Abstract
Background
Piriformis syndrome (PS) is a common disease that is difficult to clinically treat, which seriously affects people’s health and living quality. Multiple clinical studies have demonstrated that acupuncture therapy is an effective treatment for PS, but the optimal method of various acupuncture methods has remained unknown. The aim of this study protocol is to compare the efficacy and the safety of different acupuncture methods for PS.
Methods
We will search seven electronic bibliographic databases (PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure, Wanfang Database, Chinese Biomedical Literature Database, and Chongqing VIP Database) from inception to June 2023. Randomized controlled trials (RCTs) will be selected for assessing the effectiveness of acupuncture therapy on PS. Primary outcome measure for this study is pain intensity, and the secondary outcomes are clinical symptoms and signs, physical activity, effective rate, and adverse events. Study selection, data extraction, and risk of bias assessment will be independently completed by at least two reviewers. Then, standard pairwise meta-analysis and network meta-analysis will be conducted using Revman 5.3, Stata V.15.1 and OpenBUGS V.3.2.3. The heterogeneity will be explored by subgroup, meta-regression, and sensitivity analysis, if applicable. Finally, Grading of Recommendations, Assessment, Development and Evaluation (GRADE) pro system will be used to evaluate the quality of evidence.
Results
Our systematic review and network meta-analysis will identify the best acupuncture treatment method for PS patients.
Conclusion
The results of our review will help decision-makers make educated choices regarding evidence-based acupuncture management options for PS.
Prospero Registration Number
No. CRD42022335028.
Keywords: piriformis syndrome, systematic review, network meta-analysis, protocol
Introduction
The piriformis muscle is closely related to the sciatic nerve, as the sciatic nerve passes under or goes through the piriformis muscle.1 Piriformis syndrome (PS) is a painful disease in the posterior part that restricts hip movement due to persistent contraction of the piriformis muscle and repetitive trauma or ischemia, which may lead to sciatic nerve entrapment, manifested as pain, numbness or tingling in the hip.2 The prevalence of PS ranged from 12.2% to 27%. PS usually occurs unilaterally in women and middle-aged people.3,4 It is estimated that 0.3% to 6% of the people suffering from low back pain and sciatica may be caused by PS, with an annual incidence of around 2.4 million cases of PS.5 PS not only seriously affects the patients’ work and daily activities but also adds a heavy burden of medical costs to society and families.
In clinical practice, PS is mainly treated with anti-inflammatory, antipyretic and analgesic drugs such as diclofenac sodium or ibuprofen, but their efficacy is not satisfactory and they are often accompanied by certain side effects and gastrointestinal adverse reactions.6 Therefore, there is an urgent need to find alternative therapies, especially traditional Chinese medicine therapies.
Acupuncture therapy is becoming increasingly popular globally.7 As a complementary and alternative therapy, it has been used to relieve a variety of painful conditions, including PS.8,9 In China, many clinical trials have been reported that various acupuncture methods such as manual acupuncture, electroacupuncture, and warm acupuncture can effectively treat PS. The effects of these methods may vary because their mechanisms are not identical. For example, manual acupuncture has been observed to elicit a diverse array of central nervous system reactions, which implicate various limbic structures such as the amygdala, hippocampus, hypothalamus, and cerebellum, as evidenced by fMRI and electroencephalography.10 It is believed that electroacupuncture provides a greater “dose” of acupuncture treatment compared to manual acupuncture due to the extended duration and heightened intensity of stimulation. Additionally, it is thought to elicit a more significant activation of endogenous opioid mechanisms.11 This phenomenon has the potential to result in greater clinical outcomes in conditions related to pain.11,12 Furthermore, the mechanism of warm acupuncture is primarily associated with the thermal effects, radiation effects, and pharmacological actions of moxa and its combustion products.13 As for laser acupuncture, its mechanisms may relate to changes in gene expression mediated via changes in nitric oxide.14 At present, there is no evidence-based recommendation for acupuncture treatment of PS. Thus, the relative effectiveness of different acupuncture therapies for PS is warranted to be further explored.
Network meta-analysis (NMA) is a method to compare multiple treatments simultaneously in a single meta-analysis, which can be used to obtain the potential best choice among different treatments.15 Therefore, we will comprehensively retrieve relevant data to assess and compare the effectiveness and safety of different acupuncture therapies (and their combinations) for the treatment of PS using NMA.
The purpose of this NMA is to compare the effectiveness and safety of all available acupuncture methods in the treatment of patients with PS. Our primary objective is to evaluate pain control effects. We will also compare their effect on clinical symptoms and physical signs, physical activity, effective rate, and treatment safety.
Methods
Study Registration
This NMA will be conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)16 and PRISMA-NMA guidelines.17 The proposed systematic review was registered on PROSPERO (CRD42022335028) and is available on the PROSPERO.com website (https://www.crd.york.ac.uk/prospero/).
Eligibility Criteria
Types of Studies
This system review will only include randomized controlled trials (RCTs) reported in English or Chinese. Ongoing studies, cross-over trials, quasi-RCTs, cluster RCTs or any other types of non-RCTs will be excluded.
Types of Participants
Adult patients diagnosed with PS, without severe hepatic and renal impairment, and patients with tumors; while race, nationality, gender, and age are not restricted.
Types of Interventions
Studies incorporating acupuncture as the primary intervention modality will be included. We will include any of the following treatments: manual acupuncture, electroacupuncture, warm acupuncture, auricular acupuncture, etc, or a combination of any two or three of these methods. Furthermore, studies that apply acupuncture as the experimental intervention in conjunction with other pharmacological or physical treatments, with a primary focus on evaluating the efficacy of acupuncture, will also be included. There are no restrictions on the selection of acupuncture points, methods of operation, duration of treatment and follow-up period.
Types of Control Groups
Studies using placebo, sham acupuncture or conventional drugs in the control groups and studies comparing different types of acupuncture therapies will be included. However, studies comparing different acupuncture point prescriptions or manual needling techniques will be excluded.
Types of Outcome Measurements
We will include trials with one or more of the outcomes mentioned below, or else exclude the trial.
Primary Outcome(s)
Our primary outcome of this review will be the pain intensity. Based on preliminary searches of relevant articles, pain intensity measurements were reported in most studies. Pain intensity is usually presented by using the Visual Analogue Scale or other validated scales.
Secondary Outcome(s)
The secondary outcomes will include (i) clinical symptoms and signs measured using the validated scales; (II) physical activity measured using the Harris hip scoring (HHS) system or other validated scales; and (III) effective rate measured mainly on the basis of relief in the sign and symptoms of the disease. Safety outcomes include the type and frequency of adverse events, such as syncope, abnormal sensation, and subcutaneous hematoma.
Data Sources and Search Strategy
We will search electronic libraries in English and Chinese, including PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang Database, China Biomedical Literature Database (CBM), and Chongqing VIP Database (VIP), and the retrieval time will be set from inception to June 2023. Languages will be limited to Chinese and English. The search terms we will use in this review will be a combination of medical subject terms and free-text terms. Search strategies take PubMed as an example, which is shown in Table 1. Depending on the characteristics of each database, this search strategy will be adjusted according to the constraints of each database.
Table 1.
Search Strategy for PubMed Database
| No. | Search Terms |
|---|---|
| #1 | MeSH terms: “piriformis muscle syndrome” |
| #2 | Title/Abstract: “piriformis syndrome” OR “piriformis muscle syndrome” OR “musculi piriformis syndrome” OR “PS” OR “PMS” |
| #3 | #1 OR #2 |
| #4 | MeSH terms: “acupuncture therapy” OR “acupuncture” OR “cupping therapy” OR “bloodletting” |
| #5 | Title/Abstract: “acupuncture” OR “manual acupuncture” OR “electroacupuncture” OR “body acupuncture” OR “auricular acupuncture” OR “electro-acupuncture” OR “auricular acupressure” OR “warm needling” OR “warm acupuncture” OR “fire acupuncture” OR “cupping” OR “bloodletting” OR “blood-letting” OR “pricking blood” OR “needle” OR “needles” OR “needling” |
| #6 | #4 OR #5 |
| #7 | Publication Type: “randomized controlled trial” |
| #8 | MeSH terms: “randomized controlled trials as topic” |
| #9 | Title/abstract: “randomized” OR “randomly” OR “RCT” OR “trial” |
| #10 | #7 OR #8 OR #9 |
| #11 | #3 AND #6 AND #10 |
Study Selection
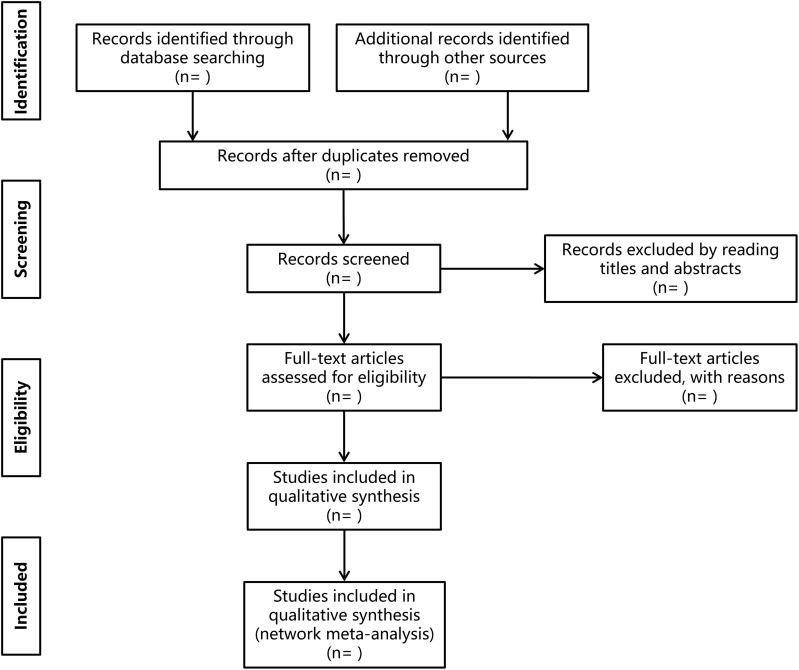
All researchers will receive complete system evaluation training. Bibliographic information and additional records from the search results in each database will be merged and imported into Endnote X9.2 after duplicate data elimination. Two researchers (Yujun He and Furui Miao) will independently search the databases and evaluated eligible articles based on the inclusion and exclusion criteria described above. They will screen the abstracts for all identified potential studies. All potentially relevant articles will be searched in full text for comprehensive assessment. Disagreement will be resolved by discussion or consensus with a third author (Yushan Fan). Contact the corresponding author by telephone or e-mail to obtain the missing data if necessary. The PRISMA flow diagram (Figure 1) will be used to show the research screening process.
Figure 1.
A PRISMA flow diagram of the literature screening and selection processes.
Notes: Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. Creative Commons.16
Data Extraction and Management
Two reviewers (Yujun He and Furui Miao) will independently extract the data from the included studies using a self-designed data acquisition form based on the Cochrane Handbook. The extracted data include (I) general information (author, publication year, journal, etc); (II) patient demographics (sample size, age, gender); (III) intervention details (type, frequency, and duration of acupuncture therapy); (IV) details of the control group (drug name, dose, acupuncture method, frequency, and duration of treatment); (V) outcomes (data for primary outcome indicators, secondary outcome indicators, adverse events); (VI) main conclusion and funding sources; and (VII) the complete list of acupuncture points. To ensure that results can be combined, multi-armed trials will be assigned to two-armed trials. Disagreement will be resolved through discussion or negotiation with a third author (Cai He or Jiujie He).
Risk of Bias Assessment
The Cochrane Risk of Bias (ROB2) Tool18 will be utilized by two reviewers (Fangzhi Zhang and Pu Yang) to evaluate the risk of bias associated with methodological quality. The tool in question consisted of six distinct components (randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, selection of the reported result, and overall bias) and the methodological quality was assessed and categorized as either low risk, high risk, or some concerns. The final decision-making process will be aided by a third author (Xinyi Zhao or Miaodong Wang). The ROB 2 plot will be generated using the revised Cochrane ROB 2 tool for randomized trials.
Statistical Analysis
Descriptive Statistics
We will conduct descriptive statistics for the frequency of acupoints in order to guide future studies on the standardization of effective acupuncture protocols. All of the acupoints from the included literature will be loaded into an Excel 2019 table, which will then be used to create a PivotTable to perform descriptive statistical analysis on the frequency of included acupoints.
Standard Pairwise Meta-Analysis
Standard pairwise meta-analysis will be performed using RevMan 5.3 (Cochrane Collaboration Network, London, UK). Binary data will be expressed as risk ratio (RR). For continuous variables, the mean difference (MD) and their 95% confidence intervals (CIs) of the change score will be considered as a measure of relative treatment effect. When experiments used different measurement scales for a given outcome, the standardized MD (SMD) can be chosen. The I2 statistic will be used to assess heterogeneity among studies. When I2 < 50%, the Fixed Effect model will be adopted, and when I2 > 50%, the Random Effect model will be used.
Network Meta-Analysis
NMA is typically used to compare multiple interventions simultaneously. We will use Stata V.15.1 to generate all network graphs containing comparisons for each outcome. The results of various types of acupuncture effects will be displayed: each line between two nodes means that the two interventions can be directly compared, and no line means that there is no direct correlation. Studies that are not connected to the network will be excluded from NMA. We will execute NMA within the framework of Bayesian hierarchy in OpenBUGS V.3.2.3. The random effect model with fuzzy prior will be fitted, and the combined treatment effect with 95% confidence interval will be obtained using Markov chain Monte Carlo (MCMC) method. We will run three MCMC chains with different initial value sets simultaneously. For each initial value, after dropping 10,000 simulations as a burn-in period, 60,000 simulations will be performed and convergence will be visually evaluated using GelmanRubin statistics.19 The posterior mean residual will be calculated and compared with the number of data points in the model to evaluate model fit.20 The subsurface cumulative ranking curve analysis in Stata V.15.1 will be used to evaluate the ranking probability of all included interventions.21,22
Assessment of Heterogeneity
The Q test and I² statistics will be used to assess the statistical heterogeneity among studies. According to the Cochrane Handbook, the thresholds for the interpretation of the I² statistics are as follows: 0–40%, might not be important; 30–60%, may reflect moderate heterogeneity; 50–90%, may indicate substantial heterogeneity; and 75–100%, represents considerable heterogeneity.23 If there is significant heterogeneity, we will look for potential sources of heterogeneity. Meanwhile, sensitivity or subgroup analysis will be performed to investigate the possible causes of heterogeneity.
Meta‐regression, Subgroup and Sensitivity Analysis
To assess the impact of covariates in heterogeneity, we will explore subgroup analysis or meta-regression when feasible. We will use the following study‐level covariates for meta‐regression: (I) sample size; (II) average age; and (III) the duration, frequency, and course of acupuncture methods. Subgroup analysis will be employed based on the different scales of pain, comparators and various forms of acupuncture methods. If subgroup analysis is still significantly heterogeneous, a sensitivity analysis will be performed. We will remove low-quality studies one by one and then merge the data. The meta-analysis will be repeated, and more low-quality studies will be excluded.
Assessment of Publication Bias
If more than 10 trials are included, we will use the funnel plot to assess the reported bias.24 We will use Egger’s regression test to analyze if the funnel plot is found to be asymmetrical.
Credibility of the Evidence
We will use the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) pro system (https://gradepro.org/) to grade the quality of evidence.25 This system assesses the following aspects: risk of bias, inconsistency, indirectness, imprecision, and other considerations.
Discussion
PS is caused by hypertrophy of the piriformis muscle compressing the sciatic nerve and manifests as signs and symptoms of sciatica, which are exacerbated by activity, prolonged sitting or walking.26 PS is a common and complex disease in the population, which seriously affects peoples’ quality of life.27 The treatment of PS usually includes short-term rest, the use of muscle relaxants, nonsteroidal anti-inflammatory drugs, and physical therapy. However, many patients with PS do not choose these treatments because of their poor pain relief and high side effects. In recent years, there have been many reports on the use of intramuscular injection therapy in the treatment of PS.28,29 Severe cases may require surgery, but the efficacy and safety of it for PS treatment is controversy.30 Recent studies have found that acupuncture is effective and safe in the treatment of neuropathic pain.31,32 However, there is a lack of relevant evidence-based medical evidence for PS.
NMA is a technique that integrates multiple variables for direct and indirect comparisons, which can be used to compare the efficacy of multiple treatments simultaneously in a single analysis.33 NMA for direct and indirect comparisons in a group of treatments, limited to the results of RCT studies, heterogeneity and inconsistency, which can analyze the inter-relationship between multiple interventions.34–36 In our protocol, only studies published in English or Chinese will be included, which may lead to potential selection bias. Our NMA will clearly define the types of acupuncture therapies included and their combined use to fully evaluate their effectiveness in the management of PS, which will be more persuasive.37 To the best of our knowledge, this study will be the first standard pairwise meta-analysis and NMA of acupuncture therapies for the treatment of PS. Despite these limitations, our proposed methodology will compare the efficacies of different acupuncture methods in the treatment of PS, so as to provide a clinical evidence-based medical basis.
Conclusion
Our findings will provide evidence for the optimal acupuncture method for patients with PS, helping clinicians and patients make a more informed decision together.
Strengths and Limitations of This Study
This study will be the first comprehensive analysis comparing various acupuncture therapies in the treatment of PS.
The data report will follow the PRISMA and PRISMA-NMA guidelines.
We will only include Chinese and English databases, which may result in potential bias.
We will only analyze acupuncture methods, not manual needling techniques.
Acknowledgments
The author would like to thank Professor Yushan Fan for his help in this study.
Funding Statement
This study is supported by National Natural Science Foundation of China (No: 82260983); The Special Project of TCM Talent Team Construction of Guangxi Administration of Traditional Chinese Medicine—Prof. Yushan Fan Guangxi Famous TCM Inheritance Studio (No: 2023017-05-07); Innovation Project of Guangxi Graduate Education (No: YCBZ2023149, No: YCSW2022351, No: YCSZ2022009).
Patient and Public Involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Ethics and Dissemination
Since the study was based on published systematic reviews, no ethical approval was required. The results of this systematic review will be disseminated through peer-reviewed publications or conference presentations.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to declare.
References
- 1.Smoll NR. Variations of the piriformis and sciatic nerve with clinical consequence: a review. Clin Anat. 2010;23(1):8–17. doi: 10.1002/ca.20893 [DOI] [PubMed] [Google Scholar]
- 2.Rodrigue T, Hardy RW. Diagnosis and treatment of piriformis syndrome. Neurosurg Clin N Am. 2001;12(2):311–319. doi: 10.1016/S1042-3680(18)30056-1 [DOI] [PubMed] [Google Scholar]
- 3.Leung FT, Mendis MD, Stanton WR, Hides JA. The relationship between the piriformis muscle, low back pain, lower limb injuries and motor control training among elite football players. J Sci Med Sport. 2015;18(4):407–411. doi: 10.1016/j.jsams.2014.06.011 [DOI] [PubMed] [Google Scholar]
- 4.Shah SS, Consuegra JM, Subhawong TK, Urakov TM, Manzano GR. Epidemiology and etiology of secondary piriformis syndrome: a single-institution retrospective study. J Clin Neurosci. 2019;59:209–212. doi: 10.1016/j.jocn.2018.10.069 [DOI] [PubMed] [Google Scholar]
- 5.Chang A, Ly N, Varacallo M. Piriformis Injection. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022. [Google Scholar]
- 6.Zhu Q, Zhu S, Xiong J, et al. Little needle-scalpel for piriformis syndrome: a protocol for systematic review and meta-analysis. Medicine. 2021;100(12):e25242. doi: 10.1097/md.0000000000025242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bücker B, Groenewold M, Schoefer Y, Schäfer T. The use of complementary alternative medicine (CAM) in 1 001 German adults: results of a population-based telephone survey. Gesundheitswesen. 2008;70(8–9):e29–e36. doi: 10.1055/s-2008-1081505 [DOI] [PubMed] [Google Scholar]
- 8.Shu H. Clinical observation on acupuncture treatment of piriformis syndrome. J Tradit Chin Med. 2003;23(1):38–39. [PubMed] [Google Scholar]
- 9.Spiller J. Acupuncture, ketamine and piriformis syndrome--a case report from palliative care. Acupunct Med. 2007;25(3):109–112. doi: 10.1136/aim.25.3.109 [DOI] [PubMed] [Google Scholar]
- 10.Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KKS. Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI. Hum Brain Mapp. 2005;24(3):193–205. doi: 10.1002/hbm.20081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayor D. An exploratory review of the electroacupuncture literature: clinical applications and endorphin mechanisms. Acupunct Med. 2013;31(4):409–415. doi: 10.1136/acupmed-2013-010324 [DOI] [PubMed] [Google Scholar]
- 12.Langevin HM, Schnyer R, MacPherson H, et al. Manual and electrical needle stimulation in acupuncture research: pitfalls and challenges of heterogeneity. J Altern Complement Med. 2015;21(3):113–128. doi: 10.1089/acm.2014.0186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deng H, Shen X. The mechanism of moxibustion: ancient theory and modern research. Evid Based Complement Alternat Med. 2013;2013:379291. doi: 10.1155/2013/379291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chung H, Dai T, Sharma SK, Huang -Y-Y, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516–533. doi: 10.1007/s10439-011-0454-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naing C, Reid SA, Aung K. Comparing antibiotic treatment for leptospirosis using network meta-analysis: a tutorial. BMC Infect Dis. 2017;17(1):29. doi: 10.1186/s12879-016-2145-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(jul21 1):b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–2385. doi: 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- 18.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 19.Gelman A, Rubin DB. Inference from iterative simulation using multiple sequences. Statis Sci. 1992;7(4):457–472. doi: 10.1214/ss/1177011136 [DOI] [Google Scholar]
- 20.Dias S, Ades AE, Welton NJ, Jansen JP, Sutton AJ. Network meta-analysis for decision making. 2018.
- 21.Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:58. doi: 10.1186/s12874-015-0060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bian Z, Yu J, Tu M, et al. Acupuncture therapies for postherpetic neuralgia: a protocol for a systematic review and Bayesian network meta-analysis. BMJ Open. 2022;12(3):e056632. doi: 10.1136/bmjopen-2021-056632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell; 2008. [Google Scholar]
- 24.Wang L, Xu M, Zheng Q, Zhang W, Li Y. The effectiveness of acupuncture in management of functional constipation: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2020;2020:6137450. doi: 10.1155/2020/6137450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Atkins D, Best D, Briss PA, Eccles M, Zaza S. GRADE Working Group: grading quality of evidence and strength of recommendations. 2009.
- 26.Aldashash F, Elraie M. Solitary osteochondroma of the proximal femur causing sciatic nerve compression. Ann Saudi Med. 2017;37(2):166–169. doi: 10.5144/0256-4947.2017.166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parlak A, Aytekin A, Develi S, Ekinci S. Piriformis syndrome: a case with non-discogenic sciatalgia. Turk Neurosurg. 2014;24(1):117–119. doi: 10.5137/1019-5149.Jtn.7904-13.0 [DOI] [PubMed] [Google Scholar]
- 28.Ozisik PA, Toru M, Denk CC, Taskiran OO, Gundogmus B. CT-guided piriformis muscle injection for the treatment of piriformis syndrome. Turk Neurosurg. 2014;24(4):471–477. doi: 10.5137/1019-5149.Jtn.8038-13.1 [DOI] [PubMed] [Google Scholar]
- 29.Ro TH, Edmonds L. Diagnosis and management of piriformis syndrome: a rare anatomic variant analyzed by magnetic resonance imaging. J Clin Imaging Sci. 2018;8:6. doi: 10.4103/jcis.JCIS_58_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nazlıkul H, Ural FG, Öztürk GT, Öztürk ADT. Evaluation of neural therapy effect in patients with piriformis syndrome. J Back Musculoskelet Rehabil. 2018;31(6):1105–1110. doi: 10.3233/bmr-170980 [DOI] [PubMed] [Google Scholar]
- 31.Macone A, Otis JAD. Neuropathic Pain. Semin Neurol. 2018;38(6):644–653. doi: 10.1055/s-0038-1673679 [DOI] [PubMed] [Google Scholar]
- 32.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002;136(5):374–383. doi: 10.7326/0003-4819-136-5-200203050-00010 [DOI] [PubMed] [Google Scholar]
- 33.Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331(7521):897–900. doi: 10.1136/bmj.331.7521.897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shim S, Yoon BH, Shin IS, Bae JM. Network meta-analysis: application and practice using Stata. Epidemiol Health. 2017;39:e2017047. doi: 10.4178/epih.e2017047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li T, Puhan MA, Vedula SS, Singh S, Dickersin K. Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. 2011;9:79. doi: 10.1186/1741-7015-9-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mills EJ, Thorlund K, Ioannidis JP. Demystifying trial networks and network meta-analysis. BMJ. 2013;346:f2914. doi: 10.1136/bmj.f2914 [DOI] [PubMed] [Google Scholar]
- 37.Corneille O, Havemann J, Henderson EL, et al. Beware ‘persuasive communication devices’ when writing and reading scientific articles. Elife. 2023;12. doi: 10.7554/eLife.88654 [DOI] [PMC free article] [PubMed] [Google Scholar]