Abstract
Background
According to previous research, hip internal rotation (HIR) aggravates low back pain (LBP) symptoms, especially in patients with lumbar flexion with rotation (F + R) syndrome. Therefore, the present study aimed to examine the lumbopelvic-hip rhythm during the HIR test in patients with this syndrome.
Methods
In this cross-sectional study, 20 men without LBP and 20 matched men with LBP, subcategorized in the F+R subgroup, participated. The participants performed the HIR test. Kinematics data were recorded using a motion analysis system. After processing the kinematics, a comparison was made in the hip and pelvic kinematics between the groups.
Results
A statistical analysis based on an independent t test revealed a significant increased (P < 0.05) pelvic rotation during the tests with the dominant ( P = 0.007) and nondominant limbs (P = 0.025) in those with LBP. The analysis also showed that during the test with the dominant lower limb, the pelvis and hip moved with a more synchronized pattern in patients with LBP (P = 0.001).
Conclusion
In the patients with lumbar F + R syndrome, there was a tendency for early pelvic rotation during the dominant HIR test. Moreover, LBP people also exhibited a greater pelvic rotation range of motion in the first half and whole pathways of the test. These impairments could be a risk factor for the development of LBP symptoms in these patients.
Keywords: Low Back Pain, Lumbopelvic, Hip, Kinematics, Rotation
↑What is “already known” in this topic:
Limb movements are associated with lumbopelvic motions. Generally, if these motions take place in an excessive range during limb movement, LBP occurs accordingly. One limb movement that is associated with LBP, especially in those subcategorized in the F + R subgroup, is hip rotation. Previous studies have shown that patients with F + R syndrome might benefit from decreasing lumbopelvic rotation with limb movements.
→What this article adds:
The present study indicated an increased and early lumbopelvic motion in the transverse plane plan of motion in patients with the F + R syndrome. These findings reveal how LBP occurs during or after activities requiring limb movements in patients.
Introduction
Low back pain (LBP) and its associated impairments are known as the first causes of disability among musculoskeletal disorders worldwide (1 , 2). Despite extensive research with attempts to design and propose a confirmed plan of treatment, none of them have been successful (3). Recently, some authors believe that subclassifying patients with LBP in homogeneous subgroups could considerably help in solving the problem (3-5). Differences in movement patterns of lumbopelvic of subgrouped people with LBP were also indicated in previous studies (4, 6 -9). Therefore, some authors have proposed models for the subgrouping of patients with LBP.
The Movement system impairment model (MSI) is a new, valid model of classification, which is used for subclassifying patients with LBP (10). In this model, an LBP patient lies in 1 of the 5 subgroups: (1) lumbar flexion; (2) lumbar extension; (3) lumbar rotation; (4) lumbar flexion with rotation (F + R); and (5) lumbar extension with rotation, based on which the direction of lumbar movement stimulates pain symptom (10). Efficiency of this model in treatment of people with LBP has been established in clinical studies ( 11, 12). Therefore, we aimed to use the MSI model for specifying the patients who attended this study.
Investigations have indicated that not only trunk movements, but also limb movements, can provoke LBP symptoms (12, 13). A number of researchers believe that lumbopelvic movement impairments during lower limb movements could be a cause of the complaint (13, 14). In this regard, because these impairments were not well determined, they were not corrected effectively in patients and have led to persistence of the symptoms (15). These authors have suggested that the insufficient control of the lumbopelvic in a specific direction can result in early or/and excessive lumbopelvic motion when a limb moves (14-16). These forms of the lumbopelvic motion may contribute to LBP, when repeated frequently during habitual activities. Based on this concept, a precise examination of the lumbopelvic movement pattern during tests of lower limb movement is essential in subgroups of people with the LBP.
One subgroup of people with LBP, based on MSI, is a subgroup of patients with lumbar (F + R) syndrome: patients who have LBP symptoms related to flexion and rotation direction of lumbar spine movements (10). Based on the reports, the subgroup of patients with lumbar F + R syndrome has a significant distribution among patients with LBP (15, 17). Previous studies have also demonstrated that this subgroup of patients had pain during lower limb rotation movements such as hip rotation (18, 19), and when the hip internally rotated, the pelvic rotation was restricted, which alleviated or lessened the symptom (12, 18 , 19). Therefore, clinical evidences suggest a relationship between hip internal rotation (HIR) motion, pelvic rotation motion, and LBP symptom in patients who are categorized in the F + R subgroup. LBP in these patients may result from excessive pelvic motion in the transverse plane as the hip rotates, which puts strain on the lumbar tissues beyond what is normally tolerated. A review of the laboratory studies shows that the lumbopelvic-hip rhythms of patients with lumbar F + R syndrome have been examined in a limited number of studies, and these examinations were also limited to sagittal plane (15, 17, 20). Therefore, no study has so far examined lumbopelvic movement patterns in LBP people with F + R syndrome in the transverse plane and during a lower limb rotation test such as the HIR test.
Therefore, the purpose of this study was to examine the lumbopelvic movement patterns of LBP with F + R syndrome patients and healthy controls during the HIR test in the transverse plane. In this study, we hypothesized that the LBP patients would demonstrate more and/or early lumbopelvic rotation during the test as compared with healthy people.
Methods
Participants
In total, 40 men volunteered to participate in this cross-sectional study: 20 men without LBP and 20 with LBP. The participants were divided into 2 groups (LBP and control) and were matched based on weight, height, and age. Those participants who met the inclusion criteria signed a consent form approved by Shahid Beheshti University of Medical Sciences (IR, SBMU.RETECH, and REC.1395.365). Controls were included if they (1) were aged 20 to 50 years, (2) had no LBP symptoms in the past year, and (3) had no previous lumbar spine surgery. Patients with LBP were enrolled in the study if they (1) were included in the lumbar F + R syndrome based on the approach proposed by Sahrmann for subgrouping patients (15, 21); (2) had LBP symptoms more than 3 months (chronic LBP) (22); (3) were labeled as patients with nonspecific LBP by physicians; (4) had LBP symptoms that intensified gradually with or after flexion- and rotation-related activities; and (5) were 20 to 50 years old. Participants characteristics are included in Table 1. The following formula was utilized to determine the sample size for the study.
Table 1. Demographic and clinical characteristics of the participants.
| Variable | Low Back Pain Group N=20 Mean (SD) | Control Group N=20 Mean (SD) | P Value | |
|---|---|---|---|---|
| Age (yr.) | 27.75 (7.59) | 24.42 (2.87) | 0.080 | |
| Height (M) | 1.74 (0.05) | 1.78 (0.06) | 0.109 | |
| Weight (kg) | 74.8 (5.6) | 73.9 (8.9) | 0.726 | |
| Body Mass Index (BMI) | 24.5 (2.49) | 23.25 (0.02) | 0.094 | |
| Baecke score | 7.36 (1.34) | 8.38 (1.69) | 0.045 | |
| Oswestry disability index score | 16.1 (8.29) | - | - | |
| Duration of pain (month) | 19.5 (16.8) | - | - |
Significant p-values are presented in bold.
Participants were excluded from the study if they had (1) a previous history of lower limbs or spinal surgery; (2) degenerative joint disease in a lower limb or lumbar spine; (3) pathological conditions, such as tumor, infection, et cetera in the lumbar spine; (4) psychological illness, leg length discrepancy, radiculopathy, neuropathy; or (5) a history of serious head injury.
Clinical Measures
Participants initially completed a demographic questionnaire. Those with the LBP also completed 3 additional questionnaires: (a) the visual analog scale questionnaire (VAS) for determining the pain intensity of patients; (b) a Persian version of Oswestry Disability Index (ODI) questionnaire, a questionnaire of perceived LBP-related disability (23); and (c) a Persian version of Baecke Habitual Physical Activity questionnaire (BHPAQ) (24).
Kinematic Measurement and Processing
We employed a 7-camera, 3-dimensional, motion measurement system (Qualisys Motion Capture Systems), located in Isfahan University of Medical Sciences, for recording the kinematics data. We aimed to record kinematics data of the hip and lumbopelvic regions in the transverse plane (rotation motion). For this purpose, we attached retroreflective markers on the specified anatomical landmarks including (1) the left and right posterior superior iliac spine, (2) medial side of the left and right knee joints line, and (3) the left and right medial malleolus, demonstrated in Figure 1 and Figure 2. The kinematics data collection was performed with a sampling rate of 100 Hz.
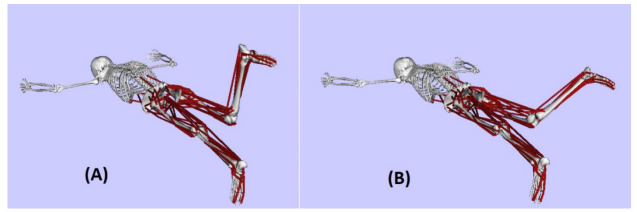
Figure 1.
Start (A), and end position (B) of the test performed by a subject in the prone position
Figure 2.
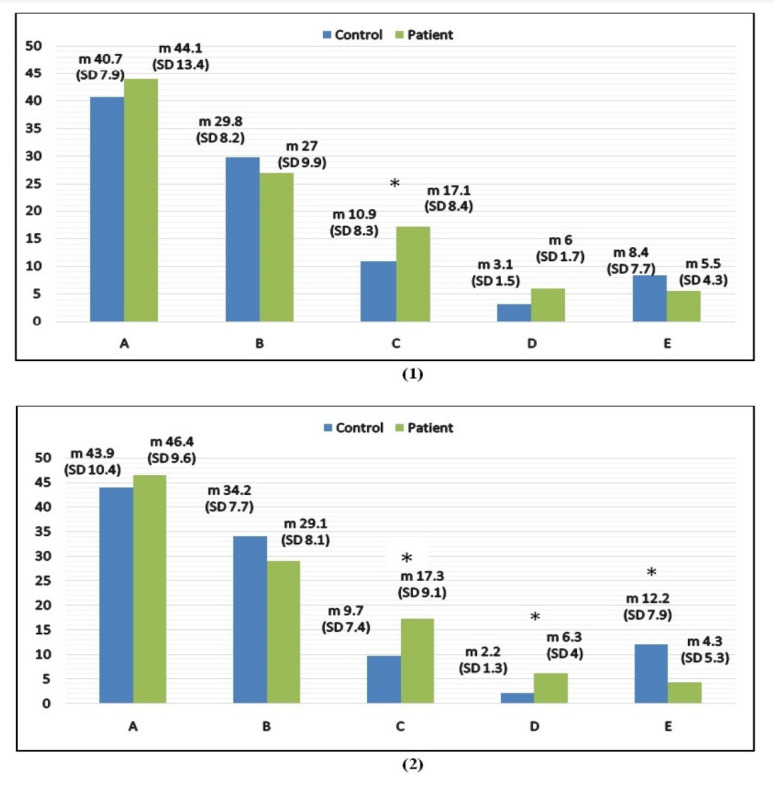
Result of the Kinematics Measurements and Differences between the 2 Groups during the Tests with the Nondominant (1) and Dominant (2) Limb A, range of lower limb rotation; B, range of hip rotation; C, range of pelvic rotation; D, amount of pelvic rotation in first half of pathway; E, hip/pelvic synchroniza-tion; SD, Standard deviation; m, mean. *Significant value (P < 0.05).
The Test
Participants were asked to perform the HIR test in the prone position (25). Three trials with the dominant limbs and 3 trials with the nondominant lower limbs were performed. Procedures involved in the performance of the test were based on the study of Sadeghisani et al (26). For this purpose, we asked the patients to assume prone position and hold a knee in the 90˚ of flexion. Then, the patients were instructed to internally rotate their lower limb as much as they can and return the limb to the initial position. We requested the patients to perform the test at a speed of their choosing while a randomly chosen limb was used to initiate the test. Figure 1 illustrates the procedures of performing the test in the prone position.
After data collection, a Butterworth filter filtered all the raw data. Cutoff frequency of the filter was 2.5 Hz. Then, kinematics variables, regarding the hip-pelvic regain, were calculated in the transverse plane. The kinematics variables included an amount of hip and pelvic rotation range of motion during the test, the range of pelvic rotation from the starting point to the mid-point of the test, and the range of hip rotation from the start point of the test to the point in which pelvic rotation initiated. The start and end points of the limb and pelvic rotation motions were determined based on the method used in previous studies (7, 25). Reliability of the variables measured was tested in a sample of 10 participants without a history of LBP during the test with the dominant limb. The intraclass correlation coefficient (ICC, 3,1) was used to index reliability. The values for each test was found to be reliable and are reported in Table 2.
Table 2. ICC (3, 1) values of variables obtained in the study.
| Variables | Lower Limb Rotation Range | Pelvic Rotation Range | The Completed Range of Hip Rotation Before the Starting Point of Pelvic Motion | Range of Pelvic Rotation During the First Half of the Test |
|---|---|---|---|---|
| ICC (3,1) | 0.99 | 0.97 | 0.77 | 0.93 |
Statistical Analysis
All statistical analyses were completed using SPSS Version 20. Initially, normality of the data distribution was assessed using the Kolmogrov-Smiranov test. Next, independent samples t tests were used to compare dependent variables between the groups, that is, with and without LBP.
Results
In the study, 20 healthy men (mean age, 24.42 ± 2.87 years) and 20 LBP men (mean age, 27.75 ± 7.59 years) participated (P > 0.05). The demographic data comparison revealed that the patient group had lower physical activities level than healthy controls ( P = 0.045).
Results indicated that the patients exhibited a statistically significant pelvic rotation during the tests with the dominant (P = 0.007) and nondominant limbs ( P = 0.025), which were more than that for the healthy participants (P < 0.05) (Figure 2). Less hip rotation was possible in the patients, but the changes were not statistically significant. (P > 0.05). The obtained results demonstrated that in the patient group, pelvic rotation initiated after 4.3˚ of limb rotation. The initiation of pelvic rotation in the healthy group was after 12.2˚ of limb rotation. Therefore, these data demonstrated that pelvic and hip moved in more synchronized patterns in the patients than in the healthy controls ( P = 0.001).
Analysis demonstrated that during the test with the dominant lower limb, in the first half of the test, pelvic rotation motion in people with LBP took place in a greater magnitude (6.3˚) than in people without LBP (2.2˚), with a significant difference between the 2 groups (P = 0.002). However, the difference was not significant between these groups when the nondominant limb did the test (P = 0.092).
Discussion
Among biopsychosocial risk factors related to LBP, the biomechanical factor is the most prominent factor in most of the cases (27). Many biomechanical characteristics, which may be related to LBP, have been the focus of previous studies. Therefore, many biomechanical features have been proposed as the causes of LBP. Recently, numerous authors and researchers have focused on the lumbopelvic and hip movement impairments (14, 15 , 20, 26). They believe that increased lumbopelvic motion, during trunk and/or lower limb motion, in a specific direction, is associated with an excessive load on the lumbopelvic region (14, 15, 26). Based on this concept, with the repetition of the loads, LBP would be possible to be observed. Therefore, examining patterns of lumbopelvic-hip movement can help clinicians to explore the causes of LBP and making decisions for considering the problem (28).
Based on evidence, patients with F + R are a frequent group of patients among people who suffer from LBP symptoms, and the symptoms were associated with lower limb motions that caused rotation in the lumbopelvic region. A lower limb motion caused lumbopelvic rotation motion and pain in these people was HIR. However, no study has yet investigated the lumbopelvic-hip rhythm of patients with F + R during HIR. As a result, it was examined in the present study. According to the study's findings, patients conducted the HIR tests with greater pelvic rotation when using both their dominant and nondominant limbs. Findings of the present study were consistent with those of Scholtes et al who found similar findings in patients with LBP during the hip external rotation test (14). Sadeghisani et al also observed an excessive pelvic rotation in a group of athletes with LBP during HIR test compared with healthy controls (25). Previous research has shown that limiting pelvic motion can be associated with a decrease in pain intensity when a limb movement leads to the symptoms ( 12, 29). We may therefore conclude that the poor lumbopelvic rotation found in the study's patients may be a contributing factor to the LBP and that it needs to be properly corrected. The obtained results can clarify how limb rotation may be related to LBP in patients with lumbar F + R syndrome. Some authors have suggested that increased lumbopelvic motion in a specific direction is a result of increased flexibility of the lumbopelvic soft tissues in those directions, which is induced by repeated movement of lumbopelvic motion in such directions through habitual or functional activities (4, 28 , 30). Sadeghisani et al also demonstrated that forming of pattern of lumbopelvic movement impairment is a task-related sequence (28). Therefore, the increased lumbopelvic rotation motion observed in patients with F + R syndrome may be related to the tasks they perform during habitual physical activities.
Previously, some authors focused on the hip rotation range of motion impairment in patients with LBP (31-34). They hypothesized that limited hip rotation would be followed by an increase in the lumbopelvic rotation as a result of compensatory motion. Based on this concept, the ranges of hip rotation were examined in different groups of patients with LBP. Research, however, has revealed that decreased HIR range of motion has a potent relationship with LBP (35). The results of the present study support earlier studies' findings that people with LBP have reduced HIR range of motion than healthy individuals. On the contrary, this study revealed that group differences were not statistically significant. It appears that HIR impairment in the F + R subgroup of patients needs to be taken into consideration as a significant clinical finding. There were 2 more kinematic variables examined for the participant groups. The first was the amount of pelvic rotation in the first mid-range of the test, as an index for describing lumbopelvic and hip motion behavior during the functional activities (15, 36). The second was the amount of hip rotation from the start point of the test to the point of the test that pelvic rotation initiated, which functioned as an index for describing lumbopelvic and hip motion synchronization (7, 15, 25, 36). As Figure 2 shows, during the test with the dominant limb, pelvic moves had a greater magnitude in the first half of the test and earlier in the patients. Data revealed that in patients with lumbar F + R syndrome, there was a greater tendency of the lumbopelvic rotation during the dominant HIR, which may happen during habitual activities. It has been suggested that behavior of the lumbopelvic region, when a limb moves in a specific direction, can identify its behavior during functional activities (26). Nevertheless, further studies are needed to ascertain the idea.
Limitations
This study was not without limitation. The following limitations need to be considered by researchers in future studies. The first limitation deals with the notion that only 1 subgroup of patients was compared with the healthy group. We recommend that other subgroups of patients be compared with healthy controls. The second limitation relates to the fact that differences between the groups were examined based on the HIR test. In the future studies, attention should be paid to the examination of the lumbopelvic movements, which must be performed during other limb motions. The third limitation was that the test employed in the study was a nonfunctional test. We recommend that assessments be performed based on functional activities in future studies. Last, the present study was limited to the transverse plane. Examination of lumbopelvic motion in the other planes is required to be included in addition to the transverse plane.
Conclusion
During the dominant or nondominant HIR tests, it was revealed that lumbopelvic region in LBP patients with F + R syndrome moved in a greater range than in people without LBP. In addition, as compared to healthy individuals, the patients showed earlier pelvic rotation and better hip/pelvic rotation on the dominant HIR test. Moreover, with the dominant limb internal rotation movement, it was found that patients with lumbar F + R syndrome exhibited greater magnitude of pelvic rotation in the first half of the movement as compared with people without LBP.
Conflict of Interests
The authors declare that they have no competing interests.
Acknowledgment
The authors would like to thank Dr Mohammad Taghi Karimi, Farideh Dehghan Manshadi, and Dr Abbas Rahimi for all their conceptual supports. This study was part of a doctoral thesis design by research (IR, SBMU.RETECH, and REC.1395.365).
Ethical Considerations
The present study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR, SBMU.RETECH, and REC.1395.365).
Cite this article as : Sadeghisani M, Khademi Kalantari Kh, Satari M. Lumbopelvic-Hip Rhythm in People with Lumbar Flexion-with-Rotation Syndrome during Hip Internal Rotation. Med J Islam Repub Iran. 2023 (24 May);37:58. https://doi.org/10.47176/mjiri.37.58
References
- 1.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646. [PMC free article] [PubMed] [Google Scholar]
- 2.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 3.O'Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10(4):242. doi: 10.1016/j.math.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Sadeghisani M, Shaterzadeh MJ, Karimi MT, Fatoye F, Akbari M, Dehghan M, Kabir MM. Kinematic differences in lumbopelvic and hip movement patterns during a lower limb movement test between two groups of people with low back pain. J Mech Med Biol. 2017;17(2):1750030. doi: 10.1142/S0219519417500300. [DOI] [Google Scholar]
- 5.Maluf KS, Sahrmann SA, Van Dillen. Use of a classification system to guide nonsurgical management of a patient with chronic low back pain. Phys Ther. 2000;80(11):1097. [PubMed] [Google Scholar]
- 6.Van Dillen, Gombatto SP, Collins DR, Engsberg JR, Sahrmann SA. Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain. Arch Physic Med Rehabil. 2007;88(3):351. doi: 10.1016/j.apmr.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 7.Sadeghisani M, Namnik N, Karimi MT, Rafiei AR, Manshadi FD, Eivazi M. et al. Evaluation of differences between two groups of low back pain patients with and without rotational demand activities based on hip and lumbopelvic movement patterns. Ortop Traumatol Rehabil. 2015;17(1):51. doi: 10.5604/15093492.1143536. [DOI] [PubMed] [Google Scholar]
- 8.Gombatto SP, Collins DR, Sahrmann SA, Engsberg JR, Van Dillen. Patterns of lumbar region movement during trunk lateral bending in 2 subgroups of people with low back pain. Physic Ther. 2007;87(4):441. doi: 10.2522/ptj.20050370. [DOI] [PubMed] [Google Scholar]
- 9.Dankaerts W, O’Sullivan P, Burnett A, Straker L, Davey P, Gupta R. Discriminating healthy controls and two clinical subgroups of nonspecific chronic low back pain patients using trunk muscle activation and lumbosacral kinematics of postures and movements: a statistical classification model. Spine. 2009;34(15):1610. doi: 10.1097/BRS.0b013e3181aa6175. [DOI] [PubMed] [Google Scholar]
- 10.Sahrmann S. Diagnosis and Treatment on Movement Impairment Syndromes. St Louis: MO: Mosby ; 2002. [Google Scholar]
- 11.Harris-Hayes M, Van Dillen, Sahrmann SA. Classification, treatment and outcomes of a patient with lumbar extension syndrome. Physiother Theory Pract. 2005;21(3):181. doi: 10.1080/09593980500212987. [DOI] [PubMed] [Google Scholar]
- 12.Van Dillen, Sahrmann SA, Wagner JM. Classification, intervention, and outcomes for a person with lumbar rotation with flexion syndrome. Phys Ther. 2005;85(4):336. [PubMed] [Google Scholar]
- 13.Van Dillen, Sahrmann SA, Norton BJ, Caldwell CA, Fleming D, McDonnell MK. et al. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther. 2001;31(8):402. doi: 10.2519/jospt.2001.31.8.402. [DOI] [PubMed] [Google Scholar]
- 14.Scholtes SA, Gombatto SP, Van Dillen. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech (Bristol, Avon) 2009;24(1):7–12. doi: 10.1016/j.clinbiomech.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sadeghisani M, Rezvani M, Rahmani P, Tabesh H, Nikouei F. Examining the lumbopelvic-hip movement pattern in a subgroup of patients with low back pain during the active straight leg raise test. J Res Med Dent Sci. 2017;5(3):4–10. [Google Scholar]
- 16.Sheikhhoseini R, O'Sullivan K, Alizadeh MH, Sadeghisani M. Altered motor control in athletes with low back pain: A literature review. Ann Appl Sport Sci. 2016;4(4):43–50. [Google Scholar]
- 17.Sadeghisani M, Manshadi FD, Kalantari KK, Karimi MT, Azimi H, Aghazadeh A. Kinematics of the Lumbar Spine and Hip Joints in People with Persistent Low Back Pain during Sit to Stand and Stand to Sit Activities. Med J Islam Repub Iran. 2021;35 doi: 10.47176/mjiri.35.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Dillen, Maluf KS, Sahrmann SA. Further examination of modifying patient-preferred movement and alignment strategies in patients with low back pain during symptomatic tests. Man Ther. 2009;14(1):52–60. doi: 10.1016/j.math.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Dillen, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom N. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Physic Med Rehabil. 2003;84(3):313. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 20.Kim MH, Yoo WG, Choi BR. Differences between two subgroups of low back pain patients in lumbopelvic rotation and symmetry in the erector spinae and hamstring muscles during trunk flexion when standing. J Electromyogr Kinesiol. 2013;23(2):387. doi: 10.1016/j.jelekin.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 21.Sahrmann S. Diagnosis and treatment of movement impairment syndromes. Elsevier Health Sciences; ; 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krismer M, Van Tulder. Low back pain (non-specific) Best Pract Res Clin Rheumatol. 2007;21(1):77–91. doi: 10.1016/j.berh.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the Quebec Back Pain Disability Scale: translation and validation studies of the Iranian versions. Spine (Phila Pa 1976) 2006;31(14):E454. doi: 10.1097/01.brs.0000222141.61424.f7. [DOI] [PubMed] [Google Scholar]
- 24.Sadeghisani M, Manshadi FD, Azimi H, Montazeri A. Validity and reliability of the Persian version of Baecke habitual physical activity questionnaire in healthy subjects. Asian J Sports Med. 2016;7(3) doi: 10.5812/asjsm.31778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sadeghisani M, Manshadi FD, Kalantari KK, Rahimi A, Rafiei AR, Asnaashari A. et al. A comparison of the lumbopelvic-hip complex movement patterns in people with and without non-specific low back pain during an active hip test. J Mech Med Biol. 2017;17(01):1750004. [Google Scholar]
- 26.Sadeghisani M, Shaterzadeh MJ, Taghi Karimi, Rafiei AR. Lumbopelvic Movement Pattern Differences in Two Groups of Low Back Pain Subjects with and without Rotational Activities during Active Hip External Rotation Test. J Res Rehabil Sci. 2013;9(8):1200. [Google Scholar]
- 27.Diamond S, Borenstein D. Chronic low back pain in a working-age adult. Best Pract Res Clin Rheumatol. 2006;20(4):707. doi: 10.1016/j.berh.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 28.Sadeghisani M, Sobhani V, Kouchaki E, Bayati A, Ashari AA, Mousavi M. Comparison of Lumbopelvic and Hip Movement Patterns During Passive Hip External Rotation in Two Groups of Low Back Pain Patients with and without Rotational Demand Activities. Ortop Traumatol Rehabil. 2015;17(6):611. doi: 10.5604/15093492.1193032. [DOI] [PubMed] [Google Scholar]
- 29. Van Dillen LR. n SA. Norton BJ. Caldwell CA. McDonnell MK. Bloom N. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. . Arch Physic Med Rehabil. . 2003 ;84(3):313–22. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 30.Scholtes SA, Gombatto SP, Van Dillen. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech. 2009;24(1):7–12. doi: 10.1016/j.clinbiomech.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cibulka MT, Sinacore DR, Cromer GS, Delitto A. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine (Phila Pa 1976) 1998;23(9):1009. doi: 10.1097/00007632-199805010-00009. [DOI] [PubMed] [Google Scholar]
- 32.Ellison JB, Rose SJ, Sahrmann SA. Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Phys Ther. 1990;70(9):537. doi: 10.1093/ptj/70.9.537. [DOI] [PubMed] [Google Scholar]
- 33.Mellin G. Correlations of hip mobility with degree of back pain and lumbar spinal mobility in chronic low-back pain patients. Spine (Phila Pa 1976) 1988;13(6):668. [PubMed] [Google Scholar]
- 34.Vad VB, Bhat AL, Basrai D, Gebeh A, Aspergren DD, Andrews JR. Low back pain in professional golfers: the role of associated hip and low back range-of-motion deficits. Am J Sports Med. 2004;32(2):494. doi: 10.1177/0363546503261729. [DOI] [PubMed] [Google Scholar]
- 35.Sadeghisani M, Manshadi FD, Kalantari KK, Rahimi A, Namnik N, Karimi MT. et al. Correlation between Hip Rotation Range-of-Motion Impairment and Low Back Pain: A Literature Review. . Ortop Traumatol Rehabil. 2015;17(5):455. doi: 10.5604/15093492.1186813. [DOI] [PubMed] [Google Scholar]
- 36.Gombatto SP, Collins DR, Sahrmann SA, Engsberg JR, Van Dillen. Gender differences in pattern of hip and lumbopelvic rotation in people with low back pain. Clin Biomech (Bristol, Avon) 2006;21(3):263. doi: 10.1016/j.clinbiomech.2005.11.002. [DOI] [PubMed] [Google Scholar]