Abstract
Objective:
Our aim was to evaluate the trend of effect of prior caesarean delivery (CD) on obstetric outcomes; and to investigate the existence of a threshold for order of CD associated with geometrical increase in complications.
Materials and methods:
We performed a retrospective cohort study of 942 parturients who undergone CD between June 2012 and May 2015 in a teaching hospital in Nigeria. The participants were stratified by the order of caesarean deliveries. We used linear-to-linear association to assess presence of a trend between the order of CD and categorical variables while Jonckheere-Terpstra was used to investigate whether a trend exist between order of CD and continuous variables. We also used multivariate logistic regression to evaluate the relative risk ratio of the outcome variables for each order of CD.
Results:
Composite adverse maternal outcome depicted a significant increasing trend from 1st CD (5.2%) to the 5thCD (50%). The relative risk ratio for composite adverse maternal outcome increased arithmetically from 1st CD to 3rd CD: RRR2.21, 95%CI 1.2–3.98 for 2ndCD; RRR3.39, 95%CI 1.60–9.27 for 3rdCD; followed by a geometric increase between 3rdCD and 4thCD (RRR11.64, 95%CI 3.20–18.86). In contrast, composite adverse fetal outcome did not depict a significant trend. However, perinatal death increased significantly from primary CD (4.6%) to 5thCD (33.3%).
Conclusion:
Maternal and fetal complications of repeat CD increase with increasing order of CD; and this trend became astronomical after the third CD. Couples should be counselled that both maternal and fetal complications increase with each additional CD and advised strongly to forgo future pregnancies after the 3rd CD.
Keywords: Caesarean Delivery, Complications, High-Order Caesarean Delivery, Trend
Introduction
Caesarean delivery (CD) is a lifesaving procedure to both mother and baby; however it is not without associated risks of morbidities and mortalities (1,2). The term ‘caesarean section’ was probably derived from ‘Lex Caesarea’ a decree in the Roman law (715672 B.C) requiring that the child be removed from the uterus before burying a pregnant woman who died in late pregnancy or a Latin verb ‘caedere’ meaning ‘to cut’ (3). Francis Rousset introduced the concept of performing the operation upon a living woman in the 16th century (3). In 1610, the first caesarean section was done on a living patient, who later died on the 25th post-operative day (3, 4). The early caesarean deliveries were associated with 100% maternal mortality as no sutures were placed on the uterus (3). The safety of CD has increased greatly due to improved surgical skills, potent antibiotics, improved anaesthesia and availability of blood transfusion services (1,2,3,5). Nevertheless, maternal morbidities are more likely with CD compared to vaginal (6). These morbidities can be short or long term with attending increased hospital stay and higher hospital cost (7).
Despite the accompanying morbidities and mortality, the caesarean section rates have been on the increase worldwide (8). According to WHO in 1985, the recommended CD rate is between 10% and 15% (9). Recently, there have been concerns about rising CD rates worldwide. New studies however revealed that maternal and neonatal mortality reduces as CD rate approaches 10%; but this benefit is lost as it rises above 10% (10). WHO however emphasised that it is important to ensure that CD is provided for a woman when it is needed; and not just to focus on achieving a specific rate (10). This will also help to optimize the use of CD and improve the quality of care.
Both maternal and fetal morbidities also tend increase with increasing order of CD (11–14). However, there were no conclusive reports about threshold beyond which patients should be unequivocally counselled to forgo future pregnancies (11, 12, 15). A Lebanese study suggested fourth CD as a threshold for counselling women to forgo future pregnancies (16). Conversely, a study conducted in Saudi Arabia did not support convectional practice of discouraging pregnancy after the third CD (12). Majority of these studies were conducted in the developed countries like United states of America and United Kingdom where health care delivery is quite advanced and maternal and fetal health indices are better that the reports from developing countries like Nigeria. Another peculiarity about Nigeria is the entrenched culture of aversion for CD among women; thereby culminating in majority of the procedures being carried out as an emergency surgery (17–19).
We therefore aimed to evaluate the trend of effect of prior CD on obstetric outcomes; and to investigate the existence of a threshold for order of CD associated with geometrical increase in complications. We hypothesised that there is an increasing trend in maternal and fetal adverse outcomes with increasing number of CD; and presence of a cut-off beyond which complications tend to increase geometrically.
Materials and methods
There were 3209 deliveries in this centre over a 3-year study period. The study centre provides tertiary health care to obstetric population in Osun State, and surrounding states in South-west Nigeria. We performed a retrospective cohort observational study of 942 parturients who undergone CD between June 2012 and May 2015 at a teaching hospital in Nigeria. Ethics approval was obtained from the hospital’s Ethics and Research Committee. The study population included women that undergone CD in this hospital during the study period. Exclusion criteria were previous myomectomy and gross fetal anomaly. All variables were obtained from individual’s medical records at the Health Information and management department of the hospital. Individual medical records were reviewed from the antenatal period till discharge after delivery. Also, babies’ medical records were reviewed to extract relevant data like birth weight, Apgar’s score and Neonatal Intensive care Unit (NICU) admission. Our primary outcomes were composite adverse maternal outcome and composite adverse neonatal outcome.
Composite adverse maternal outcome was defined as having any one of the following: massive blood transfusion, peripartum hysterectomy, uterine rupture, organ injury, placenta praevia, placenta accreta spectrum and Intensive Care Unit (ICU) admission. A composite adverse neonatal outcome was defined as either NICU admission and/or 5 minute Apgar score less than 7. Gestational age was defined by the last menstrual period, early dating ultrasound before week 24 of pregnancy, clinically or a combination of these parameters; whichever is the most appropriate. Unbooked patients were pregnant women who did not receive antenatal care in the hospital or those whose investigations were not reviewed before delivery. Emergency CD is a CD carried out after the onset of labour or after the onset of pregnancy complications. Maternal co-morbidities included medical conditions in pregnancy like hypertensive disorders of pregnancy, renal disorders, sickle disease anaemia, diabetes mellitus, thyroid disorders, chronic liver diseases etc. Adhesions were graded subjectively by the surgeons during the procedure into mild, moderate and severe. Organ injury included injury to adjacent organs like bladder, ureters and bowels. Intra-operative blood loss was estimated from the amount of blood in suction tube and value from blood soaked abdominal mops. Estimated blood loss during surgery was estimated by the anaesthetists while the need for blood transfusion was assessed by the anaesthetist in conjunction with the surgeon putting into consideration haemoglobin, blood loss at surgery and hemodynamic status of the patient. Massive blood transfusion was defined a transfusion with 4 or more units of blood. Post-partum haemorrhage (PPH) was defined as blood loss more than 1000 mls. Conservative surgery described B-lynch sutures and ligation of uterine arteries employed for conservative surgical management of PPH. Placenta praevia described placenta implantation in the lower uterine segment while placenta accreta spectrum described firmly adherent placenta to uterine wall that could only be delivered in piecemeal. Placental abruptio was defined as premature separation of the placenta before the delivery of the baby and was diagnosed by presence of retroplacenta clot during delivery. Scar dehiscence was defined as incomplete separation of uterine scar with intact serosa while uterine rupture was defined as complete separation of the uterine scar with/without extrusion of the fetus. Exploratory laparotomy referred to repeat surgery after caesarean delivery for burst abdomen or intraabdominal/pelvic collection. Duration of hospital stay was calculated in days from the day of caesarean delivery to discharge from the hospital. The need for ICU admission was evaluated by both anaesthetist and surgeon. Preterm delivery was defined as caesarean delivery before week 37 of the pregnancy. The need for NICU admission was determined by the neonatologist.
Data obtained was analysed with Statistical Package for Social Sciences version 23 by IBM Incorporated. The participants were stratified by the order of caesarean deliveries. We summarized continuous variables with means and standard deviations and categorical variables by frequency and percentages. We used linear-to-linear association to assess presence of a trend between the order of CD and categorical variables while Jonckheere-Terpstra was used to investigate whether a trend exist between order of CD and continuous variables. We also used multivariate logistic regression to evaluate the relative risk ratio of morbidity variables for each order of CD. Presence of threshold for astronomical increase in risk of adverse outcomes was investigated with a trend graph. A p-value of <0.05 was taken as statistically significant.
Results
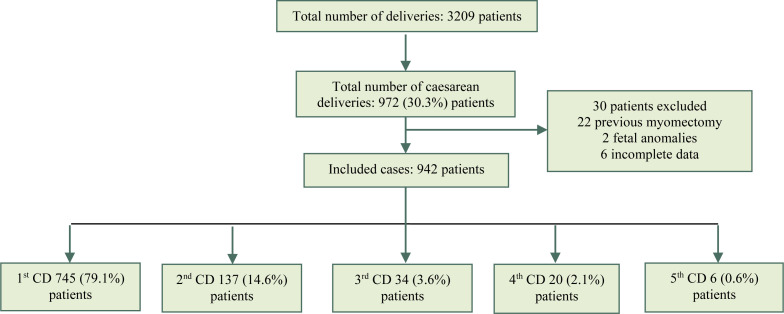
Of the 3209 deliveries in the hospital between June 2012 and May 2015, 972(30.3%) had caesarean deliveries (Figure 1). Nine hundred and forty-two participants were analyzed after excluding 30 participants (Figure 1). Among the participants, 745(79.1%), 137(14.6%), 34(3.6%), 20(2.1%) and 6(0.6%) participants undergone the 1st, 2nd, 3rd, 4th and 5th caesarean deliveries respectively. The mean age, mean estimated gestational age and mean parity of participants were 29.73years± 5.91, 38.58 weeks ± 2.5; and 1±1.25 respectively.
Figure 1:
Study participants stratified by number of caesarean deliveries
Unbooked patients (330) accounted for 35% of participants while 791(84.1%) had emergency caesarean deliveries. Most procedures (91.7%) were carried out by Senior residents in the department.
The most frequent indication for CD among the study population was failure to progress due to cephalopelvic disproportion (22.6%), trailed by fetal distress (12.7%), previous CD (9.5%), hypertensive disorders of pregnancy (9.1%), obstructed labour (8%); and others (38.95) Maternal complications were found in 171 (18.1%) women. Post-partum haemorrhage was the most common complication among the participants; it was reported in 80(8.5%) women. There were 5(0.53%) maternal deaths and 45 (4.8%) perinatal deaths.
Comparisons of baseline maternal characteristics across the stratified order of CD were presented in Table 1. There was significant trend in age, parity and maternal co-morbidities (Table 1).
Table 1:
Baseline characteristics of participants stratified by Number of caesarean deliveries
| Maternal factors | 1st CD | 2nd CD | 3rd CD | 4th CD | 5th CD | P valuea |
|---|---|---|---|---|---|---|
| Age | 29.53±5.31 | 31.23±4.47 | 29.26±6.15 | 29.50±5.07 | 32.33±3.38 | 0.02b* |
| Parity | 0.96±1.36 | 1.28±0.91 | 2.09±1.11 | 3.35±0.98 | 4.20±1.30 | <0.001b* |
| Gestational age | 38.35±2.72 | 38.52±2.72 | 38.35±1.95 | 37.95±1.91 | 38.45±2.60 | 0.18b |
| Unbooked | 287(38.5%) | 24(17.5%) | 8(23.5%) | 7(35%) | 4(66.7) | 0.96 |
| Emergency CD | 658(88.3%) | 90(65.7%) | 23(67.6%) | 15(75%) | 5(83.3%) | 0.42 |
| Multiple pregnancy | 26(3.5%) | 6(4.4%) | 0 | 0 | 0 | 0.33 |
| Maternal comorbidities | 79(10.6%) | 7(5.1%) | 3(8.8%) | 0 | 0 | 0.02* |
Statistically significant,
p-value calculated by linear-by-linear association unless otherwise specified,
p-value calculated by Jonckheere-Terpstra test for trends
CD, caesarean delivery
PPH, blood transfusion and massive blood transfusion showed highly significant increase from primary CD to the 5th CD. Surprisingly, estimated blood loss during surgery did not show a significant trend across the stratified order of CD. (Table 2) Peripartum hysterectomy increased significantly from 0.4% in primary CD to 16.7% in the 5th CD. Likewise, conservative surgeries for management of PPH increased from 0.8% in primary CD to 2.9% in the 3rd CD. Unlike placenta praevia and placenta accreta spectrum which showed a significant increasing trend from Ist CD to 5th CD, abruptio placenta and did not show a significant increasing trend. (Table 2) Scar dehiscence and uterine rupture also elucidated significant increasing trend from primary CD to 5th CD. (Table 2) The frequency of organ injury was higher in repeat CDs, reaching 10% in the 4th CD. ICU admission and maternal death were more frequent in higher-order CD (16.7% and 16.7%) compared with primary CD (0.8% and 0.3%) respectively.
Table 2:
Operative findings, maternal and fetal outcomes stratified by number of caesarean deliveries
| Maternal outcome | 1st CD (N=743) | 2nd CD (N=137) | 3rd CD (N=34) | 4th CD (N=20) | 5th CD (N=6) | p valuea |
|---|---|---|---|---|---|---|
| Composite adverse maternal outcome | 39(5.2%) | 12(8.8%) | 7(20.6%) | 7(35%) | 3(50%) | <0.001* |
| Moderate/Severe Adhesions | 0(0%) | 42(30.7%) | 19(55.8%) | 11(55%) | 4(66.7%) | 0.01* |
| Organ injury | 2(0.3%) | 2(1.5%) | 0 | 2(10%) | 0 | 0.001* |
| Estimated blood loss during surgery | 460.77± 373.66 | 554.89±554.10 | 558.33±279.71 | 515.00±205.90 | 521±298.36 | 0.26b |
| PPH | 38(5.5%) | 18(13.1%) | 10(29.4%) | 9(45%) | 3(50%) | 0.01* |
| Blood transfusion | 61(8.2%) | 19(13.9%) | 10(29.4%) | 7(35%) | 3(50%) | 0.01* |
| Massive blood transfusion | 6(0.8%) | 2(1.5%) | 4(11.8%) | 2(10%) | 1(16.7%) | <0.001* |
| Peripartum hysterectomy | 3(0.4%) | 5(3.6%) | 5(14.7%) | 4(20%) | 1(16.7%) | <0.001* |
| Conservative surgeries for PPH | 6(0.8%) | 4(2.9%) | 1(2.9%) | 0 | 0 | 0.02* |
| Placenta praevia | 39(5.2%) | 6(4.4%) | 3(8.8%) | 4(20%) | 1(16.7%) | 0.03* |
| Placenta accreta spectrum | 1(0.1%) | 5(3.6%) | 3(8.8%) | 3(15%) | 1(16.7%) | 0.01* |
| Placenta Abruptio | 39(5.2%) | 6(4.4%) | 0 | 2(10%) | 0 | 0.61 |
| Scar dehiscence | 0 | 7(5.1%) | 4(11.8%) | 3(15%) | 0 | 0.001* |
| Uterine rupture | 0 | 4(2.9%) | 2(5.9%) | 0 | 0 | 0.009* |
| Exploratory laparotomy | 11(1.5%) | 6(4.4%) | 3(8.8%) | 2(10%) | 1(16.7%) | 0.001* |
| Duration of hospital stay | 4.17±3.76 | 5.64±2.73 | 5.35±2.60 | 8.20±5.14 | 8.67±5.32 | 0.03*b |
| ICU admission | 6(0.8%) | 4(2.9%) | 2(5.9%) | 1(5%) | 1(16.7%) | 0.03* |
| Maternal death | 2(0.3%) | 0 | 1(2.9%) | 1(5%) | 1(16.7%) | 0.04* |
| Composite adverse fetal outcome | 207(27.8%) | 32(23.4%) | 4(11.8%) | 11(55%) | 2(33.3%) | 0.80 |
| Perinatal death | 34(4.6%) | 5(3.6%) | 2(5.9%) | 2(10%) | 2(33.3%) | 0.04* |
| Preterm delivery | 134(18%) | 16(11.7%) | 3(8.8%) | 5(25%) | 1(16.1%) | 0.33 |
| 1 minute Apgar score<7 | 167(22.7%) | 19(13.9%) | 7(20.6%) | 7(35%) | 3(50%) | 0.73 |
| 5 minute Apgar score<7 | 70(9.4%) | 8(5.8%) | 4(11.8%) | 3(15%) | 2(33.3%) | 0.31 |
| NICU admission | 207(27.8%) | 32(23.4%) | 4(11.8%) | 11(55%) | 2(33%) | 0.29 |
statistically significant
p value calculated by linear-by-linear association unless otherwise specified
p value calculated by Jonckheere-Terpstra test for trends
CD, caesarean delivery; ICU, Intensive care unit; PPH, post-partum haemorhage; NICU. Neonatal intensive care unit
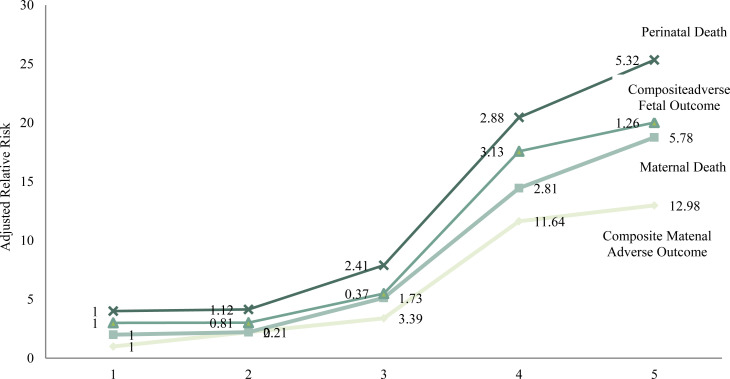
The composite adverse maternal outcome included all relevant variables to weight the effect of order of CD on maternal morbidity. There was a highly significant increasing trend from 1st CD (5.2%) to the 5th CD (50%). The relative risk ratio for composite adverse maternal outcome increased arithmetically from 1st CD to 3rd CD: RRR 2.21, 95% CI 1.2–3.98 for 2nd CD; RRR 3.39, 95%CI 1.60–9.27 for 3rd CD. However, there was a geometric increase from 3rd CD to 4th CD (RRR 11.64, 95% CI 3.20–18.86) followed closely by 5th CD (RRR 12.98, 95% CI 2.98–21.39) The trend for the increase in relative risk ratio of maternal mortality was also linear up to 3rd CD (RRR 1.73, 95% CI1.62–23.44), with a geometric increase at the 4th CD (RRR 2.81. 95% CI 1.62–23.44) followed by 5th CD (RRR 5.78, 95% CI 3.81–38.74) (Table 3).
Table 3:
Multivariate Logistic Regression for maternal Outcomes
| Maternal Outcomes | 1st CD | 2nd CD | 3rd CD | 4th CD | 5th CD |
|---|---|---|---|---|---|
| Composite adverse maternal outcome | |||||
| RRR (95% CI) | Referent | 1.50(0.95–2.37) | 3.99(3.92–16.28) | 11.39(3.35–10.98) | 17.97(3.23–31.60) |
| aRRR (95% CI) | Referent | 2.21(1.22–3.98) | 3.39(1.6–9.27) | 11.64(3.20–18.86) | 12.98(2.98–21.39) |
| p value | - | 0.02* | <0.001* | <0.001* | <0.001* |
| Post-partum Hemorrhage | |||||
| RRR (95% CI) | Referent | 2.81(1.55–5.01) | 2.60 (1.23–5.33) | 5.02(5.22–8.94) | 6.05(3.63–9.54) |
| aRRR (95% CI) | Referent | 2.07(1.12–7.66) | 4.48(2.29–14.20) | 8.48(6.78–10.39) | 7.50(3.03–10.10) |
| p value | - | <0.001* | <0.001* | 0.001* | 0.004* |
| Blood transfusion | |||||
| RRR (95% CI) | Referent | 0.98(0.50–1.91) | 1.08(0.32–3.65) | 1.98(0.56–6.94) | 5.60(1.00–10.23) |
| aRRR (95% CI) | Referent | 1.19(0.58–2.45) | 1.27(0.35–4.54) | 1.07(0.25–4.52) | 2.32(1.72–8.84) |
| p value | - | 0.63 | 0.72 | 0.92 | 0.01* |
| Massive blood transfusion | |||||
| RRR (95% CI) | Referent | 1.06(0.81–6.23) | 2.07(1.01–3.38) | 1.04(1.01–4.41) | 2.34(1.82–9.22) |
| aRRR (95% CI) | Referent | 1.70(0.34–2.40) | 1.67(1.19–2.40) | 2.22(1.19–7.78) | 3.26(1.24–7.31) |
| p value | - | 0.34 | 0.03* | 0.01* | 0.02* |
| Peripartum hysterectomy | |||||
| RRR (95% CI) | Referent | 2.48(2.36–3.47) | 6.66(1.92–10.31) | 6.17(1.50–8.53) | 3.70(3.49–9.28) |
| aRRR (95% CI) | Referent | 1.11(1.01–3.04) | 1.15(1.01–4.33) | 8.82(1.97–9.53) | 4.18(3.60–8.54) |
| p value | - | <0.001* | <0.001* | 0.001* | 0.003* |
| Placenta praevia | |||||
| RRR (95% CI) | Referent | 0.83(0.34–1.99) | 1.75(0.51–5.98) | 4.52(1.44–6.18) | 3.62(0.41–3.14) |
| aRRR (95% CI) | Referent | 0.47(0.72–1.75) | 1.71(0.49–5.98) | 4.60(1.43–7.79) | 5.40(1.58–5.97) |
| p value | - | 0.47 | 0.40 | 0.04* | 0.01* |
| Placenta accreta spectrum | |||||
| RRR (95% CI) | Referent | 2.8(2.32–12.44) | 2.7(2.50–7.12) | 3.11(1.29–13.27) | 4.18(1.84–7.25) |
| aRRR (95% CI) | Referent | 2.65(1.06–3.06) | 2.70(2.4–7.15) | 1.30(1.27–13.33) | 1.68(6.11–8.87) |
| p value | - | 0.003* | <0.001* | <0.001* | <0.001* |
| Intensive Care Unit admission | |||||
| RRR (95% CI) | Referent | 3.70(1.03–13.3) | 4.69(1.50–9.64) | 6.48(0.74–5.65) | 8.63(2.49–24.38) |
| aRRR (95% CI) | Referent | 4.55(1,18–7.47) | 4.56(1.44–9.57) | 6.93(0.77–7.20) | 8.98(1.94–20.55) |
| p value | - | 0.03* | 0.02* | 0.80 | 0.02* |
| Maternal death | |||||
| RRR (95% CI) | Referent | 0.00 | 1.25(0.99–12.73) | 3.55(1.69–22.5) | 7.43(5.76–9.57) |
| aRRR (95% CI) | Referent | 0.00 | 1.73(1.33–2.24) | 2.81(1.62–23.44) | 5.78(3.81–38.74) |
| p value | - | 0.99 | 0.03* | 0.02* | 0.003* |
Statistically significant
CD, caesarean delivery; RRR, relative risk ratio; aRRR, adjusted Relative risk ratio;
Relative risk ratios are adjusted for maternal age, parity, emergency caesarean delivery, unbooked patients, maternal co-morbidity and gestational age at delivery except for blood transfusion and massive blood transfusion that were adjusted for pre-operative packed cell volume.
Conversely, most adverse fetal outcome variables did not show any significant increase across the order of CD. (Table 2) Perinatal death is the only fetal outcome variable with a significant trend from primary CD (4.6%) to 5th CD (33.3%). The relative risk ratio for perinatal death for 5th CD was 5.32, 95% CI1.62–7.91. (Table 4) Composite adverse fetal outcome included available adverse fetal variables: NICU admission and 5 minute Apgar score less than 7; and it didn’t show any significant trend. (Table 2). Also, there was no significant trend in preterm delivery moving from 1st CD to 5th CD (Table 2).
Table 4:
Multivariate logistic Regression for fetal outcomes
| Maternal Outcomes | 1st CD | 2nd CD | 3rd CD | 4th CD | 5th CD |
|---|---|---|---|---|---|
| Composite adverse fetal outcome | |||||
| RRR (95% CI) | Referent | 0.79(0.52–1.21) | 0.35(0.12–0.10) | 3.18(1.30–7.78) | 1.30(0.24–7.15) |
| aRRR (95% CI) | Referent | 0.81(0.52–1.28) | 0.37(0.25–1.08) | 3.13(1.25–7.85) | 1.26(0.21–5.50) |
| p value | - | 0.37 | 0.07 | 0.02* | 0.99 |
| Perinatal death | |||||
| RRR (95% CI) | Referent | 0.79(0.30–2.06) | 1.31(0.30–5.68) | 2.32(0.52–10.42) | 10.46(1.85–19.09) |
| aRRR (95% CI) | Referent | 1.12(0.41–3.05) | 2.41(0.53–10.98) | 2.88(0.58–14.41) | 5.32(1.62–7.91) |
| p value | - | 0.82 | 0.26 | 0.20 | 0.02* |
| Preterm delivery | |||||
| RRR (95% CI) | Referent | 0.63(0.35–1.05) | 0.44(0.133–1.47) | 1.52(0.54–4.25) | 0.91(0.11–7.87) |
| aRRR (95% CI) | Referent | 0.68(0.38–1.21) | 0.51(0.15–1.71) | 1.62(0.57–4.58) | 1.03(0.99–1.06) |
| p value | - | 0.19 | 0.28 | 0.36 | 0.08 |
| 1 minute Apgar < 7 | |||||
| RRR (95% CI) | Referent | 0.55(0.33–0.92) | 0.88(0.37–2.06) | 1.84(0.72–4.67) | 3.41(0.68–17.04) |
| aRRR (95% CI) | Referent | 0.76(0.44–1.32) | 1.24(0.51–3.02) | 2.14(0.78–5.86) | 2.98(0.50–17.76) |
| p value | - | 0.34 | 0.64 | 0.14 | 0.23 |
| 5 minute Apgar < 7 | |||||
| RRR (95% CI) | Referent | 0.60(0.28–1.27) | 1.29(0.44–3.76) | 1.70(0.49–3.76) | 4.82(0.87–6.79) |
| aRRR (95% CI) | Referent | 0.93(0.42–2.06) | 1.97(0.64–6.10) | 2.00(0.53–7.60) | 3.70(0.57–8.79) |
| p value | - | 0.86 | 0.25 | 0.31 | 0.17 |
| NICU admission | |||||
| RRR (95% CI) | Referent | 0.79(0.52–1.21) | 0.34(0.12–1.00) | 3.18(1.30–7.78) | 1.30(0.24–7.15) |
| aRRR (95% CI) | Referent | 0.81(0.52–1.28) | 0.37(0.13–1.08) | 3.13(1.25–7.85) | 1.26(0.21–7.45) |
| p value | - | 0.37 | 0.07 | 0.02* | 0.80 |
Statistically significant
CD, caesarean delivery; NICU, neonatal intensive care unit; RRR, relative risk ratio; aRRR, adjusted Relative risk ratio;
Relative risk ratios are adjusted for maternal age, parity, emergency caesarean delivery, unbooked patients, maternal co-morbidity and gestational age at delivery
The trend graphs are available in Figure 2. The trend graphs for composite adverse maternal outcome, composite adverse fetal outcome, maternal death and fetal death depicted the 3rd CD as the game changer. There was a very steep slope between the 3rd and the 4th CD for these outcomes (Figure 2). This signifies a geometrical increase in both maternal and fetal complications after the 3rd CD.
Figure 2:
Trends of composite adverse maternal and fetal outcomes with order of caesarean delivery
Discussion
About a third of the parturients had CD, which was more than 2.1% reported by a population based study in Nigeria (18). This rate is however excusable because the hospital is a referral centre. Since this rate is higher than the recommended rate, it is quite necessary to beam a searchlight on the accompanying maternal and fetal morbidities so as to improve the quality of care being offered pregnant women (9, 10).
The convectional counselling of women to forgo future pregnancies after the 3rd or 4th CD due to anticipated morbidities without clear evidence in the literature and consideration for peculiarities of our environment dictated the need for this research (12). In Nigeria, many studies have documented increased risk of morbidities following repeat CD; but to our knowledge, neither has documented the trend in maternal and fetal morbidities nor attempt to investigate a cut-off for astronomical complications (20, 21, 22). Our findings clearly showed a steep rise in fetal and maternal complications between the 3rd and 4th CD. The risk of composite adverse maternal outcome increased geometrically by 11-fold for 4th CD and 12-fold for 5th CD compared with 3-fold increase for the 3rd CD. So, the 3rd CD appears to be the threshold for astronomical rise in complications. The findings by Makoha in Saudi Arabia showed steady rise in complications from 1st CD to 6 or more CD without any threshold for astronomical rise in complications (12). Makoha concluded that the 3rd CD did not appear as a threshold in the study population (12). Conversely, a Lebanese study showed a surge in maternal complications after the 4th CD (16). Differences in availability and accessibility of quality healthcare in these countries; and more importantly acceptability of CD among the parturients could explain these differences. A previous study in Nigeria that compared women with 4 or more CD with those with 3 or less CD found higher risk of complications among those with 4 or more CD but cut-off of 3 CD was taken arbitrarily from convectional expert opinions (20).
Likewise, there was a surge in both perinatal death and composite adverse perinatal outcome after the 3rd CD though this trend was not statistically significant. Perinatal deaths were significanty high in all the groups; subsequently the observed differences from the 1st CD to the 5th CD were not statistically significant. This may be attributed to high baseline perinatal mortality in Nigeria (23). Previous studies on fetal outcomes reported similar pattern in which difference in perinatal outcomes were not significant in countries with high perinatal mortality rates (24). In contrast, a study conducted in the United States reported earlier delivery and increased neonatal morbidity with repeat CD (13). The composite adverse perinatal mortality employed in our study did not include features like seizures and mechanical ventilation in the neonates. Exclusion of such variables may be responsible for our findings on neonatal morbidities. Preterm delivery was also not associated with number of prior CD in our study. Earlier studies have demonstrated association between preterm delivery and prior CD (13, 16).
In congruent with other studies, the risk for PPH, massive blood transfusion and peripartum hysterectomy increased significantly across the order of CD. The triad of placenta praevia, abruptio placenta and placenta accreta spectrum as a complication of multiple repeated CD has been studied by various studies. They have been found to be responsible for obstetric haemorrhage which is responsible for most morbidities (12, 25). The risk of placenta praevia and abruptio placenta increased progressively but abruptio placenta risk was insignificant. However, our finding of linear increase in scar dehiscence and uterine rupture contradicts some studies (12, 26). This observation is attributable to inherent aversion for CD in our society; thereby culminating in most procedures being done as emergency procedures after labour or complications have set in.
Being a retrospective review, some fetal outcomes were difficult to retrieve from the records and this limited the variables inculcated into composite adverse fetal outcomes. Also, some women were excluded due to incomplete data. Our study has been able to move up the level of evidence of limiting the number of CD to 3 in our environment from expert opinion to research based. However, the general is ability of this report is limited because it is a single-centre study.
Conclusion
In conclusion, maternal and fetal complications of repeat CD increase with increasing order of CD; and there appears to be astronomical increase in complications after the third CD. Couples should be counselled that both maternal and fetal complications increase with each additional CD and advised strongly to forgo future pregnancies after the 3rd CD because of geometrical increase in complication rates considering the prospect of a hospital supervised delivery in the subsequent pregnancies, religious and cultural inclinations about CD.
Acknowledgments
None.
Footnotes
Conflict of Interests
Authors have no conflict of interests.
Notes:
Citation: Okunola TO, Bola-Oyebamiji SB, Sowemimo O, Ajenifuja KO, Kuti O. Obstetric Outcomes in High-Order Repeat Caesarean Deliveries in Nigeria: A Single-Center Retrospective Study. . J Family Reprod Health 2022; 16(4): 254-63.
References
- 1.Suja D, Manjusha V, Simi B N, Nazeema A. Study of maternal outcome of emergency and elective caesarean section in a semi-rural tertiary hospital. National journal of medical research 2014; 4: 14–8. [Google Scholar]
- 2.Chu K, Cortier H, Maldonado F, Mashant T, Ford N, Trelles M. Cesarean section rates and indications in sub-Saharan Africa: a multi-country study from Medecins sans Frontieres. PLoS One 2012; 7: e44484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garba NA, Muhammad Z. Caesarean morbidity and mortality at Aminu Kano Teaching Hospital, Kano: a 2-year review. BOMJ 2011; 8: 11–4. [Google Scholar]
- 4.Decherney AH, Nathan L, Laufer N, Roman AS. CURRENT Diagnosis & Treatment: Obstetrics & Gynecology, 9th edition; McGraw Hill Publishers, 2003. [Google Scholar]
- 5.Okafor U, Efetie E, Ibe O. Anaesthesia and Outcome for Caesarean Delivery in the Parturient With Severe Co-Morbidity. The Internet Journal of Anaesthesiology. 2008; 21: 2. [Google Scholar]
- 6.Curtin SC, Gregory KD, Korst LM, Uddin SF. Maternal Morbidity for Vaginal and Cesarean Deliveries, According to Previous Cesarean History: New Data From the Birth Certificate, 2013. Natl Vital Stat Rep 2015; 64:1–13. [PubMed] [Google Scholar]
- 7.Firoz T, Chou D, von Dadelszen P, Agrawal P, Vanderkruik R, Tunçalp O, et al. Measuring maternal health: Focus on maternal morbidity. Bull World Health Organ 2013; 91:794–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hembah-Hilekaan SK, Ojabo A, Idogah S. Caesarean Section Rate in a Tertiary Hospital in Makurdi, North-Central Nigeria. General Medicine 2015; 3: 3. [Google Scholar]
- 9.Althabe F, Belizan JM. Caesarean section: The paradox. Lancet 2006; 368: 1472–3. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization . Caesarean sections should only be performed when medically necessary 2015.
- 11.Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity associated with multiple repeat Cesarean deliveries. Obstet Gynecol 2006; 107: 1226–32. [DOI] [PubMed] [Google Scholar]
- 12.Makoha FW, Felimban HM, Fathuddien MA, Roomi F, Ghabra T. Multiple cesarean section morbidity. Int J Gynaecol Obstet 2004; 87: 227–32. [DOI] [PubMed] [Google Scholar]
- 13.Forde B, DeFranco EA. Association of Prior Cesarean Delivery with Early Term Delivery and Neonatal Morbidity. Obstet Gynecol 2020; 135: 1367–76. [DOI] [PubMed] [Google Scholar]
- 14.Cook JR, Jarvis S, Knight M, Dhanjal MK. Multiple repeat caesarean section in the UK: incidence and consequences to mother and child. A national, prospective, cohort study. BJOG 2013; 120: 85–91. [DOI] [PubMed] [Google Scholar]
- 15.Lynch CM, Kearney R, Turner MJ. Maternal morbidity after elective repeat caesarean section after two or more previ procedures. Eur J Obstet Gynecol Reprod Biol 2003; 106:10–3. [DOI] [PubMed] [Google Scholar]
- 16.Ramadan MK, Ramadan K, El Tal R, Salem Wehbe GR, Itani S, Badr DA. How safe is high-order repeat cesarean delivery? An 8-year single-center experience in Lebanon. J Obstet Gynaecol Res 2020; 46:1370–7. [DOI] [PubMed] [Google Scholar]
- 17.Ezechi OC, Fasubaa OB, Kalu BE, Nwokoro CA, Obiesie LO. Caesarean delivery: why the aversion? Tropical Journal of Obstetrics and Gynaecology 2004;21: 164–7. [Google Scholar]
- 18.Adewuyi EO, Auta A, Khanal V, Tapshak SJ, Zhao Y. Caesarean delivery in Nigeria: prevalence and associated factors-a population-based cross-sectional study. BMJ Open 2019; 9:e027273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sunday-Adeoye I, Kalu CA. Pregnant Nigerian women’s view of cesarean section. Niger J Clin Pract 2011; 14: 276–9. [DOI] [PubMed] [Google Scholar]
- 20.Hyginus E, Eric NI, Lawrence I, Sylvester N. Morbidity and mortality following high order caesarean section in a developing country. J Pak Med Assoc 2012; 62: 1016–9. [PubMed] [Google Scholar]
- 21.Obuna JA, Ugboma HAA, Ejikeme BN, Umeora OUJ, Agwu UM. Pattern and outcome of higher order caesarean section in a secondary health facility in Nigeria. Research in Obstetrics and Gynecology 2012; 1: 9–22. [Google Scholar]
- 22.Orazulike NC, Alegbeleye JO. Pattern and outcome of higher order caesarean section in a tertiary health institution in Nigeria. International Journal of Tropical Disease & Health 2016; 17: 1–6. [Google Scholar]
- 23.National Population Commission (NPC) [Nigeria] and ICF . Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF. 2019. [Google Scholar]
- 24.Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet 2000; 356: 1375–83. [DOI] [PubMed] [Google Scholar]
- 25.Tamale-Sali EG, Iskander MN. Is there a risk of lower segment scar rupture in pregnancy after multiple caesarean section? Journal of Obstetrics and Gynaecology 1992; 12: 19–21. [Google Scholar]
- 26.Kirkinen P. Multiple caesarean sections: outcomes and complications. Br J Obstet Gynaecol 1988; 95: 778–82. [DOI] [PubMed] [Google Scholar]