Abstract
Background:
Burns represent a leading cause of morbidity and mortality for children. This study explores the intersecting effects of social deprivation and race in pediatric burn patients.
Methods:
We performed a retrospective review of all pediatric patients (< 18 years old) admitted to a tertiary burn center in North Carolina from 2009–2019. We used bivariate analysis to compare patients based on reported race, comparing African Americans (AA) to all others. Modified Poisson regression was used to model the probability of undergoing autologous skin grafting based on AA race.
Results:
Of 4,227 children admitted, AA children were disproportionally represented, comprising 33.7% of patients versus a state population of 22.3%. AA patients had larger %TBSA with a median of 3% (IQR 1–6) compared to 2% (IQR 1–5, p<0.001) and longer median length of stay at 5.8 days (SD 13.6) versus 4.9 days (SD 13.8). AA patients were more likely to have autologous skin grafting compared to other races, with an adjusted RR of 1.49 (95% CI 1.22–1.83) when controlling for Area Deprivation Index (ADI) national rank, age, %TBSA, and burn type.
Conclusions:
AA children were disproportionately represented and had larger burns, even when controlling for ADI. They had longer hospital stays and were more likely to have autologous skin grafting, even accounting for burn size and type. The intersection between social deprivation and race creates a unique risk for AA patients. Further investigation into this phenomenon and factors underlying surgical intervention selection are indicated to inform best treatment practices and future preventative strategies.
Keywords: burn, pediatric, ADI, race
Introduction
Unintentional injuries, including burns, represent the leading cause of morbidity and mortality among children in the United States.[1–3] Fire and burn represent the fifth leading cause of pediatric death related to unintentional injury in America, and over 100,000 children are admitted to emergency departments annually for the treatment of burn injuries.[4] Various developmental, situational, and clinical factors create an elevated risk of serious burn injury or mortality among young children, including immature motor and cognitive abilities, dependence on adult supervision, and an inability to self-rescue. Children also have thin dermal skin layers and a smaller body surface area that lead to more extensive and deeper burns.[5,6]
While unintentional injuries affect children across all races and socioeconomic classes, existing literature shows that this risk is not evenly distributed. Children from families with low socioeconomic status (SES) or those that identify as racial or ethnic minorities consistently have higher rates of burn injuries both in the United States and globally.[7–12] Although the disproportionate burden of burn injury among minorities has been previously demonstrated, regional data is needed.[7–9,13,14] In addition, there is minimal data analyzing the intersection of these factors or the independent effect of race when controlling for SES.[7,8,15] Due to the serious risk of morbidity and mortality in this patient population, it is essential to identify risk factors and predictors of clinical outcomes to develop prevention strategies.[7]
Consequently, the aim of this study was to explore the intersecting effects of social deprivation and race in pediatric burns at a busy tertiary burn center.
Methods
We performed a retrospective analysis of the burn registry at the University of North Carolina (UNC) Jaycee Burn Center. The UNC Jaycee Burn Center is located at UNC Hospitals, a tertiary center in Chapel Hill, NC. It is verified by the American Burn Association for pediatric and adult burn care. The burn center has a 21-bed burn intensive care unit, more than 30 acute care beds, and averages more than 1200 admissions per year.[16] Patients are admitted based on American Burn Association guidelines. As one of the few burn centers in the state, patients are transferred to UNC for evaluation from across North Carolina. The burn registry records patient demographics, burn injury characteristics, clinical interventions, and clinical outcomes.
Intensive care unit (ICU) admission criteria at UNC include: second and third degree burns greater than 10% total body surface area (TBSA) in patients under 10; second and third degree burns involving the face, hands, feet, genitalia, or major joints; third degree burns greater than 5% TBSA; electrical burns, including lightning chemical burns; and burn injury with pre-existing medical disorders that could complicate treatment and prolong recovery. Furthermore, children must be admitted in the case of suspected abuse or neglect, which is unfortunately common. Lastly, ICU admissions are indicated in the case of airway concerns, inhalation injury, circumferential burns, and neuro checks.
We included all pediatric patients less than 18 years old recorded in the UNC Burn Registry from 2009 through 2019. The primary aim of the study was to explore the association between burn injury severity and race and/or socioeconomic status for pediatric burn patients in North Carolina. In addition, we examined the relationship between race and/or socioeconomic status and access to surgical burn care.
We compared race based on self-reported categories during admission. For analysis, patients were compared by the following categories: African American, Caucasian (non-Hispanic), Caucasian (Hispanic), or other. The “other” category included American Indian, Asian, Native Hawaiian and Other Pacific Islander alone, and Two or More Races. Socioeconomic status was estimated using the Area Deprivation Index (ADI).[17] The ADI uses seventeen poverty, education, employment, and housing quality metrics to rank a neighborhood’s disadvantage that may impact health outcomes. The ranking runs from 1 to 100, with a 100-rank representing the most disadvantaged. The ADI has been validated to the United States Census Blocks level, identified by a Federal Information Processing Standards (FIPS) number. We matched study patient addresses to the corresponding FIPS and subsequently to its corresponding ADI national rank using a publicly available 2019 ADI database.
Our primary outcomes were burn characteristics, including % total burn surface area (TBSA) and the type of burn. We also examined whether patients required autologous skin grafting for their burns instead of wound care or temporary biological dressing. Autologous skin grafting procedures were identified using ICD-9 or ICD-10 codes recorded in the registry.
We initially described the patient population, including demographic factors, burn characteristics, and clinical outcomes. We then compared patients based on race, examining burn characteristics, burn treatment, and clinical outcomes. We used bivariate analysis, utilizing Chi-square tests for categorical variables. A one-way analysis of variance (ANOVA) was used for continuous variables because race has more than two categorical values. For continuous variables with a non-normal distribution, a Kruskal–Wallis one-way analysis of variance was used to calculate medians. Medians are reported with interquartile ranges (IQR) and means with standard deviations (SD).
We used a modified Poisson regression model to estimate the risk ratio for undergoing skin grafting after burn injury.[18,19] We initially created a model comparing African American patients with all other races. We then created an adjusted model, initially including potential confounders identified in our bivariate analysis. We used a change-in-effect method to remove covariates that did not significantly affect (< 10%) the relationship between race and skin grafting. We report an unadjusted and adjusted risk ratio with 95% confidence intervals from the final models. Lastly, we used a logistic regression model to graph the relationship between %TBSA and National ADI rank, stratified by race.
All statistical analysis was performed using Stata/SE 17.0 (Stata- Corp LP, College Station, TX). Ethics approval was obtained from the University of North Carolina Institutional Review Board.
Results
From 2009–2019, 4,227 pediatric patients (< 18 years old) were admitted to the UNC Burn Center. Table 1 shows a description of the patient population. The median age was 3 years (IQR 1–8), with a male preponderance at 59.8% (n=2,529). African Americans comprised 33.7% (n=1,423) of patients compared to 41.3% (n=1,744) of Caucasians (non-Hispanic) and 13.7% (n=579) of Caucasians (Hispanic). American Indians and Asians were less than 2% each. The median ADI National Rank was 68 (IQR 47–85). A histogram showing the frequency of National ADI Rank among all patients is shown in Figure 1.
Table 1.
Characteristics of pediatric burn patients admitted to Jaycee UNC Burn Center
| All Pediatric Patients (n=4,227) | |
|---|---|
|
| |
| Patient Age (years) | |
| Median (IQR) | 3.0 (1.0–8.0) |
| Gender: N (%) | |
| Female | 1,698 (40.2%) |
| Male | 2,529 (59.8%) |
| Race: N (%) | |
| Black, Non-Hispanic | 1,423 (33.7%) |
| Caucasian, Non-Hispanic | 1,744 (41.3%) |
| Caucasian, Hispanic | 579 (13.7%) |
| American Indian | 77 (1.8%) |
| Asian | 74 (1.8%) |
| Other | 328 (7.8%) |
| ADI National Rank | |
| Median (IQR) | 68 (47–85) |
| Insurance Status: N (%) | |
| Private | 1,196 (28.3%) |
| Medicaid | 2,691 (63.7%) |
| Self-pay | 309 (7.3%) |
| Other | 30 (0.7%) |
| Burn Type: N (%) | |
| Scald | 2,358 (55.8%) |
| Fire | 648 (15.3%) |
| Contact | 961 (22.7%) |
| Other | 260 (6.2%) |
| TBSA | |
| Median (IQR) | 2.0 (1.0–5.0) |
| Admission Status: N (%) | |
| Floor | 3,099 (77.6%) |
| Step-down | 318 (8.0%) |
| ICU | 579 (14.5%) |
| ICU Length of Stay | |
| Median (IQR) | 2.0 (1.0–5.0) |
| Hospital Length of Stay | |
| Median (IQR) | 2.0 (1.0–5.0) |
| Crude In-hospital Mortality: N (%) | 6 (0.1%) |
Figure 1.
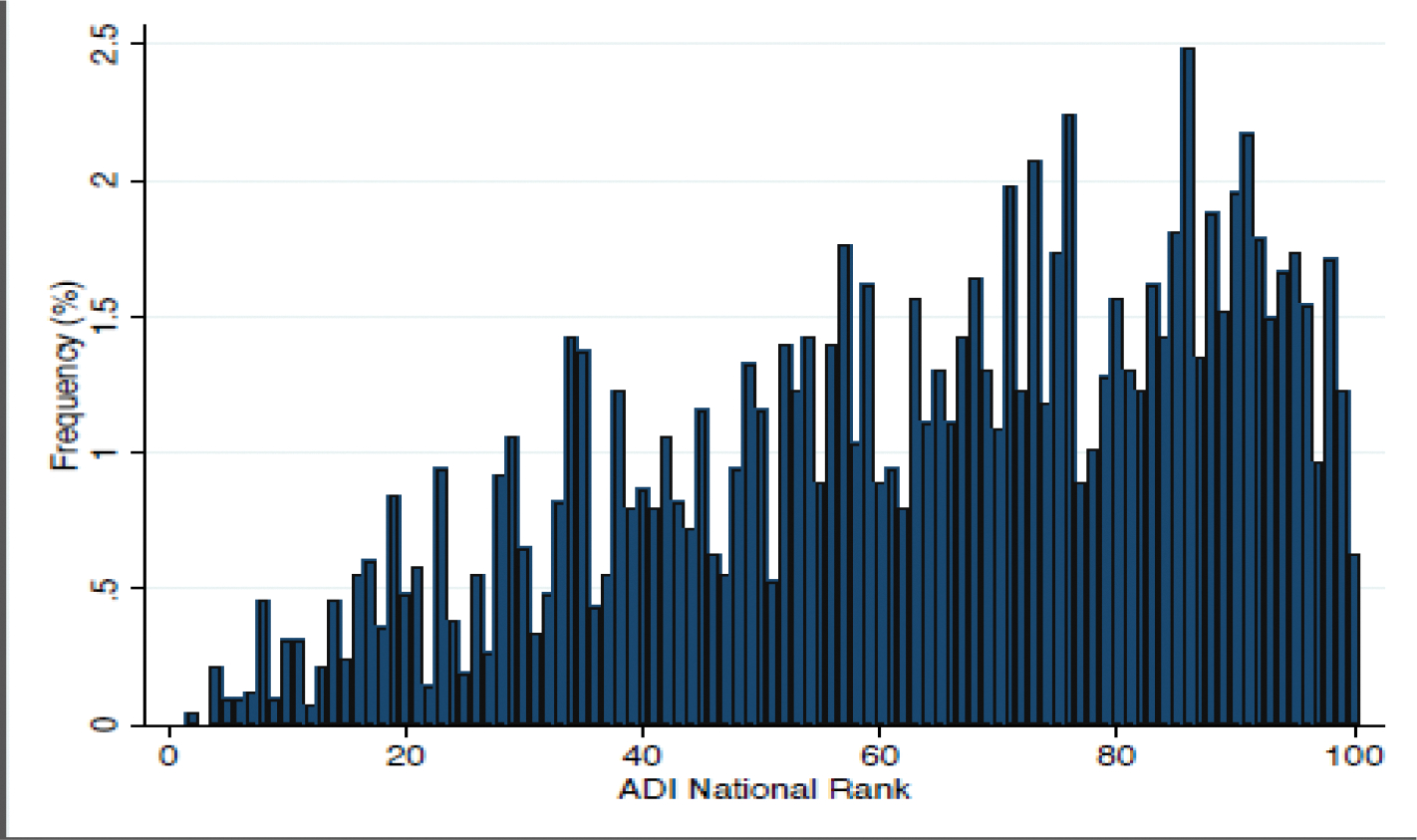
The distribution of pediatric burn patients by ADI National Rank.
Most patients had Medicaid (63.7%, n=2,691) followed by private insurance at 28.3% (n=1,196). Scald burns were the most common burn type at 55.8% (n=2,358) with a median %TBSA of 2.0 (IQR 1.0–5.0). Overall, 14.5% (n=579) were admitted to the intensive care unit (ICU) with a median ICU length of stay of 2.0 days (IQR 1.0–5.0). For all patients, the median hospital length of stay was 2.0 days (IQR 1.0–5.0). Crude in-hospital mortality was very low, with only 6 deaths (0.1%).
Table 2 compares patients based on race. Notable differences include a significantly higher median ADI National Rank among African Americans at 76 (IQR 57–89) compared to 60 (IQR 40–79) and 70 (IQR 51–85, p<0.001) among non-Hispanic Caucasians and Hispanic Caucasians, respectively. Medicaid insurance was much more common among African Americans (79.0%, n=1,124) and Caucasian and Hispanic (80.1%, n=464) patients compared to Caucasian (non-Hispanic) children (47.1%, n=822, p<0.001). Scald burns were also more common among these cohorts, with 68.5% (n=975) of African Americans and 68.2% (n=395, p<0.001) of Caucasians (Hispanic) suffering a scald burn compared to 40.1% (n=700) of Caucasians (non-Hispanic). Median TBSA was the highest in African Americans at 3% (IQR 1.0–6.0) and the lowest among Caucasians at 2.0% (IQR 1.0–4.5, p<0.001). Time to presentation was also similar between the groups with a median of 0 days for all four groups (p=0.07).
Table 2.
A comparison of pediatric burn patients, stratified by race.
| African American, Non-Hispanic | Caucasian, Non-Hispanic | Caucasian, Hispanic | Other | pvalue | |
|---|---|---|---|---|---|
|
| |||||
| Patient Age (years) | |||||
| Median (IQR) | 3.0 (1.0–8.0) | 3.0 (1.0–10.0) | 2.0 (1.0–6.0) | 2.0 (1.0–6.0) | <0.001 |
| Gender: N (%) | |||||
| Female | 608 (42.7%) | 641 (36.8%) | 245 (42.3%) | 202 (42.2%) | |
| Male | 815 (57.3%) | 1,103 (63.2%) | 334 (57.7%) | 277 (57.8%) | |
| ADI National Rank | |||||
| Median (IQR) | 76.0 (57.0–89.0) | 60.0 (40.0–79.0) | 70.0 (51.0–85.0) | 66.0 (42.0–83.0) | <0.001 |
| Insurance Status: N (%) | |||||
| Private | 204 (14.3%) | 783 (44.9%) | 59 (10.2%) | 150 (31.3%) | <0.001 |
| Medicaid | 1,124 (79.0%) | 822 (47.1%) | 464 (80.1%) | 279 (58.2%) | |
| Self-pay | 90 (6.3%) | 119 (6.8%) | 54 (9.3%) | 46 (9.6%) | |
| Other | 4 (0.3%) | 20 (1.1%) | 2 (0.3%) | 4 (0.8%) | |
| Burn Type: N (%) | |||||
| Scald | 975 (68.5%) | 700 (40.1%) | 395 (68.2%) | 287 (59.9%) | <0.001 |
| Fire | 141 (9.9%) | 375 (21.5%) | 66 (11.4%) | 65 (13.6%) | |
| Contact | 217 (15.2%) | 544 (31.2%) | 104 (18.0%) | 96 (20.0%) | |
| Other | 90 (6.3%) | 125 (7.2%) | 14 (2.4%) | 31 (6.5%) | |
| TBSA | |||||
| Median (IQR) | 3.0 (1.0–6.0) | 2.0 (1.0–4.5) | 2.5 (1.0–5.0) | 2.0 (1.0–5.0) | <0.001 |
| Time to Presentation | |||||
| Median (IQR) | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.07 |
| Had Autologous Skin Grafting? | |||||
| Yes: N (%) | 157 (11.0%) | 151 (8.7%) | 39 (6.7%) | 38 (7.9%) | 0.010 |
| Number of Grafting Operations: N (%) | |||||
| 1 | 122 (77.7%) | 116 (76.8%) | 31 (79.5%) | 25 (65.8%) | 0.4 |
| 2 | 23 (14.6%) | 28 (18.5%) | 4 (10.3%) | 9 (23.7%) | |
| 3+ | 12 (7.6%) | 7 (4.6%) | 4 (10.3%) | 4 (10.5%) | |
| Time to First Operation (Days) | |||||
| Median (IQR) | 1.0 (0.0–2.0) | 0.0 (0.0–2.0) | 1.0 (0.0–2.0) | 0.0 (0.0–2.0) | <0.001 |
| Admission Status: N (%) | |||||
| Floor | 1,023 (75.2%) | 1,296 (78.6%) | 420 (78.4%) | 358 (79.9%) | 0.2 |
| Step-down | 120 (8.8%) | 132 (8.0%) | 36 (6.7%) | 30 (6.7%) | |
| ICU | 218 (16.0%) | 221 (13.4%) | 80 (14.9%) | 60 (13.4%) | |
| ICU Length of Stay | |||||
| Median (IQR) | 2.0 (1.0–6.0) | 2.0 (1.0–4.0) | 2.0 (1.0–3.0) | 2.0 (1.0–10.0) | 0.014 |
| LOS | |||||
| Median (IQR) | 3.0 (1.0–6.0) | 2.0 (1.0–5.0) | 2.0 (1.0–4.0) | 2.0 (1.0–4.0) | <0.001 |
African American patients more often had autologous skin grafting at 11.0% (n=157) compared to 8.7% (n=151) and 6.7% (n=39, p=0.010) of Caucasians (non-Hispanic) and Caucasian (Hispanic), respectively. The median time to the first operation was clinically similar for all patients, with a median of 0–1 days for all cohorts. For patients who received surgery, the number of grafting operations were similar with most patients only having one operation (p=0.4). Admission status, including proportion of patients, was similar between the groups, with the ICU admission rate ranging from 13–16% (p=0.2). The median ICU length of stay was 2 days for all groups, but the total median hospital length of stay was higher for African Americans at 3 days (IQR 1.0–6.0, p<0.001) compared to 2 days in all other groups.
We created a modified Poisson model to estimate the probability of an African American patient undergoing autologous skin grafting. The unadjusted risk ratio was 1.35 (95% 1.12, 1.64) for African American patients compared to all other races. When controlling for ADI national rank, age, %TBSA, and burn type, the adjusted risk ratio was 1.49 (95% CI 1.22, 1.83). Using a logistic regression model, we also graphed the predicted %TBSA based on worsening ADI National Rank, stratified by race. As shown in Figure 2, African Americans had a higher predicted %TBSA than other races for any ADI National Rank above 40.
Figure 2.

The predicted probability of % total burn surface area (TBSA) based on ADI National Rank, stratified by race.
Discussion
Our study shows that among pediatric burn patients admitted to a busy tertiary burn center in North Carolina, African American patients were disproportionally represented and had larger burns, even after controlling for social deprivation. Additionally, they were more likely to undergo autologous skin grafting compared to other races and had a longer hospital length of stay. The results of this study provide important insight into the demographics of pediatric burn patients in North Carolina and the impact of race on burn severity and surgical intervention. These findings are essential for ensuring appropriate interventions in the hospital setting and designing effective prevention strategies.
The association between burn incidence and increasing levels of social deprivation is well described in the literature.[9,11,14,20–22] This relationship is complex and multi-factorial. For example, studies have found higher rates of unsafe tap water temperatures in multi-family units and rental housing, which may be compounded by variability in the inspection and enforcement of safety regulations in lower-income areas.[23] Others have found increased risks associated with young or single-parent families, lower levels of parental education, and lack of safety measures (e.g., smoke detectors), among many others.[9,22–24] Our findings support this concept, showing that there is not only a higher frequency of burns among high ADI patients, but a direct correlation between ADI National Rank and predicted values for %TBSA. This phenomenon has been demonstrated previously and is likely explained in part by many of the same elements that increase burn incidence; namely, housing circumstances and family factors. [25,26]
Another well-established trend in pediatric burn research is the impact of race, specifically, that minority children are overrepresented among burn patients globally.[7–12,14] This is consistent with our study, which demonstrates that African American children comprised 33.7% of burn patients despite comprising only 22.3% of the state’s population.[27] In addition to over-representation, African Americans also had the highest median ADI National Rank compared to Non-Hispanic and Hispanic Caucasians, demonstrating more significant overall social deprivation. This finding is particularly notable given that our data and others have consistently illustrated that burns more frequently affect children with higher levels of social deprivation.[9,11,14,20–22] Many studies have used insurance status as a proxy for socioeconomic status to investigate the relationship between burn incidence, social deprivation, and race. While our results show a correlation between the percentage of Medicaid or uninsured patients and ADI, they do not necessarily lead to the same conclusions when other variables, such as race, are considered. For example, African American patients had a higher median ADI National Rank than Hispanic patients, but a lower percentage of uninsured or Medicaid patients.[7,9,20] This finding suggests that ADI represents a more nuanced approach to assessing socioeconomic status among patients, utilizing seventeen metrics for poverty, education, employment, and housing quality that may impact health outcomes. In contrast, insurance status is, at best, a crude proxy for SES.[17] Because minorities are often at higher risk of social deprivation due to a wide variety of historical, political, environmental, and social and systemic factors, using a more accurate measure of socioeconomic status is crucial for separating the effect of SES from the outcome within a particular racial or ethnic group.[28]
Existing data on the relationship between burn severity and race have been mixed, with some studies finding populations of color having more severe burns than Caucasians, and others showing no significant difference in severity between races.[7,29,30] Unfortunately, there is a notable gap in the literature on the independent effect of race on pediatric burn injury severity (i.e., whether minorities are still at higher risk for more severe burn injury when controlling for socioeconomic factors).[8,9,13,14] Our study shows that in addition to being overrepresented in the patient population, African American children also have a larger %TBSA burn than other races. Although the difference in median TBSA between African Americans and Caucasians (non-Hispanic) was statistically significant (3% vs 2%), what is more striking is the relationship between ADI and %TBSA among African Americans compared to others. When stratifying by race, the %TBSA predicted by logistic regression demonstrated African Americans with larger burns for all ADI National Ranks above 40, with %TBSA corresponding to higher levels of area deprivation. While African Americans did have the highest percentage of scald burns, which are associated with a larger %TBSA, given that Caucasian Hispanic patients had a nearly identical rate of scald burns but decreased %TBSA, it is less likely that this accounts for the difference.[9] Furthermore, it is notable that this disparity between African American %TBSA and other races worsens as ADI increases. This implies that socioeconomic status alone cannot explain the trends in burn injuries among African American patients and further highlights the need for additional research into the independent effect of race on burn incidence and characteristics.
Despite the apparent racial disparities among the pediatric burn population, our data suggest that African American patients had adequate access to medical interventions for burns, evidenced by the high rates of autologous skin grafting. Compared to other races, African American children had a higher adjusted probability of undergoing autologous skin grafting irrespective of ADI, age, %TBSA, or burn type. Because this difference is not seen among Caucasian patients (Non-Hispanic or Hispanic), skin color may play a role. When darker-skinned individuals are burned, the contrast between the light dermal or subcutaneous tissues and the darker surrounding epidermis is stark. Few tools are available to objectively analyze the degree of burn wound severity, leading physicians to rely on clinical evaluation using visual and tactile inspection of wound characteristics.[31] Several studies have shown that the assessment of tissue damage by clinical evaluation alone results in variable ratings of wound severity among physicians. They suggest that this leads to an inconsistent analysis of burn severity, which may, in turn, impact treatment protocol selection.[31–34] Although autografts typically have better aesthetic outcomes than less aggressive approaches, they are more costly and may be associated with multiple operations, potential donor-site morbidity, and other complications.[35] Therefore, the factors involved in surgical planning for pediatric burn patients must be investigated further to ensure patients are receiving the most appropriate interventions, and consideration is given to more objective methods of analysis, such as laser Doppler imaging or histological analysis of punch biopsies.[31]
Finally, our study found that African American patients had overall longer hospital stays, despite the median time to the first operation and ICU length of stay being similar among all groups. It is conceivable that this discrepancy may be explained by the increased utilization of autologous skin grafting, as it is a more involved procedure compared to wound care, temporary biological dressing, or allograft.[36] This would make a compelling case for addressing the factors underlying differences in surgical intervention among races, as longer hospital stays are associated with increased morbidity and higher costs.[37] However, other explanations should also be explored. For example, given the higher markers for social deprivation among African Americans, patients may have had delayed discharge due to a perceived or confirmed lack of support at home following discharge, accommodation preparation, transportation issues, or other social factors. Additional reasons may include wound complications, treatment for psychological concerns, or comorbid medical conditions.[38,39] The etiology of this finding is likely multifactorial, particularly when considering the larger %TBSA and more aggressive surgical interventions for African American patients.
Our study is limited by its retrospective design, in that only patients admitted to the UNC Jaycee Burn Center were included. This excludes patients who received treatment at other facilities and those unable to seek treatment, biasing the results towards patients with larger, more severe burns who arrived via ambulance or those with access to transportation. We have attempted to reduce the impact of this bias by contextualizing the patient population using ADI and burn severity. Furthermore, although ADI is a more nuanced proxy for socioeconomic status compared to insurance status alone, it remains limited in its ability to characterize individuals as it is ultimately population-level data.
Conclusion
African American children were disproportionately represented among pediatric burn patients, even when controlling for ADI. They also had longer hospital stays and were more likely to have autologous skin grafting, even accounting for burn size and type. The overlapping features of higher social deprivation and minority status create a unique risk for African American patients. Further investigation is indicated to assess the intersection between SES and race and factors underlying specific surgical interventions to inform best treatment practices and future preventative strategies.
Highlights.
African American (AA) children were disproportionately represented in pediatric burn patients and had larger burns, even when controlling for ADI.
AA children had longer hospital stays and were more likely to have autologous skin grafting, even accounting for burn size and type.
Overlap of higher social deprivation and minority status creates a unique risk for AA patients
Further investigation is indicated to assess the intersection between SES and race and factors underlying specific surgical interventions to inform best treatment practices and future preventative strategies
Acknowledgments
Financial Support
Financial support was provided by the North Carolina Jaycee Burn Center in the Department of Surgery at the University of North Carolina for all aspects of the study, including the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Conflict of Interest
The authors have no conflict of interest to disclose. The authors have no financial relationships to disclose.
IRB: The University of North Carolina Institutional Review Board approved this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Borse NN, Gilchrist J, Rudd RA, Ballesteros MF, Sleet DA. CDC Childhood Injury Report: Patterns of Unintentional Injuries among 0 –19 Year Olds in the United States, 2000–2006. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control 2008. [Google Scholar]
- [2].Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death, 1999–2020 Results. CDC WONDER Online Database 2021. http://wonder.cdc.gov/ucd-icd10.html (accessed July 28, 2022). [Google Scholar]
- [3].Krishnamoorthy V, Ramaiah R, Bhananker SM. Pediatric burn injuries. Int J Crit Illn Inj Sci 2012;2:128–34. 10.4103/2229-5151.100889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Children’s Safety Network. Fire and Burn Prevention 2021 Resource Guide 2021. [Google Scholar]
- [5].Klas KS, Vlahos PG, McCully MJ, Piche DR, Wang SC . School-based prevention program associated with increased short- and long-term retention of safety knowledge. J Burn Care Res 2015;36:387–93. 10.1097/BCR.0000000000000151. [DOI] [PubMed] [Google Scholar]
- [6].Sharma RK, Parashar A. Special considerations in paediatric burn patients. Indian J Plast Surg 2010;43:S43–50. 10.4103/0970-0358.70719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kramer CB, Rivara FP, Klein MB. Variations in U.S. pediatric burn injury hospitalizations using the national burn repository data. J Burn Care Res 2010;31:734–9. 10.1097/BCR.0b013e3181eebe76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Fagenholz PJ, Sheridan RL, Harris NS, Pelletier AJ, Camargo CA. National study of Emergency Department visits for burn injuries, 1993 to 2004. J Burn Care Res 2007;28:681–90. 10.1097/BCR.0B013E318148C9AC. [DOI] [PubMed] [Google Scholar]
- [9].Rimmer RB, Weigand S, Foster KN, Wadsworth MM, Jacober K, Matthews MR, et al. Scald burns in young children--a review of Arizona burn center pediatric patients and a proposal for prevention in the Hispanic community. J Burn Care Res 2008;29:595–605. 10.1097/BCR.0b013e31817db8a4. [DOI] [PubMed] [Google Scholar]
- [10].Tan KT, Prowse PM, Falder S. Ethnic differences in burn mechanism and severity in a UK paediatric population. Burns 2012;38:551–5. 10.1016/j.burns.2011.10.005. [DOI] [PubMed] [Google Scholar]
- [11].Hayes JR, Groner JI. Minority status and the risk of serious childhood injury and death. J Natl Med Assoc 2005;97:362–9. [PMC free article] [PubMed] [Google Scholar]
- [12].Mistry RM, Pasisi L, Chong S, Stewart J, She RBW. Socioeconomic deprivation and burns. Burns 2010;36:403–8. 10.1016/j.burns.2009.05.021. [DOI] [PubMed] [Google Scholar]
- [13].Saeman MR, Hodgman EI, Burris A, Wolf SE, Arnoldo BD, Kowalske KJ, et al. Epidemiology and outcomes of pediatric burns over 35 years at Parkland Hospital. Burns 2016;42:202–8. 10.1016/j.burns.2015.10.011. [DOI] [PubMed] [Google Scholar]
- [14].Lee CJ, Mahendraraj K, Houng A, Marano M, Petrone S, Lee R, et al. Pediatric Burns: A Single Institution Retrospective Review of Incidence, Etiology, and Outcomes in 2273 Burn Patients (1995–2013). J Burn Care Res 2016;37:e579–85. 10.1097/BCR.0000000000000362. [DOI] [PubMed] [Google Scholar]
- [15].Brown RL. Epidemiology of injury and the impact of health disparities. Curr Opin Pediatr 2010;22:321–5. 10.1097/MOP.0b013e3283395f13. [DOI] [PubMed] [Google Scholar]
- [16].Bartley CN, Atwell K, Cairns B, Charles A. Racial and ethnic disparities in discharge to rehabilitation following burn injury. J Burn Care Res 2019;40:143–7. 10.1093/jbcr/irz001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the Neighborhood Atlas. N Engl J Med 2018;378:2456–8. 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Zou G A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–6. 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- [19].Chen W, Qian L, Shi J, Franklin M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol 2018;18:63. 10.1186/s12874-018-0519-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Padalko A, Cristall N, Gawaziuk JP, Logsetty S. Social complexity and risk for pediatric burn injury: A systematic review. J Burn Care Res 2019;40:478–99. 10.1093/jbcr/irz059. [DOI] [PubMed] [Google Scholar]
- [21].Hippisley-Cox J, Groom L, Kendrick D, Coupland C, Webber E, Savelyich B. Cross sectional survey of socioeconomic variations in severity and mechanism of childhood injuries in Trent 1992–7. BMJ 2002;324:1132. 10.1136/bmj.324.7346.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Peck MD. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns 2011;37:1087–100. 10.1016/j.burns.2011.06.005. [DOI] [PubMed] [Google Scholar]
- [23].Bentivegna K, McCollum S, Wu R, Hunter AA. A state-wide analysis of pediatric scald burns by tap water, 2016–2018. Burns 2020;46:1805–12. 10.1016/j.burns.2020.06.009. [DOI] [PubMed] [Google Scholar]
- [24].Alnababtah K, Khan S, Ashford R. Socio-demographic factors and the prevalence of burns in children: an overview of the literature. Paediatr Int Child Health 2016;36:45–51. 10.1179/2046905514Y.0000000157. [DOI] [PubMed] [Google Scholar]
- [25].Alnababtah K, Khan S. Socio-demographic factors which significantly relate to the prediction of burns severity in children. Int J Burns Trauma 2017;7:56–63. [PMC free article] [PubMed] [Google Scholar]
- [26].Purcell LN, Bartley C, Purcell ME, Cairns BA, King BT, Charles A. The effect of neighborhood Area Deprivation Index on residential burn injury severity. Burns 2021;47:447–54. 10.1016/j.burns.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].United States Census Bureau. North Carolina. United States Census Bureau QuickFacts 2021. https://www.census.gov/quickfacts/fact/table/NC (accessed July 7, 2022). [Google Scholar]
- [28].Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc 2007;99:1013–23. [PMC free article] [PubMed] [Google Scholar]
- [29].Alnababtah KM, Davies P, Jackson CA, Ashford RL, Filby M. Burn injuries among children from a region-wide paediatric burns unit. Br J Nurs 2011;20:156, 158–62. 10.12968/bjon.2011.20.3.156. [DOI] [PubMed] [Google Scholar]
- [30].Hendrix L, Charles A, Buchholz V, Jones S, Cairns B . Influence of race and neighborhood on the risk for and outcomes of burns in the elderly in North Carolina. Burns 2011;37:762–9. 10.1016/j.burns.2011.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Jaspers MEH, van Haasterecht L, van Zuijlen PPM, Mokkink LB. A systematic review on the quality of measurement techniques for the assessment of burn wound depth or healing potential. Burns 2019;45:261–81. 10.1016/j.burns.2018.05.015. [DOI] [PubMed] [Google Scholar]
- [32].Singh V, Devgan L, Bhat S, Milner SM. The pathogenesis of burn wound conversion. Ann Plast Surg 2007;59:109–15. 10.1097/01.sap.0000252065.90759.e6. [DOI] [PubMed] [Google Scholar]
- [33].Godina M, Derganc M, Brčič A. The reliability of clinical assessment of the depth of burns. Burns 1977;4:92–6. 10.1016/0305-4179(77)90123-1. [DOI] [Google Scholar]
- [34].Jackson DM. The diagnosis of the depth of burning. Br J Surg 1953;40:588–96. 10.1002/bjs.18004016413. [DOI] [PubMed] [Google Scholar]
- [35].Figus A, Leon-Villapalos J, Philp B, Dziewulski P. Severe multiple extensive postburn contractures: a simultaneous approach with total scar tissue excision and resurfacing with dermal regeneration template. J Burn Care Res 2007;28:913–7. 10.1097/BCR.0b013e318159eb8c. [DOI] [PubMed] [Google Scholar]
- [36].Ratner D Skin grafting. Semin Cutan Med Surg 2003;22:295–305. 10.1016/S1085-5629(03)00079-8. [DOI] [PubMed] [Google Scholar]
- [37].Rosman M, Rachminov O, Segal O, Segal G. Prolonged patients’ In-Hospital Waiting Period after discharge eligibility is associated with increased risk of infection, morbidity and mortality: a retrospective cohort analysis. BMC Health Serv Res 2015;15:246. 10.1186/s12913-015-0929-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Hussain A, Dunn KW. Predicting length of stay in thermal burns: a systematic review of prognostic factors. Burns 2013;39:1331–40. 10.1016/j.burns.2013.04.026. [DOI] [PubMed] [Google Scholar]
- [39].Engrav LH, Heimbach DM, Rivara FP, Kerr KF, Osler T, Pham TN, et al. Harborview burns--1974 to 2009. PLoS ONE 2012;7:e40086. 10.1371/journal.pone.0040086. [DOI] [PMC free article] [PubMed] [Google Scholar]


