pandemic restrictions imposed in early 2020 contributed to decreased physical activity, reduced access to healthy foods, and increased stress, screen time, and consumption of processed foods and sugary drinks among youths.3,4,5 Recent studies provide limited insight on longer-term associations of COVID-19 restrictions with childhood obesity prevalence. Thus, this study aimed to evaluate whether pandemic-related body mass index (BMI) changes, if any, among children persisted after restriction removal and to identify associated factors.
Methods
This cohort study was conducted using data for Monroe County, Indiana, which encompasses 2 municipalities, 2 public school systems, and extensive agrarian and forested areas and had a 2020 population of approximately 148 000 (including 22 000 youths aged 2-19 years).6 Weight and height measurements were obtained from electronic health record data for children aged 2 to 19 years in repeated cross-sections (2016-2021; annual average n = 14 595) and for longitudinal cohorts aged 5 to 11 years in 2019 (cohort 1, 2017-2019; n = 8647) and 2021 (cohort 2, 2019-2021; n = 7816). The BMI categories (underweight, healthy weight, overweight, obesity, and severe obesity) were based on the US Centers for Disease Control and Prevention growth charts for age and sex1,2 (details in the Figure). Binomial logistic regression was used to establish trends in BMI prevalence and associated factors, including age, sex, residence (zip code group), and health insurance type (race and ethnicity data were not available). Pearson χ2 was used to compare transition trends (upward, downward, or stable) between BMI categories for both cohorts by longitudinally tracking individuals with complete responses for 3 consecutive years. The Indiana University Health Bloomington Hospital and Indiana University Bloomington institutional review boards approved this study and waived informed consent because deidentified patient data were used. The study followed the STROBE reporting guideline.
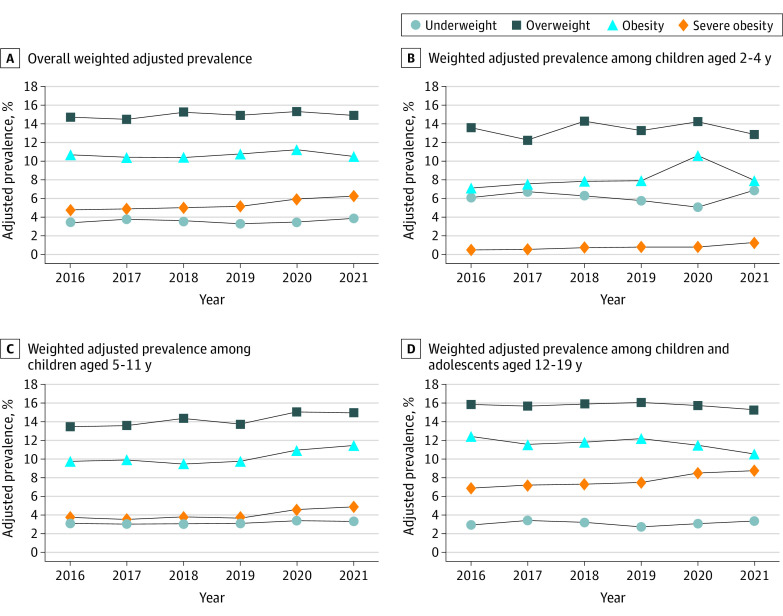
Figure. Adjusted Prevalence of Body Mass Index (BMI) Categories for Children Aged 2 to 19 Years, 2016 to 2021.
Data are from the electronic health records of children aged 2 to 19 years. A to D, Prevalence estimates are weighted and presented overall (A) and for children aged 2 to 4 years (B), 5 to 11 years (C), and 12 to 19 years (D). The BMI categories were defined based on the US Centers for Disease Control and Prevention BMI-for-age growth chart as underweight (<5th percentile), healthy (5th-<85th percentile), overweight (85th-<95th percentile), obesity (≥95th percentile), and severe obesity (≥120% of 95th percentile).
Data analysis was performed between April 2021 and April 2022. Results are presented as percentages or odds ratios (ORs) with 95% CIs. P < .05 (2-tailed) was statistically significant. All analyses were performed in Stata, version 17 (StataCorp).
Results
This study included 27 093 participants (13 497 girls [49.8%] and 13 596 boys [50.2%]; mean [SD] age, 9.8 [5.3] years). Overall severe obesity prevalence was higher in 2020 (5.9% [5.5%-6.4%]; P = .009) and 2021 (6.3% [5.8%-6.7%]; P < .001) compared with 2019 (5.1% [4.6%-5.5%]) (Figure and Table).
Table. Estimated Yearly Overall and Age-Specific Prevalence of Body Mass Index (BMI) Categories From Binomial Logistic Modelsa.
| Year | BMI category | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Underweight (<5th percentile) | Healthy weight (5th-<85th percentile) | Overweight (85th-<95th percentile) | Obesity (≥95th percentile) | Severe obesity (≥120% of 95th percentile) | |||||||||||
| Adjusted prevalence, % (95% CI) | OR (95% CI) | P value | Adjusted prevalence, % (95% CI) | OR (95% CI) | P value | Adjusted prevalence, % (95% CI) | OR (95% CI) | P value | Adjusted prevalence, % (95% CI) | OR (95% CI) | P value | Adjusted prevalence, % (95% CI) | OR (95% CI) | P value | |
| Total sample | |||||||||||||||
| 2016 | 3.5 (3.1-3.8) | 1.04 (0.90-1.21) | .56 | 66.2 (65.3-67.2) | 1.02 (0.96-1.08) | .57 | 14.8 (14.1-15.5) | 0.99 (0.91-1.07) | .78 | 10.7 (10.9-11.4) | 1.00 (0.91-1.09) | .94 | 4.8 (4.4-5.3) | 0.93 (0.82-1.07) | .32 |
| 2017 | 3.8 (3.4-4.2) | 1.15 (0.99-1.33) | .07 | 66.4 (65.4-67.3) | 1.03 (0.97-1.09) | .41 | 14.5 (13.8-15.3) | 0.97 (0.89-1.05) | .43 | 10.4 (9.8-11.0) | 0.96 (0.88-1.05) | .41 | 4.9 (4.4-5.3) | 0.95 (0.83-1.09) | .47 |
| 2018 | 3.6 (3.3-4.0) | 1.10 (0.95-1.27) | .20 | 65.7 (64.8-66.7) | 0.99 (0.94-1.05) | .84 | 15.2 (14.5-15.9) | 0.97 (0.89-1.05) | .60 | 10.4 (9.8-11.0) | 0.96 (0.88-1.05) | .41 | 5.1 (4.6-5.5) | 0.99 (0.87-1.13) | .85 |
| 2019 | 3.3 (3.0-3.7) | 1 [Reference] | NA | 65.8 (64.9-66.7) | 1 [Reference] | NA | 14.9 (14.3-15.6) | 1 [Reference] | NA | 10.8 (10.3-11.3) | 1 [Reference] | NA | 5.1 (4.7-5.6) | 1 [Reference] | NA |
| 2020 | 3.5 (3.2-3.9) | 1.05 (0.91-1.22) | .47 | 64.0 (63.1-65.0) | 0.92 (0.87-0.98) | .005 | 15.3 (14.6-16.0) | 1.02 (0.95-1.10) | .43 | 11.2 (10.6-11.8) | 1.05 (0.96-1.14) | .30 | 5.9 (5.5-6.4) | 1.18 (1.04-1.33) | .009 |
| 2021 | 3.9 (3.5-4.3) | 1.17 (1.02-1.35) | .03 | 64.5 (65.4-63.5) | 0.94 (0.89-1.00) | .04 | 14.9 (14.2-15.6) | 1.03 (0.96-1.11) | .93 | 10.5 (9.9-11.1) | 0.97 (0.89-1.06) | .55 | 6.3 (5.8-6.7) | 1.24 (1.10-1.41) | .001 |
| Age group, y | |||||||||||||||
| 2-4 | |||||||||||||||
| 2019 | 5.8 (4.9-6.7) | 1 [Reference] | NA | 72.6 (70.9-74.2) | 1 [Reference] | NA | 13.3 (12.0-14.5) | 1 [Reference] | NA | 7.9 (6.9-8.9) | 1 [Reference] | NA | 0.8 (0.5-1.1) | 1 [Reference] | NA |
| 2020 | 5.1 (4.2-6.0) | 0.87 (0.68-1.11) | .26 | 69.7 (67.9-71.4) | 0.87 (0.77-0.98) | .02 | 14.2 (12.8-15.5) | 1.08 (0.92-1.26) | .35 | 10.6 (9.4-11.8) | 1.38 (1.14-1.66) | .001 | 0.8 (0.5-1.1) | 1.01 (058-1.75) | .98 |
| 2021 | 6.9 (0.7-1.1) | 1.20 (0.95-1.53) | .13 | 71.5 (69.5-73.4) | 0.95 (0.83-1.08) | .40 | 12.9 (11.4-14.3) | 0.96 (0.81-1.14) | .67 | 7.9 (6.8-9.1) | 1.00 (0.81-1.23) | >.99 | 1.3 (0.9-1.7) | 1.58 (0.94-2.64) | .08 |
| 5-11 | |||||||||||||||
| 2019 | 3.2 (2.7-3.6) | 1 [Reference] | NA | 69.6 (68.4-70.9) | 1 [Reference] | NA | 13.8 (12.9-14.8) | 1 [Reference] | NA | 9.8 (9.0-10.6) | 1 [Reference] | NA | 3.7 (3.2-4.2) | 1 [Reference] | NA |
| 2020 | 3.4 (2.9-3.9) | 1.09 (0.87-1.36) | .44 | 66.0 (64.6-67.3) | 0.84 (0.77-0.92) | <.001 | 15.1 (14.1-16.1) | 1.11 (0.99-1.24) | .08 | 11.0 (10.1-11.8) | 1.14 (1.00-1.29) | .048 | 4.6 (4.0-5.2) | 1.26 (1.04-1.53) | .02 |
| 2021 | 3.3 (2.8-3.9) | 1.06 (0.84-1.34) | .60 | 65.3 (63.8-66.7) | 0.82 (0.75-0.89) | <.001 | 15.0 (14.0-16.1) | 1.10 (0.98-1.24) | .10 | 11.5 (10.5-12.5) | 1.20 (1.05-1.36) | .007 | 4.9 (4.2-5.5) | 1.34 (1.10-1.64) | .004 |
| 12-19 | |||||||||||||||
| 2019 | 2.8 (2.3-3.2) | 1 [Reference] | NA | 61.5 (60.0-62.9) | 1 [Reference] | NA | 16.1 (15.0-17.2) | 1 [Reference] | NA | 12.3 (11.3-13.3) | 1 [Reference] | NA | 7.5 (6.8-8.3) | 1 [Reference] | NA |
| 2020 | 3.1 (2.6-3.6) | 1.13 (0.89-1.45) | .32 | 61.2 (59.8-62.6) | 0.99 (0.91-1.08) | .80 | 15.8 (14.7-16.9) | 0.98 (0.87-1.10) | .69 | 11.5 (10.6-12.5) | 0.93 (0.82-1.06) | .28 | 8.5 (7.7-9.4) | 1.15 (0.98-1.34) | .08 |
| 2021 | 3.4 (2.8-3.9) | 1.23 (0.96-1.58) | .10 | 62.0 (60.5-63.4) | 1.02 (0.94-1.12) | .62 | 15.4 (14.3-16.5) | 0.94 (0.84-1.06) | .34 | 10.6 (9.7-11.5) | 0.85 (0.74-0.97) | .01 | 8.8 (8.0-9.7) | 1.19 (1.02-1.40) | .03 |
Abbreviations: NA, not applicable; OR, odds ratio.
Compared with 2020, no significant changes in prevalence overall and across age groups were observed in 2021. Binomial logistic regression models were adjusted for age group, sex, residence (zip code groups), health insurance type, and survey weights.
We observed the greatest increase in obesity prevalence among children aged 5 to 11 years (vs 2-4 and 12-19 years). Although healthy weight was significantly lower for this population in 2020 and 2021, their prevalence of both obesity and severe obesity was significantly higher in 2020, persisting into 2021 (11.5% [10.5%-12.5%]; P = .007 and 4.9% [4.2%-5.5%]; P = .004), compared with 2019 (9.8% [9.0%-10.6%] and 3.7% [3.2%-4.2%]). Their total unhealthy BMI prevalence (ie, overweight, obesity, and severe obesity) was also higher in 2020 (33.6% [32.7%-34.6%]) and 2021 (32.9% [32.0%-33.8%]) compared with 2019 (31.9% [31.0%-32.8%]). In addition, 2021 trends observed for these children were confirmed via longitudinal transition trend analysis, which suggested that cohort 2 experienced a significant upward BMI transition (18.1% [16.9%-19.3%]) compared with cohort 1 (14.0% [13.0%-15.0%]) (P < .001).
Finally, we observed that in 2020 and 2021 compared with 2019, female sex (OR, 1.28 [95% CI, 1.07-1.54]; P = .008 and OR, 1.32 [95% CI, 1.09-1.59]; P = .004), public insurance (OR, 1.24 [95% CI, 1.04-1.48]; P = .02 and OR, 1.36 [95% CI, 1.14-1.62]; P = .001), and residence in southeast Monroe County, a relatively high-income area (OR, 1.41 [95% CI, 1.10-1.80]; P = .006 and OR, 1.49 [95% CI, 1.17-1.91]; P = .001) were associated with higher odds of severe obesity.
Discussion
The findings of this cohort study suggest that childhood obesity, especially among US children aged 5 to 11 years, was significantly higher after COVID-19 restrictions were imposed and persisted for multiple reasons3,4,5 after restriction removal in 2021. The sampling method used may have potentially introduced selection bias, and the narrow data coverage (1 US county) limits the generalizability of these findings. Obesity prevention efforts should focus on elementary school–aged youths to prevent high prevalence of unhealthy BMI.
Data Sharing Statement
References
- 1.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315(21):2292-2299. doi: 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lohrmann D, YoussefAgha A, Jayawardene W. Trends in body mass index and prevalence of extreme high obesity among Pennsylvania children and adolescents, 2007-2011: promising but cautionary. Am J Public Health. 2014;104(4):e62-e68. doi: 10.2105/AJPH.2013.301851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruíz-Roso MB, de Carvalho Padilha P, Matilla-Escalante DC, et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during Covid-19 pandemic: an observational study. Nutrients. 2020;12(8):2289. doi: 10.3390/nu12082289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring). 2020;28(8):1382-1385. doi: 10.1002/oby.22861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hillis S, Unwin J, Cluver L, et al. Children: the hidden pandemic 2021: a joint report of COVID-19-associated orphanhood and a strategy for action. 2021. Accessed May 20, 2022. https://www.cdc.gov/coronavirus/2019-ncov/downloads/community/orphanhood-report.pdf
- 6.Indiana Business Research Center . STATS Indiana: statistical data utility for the State of Indiana. InDepth Profile of Indiana. Accessed October 28, 2021. https://www.stats.indiana.edu/profiles/profiles.asp?scope_choice=a&county_changer=18105
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement